Published online Sep 18, 2025. doi: 10.5312/wjo.v16.i9.110859
Revised: July 17, 2025
Accepted: August 25, 2025
Published online: September 18, 2025
Processing time: 85 Days and 13 Hours
Proximal humerus fractures (PHFs) are common, especially in the elderly, and optimal surgical management remains debated. This study compares clinical, functional, and radiographic outcomes of deltoid split (DS) vs deltopectoral (DP) approaches in PHFs treated with locking plates.
To evaluate and compare the clinical, functional, and radiographic outcomes-as well as postoperative complication rates-associated with the DS vs the DP surgical approach in the open reduction and internal fixation (ORIF) of PHFs using locking plate constructs.
A multicenter retrospective study of 120 patients undergoing ORIF for closed Neer type II-IV PHFs between January 2023 and December 2023. Patients were grouped by surgical approach [DS (n = 70), DP (n = 50)]. Outcome measures included Numeric Rating Scale (NRS) for pain, Quick-Disabilities in Arm, Shoulder, and Hand questionnaire (QuickDASH), Constant-Murley score, Short Form Health Survey-12v2, and radiographic alignment. Complication rates were recorded. Statistical significance was defined as P < 0.05.
Early outcomes favored the DS group: (1) Lower NRS (3.1 vs 5.9); (2) Higher Constant-Murley (68.2 vs 50.5); and (3) Better QuickDASH (25.4 vs 37.1). Complication rate was lower in the DS group (1.66% vs 5.81%). Radiographic outcomes were comparable. Long-term results were similar between groups.
While both approaches yield satisfactory long-term outcomes, the DS approach is associated with faster early recovery and fewer complications, supporting its use in selected cases.
Core Tip: This multicenter retrospective study compares deltoid split (DS) and deltopectoral approaches in proximal humerus fracture fixation with locking plates. While both methods achieved similar long-term results, the DS approach provided superior early functional outcomes and fewer complications. These findings suggest it may be the preferred technique in selected patients, particularly when early recovery is a priority.
- Citation: Cicio C, Longo G, Pavone V, Testa G, Ortuso R, Salvo GC, Ganci M, Prestianni I, Ferrara A, Kory A, Pietropaolo A, Monachino AM, Cuffaro ER, Papotto G. Deltopectoral vs deltoid split approach for proximal humerus fractures treated with locking plate: Our experience. World J Orthop 2025; 16(9): 110859
- URL: https://www.wjgnet.com/2218-5836/full/v16/i9/110859.htm
- DOI: https://dx.doi.org/10.5312/wjo.v16.i9.110859
Proximal humerus fractures (PHFs) represent approximately 5% of all fractures in adults and are the third most common fracture type in individuals over 65 years old. These injuries show a bimodal distribution, with low-energy falls in elderly patients and high-energy trauma in younger individuals. Treatment options vary depending on the fracture pattern, bone quality, and patient comorbidities. Open reduction and internal fixation (ORIF) using locking plates has become a standard approach for displaced PHFs, providing stable fixation and allowing early mobilization[1]. Two primary surgical approaches are currently used in ORIF: (1) The deltopectoral (DP); and (2) Deltoid split (DS) approaches. The DP approach offers broad exposure of the proximal humerus and familiarity among surgeons, whereas the DS approach provides direct lateral access with minimal soft tissue dissection.
Despite the widespread use of both techniques, there is no clear consensus in the literature regarding the superiority of one approach over the other in terms of clinical, functional, and radiographic outcomes. Comparative studies and meta-analyses have yielded conflicting results, with some favoring the DS approach for early recovery, while others report similar long-term outcomes between groups. Furthermore, differences in complication patterns, particularly related to humeral head vascularity and nerve injury risk, are still debated. A key unresolved question is whether the choice of surgical approach significantly influences early recovery and complication rates in patients undergoing ORIF with locking plates.
Based on this gap in current knowledge, we conducted a retrospective multicenter cohort study to compare early and long-term clinical, radiological, and functional outcomes between the DP and DS approaches for displaced PHFs treated with locking plates. Our aim was to evaluate not only functional recovery and complication rates, but also to explore whether the choice of approach independently affects these outcomes.
This was a retrospective multicenter cohort study conducted across three orthopedic departments in Italy between January 2023 and December 2023. A total of 120 patients with displaced PHFs were enrolled and treated surgically with ORIF using locking plate systems. All surgeries were performed by experienced shoulder surgeons with standardized protocols (Table 1).
| Variable | Deltoid split | Deltopectoral | P value |
| Number of patients | 70 | 50 | - |
| Female | 40 (57.1) | 28 (56.0) | 0.89 |
| Male | 30 (42.9) | 22 (44.0) | 0.89 |
| Mean age (years) | 56.0 ± 8.3 | 56.5 ± 7.9 | 0.76 |
| Fracture type (Neer II/III/IV) | 37/21/12 | 22/15/13 | 0.58 |
| Side (right/Left) | 38/32 | 27/23 | 0.97 |
| Incision length (cm) | 10.0 ± 1.2 | 13.0 ± 1.5 | < 0.001 |
| Operative time (minutes) | 68.5 ± 10.3 | 70.2 ± 9.7 | 0.45 |
| Follow-up duration (months) | 14.6 ± 2.8 | 14.3 ± 2.7 | 0.65 |
Inclusion criteria were: (1) Age > 18 years; (2) Closed, displaced PHFs classified as Neer type II, III, or IV; (3) Treatment with ORIF using either a DS or DP approach; and (4) Minimum follow-up of 12 months.
Exclusion criteria were: (1) Open or pathological fractures; (2) Pre-existing shoulder arthropathy; (3) Previous surgery on the affected shoulder; (4) Polytrauma patients; and (5) Incomplete clinical or radiographic follow-up.
Patients were divided into two groups according to the surgical approach used: (1) 70 patients underwent the DS approach; and (2) 50 patients the DP approach. In both groups, anatomical locking plates were used, and fracture reduction was confirmed intraoperatively using fluoroscopy. The choice of surgical approach was made at the discretion of the operating surgeon based on preoperative fracture pattern, soft tissue condition, surgeon’s experience, and the expected ease of fracture reduction. In general, the DS approach was preferred for fractures involving the greater tuberosity or those requiring more lateral exposure, while the DP approach was selected in complex three-part or four-part fractures requiring more extensive medial visualization and calcar reconstruction. All procedures were performed in the beach chair position under general anesthesia.
DP approach: The patient was positioned in the beach chair position with the arm draped freely. A skin incision was made along the DP groove, starting from the coracoid process and extending distally for approximately 12–15 cm. The DP interval was identified and developed with lateral retraction of the deltoid and medial retraction of the pectoralis major. The cephalic vein was preserved whenever possible. This approach provided excellent access to the anterior and medial humeral head, calcar, and lesser tuberosity, facilitating anatomical reduction in complex fractures. However, it required extensive soft tissue dissection and had limited exposure of the greater tuberosity.
DS Approach: In this technique, a skin incision of approximately 8–10 cm was made lateral to the acromion, centered over the deltoid muscle. The fibers of the anterior and middle deltoid were split bluntly in line with the muscle fibers, typically not extending more than 5 cm distal to the acromion to avoid injury to the axillary nerve. The axillary nerve was identified and protected when necessary. This approach allowed direct access to the lateral aspect of the proximal humerus, making it particularly useful for fractures involving the greater tuberosity. The DS approach minimized soft tissue disruption and preserved the anterior vascular supply but offered more limited visualization of the medial calcar.
Clinical outcomes were assessed using the following validated scoring systems.
Constant-Murley Score: A composite score evaluating shoulder function across four domains: (1) Pain (15 points); (2) Daily activities (20 points); (3) Range of motion (40 points); and (4) Strength (25 points). The maximum score is 100, with higher scores indicating better function[2].
Quick-Disabilities in Arm, Shoulder, and Hand questionnaire: An 11-item self-reported questionnaire measuring upper limb disability and symptoms. Scores range from 0 (no disability) to 100 (severe disability)[3].
Numeric Rating Scale for pain: Patients rate their pain on a scale from 0 (no pain) to 10 (worst imaginable pain), providing a simple and reliable assessment of pain intensity[4].
Short Form Health Survey-12v2: A standardized tool to assess health-related quality of life across physical and mental domains. It generates two summary scores (Physical Component Summary and Mental Component Summary), with higher values representing better perceived health status.
Radiographic analysis included: (1) Measurement of head-shaft angle; (2) Assessment of medial calcar restoration; and (3) Detection of complications such as implant failure, avascular necrosis (AVN), and nonunion.
All patients followed a standardized postoperative protocol supervised by a physiotherapist. The operated arm was immobilized in a sling for comfort for the first 10–14 days. Passive range-of-motion exercises, including pendulum movements, were initiated on postoperative day one, unless contraindicated by fracture complexity or poor fixation stability.
From week 3 to 6, assisted active motion exercises were introduced, focusing on forward flexion and external rotation. Strengthening exercises targeting the rotator cuff and deltoid muscles began after radiographic evidence of healing, typically after 6–8 weeks.
Patients operated via the DP approach often required a slightly more cautious progression due to more extensive soft tissue dissection, particularly during early abduction movements. In contrast, those undergoing the DS approach generally tolerated earlier lateral movement but required careful monitoring to avoid axillary nerve irritation.
Clinical and radiographic follow-ups were scheduled at 2 weeks, 6 weeks, 3 months, 6 months, and 12 months postoperatively.
Continuous variables were reported as mean ± SD, while categorical variables were expressed as frequencies and percentages. The Shapiro–Wilk test was used to assess normality. Between-group comparisons were performed using the Students’ t-test or Mann–Whitney U test for continuous data and the χ2 or Fisher’s exact test for categorical variables. A P < 0.05 was considered statistically significant. Data were analyzed using Statistical Package for the Social Sciences v26.0 (IBM Corp., Armonk, NY, United States) (Table 2).
| Parameter | Description |
| Study design | Multicenter retrospective cohort study |
| Study period | January 2023–December 2023 |
| Total patients | 120 |
| Surgical approaches | Deltoid split (n = 70), deltopectoral (n = 50) |
| Inclusion criteria | Age > 18, Neer type II–IV, closed fracture, open reduction and internal fixation, 12-month follow-up |
| Exclusion criteria | Open/pathological fractures, prior surgery, incomplete data, polytrauma |
| Implant type | Anatomical locking plate |
| Outcomes measured | Constant-Murley, Quick-Disabilities in Arm, Shoulder, and Hand questionnaire, Numeric Rating Scale, Short Form Health Survey-12v2 |
| Radiographic evaluation | Head-shaft angle, calcar restoration, complications |
| Statistical analysis | t-test, Mann–Whitney U, χ2, Fisher’s exact; P < 0.05 |
A total of 120 patients were included in the study, with 70 (58.3%) treated using the DS approach and 50 (41.7%) treated via the DP approach. Baseline demographics and fracture characteristics were similar between groups (Table 3). According to the Neer classification, the majority of patients presented with type II and III fractures in both cohorts (Table 4).
| Group | Number of patients | Percentage |
| Deltoid split | 70 | 58.3 |
| Deltopectoral | 50 | 41.7 |
| Group | Neer II | Neer III | Neer IV |
| Deltoid split | 37 | 21 | 12 |
| Deltopectoral | 22 | 15 | 13 |
The mean incision length was significantly shorter in the DS group (10 ± 1.2 cm) compared to the DP group (13 ± 1.5 cm). Mean operative time was 68.5 ± 10.3 minutes for DS and 70.2 ± 9.7 minutes for DP (no statistical significance of P value). All procedures were performed under general anesthesia, with the patient in the beach chair position. No intraoperative complications were reported. Postoperative radiographs confirmed an adequate reduction in all cases, defined as head-shaft angle 130° ± 10° with calcar restoration.
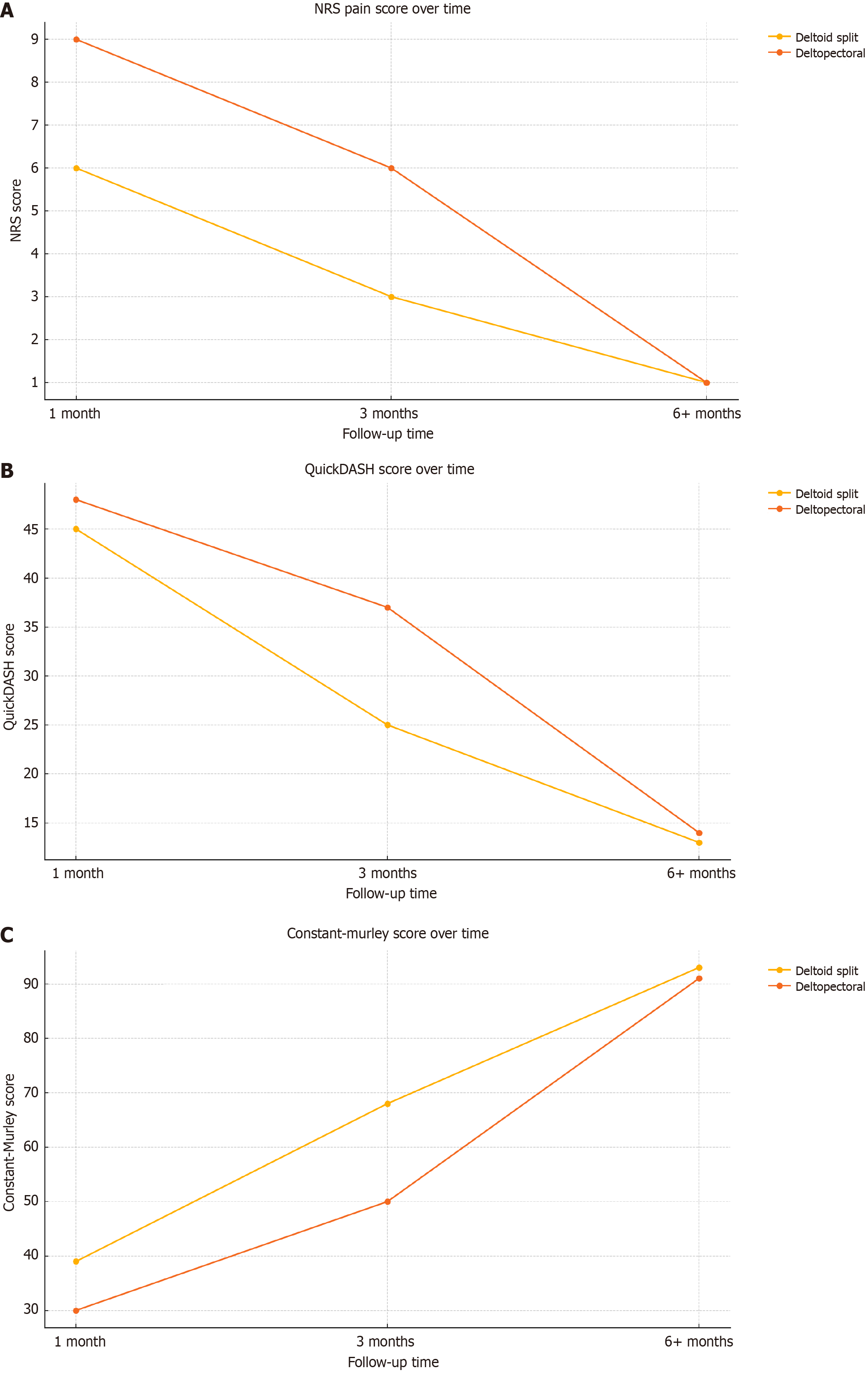
At 1-month follow-up, pain levels and functional scores favored the DS group. The DS group had a lower mean Numeric Rating Scale (NRS) score (6.0 ± 1.4) compared to the DP group (9.0 ± 1.5, P < 0.001), and a higher Constant-Murley score (39 ± 6.8 vs 30 ± 7.1, P = 0.004). Quick-Disabilities in Arm, Shoulder, and Hand questionnaire (QuickDASH) scores were also slightly better in the DS group (45.2 ± 8.7 vs 48.3 ± 7.5, P = 0.09), although not statistically significant. At 3 months, intergroup differences became more pronounced. The DS group showed: (1) Lower NRS scores (3.1 ± 1.2 vs 5.9 ± 1.3, P < 0.001); (2) Higher Constant-Murley scores (68.2 ± 8.1 vs 50.5 ± 9.4, P = 0.002); (3) Lower QuickDASH scores (25.4 ± 7.8 vs 37.1 ± 6.9, P < 0.001); and (4) Lower Short Form Health Survey (SF)-12v2 scores (32.6 ± 6.3 vs 40.3 ± 5.4, P = 0.003) (Table 5, Figure 1).
| Parameter | Deltoid split (mean ± SD) | Deltopectoral (mean ± SD) | P value |
| Numeric Rating Scale Score | 3.1 ± 1.2 | 5.9 ± 1.3 | < 0.001 |
| Quick-Disabilities in Arm, Shoulder, and Hand questionnaire | 25.4 ± 7.8 | 37.1 ± 6.9 | < 0.001 |
| Short Form Health Survey-12v2 | 32.6 ± 6.3 | 40.3 ± 5.4 | 0.003 |
| Constant-Murley | 68.2 ± 8.1 | 50.5 ± 9.4 | 0.002 |
By the 6-month follow-up and beyond, differences between the groups diminished. Both groups demonstrated favorable clinical outcomes: (1) Constant-Murley: DS: 93 ± 4.2, DP: 91 ± 5.1 (P = 0.32); (2) QuickDASH: DS: 13.2 ± 4.6, DP: 14.1 ± 5.2 (P = 0.47); and (3) NRS: 1.0 ± 0.7 in both groups (P = 0.90). These findings indicate that while early recovery is accelerated in the DS group, both approaches ultimately converge to similar long-term results (Table 6).
| Time point | Numeric Rating Scale (DS/DP) | Quick-Disabilities in Arm, Shoulder, and Hand questionnaire (DS/DP) | Short Form Health Survey-12v2 (DS/DP) | Constant-Murley (DS/DP) |
| 1 month | 6/9 | 45/48 | 47/52 | 39/30 |
| 3 months | 3/6 | 25/37 | 32/40 | 68/50 |
| 6+ months | 1/1 | 13/14 | 16/15 | 93/91 |
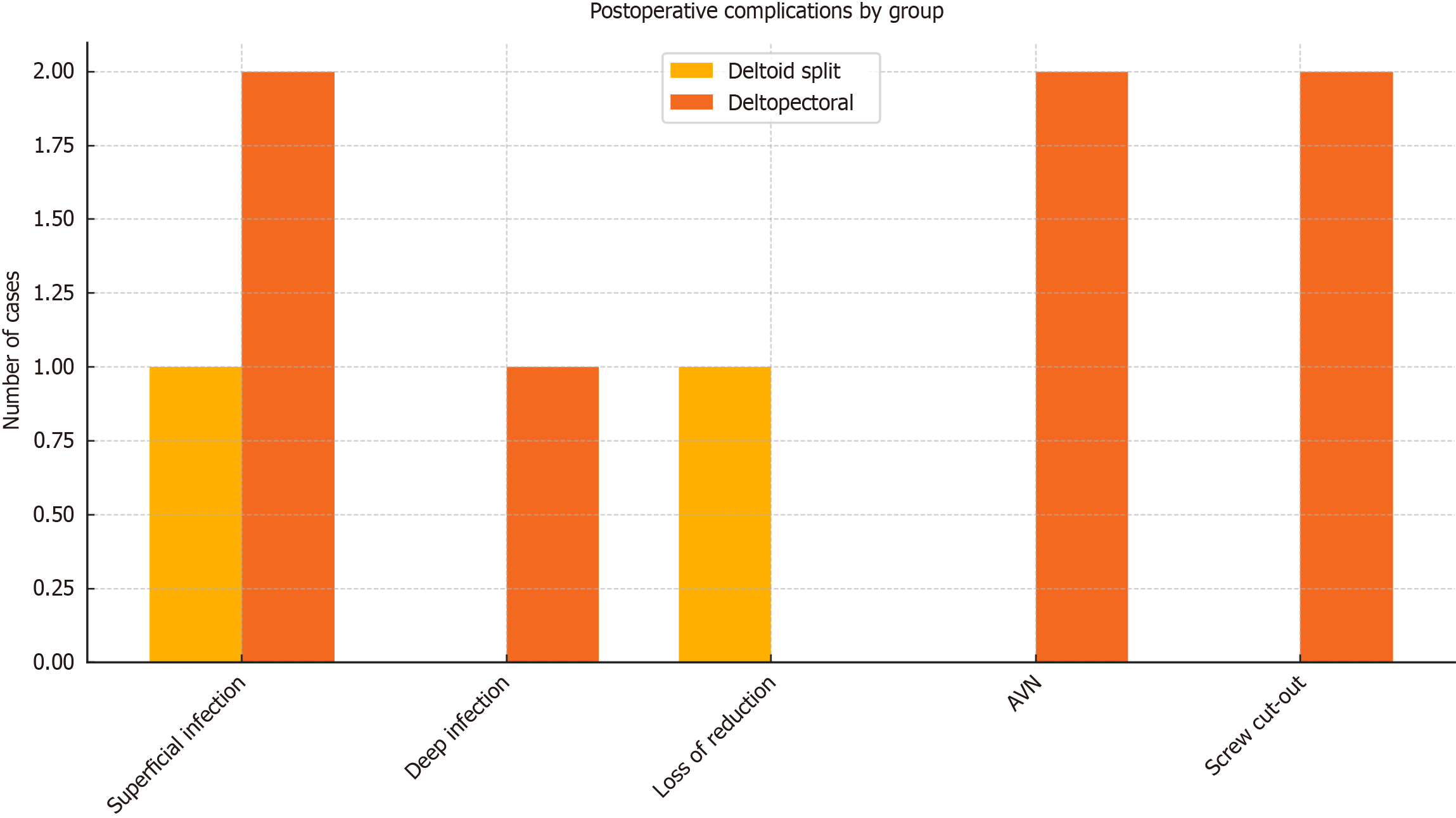
The overall complication rate was significantly lower in the DS group (1.66%) compared to the DP group (5.81%, P = 0.04) (Table 7, Figure 2). In the DS group, one patient developed a superficial wound infection and one experienced secondary loss of reduction, though clinical function was preserved. In the DP group, complications included: (1) Two superficial infections; (2) One deep infection requiring hardware removal and local antibiotic application; (3) Two cases of AVN of the humeral head; and (4) Two screw cut-outs requiring surgical revision. No cases of neurovascular injury were recorded in either group. A total of 120 patients met the inclusion criteria and were enrolled. Of these, 70 (58.3%) were treated using the DS approach, and 50 (41.7%) with the DP approach. Groups were homogeneous in terms of sex, age, and fracture classification. In the DS group, there were 40 females and 30 males (mean age 56), with 37 Neer II, 21 Neer III, and 12 Neer IV fractures. The DP group included 28 females and 22 males (mean age 56.5), with 22 Neer II, 15 Neer III, and 13 Neer IV fractures. Surgery duration was similar, though incisions were shorter in the DS group (10 cm vs 13 cm in DP). Radiographic evaluation confirmed adequate reduction in all cases. Pain and functional scores were better in the DS group during early follow-up. At 1 month, NRS was 6 in DS and 9 in DP; Constant-Murley was 39 vs 30; QuickDASH was 45 vs 48. At 3 months, DS patients improved more rapidly: (1) NRS was 3 vs 6; (2) Constant-Murley was 68 vs 50; (3) QuickDASH was 25 vs 37; and (4) SF-12v2 was 32 vs 40. At later follow-ups, outcomes were comparable (Constant-Murley was 93 vs 91, QuickDASH was 13 vs 14, NRS was 1 in both). Complications were lower in the DS group (1.66%) than in DP (5.81%). DS had one superficial infection and one loss of reduction without clinical impact. DP had two superficial infections, one deep infection requiring implant removal, two AVN cases, and two screw cut-outs needing revision surgery.
| Complication | Deltoid split (n) | Deltopectoral (n) |
| Superficial wound infection | 1 | 2 |
| Deep infection | 0 | 1 |
| Loss of reduction | 1 | 0 |
| Avascular necrosis | 0 | 2 |
| Screw cut-out | 0 | 2 |
We performed a subgroup analysis to evaluate whether clinical and functional outcomes differed based on patient age, sex, fracture type (Neer classification), side of injury, and incision length. No statistically significant interaction was observed between these variables and the choice of surgical approach.
Age and sex: Both younger and older patients achieved similar improvements in functional scores within each group, with no significant interaction between age or sex and surgical outcomes (P > 0.05).
Fracture type: Patients with Neer II, III, and IV fractures showed consistent outcome trends within each surgical group, with the DS approach maintaining superior early functional scores irrespective of fracture complexity.
Side of injury: No difference in outcomes was observed between right-sided and left-sided fractures within or between groups.
Incision length: While incision length differed significantly between approaches, it did not correlate with postoperative pain or functional recovery. Data on plate length were not systematically recorded and thus could not be included in the comparative analysis.
Numerous studies have compared the DP and DS approaches in the surgical treatment of PHFs, yet no definitive consensus has been reached regarding their relative efficacy. Several systematic reviews and meta-analyses, including those by Wu and Shen[5] and Xie et al[6], have demonstrated that the DS approach may offer advantages in terms of shorter operative time, reduced intraoperative blood loss, and improved early functional outcomes-particularly higher Constant-Murley scores at 3 months. These studies also noted that long-term outcomes such as pain scores and rates of AVN were generally comparable between approaches.
Conversely, randomized controlled trials have shown conflicting results. Rouleau et al[7] reported better long-term QuickDASH and SF-12v2 scores with the DP approach, while Basavanagowda et al[8] found no significant differences between the two techniques in long-term follow-up. Such inconsistencies highlight the complex interplay of patient factors, fracture type, and surgeon preference in determining optimal outcomes. PHFs are increasingly common due to aging populations. Palvanen et al[9] showed an increase of incidence from 32/100000 to 105/100000 from 1970 to 2002. The better treatment is still debate in literature. Iyengar et al[10] showed that nonoperative treatment of PHFs de
Strengths: This study benefits from a relatively large and homogenous sample size for a surgical cohort, with patients treated in multiple high-volume orthopedic centers following standardized surgical and postoperative protocols. Additionally, the use of validated outcome measures and long-term clinical and radiographic follow-up (up to 36 months) enhances the reliability of the findings.
Limitations: As a retrospective study, it is inherently subject to selection and information bias. Despite efforts to standardize treatment, surgical decision-making and technique may have varied slightly between centers. Moreover, the lack of randomization limits the ability to establish causality. The absence of preoperative functional scores and patient-reported outcome measures also restricts the baseline comparability. Finally, although complication rates were recorded, specific time points and severity gradings were not uniformly documented.
This multicenter retrospective cohort study demonstrates that both the DP and DS approaches for proximal humerus fracture fixation with locking plates can achieve comparable long-term functional outcomes. However, the DS approach was associated with significantly faster early recovery, lower pain scores, and a reduced complication rate-particularly concerning AVN and implant-related failures. These findings suggest that the choice of surgical approach does influence early postoperative trajectories, likely due to differences in soft tissue handling, vascular preservation, and ease of lateral exposure for implant positioning. The DS approach, when performed with meticulous technique and adequate nerve protection, represents a valuable option in selected patients, particularly in those where early mobilization and functional recovery are priorities. Future prospective, randomized controlled trials with larger cohorts are warranted to confirm these results and to further elucidate the specific patient populations that might benefit most from each surgical approach.
| 1. | Murray IR, Amin AK, White TO, Robinson CM. Proximal humeral fractures: current concepts in classification, treatment and outcomes. J Bone Joint Surg Br. 2011;93:1-11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 144] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 2. | Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987;160-164. [PubMed] |
| 3. | Beaton DE, Wright JG, Katz JN; Upper Extremity Collaborative Group. Development of the QuickDASH: comparison of three item-reduction approaches. J Bone Joint Surg Am. 2005;87:1038-1046. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 440] [Cited by in RCA: 750] [Article Influence: 35.7] [Reference Citation Analysis (0)] |
| 4. | Williamson A, Hoggart B. Pain: a review of three commonly used pain rating scales. J Clin Nurs. 2005;14:798-804. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1542] [Cited by in RCA: 2020] [Article Influence: 96.2] [Reference Citation Analysis (0)] |
| 5. | Wu Z, Shen W. An updated systematic review and metaanalysis comparing deltoidsplit approach with deltopectoral approach for proximal humerus fractures. Exp Ther Med. 2023;25:296. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 6. | Xie L, Zhang Y, Chen C, Zheng W, Chen H, Cai L. Deltoid-split approach versus deltopectoral approach for proximal humerus fractures: A systematic review and meta-analysis. Orthop Traumatol Surg Res. 2019;105:307-316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 23] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 7. | Rouleau DM, Balg F, Benoit B, Leduc S, Malo M, Vézina F, Laflamme GY. Deltopectoral vs. deltoid split approach for proximal HUmerus fracture fixation with locking plate: a prospective RAndomized study (HURA). J Shoulder Elbow Surg. 2020;29:2190-2199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 23] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 8. | Basavanagowda P, Jain P, Bisaleri J, Jakhar B. Comparative study between deltoid split approach versus delto pectoral approach for proximal humerus fracture fixation. Int J Res Orthop. 2023;9:988-993. [DOI] [Full Text] |
| 9. | Palvanen M, Kannus P, Niemi S, Parkkari J. Update in the epidemiology of proximal humeral fractures. Clin Orthop Relat Res. 2006;442:87-92. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 457] [Cited by in RCA: 434] [Article Influence: 21.7] [Reference Citation Analysis (0)] |
| 10. | Iyengar JJ, Devcic Z, Sproul RC, Feeley BT. Nonoperative treatment of proximal humerus fractures: a systematic review. J Orthop Trauma. 2011;25:612-617. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 77] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 11. | Syed UAM, Aleem AW, Wowkanech CD, Weekes D, Freedman M, Pepe MD, Tjoumakaris FP, Abboud JA, Austin LS. The Effect of Preoperative Education on Opioid Consumption in Patients Undergoing Arthroscopic Rotator Cuff Repair: A Prospective, Randomized Control Trial. J Shoulder Elbow Surg. 2018;27:e123. [DOI] [Full Text] |
| 12. | Hohmann E, Keough N, Glatt V, Tetsworth K. Surgical treatment of proximal humerus fractures: a systematic review and meta-analysis. Eur J Orthop Surg Traumatol. 2023;33:2215-2242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 19] [Reference Citation Analysis (0)] |
| 13. | Yahuaca BI, Simon P, Christmas KN, Patel S, Gorman RA 2nd, Mighell MA, Frankle MA. Acute surgical management of proximal humerus fractures: ORIF vs. hemiarthroplasty vs. reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2020;29:S32-S40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 76] [Article Influence: 12.7] [Reference Citation Analysis (0)] |
| 14. | Bhayana H, Chouhan DK, Aggarwal S, Prakash M, Patel S, Arora C, Dhillon MS. Outcomes of plate osteosynthesis for displaced 3-part and 4-part proximal humerus fractures with deltopectoral vs. deltoid split approach. Eur J Trauma Emerg Surg. 2022;48:4559-4567. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 15. | Hepp P, Theopold J, Voigt C, Engel T, Josten C, Lill H. The surgical approach for locking plate osteosynthesis of displaced proximal humeral fractures influences the functional outcome. J Shoulder Elbow Surg. 2008;17:21-28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 87] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 16. | Buecking B, Mohr J, Bockmann B, Zettl R, Ruchholtz S. Deltoid-split or deltopectoral approaches for the treatment of displaced proximal humeral fractures? Clin Orthop Relat Res. 2014;472:1576-1585. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 50] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 17. | Kishore JV, Kale AR, Patil V, Sonawane S, Kopparthi RM, Jani C, Vadlamudi A. Intraoperative Parameters of Comminuted Proximal Humerus Fractures: A Comparison Between Deltoid-Split and Deltopectoral Approaches. Cureus. 2022;14:e26443. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 18. | Liu B, Wang X, Wang C, Jiao Z, Chen W. Displaced proximal humerus fractures treated with ORIF via the deltoid interfascicular approach vs the deltopectoral approach: A prospective case-control study. Medicine (Baltimore). 2022;101:e29075. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 19. | Schliemann B, Siemoneit J, Theisen Ch, Kösters C, Weimann A, Raschke MJ. Complex fractures of the proximal humerus in the elderly--outcome and complications after locking plate fixation. Musculoskelet Surg. 2012;96 Suppl 1:S3-11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 94] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 20. | Ruchholtz S, Hauk C, Lewan U, Franz D, Kühne C, Zettl R. Minimally invasive polyaxial locking plate fixation of proximal humeral fractures: a prospective study. J Trauma. 2011;71:1737-1744. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 34] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 21. | Wang JQ, Lin CC, Zhao YM, Jiang BJ, Huang XJ. Comparison between minimally invasive deltoid-split and extended deltoid-split approach for proximal humeral fractures: a case-control study. BMC Musculoskelet Disord. 2020;21:406. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 22. | Handoll HH, Ollivere BJ, Rollins KE. Interventions for treating proximal humeral fractures in adults. Cochrane Database Syst Rev. 2012;12:CD000434. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 87] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 23. | Sirisreetreerux N, Pengrung N, Apivatthakakul T. Proximal humerus exposure with the inverted-L anterolateral deltoid flip approach, anterolateral deltoid splitting approach, and deltopectoral approach: A comparative cadaveric study. Injury. 2021;52:738-746. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 24. | Kimmeyer M, Schmalzl J, Rentschler V, Schieffer C, Macken A, Gerhardt C, Lehmann LJ. Correct positioning of the calcar screw leads to superior results in proximal humerus fractures treated with carbon-fibre-reinforced polyetheretherketone plate osteosynthesis with polyaxial locking screws. J Orthop Traumatol. 2023;24:54. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/