INTRODUCTION
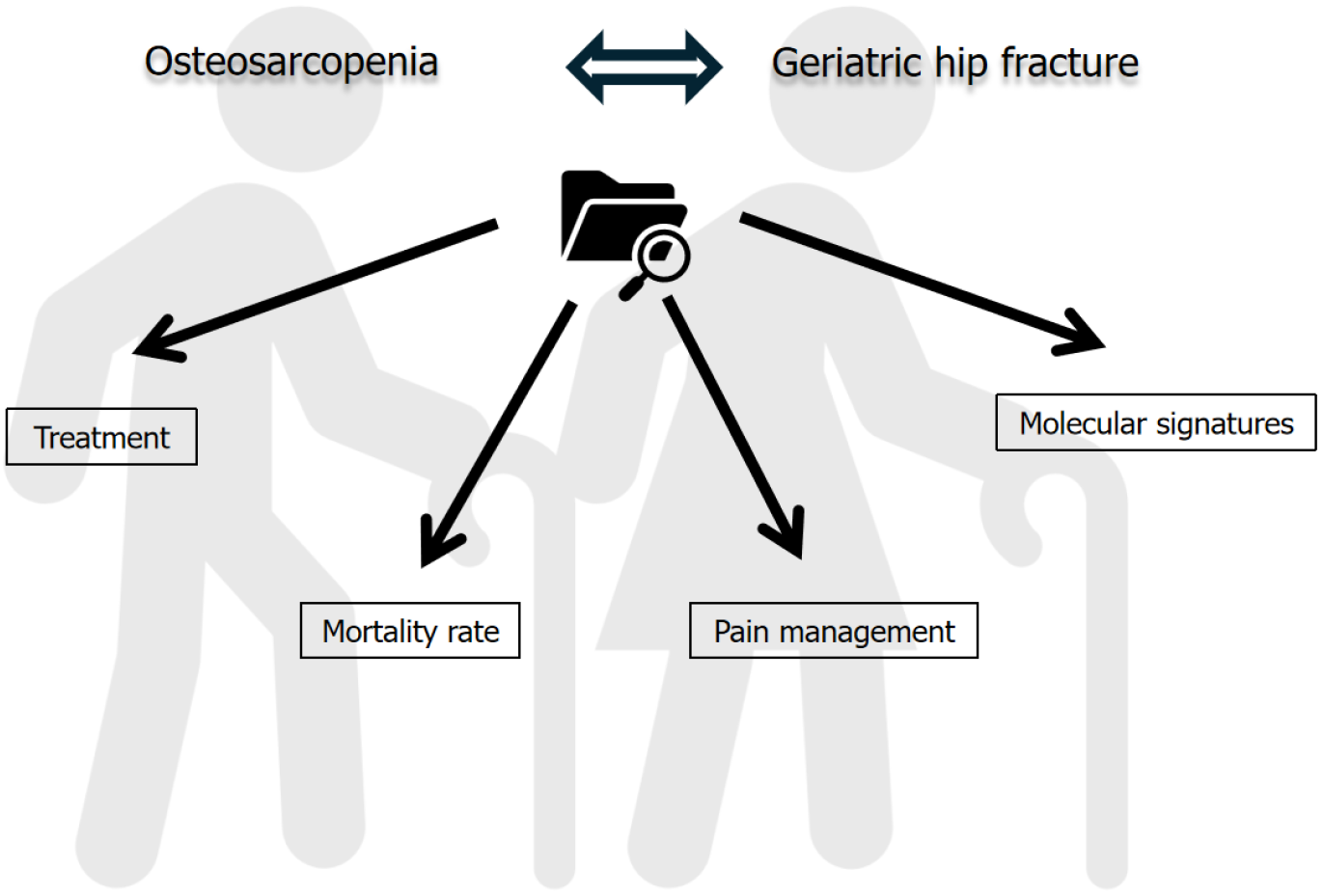
Preserving a good status during aging greatly depends on the ability of different systems of the human body to maintain their functionality. The musculoskeletal system is of paramount significance in healthy aging, not only because it facilitates ambulation but also through its role as a metabolic storage. Aging results in loss of bone mass and alteration of bone architectural structure and biomechanics, resulting in osteoporosis. As defined by the World Health Organization, osteoporosis is present when bone mineral density (BMD) is 2.5 SD or more below the average value for young healthy women (a T-score of < -2.5 SD)[1] . At the same time, the muscles lose their mass, power and strength and lead to sarcopenia. According to European Working Group on Sarcopenia in Older People, sarcopenia is defined by low levels of measures for three parameters: Muscle strength; muscle quantity/quality and physical performance as an indicator of severity[2]. Pathophysiology of sarcopenia involves several processes, such as increased inflammation, changes in neuromuscular junctions, hormonal changes and mitochondrial dysfunction[3]. These mechanisms combined with low muscle activity and poor nutrition (low in proteins) may lead to appearance of sarcopenia symptoms such as muscle size decrease, difficulty in performing daily activities, poor balance and falls[3]. The coexistence of these two conditions is described as osteosarcopenia[4]. This disorder has been correlated with a high incidence of fragility fractures, especially at the hip joint area, as well as with high rates of morbidity and mortality[4]. Although the condition may be also apparent in young population[5], it is mainly considered a geriatric syndrome. The condition is predicted to grow over the following decades considering the aging of population and the increased comorbidities of the elderlies. Fat infiltration of the musculoskeletal system, increased body mass index (BMI), and immunosuppression during aging are some of the main causes that could potentially contribute to increased incidence of osteosarcopenia among the older people. Numerous pathophysiological mechanisms involving DNA polymorphisms, alterations in endocrine system, and impaired paracrine signaling between fat - bone and muscle tissues have been correlated with the development of osteosarcopenia[4,6]. The current minireview focuses on the challenges of osteosarcopenia and hip fracture in elderly and aims to underscore the necessity of further research in the field of osteosarcopenia pathogenesis and management (Figure 1).
Figure 1
Current challenges on osteosarcopenia and hip fracture in elderly.
OSTEOSARCOPENIA: HIP FRACTURE, PREVALENCE, MORTALITY AND TREATMENT
In recent years, several studies have evaluated the incidence of osteosarcopenia during aging. At the same time, it has become evident that compared to healthy individuals the coexistence of osteoporosis and sarcopenia constitute a major risk factor for falls, fractures and increased mortality rates. According to a large systematic review and meta-analysis from Nielsen et al[7] that included 17 studies conducted until 2018, the frequency of osteosarcopenia was estimated to be between (5%-37%), while the relative risk of fracture (sarcopenic vs non-sarcopenic patients) was calculated at 1.37 (95%CI: 1.18-1.59; P < 0.001). In another case-controlled study of 134 subjects (age 65-80, 76 in hip fracture group, 58 in control group) the authors evaluated the relationship between BMD, gluteus maximus muscle volume (via computed tomography imaging) and hip fracture type and they revealed a greater risk of hip fracture in osteosarcopenic patients[8]. Additionally, Yoo et al[9] in a retrospective observational study of 324 patients with a hip fracture (246 women, 78 men, all above 60 years) identified a prevalence of osteosarcopenia of 28.7% (93/324). Osteosarcopenic patients had greater one-year mortality rate (15.1%, 14/93), compared to normal, sarcopenic or osteoporotic patient groups. Therefore, they advocated that the coexistence of osteosarcopenia and hip fracture predisposed to higher mortality risk. In alignment with the aforementioned studies, a pooled analysis of eight cohort studies and 19,836 participants performed by Teng et al[10] showed that the presence of osteosarcopenia increased the risk of fractures (OR = 2.46, 95%CI). Moreover, pooled analysis of three cohort studies indicated increased risk of falls (3144 participants, OR = 1.62, 95%CI) and increased mortality risk (2601 participants, OR = 1.66, 95%CI)[10].
In the most recent longitudinal study focusing on osteosarcopenia, Paulin et al[11] conducted a 10-year follow up study recruiting 1044 community-dwelling older women (all aged 75 years at baseline). The females were categorized into three groups: Normal, low bone mass and osteosarcopenia (confirmed or probable). The scholars concluded that the incidence of osteosarcopenia increased proportionally with age over the 10-year period (from 3.0% at 75 years to 9.2% at 85 years of age). In the group of probable osteosarcopenia (knee muscle strength < 175 Nms and femoral neck BMD T-score < -1.0) the prevalence was two to four times higher. Probable osteosarcopenia was associated with a greater risk of hip or major osteoporotic fracture and overall mortality compared with the condition of low bone mass alone. Furthermore, the median time-to-hip fracture was 7.6 years in the normal group, 6.0 years in the low bone mass group, and 5.7 years in the osteosarcopenia group. Even more recently, Veronese et al[12] conducted a systematic review with meta-analysis of nine cohort studies containing 14429 participants (mean age 70 years, 64.5% females). The authors identified a weighted prevalence of osteosarcopenia of 12.72% (95%CI: 9.650-15.78) in the studies included (1147 over 14429 participants). The presence of osteosarcopenia significantly increased the risk of mortality by 53% (RR = 1.53; 95%CI: 1.28-1.78). After accounting for publication bias, the re-calculated RR was 1.48 (95%CI: 1.23-1.72).
The above findings on osteosarcopenia frequency and fracture risk are similar to the results of previously published studies but with slightly higher risk estimates[13-15]. It is important to point out that the two longitudinal studies among Australian older men from Balogun et al[14] and Scott et al[15] showed an increased risk of falls, fractures and mortality in the presence of osteosarcopenia, but only when compared to healthy individuals. However, this effect was absent when osteosarcopenia was compared to osteoporosis or sarcopenia alone. The heterogeneity of the results between the studies may derive from various factors. The inconsistent use of definitions and criteria for diagnosis of sarcopenia or osteoporosis, the conduction of studies including mixed populations (both male and female subjects), and the difference in the age of participants could lead to different conclusions. Paulin et al[11] commented that the participation of elderly women of the same age at baseline would yield a more reliable assessment of data providing a perspective on “chronological” and “biological” trajectory of change in musculoskeletal aging.
The aforementioned inconsistencies impede valid comparisons and interpretation of the results, while there is no current treatment consensus for patients with osteosarcopenia. Several drugs have gained approval for the treatment of osteoporosis, however, no therapy with substantially beneficial effects has been approved to treat sarcopenia. To this point, few studies have examined any therapeutic strategies in sarcopenic patients with hip fractures[16,17]. A small randomized multicenter trial from Flodin et al[16] evaluated the combined effects of bisphosphonate and protein-rich nutritional supplementation in 79 hip-fractured sarcopenic patients who followed conventional rehabilitation protocols. Patients were divided into three groups, a protein and bisphosphonate group, a bisphosphonate-only group and a control group. After 12 months, there were no differences among the groups regarding changes in fat-free mass index, handgrip strength and health-related quality of life. Another small multi-centre randomized trial assessed the effectiveness of β-hydroxy-β-methylbutyrate (HMB) combined with standard diet on muscle mass and nutritional markers in 107 hip-fractured patients over 65 years[17]. Sarcopenia prevalence was 72% among entire population. Significant improvement in BMI, muscle mass, appendicular lean mass, vitamin D and calcium levels was observed in the group receiving standard diet plus HMB (55/107 patients) compared to the only standard diet group (52/ 107 patients).
Denosumab, a monoclonal antibody targeting receptor activator of the NF-kB ligand (RANKL), has been proven to reduce fracture risk, and now is widely used to treat osteoporosis[18]. Given the unexplored therapeutic strategies for osteosarcopenia, Pizzonia et al[19] aimed to prospectively compare the long-term effectiveness of bisphosphonate (alendronate) vs denosumab, on bone and muscle, in a cohort of 98 elderly patients suffering from hip fractures. The results showed positive effects of both drugs on skeletal muscle mass and function in elderly patients with hip fractures, but no significant differences between the treatment groups. Another recent study assessed whether denosumab had a dual effect on bones and muscles compared to bisphosphonates treatment in osteoporotic patients[20]. The authors found significant decrease in falls risk (P = 0.001) and improvements in all sarcopenia measures (P = 0.01) in the 5-year denosumab therapy group (n = 135), compared to the 3-year bisphosphonate therapy group (n = 272). Importantly, one year upon denosumab discontinuation, significant worsening of both falls risk and sarcopenia measures (P = 0.01) was observed. This finding highlighted a potential benefit of denosumab in the treatment of osteosarcopenia.
MOLECULAR INSIGHTS INTO OSTEOSARCOPENIA AND HIP FRACTURE
The prevalence of osteosarcopenia in elderly population along with the potential health risks and the absence of specific treatment strategies, underline the necessity for understanding the underlying pathology of the condition and clarify the role of interplay between osteoporosis and sarcopenia through genetic and molecular mechanisms and approaches. Kang et al[21] performed an RNA sequencing profile study in elderly female patients with osteoporotic hip fracture in the presence or absence of sarcopenia. The study included 324 female patients over 65 years of age who had undergone hip fracture surgery. After the implementation of several exclusion criteria, RNA sequencing was performed on muscle tissue (gluteus maximus) from 5 non-sarcopenic and 6 sarcopenic patients. The authors identified 15 genes related to exosome, enzyme and autophagy functions, which were differentially expressed between sarcopenic and non-sarcopenic osteoporotic hip fracture patients. One serious limitation of this study was the small sample number, although demographic factors such as age and sex were matched between the study groups. A recent study from Chen et al[22], integrated both transcriptomics and proteomics to deepen understanding of the molecular association of osteoporosis with sarcopenia. The study included 6 female patients awaiting hip replacement surgery (3 with osteosarcopenia, 3 with osteoporosis - control group). The received samples were categorized into four groups: Bone tissue from patients with osteosarcopenia, bone tissue from osteoporotic only patients, muscle tissue from patients with osteosarcopenia and muscle tissue from patients with only osteoporosis. The analysis of pathways and gene expression revealed that the differentially expressed genes and proteins between the four groups played a role in oxidative-reduction balance, cellular metabolism, immune response, osteoclast differentiation and NF-kappa B signaling pathways, all of which could serve as potential therapeutic targets. Although these studies have offered important insights into the pathophysiology of osteosarcopenia and hip fracture, it is evident that additional studies with larger sample size are needed to shed more light on the molecular basis of osteosarcopenia.
MUSCLE-BONE “ENDOCRINE AND PAIN” CROSSTALK
In the last two decades, a significant number of studies have revealed that bone and skeletal muscle can function as endocrine organs. It seems that they are able to closely communicate via osteokines and myokines, thus providing new prospects to uncover the mechanisms of osteosarcopenia development[23]. In addition, it is known that this “muscle-bone crosstalk” is critical for fracture healing[24]. A recent review focused on several well-defined myokines and osteokines that could be involved in osteosarcopenia-related fracture process[25]. The authors revealed that the myokines myostatin and irisin and the osteokines RANKL and SOST not only regulated the skeletal muscle and bone metabolism, but also accelerated the fracture healing process, making those molecules interesting therapeutic targets.
The relationship between osteosarcopenia and pain has also been investigated. According to a systematic review and meta-analysis from Lin et al[26], there was a strong positive correlation between sarcopenia and pain as the prevalence of sarcopenia alone was very high in pain patients. Recently, a first-to-its-kind narrative review was published to consolidate the existing knowledge on the molecular processes involved in the onset and persistence of pain in patients with osteoporosis and sarcopenia and to define any potential therapeutic (pharmacological or non-pharmacological) strategies for pain management in elderly sarcopenic patients. Bonanni et al[27], studied 120 articles related to pain development in patients with osteosarcopenia and concluded that in elderly individuals the presence of the typical constant chronic inflammation could promote nociceptive stimulation to musculoskeletal system and pain sensitization. The molecular basis of this effect relies on the release of prostaglandin (PGE2), interleukin-6 and histamine by immune cells which ultimately result in the gating of ion channels and propagation of the nociceptive signal. These insights are quite important since there is a profound demand for development of strategies for treating musculoskeletal pain, especially in osteosarcopenia patients with hip fractures, as specific therapies are largely missing nowadays.