INTRODUCTION
Fractures of the hip joint are most dreaded among the fragility fractures, which are associated with osteoporosis[1]. They are still a significant concern, especially in the elderly population, due to the morbidity and mortality that are prevalent with hip fractures[2-5]. These injuries not only affect individual patients’ lives but also place a significant and ever-growing economic burden on the healthcare systems and societies at large. As global demographics shift towards an ageing population[6], the severity of the problem becomes increasingly relevant and urgent[7,8].
Worldwide incidence of osteoporotic hip fractures in 1990 and 2000 was estimated to be approximately 1.3 million[9] and 1.6 million in people aged above 50 years[2]. Gullberg et al[9] estimated the projections of worldwide incidence of hip fractures with an assumption of no change in sex and age-specific incidence, to double by 2025 to 2.6 million and reach around 5 million annually by 2050. This number can vary anywhere between 5 to 21 million by 2050. Particularly, the burden of these fractures is prominent in Asia, which accounted to be 26% in 1990, and projections indicate this will probably rise to 37% by 2025 and may even reach 45% by 2050. As the global population continues to age[6], healthcare systems will face significant challenges, with the associated financial burden of hip fractures expected to double by 2050 compared to 2018 levels.
The burden on the healthcare systems is even more when treatment outcomes and fixation failures, which range from 5% to 41%, even in the best of circumstances[10]. In pertrochanteric fractures, fixation failure is described up to 5%, but when one considers displaced and undisplaced neck of femur fractures, the failure rates skyrocket to 15% and 41%, respectively. The impact of these injuries on the function of the individuals involved is severe, with only 30%-40% of the patients regaining their pre-fracture mobility[3,4,11]. Cumulative mortality rates at 1 year following such injuries range between 20% and 40%, with men experiencing a higher risk of death than women[3,4,12-14]. Beyond immediate mortality, a hip fracture significantly increases the long-term risk of death, with mortality rates remaining elevated for a decade compared to the general population.
The postoperative recovery phase plays a crucial role in shaping a patient’s long-term survival and ability to regain independence. During this critical period, complications such as delirium, anaemia, and pressure ulcers frequently arise, contributing to higher mortality rates within the first year. Additionally, delayed mobilisation post-surgery remains a key challenge, often leading to poor functional outcomes after discharge and an elevated risk of mortality within six months. Tackling these issues requires a comprehensive approach that combines preventive strategies, optimised rehabilitation protocols, and proactive medical interventions to minimise complications and enhance recovery. By prioritising early mobilisation, tailored perioperative care, and multidisciplinary support, healthcare providers can significantly improve outcomes and reduce the burden of fragility fractures on elderly patients.
PROPHYLACTIC FIXATION RATIONALE
Prophylactic fixation (ProFix) of the proximal femur in elderly individuals with osteoporosis presents a proactive approach to reducing the likelihood of severe fractures and their associated complications[1,15,16]. By reinforcing skeletal stability in high-risk individuals, ProFix has the potential to significantly lower fracture incidence, particularly in cases of low-energy falls, which are a leading cause of fragility fractures[15].
Beyond its direct clinical benefits, this strategy may also prove cost-effective, improving long-term outcomes by minimising hospital stays, expediting recovery, and preserving mobility. As osteoporosis often remains undiagnosed until a fracture occurs, early identification and targeted interventions such as ProFix could be instrumental in preventing avoidable fractures and improving overall quality of life in ageing populations[16-18]. By preventing the fractures, the associated complications associated with prolonged immobilisation, loss of independence and reduced life expectancy can be avoided[3,4,10,12,19-23]. It is also expected to shorten hospital stays, facilitate faster postoperative recovery, and better mobility, allowing patients to maintain a higher quality of life.
Considering the high prevalence of undiagnosed osteoporosis, particularly in elderly individuals, identifying those at risk is critical[2,24]. For individuals aged over 60 years who are at high risk of fractures, ProFix can prove to be a cost-effective intervention[15]. Early diagnosis and timely intervention can significantly reduce the incidence of fractures and improve outcomes for this vulnerable population[25-31]. By preventing the need for emergency surgery and reducing hospital readmissions, healthcare systems can save resources while delivering better care. Advances in surgical technology now enable minimally invasive targeted procedures under low-risk anaesthesia that preserve mobility, reduce surgical risks and promote quick recovery, further supporting the case for ProFix.
MILESTONE ESSENTIALS FOR PROFIX
The concept of ProFix demonstrates considerable potential in improving outcomes for elderly patients with osteoporosis. Developing effective screening tools is essential for identifying high-risk individuals. Advances in imaging techniques, such as computed tomography (CT) scans combined with clinical parameters, have significantly improved the prediction of bone mineral density (BMD) and fracture risk. Convolutional neural networks applied to quantitative CT images have demonstrated remarkable accuracy, with substantial clinical implications[32-34].
While the fracture risk assessment tool remains a widely utilised method for evaluating osteoporosis-related fracture risk, its predictive accuracy has certain limitations, particularly in identifying individuals most likely to experience fractures. To address these gaps, emerging technologies are refining risk assessment through machine learning and artificial intelligence (AI)-driven models, improving the precision of fracture prediction and enabling earlier preventive interventions[35,36]. Advanced AI-powered tools like OsteoDetect have demonstrated enhanced capabilities in detecting fractures by analysing X-ray and CT imaging, offering more reliable and automated screening processes. By integrating patient-specific data, imaging analytics, and AI-assisted diagnostics, these innovations are paving the way for more personalised and proactive orthopaedic care, allowing clinicians to intervene at optimal moments to prevent debilitating fractures in high-risk individuals[37]. These tools, when integrated with patient-specific data, can enhance diagnostic accuracy and reduce the likelihood of missed diagnosis, especially when used along with human aid[38-40]. Machine learning techniques, which incorporate factors such as genetic markers, gait stability from wearable sensors, and biomechanical modelling, offer a more personalised approach to risk stratification[35,36]. Advanced AI-driven systems are now revolutionising osteoporosis screening by combining multiple diagnostic elements, including radiographic imaging, patient history, and molecular biomarkers. By integrating these diverse data sources, AI enhances fracture risk prediction, allowing for earlier and more targeted interventions. This approach helps clinicians identify high-risk individuals more accurately, enabling timely preventive strategies such as pharmacologic treatments or ProFix. As these technologies continue to evolve, they offer a promising shift toward personalised orthopaedic care, improving long-term outcomes and reducing the burden of fragility fractures in ageing populations. These innovations not only refine diagnostics but also inform surgical decision-making, optimising the timing and method of ProFix. AI-assisted planning tools allow for individualised implant selection based on trabecular strength, improving structural integrity while minimising surgical risks[38-40]. As these technologies continue to evolve, predictive analytics is set to transform fracture prevention, bridging the gap between risk assessment and proactive orthopaedic interventions.
FEASIBILITY OF PROFIX
Several advancements in diagnostic tools and treatment modalities support the feasibility and effectiveness of ProFix for high-risk patients. Measuring BMD using dual-energy absorptiometry (DXA) remains the gold standard for diagnosing osteoporosis and assessing the fracture risk[35,41,42]. However, DXA’s sensitivity is limited in distinguishing fracture-prone individuals from those who are not. Trabecular bone scans can evaluate bone microarchitecture, independent of BMD and DXA, with 3d modeling can provide additional structural insights[43-45]. Newer algorithms using machine learning are being developed that can predict and stratify patients using digital X-rays, which are commonly available[35,46].
Using advanced guided navigation techniques can help to limit the surgical insult to the bare minimum, so much so that prophylactic surgeries can be done with local anaesthesia with monitored anaesthesia care[47,48]. The advancements in virtual reality (VR) technology in the operating room can simplify implant positioning and reduce timing to a greater extent[49-51]. AI and machine learning have shown promise in the screening, detection, and prediction of fractures[36,52]. These tools can not only enable us to identify high-risk patients more effectively but also personalise treatment strategies, including the type of implants and their sizing based on individual risk profiles[53,54].
CHALLENGES IN PROFIX
Despite its potential, the implementation of ProFix presents several clinical, ethical and economic challenges that must be addressed to facilitate broader adoption[16]. It is cost-effective only in carefully selected high-risk individuals, underscoring the need for judicious patient selection to justify the associated resource utilisation[15]. While ProFix is designed to strengthen bone integrity and reduce the likelihood of fractures, careful consideration must be given to minimising surgical risks and potential complications. One of the primary concerns is the long-term stability of implants, especially given the fragile nature of osteoporotic bone. Factors such as implant design, bone remodelling, and load distribution play crucial roles in ensuring durability while maintaining functional support. Optimising surgical techniques and tailoring implant selection to individual patient profiles can help mitigate risks, improving both short-term recovery and long-term outcomes. A balanced approach that incorporates advanced biomaterials, precision surgical methods, and postoperative monitoring will be essential in maximising the benefits of ProFix while ensuring patient safety and efficacy[10]. The effectiveness of ProFix depends on several patient-specific variables, including BMD, existing comorbidities, and the surgical techniques used. Since osteoporosis weakens bone structure, ensuring implant stability while maintaining natural healing potential is critical. Ideally, fixation constructs must provide sufficient mechanical support to reduce fracture risk while allowing the bone to undergo its natural remodelling process if a fracture occurs post-fixation. Balancing implant stiffness is essential—while a rigid structure can prevent immediate collapse, excessive stiffness may hinder adaptive bone healing over time. A patient-tailored approach, incorporating optimised surgical techniques and biomaterial selection, can enhance fixation outcomes, ensuring long-term durability while preserving bone integrity[16].
The adoption of ProFix in osteoporotic individuals brings forth several ethical considerations that require careful evaluation. One of the most fundamental concerns is patient autonomy and informed consent, as this intervention involves a surgical procedure for a condition that has not yet developed. Patients must be fully informed about the potential risks, benefits, and long-term implications to ensure their ability to make a well-informed decision regarding their treatment. Transparency in discussions between physicians and patients is crucial to maintaining ethical standards and respecting individual choice.
Another key issue is appropriate patient selection, as the procedure must be both clinically justified and cost-effective for high-risk individuals while avoiding unnecessary surgical interventions in those with lower fracture risk. Overdiagnosis and overtreatment could lead to complications such as implant-related failures, perioperative morbidity, and long-term musculoskeletal consequences. Establishing stringent evidence-based risk stratification protocols can help determine which patients would benefit most from ProFix, ensuring ethical and efficient resource utilisation.
Additionally, healthcare accessibility and equity remain pressing challenges, as sophisticated screening tools and AI-assisted predictive models may not be readily available in all clinical settings—particularly in underserved regions. This raises concerns about health disparities, where individuals at high risk for fragility fractures may lack access to preventive interventions like ProFix, increasing their vulnerability. Addressing this issue requires strategic policymaking and collaboration among healthcare providers, researchers, and policymakers to ensure equitable access to advanced preventive orthopaedic care across different healthcare systems.
Finally, the ethical balance between innovation and clinical validation must be considered. While AI-assisted fracture prediction and minimally invasive surgical techniques present exciting advancements, their long-term efficacy and safety must be thoroughly tested through rigorous clinical trials before widespread implementation. Ethical frameworks should guide these decisions, ensuring that new technologies are backed by robust scientific evidence, prioritising patient safety while optimising clinical benefits. Further challenges include delayed surgical intervention, managing complications in frail individuals, and the complexity of postoperative pain control in elderly patients. Overcoming these hurdles demands a multidisciplinary approach, integrating evidence-based surgical techniques, perioperative care, and rehabilitation strategies to maximise outcomes while adhering to ethical and medical standards.
IMPLEMENTATION PLAN
AI-powered models are transforming fracture risk assessment by analysing extensive datasets, including DXA scans, patient history, and genetic markers, to provide more precise predictions than conventional methods[55-58]. Deep learning algorithms are now being used in imaging analysis to detect early structural changes in bone, allowing for proactive interventions before fractures occur[59]. Additionally, wearable technology and motion sensors are emerging as valuable tools for assessing gait stability and fall risk—key factors in preventing fractures among elderly individuals[60-63]. Another important consideration is sarcopenia, the age-related loss of muscle mass, which significantly increases fracture susceptibility. Early identification of sarcopenia using DXA-derived appendicular lean mass index and bioelectrical impedance analysis enables targeted strategies to preserve musculoskeletal health and reduce fracture risk. By integrating these AI-driven approaches with clinical expertise, healthcare providers can develop personalised prevention protocols, improving overall patient outcomes in osteoporosis management[64]. Hence, an effective implementation framework for ProFix in osteoporotic individuals requires a structured, multi-phase approach that integrates risk assessment, surgical advancements, and healthcare system optimisation. The first crucial step involves developing robust screening protocols, leveraging AI-driven predictive analytics and machine learning models to accurately stratify fracture risk. Incorporating tools like quantitative CT imaging, trabecular bone analysis, and motion sensors will enhance early identification of high-risk patients, ensuring timely intervention.
Refining surgical techniques is key to minimising procedural risks and ensuring optimal patient outcomes in ProFix. Advancements in minimally invasive fixation methods, AI-assisted navigation, and robotic surgical systems have enabled more precise implant placement, reducing anaesthesia requirements and recovery time. Personalised implant selection, guided by AI-driven predictions of trabecular bone strength, further enhances long-term fixation stability. In geriatric patients with a high risk of femoral neck fractures, triangulated cancellous screws can be placed more efficiently than in patients who have already sustained fractures, as the procedure requires less anaesthesia, allows easier positioning, and benefits from VR and AI-based navigation tools[65,66]. Recent studies highlight the effectiveness of antegrade femoral nails with proximal and distal interlocking screws, demonstrating superior stabilisation of the proximal femur in high-risk osteoporotic patients. The use of minimally invasive techniques further improves feasibility, offering shorter recovery times and better functional outcomes.
Successful implementation of ProFix requires healthcare systems to invest in early screening protocols and validated risk assessment tools to identify high-risk individuals before fractures occur. Training surgeons in advanced techniques and AI-driven planning tools will be essential for ensuring consistent and effective application of ProFix. By combining cutting-edge diagnostic technologies with conventional risk stratification models, clinicians can identify the most suitable patients for ProFix and deliver personalised interventions, whether through pharmacological treatments, lifestyle modifications, or surgical approaches.
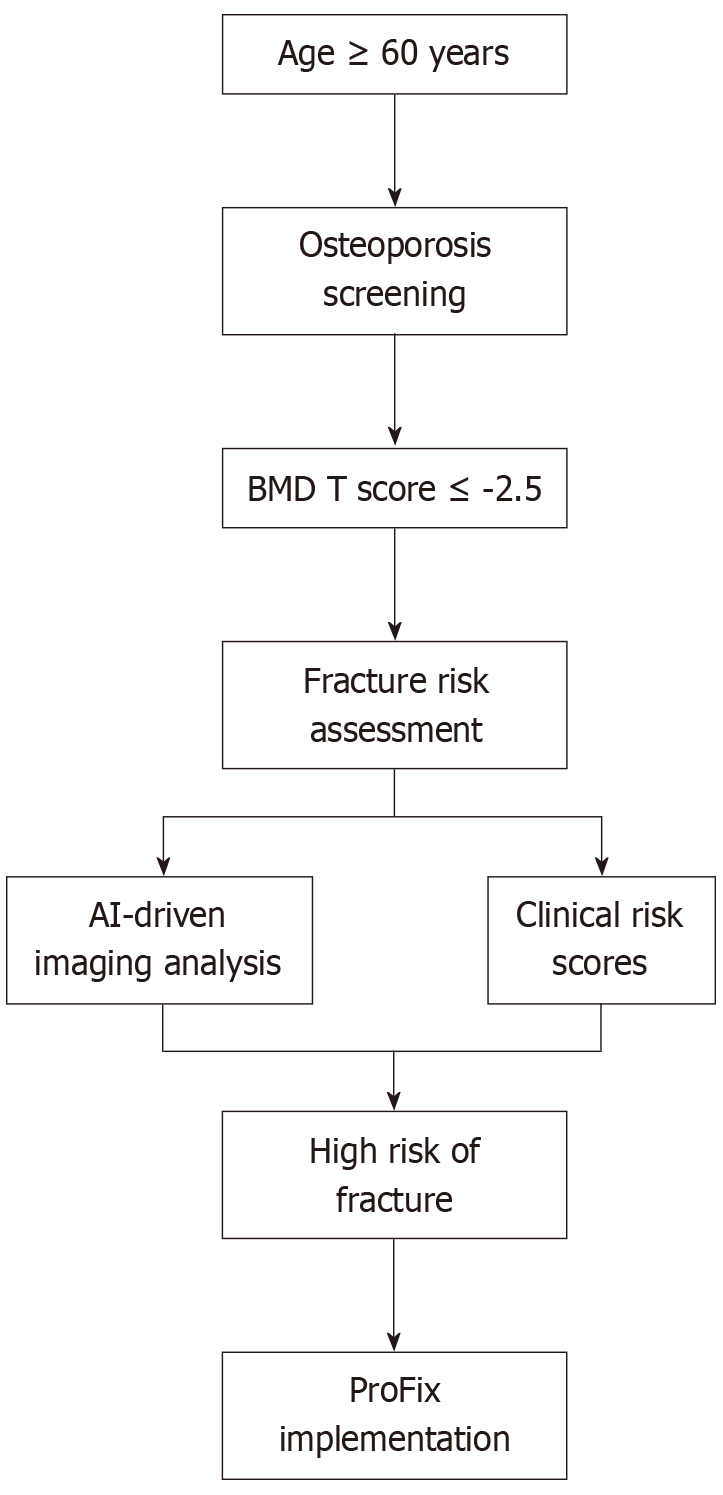
Lastly, continuous clinical monitoring plays a crucial role in validating the long-term effectiveness of ProFix. Wearable technology for gait and mobility assessment, coupled with AI-assisted postoperative analysis, provides real-time insights into recovery progress, enabling personalised adjustments to rehabilitation strategies. By integrating predictive analytics, surgical precision, and data-driven postoperative care, ProFix can become a transformative approach in orthopaedic management, helping to reduce fracture-related morbidity and improve the quality of life for elderly patients. The implementation pathway is depicted in Figure 1.
Figure 1 Prophylactic fixation implementation pathway.
ProFix: Prophylactic fixation; BMD: Bone mineral density; AI: artificial intelligence.
The feasibility of widespread implementation of ProFix is closely tied to national healthcare reimbursement models, which vary significantly across regions. Countries with government-funded healthcare systems may find preventive orthopaedic interventions like ProFix appealing due to their potential to reduce long-term healthcare costs associated with fragility fractures. Conversely, in systems reliant on private insurance, reimbursement eligibility for prophylactic procedures may be limited, thereby potentially limiting their widespread adoption. To address this, structured policies supporting early osteoporosis screening and preventive interventions could incentivise ProFix adoption. Integrating AI-driven fracture risk assessment tools into routine clinical practice, combined with reimbursement structures that prioritise prevention, may enhance accessibility while improving patient outcomes and cost efficiency across diverse healthcare settings.
ADVANTAGES OF PROFIX
ProFix presents a promising strategy for managing osteoporosis-related fractures by reinforcing skeletal stability and reducing the likelihood of recurrent fractures, which are linked to increased mortality in elderly individuals. By strengthening the proximal femur, ProFix provides structural support, complementing existing pharmacological treatments and addressing the shortcomings of external protective devices. This approach ensures immediate stabilisation, helping patients retain mobility and independence[65]. Additionally, by lowering the need for emergency surgeries, extended hospital stays, and intensive post-hospital care, ProFix contributes to cost-effective management of osteoporosis-related fractures, particularly for high-risk patients[15,29]. Early mobilisation following ProFix plays a key role in preventing secondary complications, such as pressure sores, thromboembolism, and cardiopulmonary issues, thereby enhancing recovery outcomes and overall quality of life.
While ProFix offers a proactive surgical approach to reducing fragility fractures, it is essential to contextualise its benefits alongside existing preventive strategies. Pharmacological therapy, including bisphosphonates, selective estrogen receptor modulators, and monoclonal antibodies, remains a cornerstone of osteoporosis management, aiming to enhance BMD and reduce fracture risk. However, medication adherence, potential side effects, and variability in individual response can limit its effectiveness. Serum biomarker monitoring is another emerging preventive strategy, utilising biochemical indicators such as bone turnover markers and calcium metabolism profiles to assess fracture risk dynamically. While this approach allows for personalised intervention, it lacks immediate structural reinforcement, making it more suited for monitoring rather than direct prevention. Compared to these strategies, ProFix offers immediate skeletal reinforcement, significantly reducing the likelihood of catastrophic fractures from low-energy falls. Furthermore, technological advancements in AI-driven risk prediction, minimally invasive surgical techniques, and optimised implant designs enhance the feasibility and cost-effectiveness of ProFix. Ideally, a combined approach integrating pharmacological treatment, biomarker monitoring, and selective ProFix application based on risk stratification could yield the most comprehensive preventive framework.
FUTURE DIRECTION
The future of ProFix hinges on ongoing innovation and the seamless integration of advanced technologies into clinical practice. AI-driven algorithms designed specifically for fracture detection and risk assessment are enhancing predictive accuracy, allowing for precise identification of high-risk individuals and enabling more personalised treatment approaches. As orthopaedic advancements continue, novel implant designs, customised surgical instrumentation, navigated jigs, and robotic-assisted techniques are revolutionising fixation procedures. These innovations not only improve surgical efficiency and precision but also pave the way for minimally invasive interventions with reduced anaesthesia requirements, postoperative pain, and radiation exposure.
Beyond surgical advancements, comprehensive orthopaedic care for osteoporotic patients relies on timely interventions, optimised pain management, and adherence to key lifestyle modifications. Maintaining adequate calcium intake and engaging in weight-bearing physical activity remain fundamental in preserving bone health and preventing future fractures. A multifaceted approach that combines predictive analytics, minimally invasive surgical techniques, and proactive patient management will be crucial in ensuring better clinical outcomes.
To ensure robust validation of ProFix in future clinical studies, clearly defined inclusion and exclusion criteria are necessary. Inclusion criteria should focus on individuals aged ≥ 60 years with a high risk of fragility fractures, as determined by BMD < -2.5 SD, trabecular bone deterioration on imaging, or a history of osteoporotic fractures. Patients with impaired gait stability, identified through wearable sensor analysis, may also be considered. Exclusion criteria should include patients with severe comorbidities affecting surgical candidacy, those with advanced osteoarthritis requiring joint replacement, and individuals with contraindications to surgical interventions. Further, a structured follow-up plan is critical for tracking recovery progress. A timeline consisting of 1-month, 3-month, 6-month, and 1-year intervals will facilitate monitoring of functional mobility, healing progression, and complication rates. Imaging assessments (e.g., DXA scans, radiographs) at 6 months and 1 year can provide insights into bone remodelling and implant stability. In addition, to ensure a comprehensive evaluation, key metrics such as fracture incidence (monitoring the occurrence of new fractures post-ProFix), functional mobility scores (e.g., Timed Up and Go test, gait stability tracking), quality-of-life indices (validated tools such as the 36-Item Short Form Health Survey, EuroQoL-5-dimension), implant-related complications (revision surgery rates, fixation failure), and hospital stay duration and healthcare costs (for comparative feasibility assessments) should be included in the analysis. By integrating these standardised selection criteria, structured follow-up intervals, and validated outcome measures, future studies can ensure methodological consistency, enabling reproducibility across clinical trials and real-world applications.
CONCLUSION
ProFix represents a transformative strategy for reducing fracture-related morbidity and improving long-term outcomes in osteoporotic patients at high risk for neck of femur fractures. By incorporating predictive analytics, AI-assisted screening, and precision-driven surgical techniques, this approach holds significant promise for early intervention and reduced healthcare burden. However, successful implementation requires careful patient selection, guided by validated risk assessment models to prevent unnecessary surgical procedures. Ethical considerations—such as patient autonomy, equitable healthcare access, and implant durability—must remain central to its adoption. As technology continues to refine predictive models and surgical precision, a multidisciplinary framework integrating clinical evidence, AI-driven diagnostics, and proactive prevention strategies will be essential in optimising orthopaedic care for high-risk patients. Future research and clinical trials must establish the efficacy and cost-effectiveness of ProFix, ensuring that this approach strikes a balance between innovation, feasibility, and ethical responsibility in orthopaedic care.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country of origin: India
Peer-review report’s classification
Scientific Quality: Grade C, Grade C
Novelty: Grade C, Grade C
Creativity or Innovation: Grade C, Grade C
Scientific Significance: Grade C, Grade C
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
P-Reviewer: Fu XP, PhD, Researcher, China; Lu SR, MD, Adjunct Professor, Director, China S-Editor: Liu H L-Editor: A P-Editor: Zhao YQ