Published online May 18, 2024. doi: 10.5312/wjo.v15.i5.469
Revised: February 23, 2024
Accepted: April 12, 2024
Published online: May 18, 2024
Processing time: 125 Days and 2.5 Hours
Intertrochanteric fracture of the femur occurs mostly among older people, and seriously affects daily life and quality of life. At present, physical intervention, drug treatment, routine intervention and rehabilitation training are widely used for prevention of side effects, but it is still inconclusive which intervention has the best effect.
To compare the effects of new intervention measures for preventing side effects of artificial joint replacement.
We searched the Chinese and English literatures for comparative studies on the prevention of side effects of new interventions for artificial joint replacement from July 2013 to June 2023 in China HowNet, PubMed, Wanfang, Weipu and other databases. Study quality was evaluated by improved Jadad scoring standard, and the effects of different interventions on preventing different complications were analyzed by meta-analysis of evidence-based medicine with Review Manager 5.0 software.
Ten articles, including 869 cases, were finally included. The preventive effects of different interventions on the side effects of artificial joint replacement were studied, and valid data were extracted. There were two articles on the preventive effects of drug intervention, four on comparison of the preventive effects of combined and single interventions, and three on the preventive effects of physical intervention, rehabilitation training and routine intervention. Meta-analysis showed that the preventive effect of rivaroxaban was significantly better than low molecular weight heparin calcium [mean difference (MD) = -0.16, 95%CI: -0.28 to -0.04, P < 0.05]. The effect of combined intervention was significantly better than that of single intervention (MD = -0.08, 95%CI: -0.16 to -0.01, P < 0.001). Physical intervention was significantly better than routine intervention and rehabilitation training (MD = 0.26, 95%CI: 0.16–0.36, P < 0.001).
Rivaroxaban combined with rehabilitation training is preferred for preventing deep vein thrombosis after artificial joint replacement. In the prevention of pulmonary embolism, rivaroxaban drug intervention is given priority. The effect of combined intervention is better than that of single intervention.
Core Tip: Physical intervention, drug therapy, routine intervention and rehabilitation training are widely used clinically to prevent side effects of artificial joint replacement, but it is still inconclusive which intervention method is best. This meta-analysis assessed new methods of intervention for prevention of side effects of artificial joint replacement for intertrochanteric fracture.
- Citation: Jiang W, Zhu TB. Meta-analysis of new intervention measures for preventing side effects of artificial joint replacement. World J Orthop 2024; 15(5): 469-476
- URL: https://www.wjgnet.com/2218-5836/full/v15/i5/469.htm
- DOI: https://dx.doi.org/10.5312/wjo.v15.i5.469
Intertrochanteric fracture of the femur occurs mostly among older people, and seriously affects patients’ daily life and quality of life. With the acceleration of aging in China and worldwide, prevalence of common diseases among older people has increased rapidly, including intertrochanteric fracture of the femur[1]. At present, there are many clinical treatments for this fracture type, but because most of the patients are older, their physical function declines, resulting in the treatment not achieving the best effect[2]. In recent years, traction therapy and surgical treatment have commonly been used. Traction therapy is less harmful to patients than surgical treatment but its effect is not ideal, and patients need to stay in bed for a long time, resulting in serious complications such as urinary tract infection, deep vein thrombosis and avascular necrosis of the femoral head[3]. Although artificial joint replacement can reduce mortality in patients with intertrochanteric fracture and deformation of the fracture site, according to recent clinical feedback, artificial joint repl
We searched China HowNet, PubMed and other databases for randomized controlled trials of new intervention measures to prevent side effects of artificial joint replacement, using Chinese keywords for artificial joint replacement, joint replacement, venous thrombosis, hip replacement, complications, intervention measures, side effects, etc., and English search terms artificial joint replacement, joint replacement, risky permeability, hip replacement, complications, intervention measures and side effects.
Inclusion criteria: (1) All patients underwent artificial joint replacement; (2) randomized controlled trials; (3) interventions such as rivaroxaban, rehabilitation training, low molecular weight heparin (LMWH) calcium, LMWH sodium, periodic inflation and compression, gradient elastic compression socks, arteriovenous foot pump, LMWH calcium and gradient elastic compression socks, LMWH calcium and periodic inflation and compression system, rehabilitation training and LMWH calcium, and rivaroxaban and rehabilitation training; (4) access to the full text; and (5) Chinese or English language. Exclusion criteria: (1) Nonrandomized controlled trials; (2) patients < 65 years old; (3) pathological fractures; (4) duplicate documents; and (5) studies with incorrect statistical methods.
Jadad Quality Rating Scale[6] was used to evaluate the quality of the literature, and the experimental methods were assessed, including the method of generating the random grouping sequence, double-blind method, and patient withdrawal and loss to follow-up. The total score of the three items was 5, of which < 2 was low-quality research and > 3 was high-quality research.
The following information was extracted: (1) General information: title, authors’ names, and publication year; (2) patient characteristics: Number of patients, ratio of male to female, average age, etc.; (3) intervention measures and duration: intervention methods, duration, and follow-up time; and (4) outcome indicators: venous thromboembolism, pulmonary embolism and deep venous thrombosis.
RevMan 5.0 was used to process and meta-analyze the data. Numerical data were expressed as odds ratio (OR) and 95% confidence interval (CI). P < 0.05 indicated that the was statistically significant. The χ2 test and P value were used to analyze heterogeneity among the studies, and I2 was used to test the heterogeneity among the studies. If I2 ≤ 50% and P ≥ 0.1 were satisfied at the same time, the heterogeneity was small, and the fixed-effect model was used for analysis. If I2 was > 50% or P < 0.1, the heterogeneity was large, so it was necessary to analyze the causes of heterogeneity. If heterogeneity still existed, a rando- effect model was used for analysis.
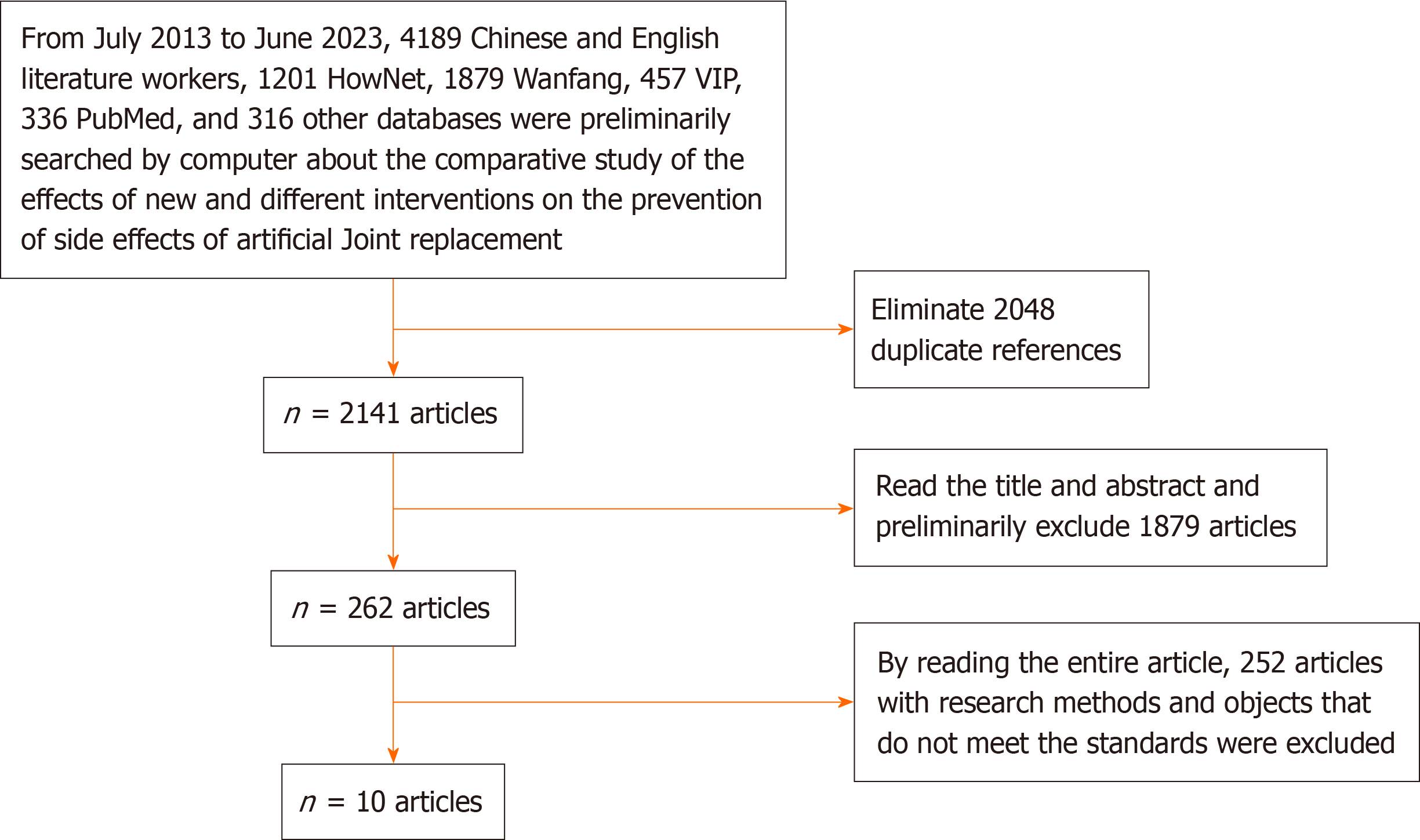
From July 2013 to June 2023, there were 4189 Chinese and English comparative studies on the effects of new intervention measures for preventing the side effects of artificial joint replacement: 1201 from HowNet, 1879 from Wanfang, 457 from VIP, 336 from Pubmed and 316 from other databases. We excluded 2048 duplicate articles, leaving 2141. By reading the titles and abstracts, 1879 articles were initially excluded, leaving 262. After reading the full text, 252 papers with substandard research methods and objectives were excluded, and the remaining 10 were finally included in the meta-analysis[7-16], including 869 patients with artificial joint replacement (Figure 1). Table 1 shows the general information, intervention measures, time, and outcome indicators. Study quality evaluation based on Jadad quality rating scale ais shown in Table 2.
| Ref. | Number of cases | Gender (male/female) | Age (mean ± SD, yr) | Intervention measures | Intervention time | Outcome indicators | ||||
| Observers | Control group | Observers | Control group | Observers | Control group | Observers | Control group | |||
| Ye et al[7], 2020 | 30 | 30 | 19/11 | 17/13 | 72.51 ± 6.31 | 73.16 ± 5.87 | Low molecular weight heparin calcium + periodic inflation pressurization system | Low molecular weight heparin calcium | 14 d | Deep vein thrombosis |
| Yuan et al[8], 2019 | 40 | 40 | 18/22 | 21/19 | 71.36 ± 4.37 | 70.85 ± 5.04 | Low molecular weight heparin calcium + periodic inflation pressurization system | Routine prevention | 7-10 d | Deep vein thrombosis |
| Peng et al[9], 2019 | 32 | 32 | 20/12 | 19/13 | 74.88 ± 6.02 | 75.13 ± 5.42 | Rivaroxaban | Low molecular weight heparin calcium | 14 d | Deep vein thrombosis |
| Deng et al[10], 2016 | 43 | 40 | 24/19 | 22/18 | 69.17 ± 6.52 | 70.49 ± 5.88 | Rivaroxaban | Low molecular weight heparin calcium | 14 d | Deep vein thrombosis |
| Peng et al[11], 2013 | 40 | 40 | 23/17 | 24/16 | 76.10 ± 5.23 | 75.78 ± 4.36 | Low molecular weight heparin calcium + gradient elastic compression socks | Gradient elastic compression socks | 4-6 wk | Deep vein thrombosis |
| Wu et al[12], 2014 | 40 | 40 | - | - | - | - | Periodic inflation and pressurization system | Routine prevention | 14-21 d | Deep vein thrombosis |
| Jin et al[13], 2018 | 37 | 37 | 22/15 | 23/14 | 72.54 ± 3.48 | 74.01 ± 5.12 | Low molecular weight heparin calcium | Routine prevention | 7 d | Deep vein thrombosis pulmonary embolism |
| Rao et al[14], 2018 | sixty-eight | sixty-eight | 36/32 | 32/36 | 71.28 ± 5.01 | 70.64 ± 4.51 | Rehabilitation training + periodic inflation and pressurization system | Rehabilitation training | - | Deep vein thrombosis |
| Qian et al[15], 2019 | 63 | 63 | 30/33 | 31/32 | 74.52 ± 6.14 | 73.68 ± 5.43 | Arteriovenous foot pump | Routine prevention | - | Deep vein thrombosis |
| Liu et al[16], 2015 | 43 | 43 | 30/13 | 32/11 | 70.46 ± 5.55 | 71.18 ± 4.61 | Low molecular weight heparin calcium | Gradient elastic compression socks | 10 d | Deep vein thrombosis |
| Ref. | Random sequence generation method | Blinding | Exit and lost visits | Quality score |
| Ye et al[7], 2020 | 1 | 1 | 1 | 3 |
| Yuan et al[8], 2019 | 2 | 1 | 1 | 4 |
| Peng et al[9], 2019 | 2 | 1 | 0 | 3 |
| Deng et al[10], 2016 | 1 | 2 | 0 | 3 |
| Peng et al[11], 2013 | 1 | 1 | 1 | 3 |
| Wu et al[12], 2014 | 1 | 2 | 1 | 4 |
| Jin et al[13], 2018 | 2 | 2 | 1 | 5 |
| Rao et al[14], 2018 | 1 | 2 | 0 | 3 |
| Qian et al[15], 2019 | 0 | 2 | 1 | 3 |
| Liu et al[16], 2015 | 2 | 2 | 0 | 4 |
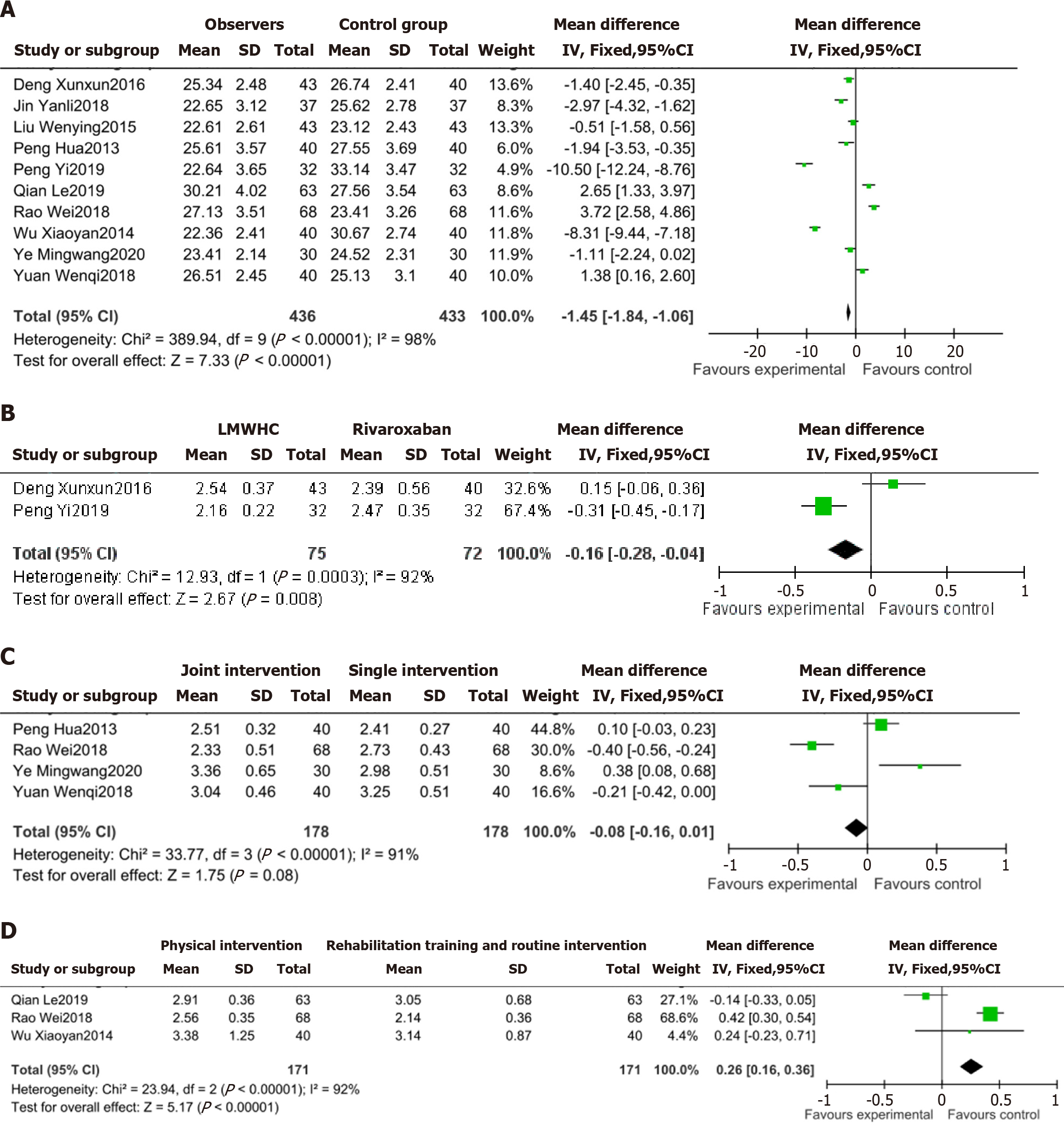
The results of the 10 studies that compared different interventions for prevention of side effects of artificial joint repla
Two studies compared rivaroxaban and LMWH calcium for prevention of side effects of artificial joint replacement, and the results of each study were heterogeneous (I2 = 92%, P < 0.001). The random-effect model showed that the preventive effect of rivaroxaban was significantly better than that of LMWH calcium (MD = -0.16, 95%CI: -0.28 to -0.04), P < 0.05) (Figure 2B).
Four studies compared the preventive effect of combined and single interventions, and the results of each study were heterogeneous (I2 = 91%, P < 0.001). The random-effect model showed that the preventive effect of combined intervention was significantly better than that of single intervention (MD = -0.08, 95%CI: -0.16 to -0.01, P < 0.001) (Figure 2C).
Three studies compared the preventive effect of physical intervention and rehabilitation training and routine inter
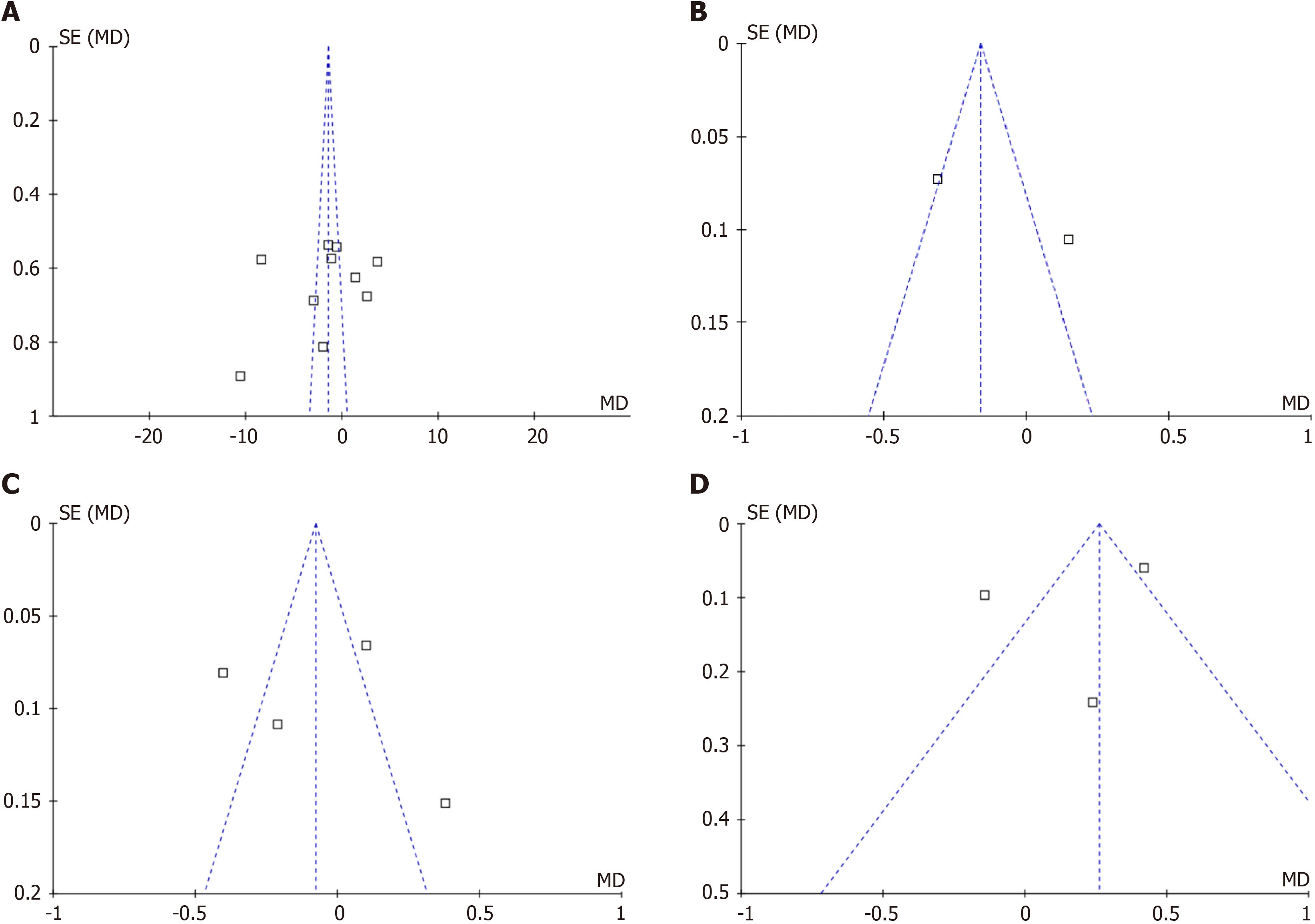
The effect of different intervention measures on the side effects of artificial joint replacement was reported in 10 studies. Due to the limited number of studies, the funnel diagram was sparse, but the overall symmetry was good, suggesting that the publication bias was small (Figure 3A).
Two studies investigated the preventive effect of drug intervention. The funnel diagram was sparse, but the overall symmetry was good, suggesting that the publication bias was small (Figure 3B).
Four studies investigated the preventive effect of combined intervention and single intervention. The funnel diagram was sparse, but the overall symmetry was good, suggesting that the publication bias was small (Figure 3C).
Three studies investigated the preventive effects of physical intervention and rehabilitation training and routine intervention. The mapping results showed that the overall symmetry was poor and there was publication bias (Figure 3D).
Artificial joint replacement is the main treatment for hip fracture in older patients, but it can cause postoperative venous thromboembolism after operation, mainly including deep venous thrombosis and pulmonary embolism[17]. Patients can have symptoms such as limb swelling and pain after venous thromboembolism, which can lead to prolonged hospitalization, increased treatment cost, poor treatment outcome, and even pulmonary embolism and death[18]. Clinical attention has been paid to these types of side effects, and many different intervention measures have been taken to prevent them. There are many preventive measures for venous thromboembolism, including routine prevention, physical prevention, rehabilitation training and drug therapy[19]. Common physical prevention methods include gradient elastic compression socks, periodic inflation compression system and arteriovenous foot pump, and LMWH sodium, LMWH calcium and rivaroxaban are commonly used in drug therapy. According to many clinical studies, physical intervention and drug therapy can reduce the incidence of side effects and promote the recovery of patients, but no research has clearly pointed out which prevention method is the most effective[20].
For prevention of deep venous thrombosis, rivaroxaban combined with rehabilitation training is better than other intervention methods. Rivaroxaban is a new oral anticoagulant drug that inhibits production of thrombin and reduce the risk of thrombosis. Rehabilitation training plays an irreplaceable role in promoting blood circulation and reducing limb swelling[21]. There are also studies comparing physical prevention and rehabilitation training, which have shown that the preventive effect of periodic inflation and pressurization is better than that of rehabilitation training. The researchers pointed out that rehabilitation is affected by self-consciousness and patients’ limb movements, and compliance is poor, which is not conducive to recovery. Periodic inflation and pressurization are designed according to the principles of human biomechanics, and regularly exert pressure on patients’ ankles, calves, and thighs. This prevents blood stasis in the lower limbs and generates pulsatile blood flow, which then passes through the deep veins of distal limbs to promote the blood reflux of deep veins in lower limbs, so as to reduce the occurrence of thrombosis[22]. Some scholars have pointed out that in physical prevention, the arteriovenous foot pump is better than gradient elastic compression socks, mainly because it is an automated system, whereas gradient elastic compression socks are a passive method, and their mild antithrombotic duration is lower than that of the arteriovenous foot pump[23]. Thus, the combination of drugs and physical intervention or a single prevention method is better than rehabilitation training.
For prevention of pulmonary embolism, some studies have pointed out that rivaroxaban is superior to other methods. The reason is that rivaroxaban acts rapidly, within 2 h. It is less affected by other drugs, and is not accumulated after multiple administrations. It has a marked effect in reducing thrombosis and preventing pulmonary embolism[24]. LMWH was a commonly used anticoagulant drug in the past. Although its anticoagulant effect is good, it has the risk of subcutaneous bleeding, and it needs to be injected by trained medical staff, which is inconvenient for discharged patients[25]. Combined intervention is superior to single intervention, which may compensate for any deficiency of the single intervention. For example, drug therapy exerts its preventive effect via the cardiovascular and gastrointestinal systems, whereas physical intervention and rehabilitation training act via external factors, so their combination can maximize the preventive effect[26]. Therefore, when preventing the side effects of artificial joint replacement in the clinic, medical staff should establish the etiology, risk, and symptoms of venous thromboembolism, and take effective intervention measures to reduce the risk of complications.
The effect of joint intervention is clearly better than that of single intervention. However, there were some limitations to this study. First, there was a possibility of selection, implementation, measurement, and loss bias in the selection of studies. Second, information such as the method of randomization, distribution and concealment, and the use of blinding method were not clearly explained in some of the included studies, which affected the quality of the studies and their conclusions. Third, some interventions with good comprehensive effects have not been widely studied. Finally, the sample size was small.
Rivaroxaban combined with rehabilitation training is preferred for preventing deep vein thrombosis after artificial joint replacement. In the prevention of pulmonary embolism, rivaroxaban drug intervention is given priority. The effect of combined intervention is better than that of single intervention.
| 1. | Fan J, Xu X, Zhou F, Zhang Z, Tian Y, Ji H, Guo Y, Lv Y, Yang Z, Hou G. Risk factors for implant failure of intertrochanteric fractures with lateral femoral wall fracture after intramedullary nail fixation. Injury. 2021;52:3397-3403. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 21] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 2. | Yoo JI, Cha Y, Kwak J, Kim HY, Choy WS. Review on Basicervical Femoral Neck Fracture: Definition, Treatments, and Failures. Hip Pelvis. 2020;32:170-181. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 25] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 3. | Abbas A, Kazem GED, Alem A, Shoulah SA. Different Methods of Treatment of Trochanteric Fractures in Elderly. 2021. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 4. | Doğan N, Ertürk C, Gülabi D. Is proximal femoral nailing of unstable intertrochanteric fractures in the lateral decubitus position without a traction table as safe and effective as on a traction table? Injury. 2022;53:555-560. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 13] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 5. | Chen JM, Yue C, He PL, Zhang JT, Sun MY, Liu YW. Hip arthroplasty vs proximal femoral nail antirotation for intertrochanteric fractures in older adults: a meta-analysis. Xunzheng Yixue. 2021;25:1452. |
| 6. | Mickenautsch S, Miletić I, Rupf S, Renteria J, Göstemeyer G. The Composite Quality Score (CQS) as a trial appraisal tool: inter-rater reliability and rating time. Clin Oral Investig. 2021;25:6015-6023. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 7. | Ye MW, Wang HQ, Ma WJ, Wu ZF, Zeng RF. The efficacy of intermittent pneumatic compression therapy combined with low molecular heparin calcium in preventing lower extremity venous thrombosis after artificial hip arthroplasty. Jiceng Yixue Luntan. 2020;24:4581-4582. [DOI] [Full Text] |
| 8. | Yuan WQ, Wang HP. Observation on Preventive Effect of Low Molecular Weight Heparin Calcium Combined with Pressure Antithrombotic Pumps on Deep Venous Thrombosis (DVT) Formation after Hip Arthroplasty. Zhongguo Heli Yongyao Tansuo. 2019;16:102-104. [DOI] [Full Text] |
| 9. | Peng Y, Meng J. Comparison of Rivaroxaban and Low Molecular Weight Heparin in Prevention of Deep Venous Thrombosis after Hip Arthroplasty. Xueshuan Yu Zhixuexue. 2019;25:794-795. [DOI] [Full Text] |
| 10. | Deng XX, Huang YG. Efficacy of rivaroxaban for the prevention of 43 cases of elderly patients with deep venous thrombosis after hip joint surgery. Shanghai Yiyao. 2016;37:25-27+54. |
| 11. | Peng H, Wang JY, Guo S. Study on prevention of lower extremity deep vein thrombosis after total hip arthroplasty by low molecular heparin with medical compression stockings. Zhongguo Shiyong Yiyao. 2013;8:176-178. [DOI] [Full Text] |
| 12. | Wu XY, Chai XL, Wang ZJ, Liu WM, Song MJ. Prevention and nursing research of early use of ASPCP in elderly patients with deep vein thrombosis after total arthroplasty hip replacement. Xibei Guofang Yixue Zazhi. 2014;35:274-276. [DOI] [Full Text] |
| 13. | Jin YL, Liu T, Feng P, Miao Q. Effects of Low Molecular Weight Heparin on Preoperative Blood Hypercoagulability and Postoperative Deep Venous Thrombosis in Middle-aged and Elderly Patients Undergoing Hip Replacement. Linchuang Wuzhen Wuzhi. 2018;31:54-59. [DOI] [Full Text] |
| 14. | Rao W. The Role of Intermittent Pneumatic Therapy in Early Rehabilitation after Total Hip Arthroplasty. Zhongwai Yiliao. 2018;37:83-84+87. [DOI] [Full Text] |
| 15. | Qian L, Liu L. Nursing analysis of application of plantar vein pump to prevent lower extremity deep vein thrombosis after artificial joint replacement surgery. Dangdai Linchuang Yikan. 2019;32:213+215. [DOI] [Full Text] |
| 16. | Liu WY. The effect of low molecular heparin calcium with medical compression stockings in preventing lower extremity deep vein thrombosis after hip arthroplasty and nursing care experience. Zhongguo Yaoye. 2015;24:69-70. |
| 17. | Feng W, Wang X, Huang D, Lu A. Ranking the efficacy of anticoagulants for the prevention of venous thromboembolism after total hip or knee arthroplasty: A systematic review and a network meta-analysis. Pharmacol Res. 2021;166:105438. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 18. | Børvik T, Evensen LH, Morelli VM, Melbye H, Brækkan SK, Hansen JB. Impact of respiratory symptoms and oxygen saturation on the risk of incident venous thromboembolism-the Tromsø study. Res Pract Thromb Haemost. 2020;4:255-262. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 19. | Funayama M, Takata T. Psychiatric inpatients subjected to physical restraint have a higher risk of deep vein thrombosis and aspiration pneumonia. Gen Hosp Psychiatry. 2020;62:1-5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 28] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 20. | Al-Mugheed K, Totur Dikmen B, Bayraktar N, Farghaly Abdelaliem SM, Ahmed Alsenany S. Nursing Care and Barriers for Prevention of Venous Thromboembolism in Total Knee and Hip Arthroplasty Patients: A Qualitative Study. J Multidiscip Healthc. 2023;16:547-556. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 21. | Zhou B, She J, Wang Y, Ma X. A Case of Coronavirus Disease 2019 With Concomitant Acute Cerebral Infarction and Deep Vein Thrombosis. Front Neurol. 2020;11:296. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 33] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 22. | Wang S, Lu H, Li S. Prevention of deep venous thrombosis in patients undergoing knee arthroplasty by intermittent pneumatic compression apparatus. Am J Transl Res. 2021;13:10765-10770. [PubMed] |
| 23. | Sussman M, Almeida J. Chapter 17 - Deep vein thrombosis and prevention of postthrombotic syndrome. In: Shortell CK, Markovic JN, editors. Venous Ulcers (Second Edition): Academic Press, 2023: 297-314. [DOI] [Full Text] |
| 24. | Barco S, Schmidtmann I, Ageno W, Bauersachs RM, Becattini C, Bernardi E, Beyer-Westendorf J, Bonacchini L, Brachmann J, Christ M, Czihal M, Duerschmied D, Empen K, Espinola-Klein C, Ficker JH, Fonseca C, Genth-Zotz S, Jiménez D, Harjola VP, Held M, Iogna Prat L, Lange TJ, Manolis A, Meyer A, Mustonen P, Rauch-Kroehnert U, Ruiz-Artacho P, Schellong S, Schwaiblmair M, Stahrenberg R, Westerweel PE, Wild PS, Konstantinides SV, Lankeit M; HoT-PE Investigators. Early discharge and home treatment of patients with low-risk pulmonary embolism with the oral factor Xa inhibitor rivaroxaban: an international multicentre single-arm clinical trial. Eur Heart J. 2020;41:509-518. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 80] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 25. | Bistervels IM, Buchmüller A, Wiegers HMG, Ní Áinle F, Tardy B, Donnelly J, Verhamme P, Jacobsen AF, Hansen AT, Rodger MA, DeSancho MT, Shmakov RG, van Es N, Prins MH, Chauleur C, Middeldorp S; Highlow Block writing committee; Highlow Investigators. Intermediate-dose versus low-dose low-molecular-weight heparin in pregnant and post-partum women with a history of venous thromboembolism (Highlow study): an open-label, multicentre, randomised, controlled trial. Lancet. 2022;400:1777-1787. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 60] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 26. | Gouverneur A, Lair A, Arnaud M, Bégaud B, Raschi E, Pariente A, Salvo F. DPP-4 inhibitors and venous thromboembolism: an analysis of the WHO spontaneous reporting database. Lancet Diabetes Endocrinol. 2020;8:365-367. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 19] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: China
Peer-review report’s classification
Scientific Quality: Grade B
Novelty: Grade B
Creativity or Innovation: Grade B
Scientific Significance: Grade B
P-Reviewer: Gadour E, United Kingdom S-Editor: Liu JH L-Editor: A P-Editor: Zhao YQ