Published online May 18, 2024. doi: 10.5312/wjo.v15.i5.444
Revised: March 5, 2024
Accepted: April 12, 2024
Published online: May 18, 2024
Processing time: 112 Days and 14.5 Hours
Unicompartmental knee arthroplasty (UKA) and high tibial osteotomy (HTO) are well-established operative interventions in the treatment of knee osteoarthritis. However, which intervention is more beneficial to patients with knee osteo
To compare UKAs and HTOs as interventions for medial-compartment knee osteoarthritis: Examining differences in clinical outcome and investigating the relationship of joint alignment with respect to this.
This longitudinal observational study assessed a total of 42 patients that had undergone UKA (n = 23) and HTO (n = 19) to treat medial compartment knee osteoarthritis. Patient-reported outcome measures (PROMs) were collected to evaluate clinical outcome. These included two disease-specific (Knee Injury and Osteoarthritis Outcome Score, Oxford Knee Score) and two generic (EQ-5D-5L, Short Form-12) PROMs. The radiographic parameters of knee alignment assessed were the: Hip-knee-ankle angle, mechanical axis deviation and angle of Mikulicz line.
Statistical analyses demonstrated significant (P < 0.001), preoperative to postoperative, improvements in the PROM scores of both groups. There were, however, no significant inter-group differences in the postoperative PROM scores of the UKA and HTO group. Several significant correlations associated a more distolaterally angled Mikulicz line with worse knee function and overall health preoperatively (P < 0.05). Postoperatively, two clusters of significant correlations were observed between the disease-specific PROM scores and knee joint alignment para
UKAs and HTOs are both efficacious operations that provide a comparable degree of clinical benefit to patients with medial compartment knee osteoarthritis. Clinical outcome has a limited association with radiographic para
Core Tip: A great deal of uncertainty exists in the literature about which operation, out of unicompartmental knee arthroplasty (UKA) or high tibial osteotomy (HTO), is more beneficial in the treatment of knee osteoarthritis. This study adds evidence to the existing literature base, concluding that HTOs and UKAs are equally efficacious operative interventions capable of providing a comparable degree of improvement in joint function and global health-related quality of life, to those with medial compartment knee osteoarthritis at one year postoperatively. This study is the first of its kind to report a correlation analysis between the angle of Mikulicz line and patient-reported health outcomes. It demonstrated that preoperatively, a more distolaterally angled Mikulicz line was associated worse knee function/health-related quality of life. The mechanisms underlying this relationship remain unknown and represent an avenue for future research; the authors of this study posit an association with the external knee adduction moment.
- Citation: Wyatt FW, Al-Dadah O. Unicompartmental knee arthroplasty vs high tibial osteotomy for knee osteoarthritis: A comparison of clinical and radiological outcomes. World J Orthop 2024; 15(5): 444-456
- URL: https://www.wjgnet.com/2218-5836/full/v15/i5/444.htm
- DOI: https://dx.doi.org/10.5312/wjo.v15.i5.444
In 2019 osteoarthritis was the 15th leading cause of years lived with disability worldwide, with knee osteoarthritis acco
UKA and HTO are often indicated ahead of total knee arthroplasty as these joint-preserving operations represent less invasive alternatives that enable more elements of the native knee joint to be retained whilst providing the opportunity to delay, or even prevent, the need for total knee arthroplasty[3,5].
Previous research has established that, with the correct inclusion/exclusion criteria applied, HTOs and UKAs are safe and effective surgical interventions[5]. Despite this, which of these interventions is more beneficial in the treatment of isolated medial compartment knee osteoarthritis is yet to be clarified within the literature and remains a topic of much debate[6-8]. In particular, there is a paucity of research that assesses and compares the impact of these operations on patient-reported outcomes, with the majority of current literature centred around clinician-assessed objective outcomes[9]. This is of clinical significance as, despite “ideal” indications varying between HTO and UKA, there are many patients that would be considered eligible for both operations.
Further to this, only a small number of studies have directly compared the radiographic parameters of knee joint align
The primary aim of this study was to assess and compare the patient reported outcome measures (PROMs) of patients undergoing HTO and UKA, to determine which of these interventions is more beneficial in the treatment of isolated medial compartment knee osteoarthritis, if indeed a significant difference were to exist. The secondary aim was to investigate the relationship between radiographic parameters of knee joint alignment and PROMs; preoperatively and following UKA and HTO.
The authors developed three hypotheses with respect to the aforementioned aims. Hypothesis 1: HTO and UKA provide significant, preoperative to postoperative, improvements in patient-reported symptomatology. Hypothesis 2: UKA and HTO are equally efficacious operative interventions in the treatment of isolated medial compartment knee osteoarthritis. Hypothesis 3: Radiographic parameters of knee joint alignment do not correlate with PROM scores.
Patients that had undergone an elective HTO or UKA for medial compartment knee osteoarthritis between 2015 and 2019, under the care of a single consultant orthopaedic surgeon with a specialist interest in knee surgery at a district general hospital, were screened for study eligibility. Inclusion criteria: Isolated medial compartment knee osteoarthritis and completion of relevant PROMs. Exclusion criteria: Revision surgery, cruciate or collateral ligament insufficiency and multi-compartment knee osteoarthritis. This study was exempt from Institutional Review Board/Ethics Committee approval as it was a pragmatic study evaluating the existing clinical practice of the senior author. This therapeutic resea
This study adopted a longitudinal observational design. Data collection commenced during each patient’s initial out
HTO group: A standard direct medial approach was used to perform the biplanar medial opening-wedge HTOs. A TomoFix Plate (DePuy Synthes, Pennsylvania, United States) was used to fixate the osteotomy site. The target limb alignment within the HTO group was such that the mechanical axis would intersect Fujisawa’s point (marginally lateral to the lateral tibial spine). Preoperative planning, for all patients, was undertaken on AP long-leg alignment radiographs according to the technique described by Miniaci et al[10]. All HTO patients underwent a simultaneous knee arthroscopy and microfracture of the medial femoral condyle and medial tibial plateau. Those with degenerate meniscal tears also underwent a partial meniscectomy. All patients were mobilised non-weight bearing, but with full range of movement, for 6 wk following surgery. Thereafter, full weight bearing was commenced under the guidance of a structured postoperative physiotherapy lead rehabilitation programme.
UKA group: A minimally invasive, quadriceps sparing, approach was used to perform the UKAs. Each patient was treated with a cemented JOURNEY UNI (Smith and Nephew, Memphis, Tennessee, United States) medial unicompartmental knee system with a fixed-bearing, metal-backed tibial component and an oxinium femoral component as stand
Two generic and two disease-specific PROMs were obtained from each patient. The generic PROMs consisted of the Short Form-12 (SF-12) and EQ-5D-5L. Disease specific PROMs consisted of the Oxford Knee Score (OKS) and Knee Injury and Osteoarthritis Outcome Score (KOOS). Higher PROM scores were indicative of better health outcomes, and vice versa, for all the PROMs used within this study.
Two summary scores were derived from the SF-12: A mental component score and a physical component score[11,12]. The EQ-5D-5L consisted of a descriptive score and a visual analogue scale score[13]. KOOS assessed the impact of knee osteoarthritis across five subscales: Pain, activities of daily living (ADL), sports and recreation (Sport/Rec), knee-related quality of life (QoL), and other symptoms[14,15]. The OKS was calculated using the updated standardised scoring system[16,17]. Data regarding patient co-morbidities was collected via the Self-Administered Comorbidity Questionnaire: A validated, self-reported, generic-health questionnaire. Self-Administered Comorbidity Questionnaire scoring was cond
All digital films were stored, viewed, and evaluated - using software tools-on the Picture Archive and Communication System (Centricity version 6, GE Healthcare, Chicago). Measurements were accurate to within ± 0.05° and ± 0.05 mm.
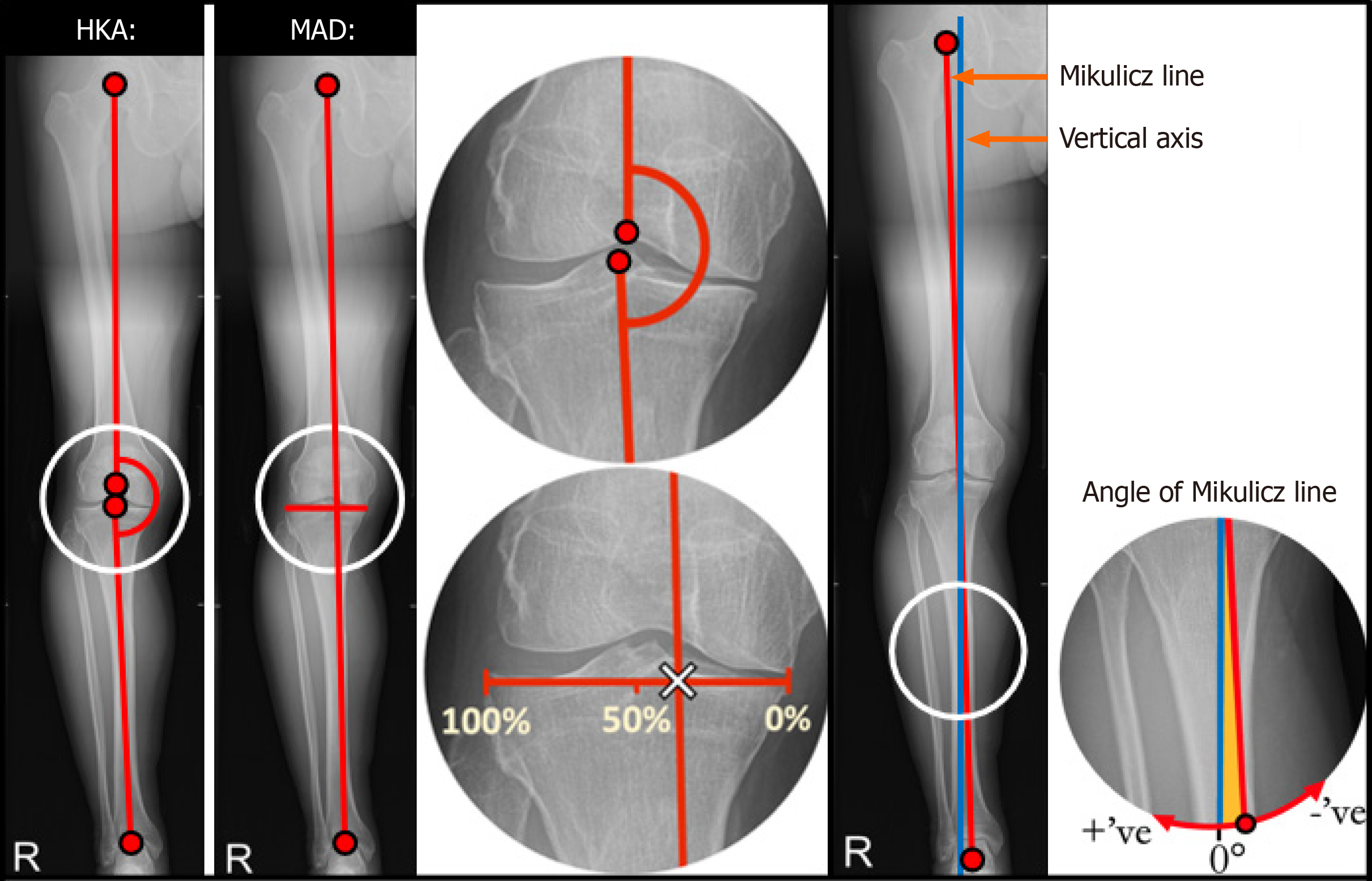
Knee osteoarthritis severity was determined by assessing preoperative Rosenberg and long leg AP films using the Kellgren-Lawrence grading system[19]. Pre- and postoperative long-leg AP weight-bearing films were used to assess the lower limb mechanical axes of each patient, which were defined by proximal and distal joint-centre points as outlined by Paley and Pfeil[20]. These mechanical axes were used to determine the hip knee ankle angle (HKA), mechanical axis deviation (MAD) and angle of Mikulicz line (lower-limb mechanical axis) of each participant pre- and postoperatively.
The HKA is the medial angle subtended by the intersection of the mechanical axes of the femur and tibia (Figure 1). Varus and valgus deformities were represented by HKAs of < 180° and > 180° respectively. “Neutral” alignment, in non-arthritic individuals, rests in 1-1.5° of varus (178.5° < HKA < 179°)[21].
MAD is a quantitative measure of where the lower limb mechanical axis (Mikulicz line) passes through the knee joint. This parameter identifies the location through which load-transmission forces pass through the knee (Figure 1). To standardise against natural variations in physique, raw values for MAD were expressed as a percentage of overall tibial width[22]. Mechanical axes passing medially to the entire tibial plateau were ascribed negative values.
The mechanical axis of the lower limb (Mikulicz line) allows ground reaction forces, passing from the centre of the ankle to the femoral head, to be visualised. The angle of the Mikulicz line relative to the vertical axis was measured (Figure 1). Distolaterally oriented Mikulicz lines were ascribed positive values, whereas distomedially oriented Mikulicz lines were ascribed negative values.
The power calculation for this study was derived from the findings of a related previously published clinical study[23]. The sample sizes were based on a conventional alpha of 0.05 and a power of 80%. The calculation revealed that a sample size of approximately 17 subjects per group was required for a clinically relevant postoperative PROM score (International Knee Documentation Committee) between group mean difference of 11.1, based on a pooled standard deviation of 11.05. Plotted histograms with fitted curve lines, box-plots, normal Q-Q plots and the Kolmogorov-Smirnov statistic were used to confirm that a normal distribution was an appropriate assumption for all the continuous variables in the study. The relevant parametric statistical tests were used. The independent-sample Student's t-test was used for the between group analyses and the paired Student’s t-test was used for the within group analysis. The Pearson product-moment test was used for the correlation analysis. To quantify the strengths of the observed linear relationships, correlation co-efficient cut-off values were used as outlined by Chan[24]: > 0.8 (very strong), 0.6-0.8 (moderately strong), 0.3-0.5 (fair) and < 0.3 (poor). The level of statistical significance was set at P < 0.05. Statistical analysis was performed using SPSS for Windows version 26.0 (IBM Corp., Armonk, New York). The power calculation was performed using Minitab statistical software version 18 (Minitab LLC, State College, PA, United States).
A total of 42 patients (UKA group = 23, HTO group = 19) were included in this study. Table 1 displays the demographic data of the UKA and HTO group. Overall, the HTO group were slightly younger and had proportionately more males than the UKA group. These differences are a reflection of patient selection with respect to treatment suitability at the time of initial clinic consultation and also the treatment preferences of the patients once they had been engaged in a shared decision-making process.
| UKA group (n = 23) | HTO group (n = 19) | |
| Age (years), mean (SD) | 66.9 (8.6) | 54.3 (10.8) |
| Sex (male:female) | 12:11 | 18:1 |
| Laterality (left:right) | 15:8 | 11:8 |
| Smoking, n (%) | 1 (4.5) | 1 (5.6) |
| Height (cm), mean (SD) | 167.1 (10.0) | 174.2 (9.1) |
| Weight (kg), mean (SD) | 84.2 (18.4) | 95.6 (16.8) |
| BMI (kg/m2), mean (SD) | 30.0 (4.6) | 31.5 (4.8) |
| ASA, median (range) | 2 (1 to 3) | 2 (1 to 2) |
| SCQ, median (range) | 3.5 (0 to 12) | 3 (0 to 10) |
There were no significant preoperative between-group differences for any of the preoperative PROM scores except for the SF-12 mental component score which was only of borderline significance (P = 0.043) (Table 2).
| Preoperative | Postoperative | |||||||
| UKA group mean (SD) | HTO group mean (SD) | P value1 | 95%CI | UKA group mean (SD) | HTO group mean (SD) | P value1 | 95%CI | |
| KOOS: | ||||||||
| Pain | 32.5 (8.2) | 35.2 (17.7) | 0.530 | -5.8 to 11.1 | 91.1 (12.7) | 87.2 (12.4) | 0.419 | -13.5 to 5.8 |
| Symptoms | 42.3 (17.8) | 38.2 (17.8) | 0.462 | -15.2 to 7.1 | 87.0 (12.9) | 73.0 (17.3) | 0.012a | -24.6 to -3.3 |
| ADLs | 38.0 (9.1) | 42.2 (17.3) | 0.320 | -4.2 to 12.6 | 90.6 (13.9) | 90.2 (10.8) | 0.936 | -9.8 to 9.1 |
| Sport/Rec | 19.0 (21.3) | 14.4 (12.4) | 0.455 | -16.9 to 7.7 | 78.7 (28.9) | 71.8 (27.6) | 0.549 | -30.1 to 16.4 |
| QoL | 17.8 (11.9) | 13.0 (11.9) | 0.211 | -12.5 to 2.9 | 80.1 (21.8) | 67.8 (14.8) | 0.107 | -27.4 to 2.8 |
| Overall | 29.1 (7.9) | 27.1 (13.1) | 0.580 | -9.3 to 5.3 | 85.2 (17.3) | 78.4 (13.6) | 0.295 | -19.8 to 6.3 |
| OKS | 16.5 (5.6) | 18.4 (7.8) | 0.362 | -2.3 to 6.1 | 42.4 (6.3) | 42.1 (5.2) | 0.872 | -4.7 to 4.0 |
| EQ-5DIndex | 35.6 (24.0) | 37.4 (29.7) | 0.834 | -15.4 to 19.0 | 84.7 (18.8) | 80.8 (15.1) | 0.557 | -17.4 to 9.6 |
| EQ-5DVAS | 72.4 (17.6) | 64.8 (23.4) | 0.237 | -20.4 to 5.2 | 88.3 (12.7) | 82.9 (9.6) | 0.210 | -14.0 to 3.2 |
| SF-12 PCS | 28.9 (5.8) | 32.1 (7.7) | 0.143 | -1.1 to 7.5 | 50.9 (7.7) | 50.0 (8.9) | 0.983 | -7.4 to 5.5 |
| SF-12 MCS | 51.0 (11.4) | 42.9 (13.0) | 0.043a | -15.9 to -0.3 | 51.8 (9.7) | 50.8 (10.5) | 0.511 | -8.8 to 6.9 |
Overall, there were no significant differences in postoperative PROM scores between the HTO group and the UKA group (Table 2), except for the KOOS: Symptoms subscore (P = 0.012) in which UKA demonstrated a superior result.
The longitudinal within-group analysis (Table 3) demonstrated a significant improvement of all PROM scores following surgery, except for the EQ-5D-5L visual analogue score in the HTO group and SF-12 mental component score in both groups.
| UKA Group | HTO Group | |||||||
| Pre-op mean (SD) | Post-op mean (SD) | P value1 | 95%CI | Pre-op mean (SD) | Post-op mean (SD) | P value1 | 95%CI | |
| KOOS: | ||||||||
| Pain | 32.5 (8.2) | 91.1 (12.7) | < 0.001a | 51.8 to 63.3 | 35.2 (17.7) | 87.2 (12.4) | < 0.001a | 37.5 to 63.0 |
| Symptoms | 42.3 (17.8) | 87.0 (12.9) | < 0.001a | 37.3 to 52.1 | 38.2 (17.8) | 73.0 (17.3) | < 0.001a | 25.7 to 49.5 |
| ADLs | 38.0 (9.1) | 90.6 (13.9) | < 0.001a | 47.6 to 57.1 | 42.2 (17.3) | 90.2 (10.8) | < 0.001a | 32.9 to 53.9 |
| Sport/Rec | 19.0 (21.3) | 78.7 (28.9) | < 0.001a | 44.9 to 76.5 | 14.4 (12.4) | 71.8 (27.6) | < 0.001a | 39.7 to 71.2 |
| QoL | 17.8 (11.9) | 80.1 (21.8) | < 0.001a | 53.9 to 71.6 | 13.0 (11.9) | 67.8 (14.8) | < 0.001a | 40.9 to 62.6 |
| Overall | 29.1 (7.9) | 85.2 (17.3) | <0.001a | 47.8 to 63.6 | 27.1 (13.1) | 78.4 (13.6) | < 0.001a | 37.7 to 58.1 |
| OKS | 16.5 (5.6) | 42.4 (6.3) | < 0.001a | 23.0 to 28.6 | 18.4 (7.8) | 42.1 (5.2) | < 0.001a | 16.4 to 27.8 |
| EQ-5DIndex | 35.6 (24.0) | 84.7 (18.8) | < 0.001a | 38.8 to 57.2 | 37.4 (29.7) | 80.8 (15.11) | < 0.001a | 23.8 to 48.9 |
| EQ-5DVAS | 72.4 (17.6) | 88.3 (12.7) | < 0.001a | 8.6 to 23.0 | 64.8 (23.4) | 82.9 (9.6) | 0.069 | -1.2 to 27.0 |
| SF-12 PCS | 28.9 (5.8) | 50.9 (7.7) | < 0.001a | 16.3 to 25.4 | 32.1 (7.7) | 50.0 (8.9) | 0.001a | 9.1 to 25.8 |
| SF-12 MCS | 51.0 (11.4) | 51.8 (9.7) | 0.476 | -3.0 to 6.2 | 42.9 (13.0) | 50.8 (10.5) | 0.115 | -1.8 to 14.1 |
To increase the power of this analysis, the data from both the HTO and UKA group were combined. This was deemed appropriate under the assumption that knee osteoarthritis, a factor common to both groups, was the principal cause of any preoperative correlations observed, and not confounding factors unique to either group. The angle of the Mikulicz line demonstrated significant negative correlations with: KOOS symptoms; KOOS: ADLs; KOOS: QoL; KOOS: Overall; OKS and the EQ-5D-5L descriptive score (Table 4). Each correlation was “fair” in strength, with r values between -0.3 ≥ r > -0.5[24]. These results suggest that, for patients with medial compartment knee osteoarthritis, a more distolaterally angled Mikulicz line is typically associated with worse knee joint function (KOOS-multiple, OKS) and health-related quality of life (EQ-5D-5L descriptive score). A single significant positive correlation was observed in isolation with respect to MAD; this was between MAD and the SF-12 physical component score. No significant correlations were observed with respect to HKA (Table 4).
| Angle of Mikulicz line | HKA | MAD | |
| r (P value1) | r (P value1) | r (P value1) | |
| KOOS: | |||
| Pain | -0.18 (0.290) | -0.12 (0.484) | -0.01 (0.938) |
| Symptoms | -0.36 (0.022a) | 0.15 (0.352) | 0.16 (0.336) |
| ADLs | -0.37 (0.020a) | 0.06 (0.707) | 0.10 (0.534) |
| Sport/Rec | -0.04 (0.839) | 0.06 (0.737) | 0.16 (0.357) |
| QoL | -0.34 (0.040a) | -0.23 (0.169) | -0.14 (0.415) |
| Overall | -0.38 (0.026a) | -0.04 (0.844) | 0.07 (0.698 |
| OKS | -0.41 (0.010a) | 0.13 (0.422) | 0.21 (0.201) |
| EQ-5DIndex | -0.45 (0.005a) | -0.07 (0.670) | -0.02 (0.896) |
| EQ-5DVAS | -0.29 (0.071) | 0.03 (0.843) | 0.06 (0.709) |
| SF-12 PCS | -0.23 (0.158) | 0.26 (0.112) | 0.34 (0.035a) |
| SF-12 MCS | -0.23 (0.173) | -0.05 (0.773) | -0.08 (0.641) |
Following surgery, the HKA and MAD both exhibited significant correlations within the HTO group with KOOS: Sym
| UKA Group | HTO Group | |||||
| Angle of Mikulicz line, r (P value1) | HKA, r (P value1) | MAD, r (P-value1) | Angle of Mikulicz line, r (P-value1) | HKA, r (P-value1) | MAD, r (P-value1) | |
| KOOS: | ||||||
| Pain | -0.17 (0.483) | -0.15 (0.518) | -0.07 (0.760) | 0.13 (0.716) | 0.41 (0.238) | 0.53 (0.119) |
| Symptoms | -0.17 (0.450) | -0.07 (0.772) | 0.02 (0.922) | 0.26 (0.436) | 0.65 (0.032a) | 0.62 (0.040a) |
| ADLs | -0.22 (0.328) | -0.05 (0.837) | 0.01 (0.961) | 0.09 (0.790) | 0.59 (0.055) | 0.62 (0.041a) |
| Sport/Rec | -0.21 (0.459) | 0.15 (0.584) | 0.28 (0.317) | 0.46 (0.178) | 0.5 (0.103) | 0.53 (0.113) |
| QoL | -0.27 (0.249) | -0.11 (0.635) | -0.03 (0.898) | 0.14 (0.693) | 0.58 (0.080) | 0.60 (0.065) |
| Overall | -0.26 (0.357) | -0.01 (0.959) | 0.12 (0.676) | 0.32 (0.373) | 0.65 (0.041a) | 0.68 (0.031a) |
| OKS | -0.34 (0.137) | -0.02 (0.950) | 0.03 (0.884) | 0.24 (0.481) | 0.65 (0.032a) | 0.61 (0.045a) |
| EQ-5DIndex | -0.23 (0.334) | -0.70 (0.768) | 0.01 (0.974) | -0.13 (0.724) | 0.47 (0.175) | 0.45 (0.191) |
| EQ-5DVAS | -0.23 (0.304) | -0.02 (0.942) | 0.03 (0.881) | 0.10 (0.776) | 0.21 (0.534) | 0.21 (0.544) |
| SF-12 PCS | -0.14 (0.584) | -0.13 (0.615) | -0.02 (0.929) | -0.07 (0.850) | 0.15 (0.680) | 0.18 (0.616) |
| SF-12 MCS | -0.49 (0.041a) | -0.24 (0.341) | -0.19 (0.455) | -0.02 (0.953) | 0.38 (0.279) | 0.29 (0.422) |
The UKA group demonstrated significant differences (P < 0.001) between the preoperative and postoperative values of the HKA and MAD. A far more anatomic knee joint alignment was achieved postoperatively within the UKA group, with the mean HKA increasing from a varus position (174.5° ± 2.7°) to a neutral one (180.2° ± 3.3°) resulting in the mechanical axis crossing the centre of the knee (postoperative MAD = 48.9%) as opposed to the medial compartment (preoperative MAD = 23.5%) (Table 6).
| UKA Group | HTO Group | |||||||
| Pre-op mean (SD) | Post-op mean (SD) | P value1 | 95%CI | Pre-op mean (SD) | Post-op mean (SD) | P value1 | 95%CI | |
| Angle of Mikulicz line (°) | 0.3 (2.6) | -0.2 (1.8) | 0.326 | -1.6 to 0.6 | 0.7 (2.0) | 0.2 (1.5) | 0.951 | -1.5 to 1.6 |
| HKA (°) | 174.5 (2.7) | 180.2 (3.3) | < 0.001a | 4.3 to 7.1 | 173.9 (4.0) | 182.5 (2.8) | < 0.001a | 5.2 to 12.0 |
| MAD (%) | 23.5 (10.8) | 48.9 (13.6) | < 0.001a | 20.7 to 30.0 | 22.3 (14.5) | 59.9 (12.0) | < 0.001a | 24.2 to 51.0 |
The HTO group demonstrated significant differences (P < 0.001) between the preoperative and postoperative values of the HKA and MAD. HTOs are operative interventions that alter the angle of the tibia distal to the osteotomy site: the re-angulation of the tibial mechanical axis is, unsurprisingly, represented within the significantly different postoperative HKA and MAD values. The mean HKA, of the HTO group, increased from a varus position preoperatively (173.9° ± 4°), to a slight valgus position postoperatively (182.5° ± 2.8°). The goal of HTO is to relieve pressure from the medial compa
Patients within both the UKA and HTO group demonstrated significant clinical improvements following surgery, as compared to their preoperative state. There was no significant difference in the generic and disease-specific postoperative PROM scores between the HTO and UKA groups, reflecting that both surgical interventions are equally as efficacious in terms of improving knee joint function and global health-related quality of life at one year postoperatively. Overall, radiographic parameters of knee joint alignment demonstrated limited correlation with PROM scores. However, two isolated clusters of significant correlations were observed with respect to PROMs and the angle of Mikulicz line preoperatively; and joint alignment (HKA and MAD) within the HTO group postoperatively.
Significant preoperative to postoperative improvements were observed within almost all the PROM scores of the UKA and HTO group. Statistical significance does not always equate to clinical significance. Postoperative PROM scores are best contextualised with reference to ‘patient acceptable symptom state’ thresholds: PROM scores equating to the highest level of symptomatic burden that the average patient would consider acceptable postoperatively. PROM patient accep
The mean postoperative score of each PROM that had increased significantly postoperatively, also superseded their corresponding PROM patient acceptable symptom state threshold; indicating that UKAs and HTOs are operative inte
This study found UKAs and HTOs to be comparable operative interventions for knee osteoarthritis as the postoperative PROM scores were, with the exception of KOOS: Symptoms, not significantly different between the two groups. The findings of this study prove hypothesis 2 to be true and are consistent with those of previous studies, with UKAs resu
Conversely, retrospective comparative studies conducted by Ivarsson and Gillquist[30] and Ryu et al[7], with shorter follow up periods of 3-6 months, demonstrated statistically significant differences in postoperative PROM scores in favour of UKAs. These findings possibly reflect the lengthier rehabilitation process associated with HTOs: as more time elapses postoperatively, HTO patients report improved PROM scores that are eventually comparable to those of UKAs (which allow patients to fully weight-bear from the day of surgery). Yokoyama et al[31] estimated that the time required to functionally heal, following HTO, is approximately 6 months; a conclusion that supports this hypothesis and better contextualises the non-significance of the 1-year postoperative results of the current study (Table 2), relative to the signi
Despite the observed similarity in postoperative clinical outcomes achieved, UKAs and HTOs are fundamentally very different operations, associated with their own relative merits. HTOs are associated with an increased postoperative range of motion[4-6] and lower risk of revision surgery[32]; whereas patients undergoing UKA typically benefit from a shorter recovery period[5,33]. It is these differences, alongside postoperative health outcomes, that require careful consideration from both the surgeon and the patient in clinical practice. Within a patient-centred model of healthcare, which operative intervention is more beneficial in the treatment of knee osteoarthritis will, in part, depend upon the value-system of the patient and the significance that they ascribe to these differences.
Previous studies have identified abnormal knee joint biomechanics as a predictor of radiographic knee osteoarthritis disease progression[34]. There is, however, a paucity of research investigating the relationship between preoperative knee joint alignment and patient-centred health outcomes[35]. Currently available literature shows radiographic parameters of knee joint alignment to demonstrate poor relationships with patient-reported health outcomes[36]. This in keeping with the findings of the current study, in which conventional radiographic parameters of joint alignment (HKA, MAD) did not demonstrate significant correlations with the preoperative PROMs.
Owing to the multifactorial aetiology of knee osteoarthritis, PROM scores almost certainly depend upon the influence of a myriad of co-variates not visible on radiographic imaging, including dynamic joint kinematics and soft tissue chan
The mechanical axis of the lower limb (Mikulicz line) allows ground reaction forces, passing from the ankle to the hip, to be visualised. The physiological angle of Mikulicz line, relative to the vertical axis, corresponds approximately to a 3° distomedial slope. There is, however, little mention of the angle of Mikulicz line in the literature beyond this[37,38]. Mikulicz line is required to calculate MAD and shares joint-centre points with the mechanical axes used to calculate the HKA. These parameters are frequently calculated in clinical practice, whereas the angle of Mikulicz line is not. Given the ease with which this angle can be calculated, and lack of associated literature surrounding it, this study included the angle of the Mikulicz line as an additional, non-conventional, parameter of interest. To our knowledge to date, this is the first study to report a correlation analysis between the angle of Mikulicz line and patient reported health-outcomes of any kind. The results of which demonstrated significant correlations observed across multiple PROMs.
Worse knee function (OKS, KOOS–multiple) and global health-related quality of life (EQ-5D-5L descriptive score) was associated with a wider stance, as represented by a Mikulicz line angled more distolaterally (Table 4). The external knee adduction moment is: A surrogate for medial tibiofemoral contact force during gait[39]; has been associated with pain[40-43], disability[41,42], osteoarthritis severity[44-46] and disease progression[47]; and is the target of many orthopaedic interventions[48-50]. A wider stance has been shown to reduce the external knee adduction moment[39,51]. It is therefore possible that the wider stance, observed within individuals with worse joint function, occurs as a result of a compen
The identification of novel relationships such as these represents an important initial step in the process of further clarifying which factors are causative of poor health outcomes in knee osteoarthritis. Once identified, interventions can then be designed to target and attenuate these factors, thereby facilitating the advancement of patient care. Future rese
The findings of this study are in keeping with those of the wider literature, with virtually no significant correlations being observed between postoperative joint alignment and patient-reported health outcomes following UKA[52,53]. Conflicting evidence from Zuiderbaan et al[4] has, however, associated a residual varus of 1°-4° with optimised joint-function PROM scores following UKA. Other studies have proposed that a postoperative varus of 1°-4° decreases the risk of contralateral compartment degeneration (associated with over-correction) and reduced prosthesis survival time (associated with under-correction): supporting this as a suitable target alignment angle range, irrespective of PROM scores and the obse
This study found greater postoperative HKA and MAD values to exhibit some association with superior knee function following HTO; a finding that is well supported within the current literature[55,56]. These results suggest that a more valgus knee positioning, and further lateral position of the lower limb mechanical axis, may be associated with improved knee function one year following HTO. When considering the clinical utility of this finding it is essential to maintain an awareness of the additional factors, beyond patient-reported outcomes, that are influenced by joint alignment (e.g. knee compartment degeneration). A seminal paper by Hernigou et al[57] concluded that, following HTO, a HKA of 183°-186° provides good functional results whilst simultaneously minimising the risk of lateral compartment degeneration, asso
The mean postoperative HKA of the HTO group was 182.5° (SD ± 2.8°), falling 0.5° short of the lower bound of Her
Hypothesis 3 was partially rejected: The majority of correlations investigated between joint alignment and PROMs were non-significant, however two clusters of significant correlations were observed with respect to PROMS and the angle of Mikulicz line preoperatively; and joint alignment (HKA and MAD) within the HTO group postoperatively.
The current study was subject to some limitations. Firstly, all HTOs and UKAs were undertaken within a single centre, by a single surgeon specialising in knee surgery which may reduce the generalisability of the findings. Despite the relatively small groups of patients (which can increase the susceptibility of type II statistical errors), the number of patients included in each group still exceeded that determined by the power calculation. Furthermore, sufficient power was achieved to allow for the identification of numerous statistically significant findings. Sample sizes were restricted by the cancellation of routine clinic appointments and cessation of elective surgery during the COVID-19 pandemic. Thirdly, some demographic differences were noted between the two groups, namely age and gender distribution. Despite this, the only PROM score to demonstrate a significant between-group difference at baseline (preoperatively) was the SF-12 mental component score, thus assuring the inter-group comparability with respect to the remaining PROMs.
This study demonstrated that UKAs and HTOs are both efficacious operative interventions capable of providing signi
This study appears to be the first to examine the relationship between the angle of the Mikulicz line and health outcomes. Postoperatively, joint alignment parameters exhibited little association with PROMs within the UKA group, yet an increased HKA/MAD exhibited some association with superior joint function at one year post-HTO. Preoperatively, traditional measures of joint alignment (HKA, MAD) demonstrated little correlation with PROMs. However, a more distolaterally angled Mikulicz line was observed to be associated with worse knee function and overall health-related quality of life preoperatively. Future research should seek to assess the reproducibility of this finding and aim to characterise/better understand the mechanisms behind this relationship.
| 1. | Hunter DJ, March L, Chew M. Osteoarthritis in 2020 and beyond: a Lancet Commission. Lancet. 2020;396:1711-1712. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 192] [Cited by in RCA: 583] [Article Influence: 97.2] [Reference Citation Analysis (0)] |
| 2. | Cui A, Li H, Wang D, Zhong J, Chen Y, Lu H. Global, regional prevalence, incidence and risk factors of knee osteoarthritis in population-based studies. EClinicalMedicine. 2020;29-30:100587. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 351] [Cited by in RCA: 855] [Article Influence: 142.5] [Reference Citation Analysis (0)] |
| 3. | Wang WJ, Sun MH, Palmer J, Liu F, Bottomley N, Jackson W, Qiu Y, Weng WJ, Price A. Patterns of Compartment Involvement in End-stage Knee Osteoarthritis in a Chinese Orthopedic Center: Implications for Implant Choice. Orthop Surg. 2018;10:227-234. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 23] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 4. | Zuiderbaan HA, van der List JP, Kleeblad LJ, Appelboom P, Kort NP, Pearle AD, Rademakers MV. Modern Indications, Results, and Global Trends in the Use of Unicompartmental Knee Arthroplasty and High Tibial Osteotomy in the Treatment of Isolated Medial Compartment Osteoarthritis. Am J Orthop (Belle Mead NJ). 2016;45:E355-E361. [PubMed] |
| 5. | Santoso MB, Wu L. Unicompartmental knee arthroplasty, is it superior to high tibial osteotomy in treating unicompartmental osteoarthritis? A meta-analysis and systemic review. J Orthop Surg Res. 2017;12:50. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 89] [Cited by in RCA: 95] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 6. | Cao Z, Mai X, Wang J, Feng E, Huang Y. Unicompartmental Knee Arthroplasty vs High Tibial Osteotomy for Knee Osteoarthritis: A Systematic Review and Meta-Analysis. J Arthroplasty. 2018;33:952-959. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 119] [Article Influence: 14.9] [Reference Citation Analysis (0)] |
| 7. | Ryu SM, Park JW, Na HD, Shon OJ. High Tibial Osteotomy versus Unicompartmental Knee Arthroplasty for Medial Compartment Arthrosis with Kissing Lesions in Relatively Young Patients. Knee Surg Relat Res. 2018;30:17-22. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 42] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 8. | Dettoni F, Bonasia DE, Castoldi F, Bruzzone M, Blonna D, Rossi R. High tibial osteotomy versus unicompartmental knee arthroplasty for medial compartment arthrosis of the knee: a review of the literature. Iowa Orthop J. 2010;30:131-140. [PubMed] |
| 9. | Koh IJ, Kim MS, Sohn S, Song KY, Choi NY, Jung H, In Y. Predictive factors for satisfaction after contemporary unicompartmental knee arthroplasty and high tibial osteotomy in isolated medial femorotibial osteoarthritis. Orthop Traumatol Surg Res. 2019;105:77-83. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 43] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 10. | Miniaci A, Ballmer FT, Ballmer PM, Jakob RP. Proximal tibial osteotomy. A new fixation device. Clin Orthop Relat Res. 1989;(246):250-259. [PubMed] |
| 11. | OrthotoolKit. Free online SF-12 score calculator 2024. Available from: https://orthotoolkit.com/sf-12/. |
| 12. | Ware J Jr, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220-233. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11319] [Cited by in RCA: 13221] [Article Influence: 440.7] [Reference Citation Analysis (0)] |
| 13. | EuroQol Research Foundation. EQ-5D-5L User Guide 2019. Available from: https://euroqol.org/publications/user-guides. |
| 14. | Roos EM. 30 years with the Knee injury and Osteoarthritis Outcome Score (KOOS). Osteoarthritis Cartilage. 2024;32:421-429. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 36] [Article Influence: 18.0] [Reference Citation Analysis (0)] |
| 15. | Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD. Knee Injury and Osteoarthritis Outcome Score (KOOS)--development of a self-administered outcome measure. J Orthop Sports Phys Ther. 1998;28:88-96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2362] [Cited by in RCA: 2967] [Article Influence: 106.0] [Reference Citation Analysis (0)] |
| 16. | Murray DW, Fitzpatrick R, Rogers K, Pandit H, Beard DJ, Carr AJ, Dawson J. The use of the Oxford hip and knee scores. J Bone Joint Surg Br. 2007;89:1010-1014. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 793] [Cited by in RCA: 1143] [Article Influence: 60.2] [Reference Citation Analysis (0)] |
| 17. | Dawson J, Fitzpatrick R, Murray D, Carr A. Questionnaire on the perceptions of patients about total knee replacement. J Bone Joint Surg Br. 1998;80:63-69. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 655] [Cited by in RCA: 942] [Article Influence: 33.6] [Reference Citation Analysis (0)] |
| 18. | Sangha O, Stucki G, Liang MH, Fossel AH, Katz JN. The Self-Administered Comorbidity Questionnaire: a new method to assess comorbidity for clinical and health services research. Arthritis Rheum. 2003;49:156-163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1207] [Cited by in RCA: 1499] [Article Influence: 65.2] [Reference Citation Analysis (0)] |
| 19. | KELLGREN JH, LAWRENCE JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16:494-502. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9311] [Cited by in RCA: 9213] [Article Influence: 133.5] [Reference Citation Analysis (0)] |
| 20. | Paley D, Pfeil J. [Principles of deformity correction around the knee]. Orthopade. 2000;29:18-38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 105] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 21. | Sheehy L, Felson D, Zhang Y, Niu J, Lam YM, Segal N, Lynch J, Cooke TD. Does measurement of the anatomic axis consistently predict hip-knee-ankle angle (HKA) for knee alignment studies in osteoarthritis? Analysis of long limb radiographs from the multicenter osteoarthritis (MOST) study. Osteoarthritis Cartilage. 2011;19:58-64. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 91] [Cited by in RCA: 96] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 22. | Iseki Y, Takahashi T, Takeda H, Tsuboi I, Imai H, Mashima N, Watanabe S, Yamamoto H. Defining the load bearing axis of the lower extremity obtained from anterior-posterior digital radiographs of the whole limb in stance. Osteoarthritis Cartilage. 2009;17:586-591. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 40] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 23. | Jeon YS, Ahn CH, Kim MK. Comparison of HTO with articular cartilage surgery and UKA in unicompartmental OA. J Orthop Surg (Hong Kong). 2017;25:2309499016684092. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 22] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 24. | Chan YH. Biostatistics 104: correlational analysis. Singapore Med J. 2003;44:614-619. [PubMed] |
| 25. | Patel S, Haunschild E, Gilat R, Knapik D, Evuarherhe AJ, Parvaresh KC, Chahla J, Yanke AB, Cole BJ. Defining clinically significant outcomes following high tibial osteotomy with or without concomitant procedures. JCJP. 2021;1:100014. [DOI] [Full Text] |
| 26. | Goh GS, Liow MHL, Chen JY, Tay DK, Lo NN, Yeo SJ. The patient acceptable symptom state for the knee society score, oxford knee score and short form-36 following unicompartmental knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2023;31:1113-1122. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 14] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 27. | Jacquet C, Gulagaci F, Schmidt A, Pendse A, Parratte S, Argenson JN, Ollivier M. Opening wedge high tibial osteotomy allows better outcomes than unicompartmental knee arthroplasty in patients expecting to return to impact sports. Knee Surg Sports Traumatol Arthrosc. 2020;28:3849-3857. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 49] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 28. | Yim JH, Song EK, Seo HY, Kim MS, Seon JK. Comparison of high tibial osteotomy and unicompartmental knee arthroplasty at a minimum follow-up of 3 years. J Arthroplasty. 2013;28:243-247. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 51] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 29. | Krych AJ, Reardon P, Sousa P, Pareek A, Stuart M, Pagnano M. Unicompartmental Knee Arthroplasty Provides Higher Activity and Durability Than Valgus-Producing Proximal Tibial Osteotomy at 5 to 7 Years. J Bone Joint Surg Am. 2017;99:113-122. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 42] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 30. | Ivarsson I, Gillquist J. Rehabilitation after high tibial osteotomy and unicompartmental arthroplasty. A comparative study. Clin Orthop Relat Res. 1991;(266):139-144. [PubMed] |
| 31. | Yokoyama M, Nakamura Y, Onishi T, Hirano K, Doi M. Healing period after open high tibial osteotomy and related factors: Can we really say that it is long? Springerplus. 2016;5:123. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 23] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 32. | W-Dahl A, Robertsson O, Lidgren L. Surgery for knee osteoarthritis in younger patients. Acta Orthop. 2010;81:161-164. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 128] [Cited by in RCA: 131] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 33. | Tuncay İ, Bilsel K, Elmadağ M, Erkoçak ÖF, Aşçı M, Şen C. Evaluation of mobile bearing unicompartmental knee arthroplasty, opening wedge, and dome-type high tibial osteotomies for knee arthritis. Acta Orthop Traumatol Turc. 2015;49:280-287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 34. | Tanamas S, Hanna FS, Cicuttini FM, Wluka AE, Berry P, Urquhart DM. Does knee malalignment increase the risk of development and progression of knee osteoarthritis? A systematic review. Arthritis Rheum. 2009;61:459-467. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 217] [Cited by in RCA: 229] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 35. | Sharma L, Song J, Felson DT, Cahue S, Shamiyeh E, Dunlop DD. The role of knee alignment in disease progression and functional decline in knee osteoarthritis. JAMA. 2001;286:188-195. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 989] [Cited by in RCA: 1076] [Article Influence: 43.0] [Reference Citation Analysis (0)] |
| 36. | Maly MR, Costigan PA, Olney SJ. Mechanical factors relate to pain in knee osteoarthritis. Clin Biomech (Bristol, Avon). 2008;23:796-805. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 57] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 37. | Cherian JJ, Kapadia BH, Banerjee S, Jauregui JJ, Issa K, Mont MA. Mechanical, Anatomical, and Kinematic Axis in TKA: Concepts and Practical Applications. Curr Rev Musculoskelet Med. 2014;7:89-95. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 141] [Cited by in RCA: 189] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 38. | Marques Luís N, Varatojo R. Radiological assessment of lower limb alignment. EFORT Open Rev. 2021;6:487-494. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 104] [Article Influence: 20.8] [Reference Citation Analysis (0)] |
| 39. | Bowd J, Biggs P, Holt C, Whatling G. Does Gait Retraining Have the Potential to Reduce Medial Compartmental Loading in Individuals With Knee Osteoarthritis While Not Adversely Affecting the Other Lower Limb Joints? A Systematic Review. Arch Rehabil Res Clin Transl. 2019;1:100022. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 40. | Amin S, Luepongsak N, McGibbon CA, LaValley MP, Krebs DE, Felson DT. Knee adduction moment and development of chronic knee pain in elders. Arthritis Rheum. 2004;51:371-376. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 175] [Cited by in RCA: 192] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 41. | Kim WY, Richards J, Jones RK, Hegab A. A new biomechanical model for the functional assessment of knee osteoarthritis. Knee. 2004;11:225-231. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 36] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 42. | Kito N, Shinkoda K, Yamasaki T, Kanemura N, Anan M, Okanishi N, Ozawa J, Moriyama H. Contribution of knee adduction moment impulse to pain and disability in Japanese women with medial knee osteoarthritis. Clin Biomech (Bristol, Avon). 2010;25:914-919. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 80] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 43. | Robbins SM, Birmingham TB, Callaghan JP, Jones GR, Chesworth BM, Maly MR. Association of pain with frequency and magnitude of knee loading in knee osteoarthritis. Arthritis Care Res (Hoboken). 2011;63:991-997. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 38] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 44. | Henriksen M, Graven-Nielsen T, Aaboe J, Andriacchi TP, Bliddal H. Gait changes in patients with knee osteoarthritis are replicated by experimental knee pain. Arthritis Care Res (Hoboken). 2010;62:501-509. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 129] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 45. | Mündermann A, Dyrby CO, Hurwitz DE, Sharma L, Andriacchi TP. Potential strategies to reduce medial compartment loading in patients with knee osteoarthritis of varying severity: reduced walking speed. Arthritis Rheum. 2004;50:1172-1178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 313] [Cited by in RCA: 323] [Article Influence: 14.7] [Reference Citation Analysis (0)] |
| 46. | Mündermann A, Dyrby CO, Andriacchi TP. Secondary gait changes in patients with medial compartment knee osteoarthritis: increased load at the ankle, knee, and hip during walking. Arthritis Rheum. 2005;52:2835-2844. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 471] [Cited by in RCA: 508] [Article Influence: 24.2] [Reference Citation Analysis (0)] |
| 47. | Jackson BD, Teichtahl AJ, Morris ME, Wluka AE, Davis SR, Cicuttini FM. The effect of the knee adduction moment on tibial cartilage volume and bone size in healthy women. Rheumatology (Oxford). 2004;43:311-314. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 63] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 48. | Bennell KL, Kyriakides M, Metcalf B, Egerton T, Wrigley TV, Hodges PW, Hunt MA, Roos EM, Forbes A, Ageberg E, Hinman RS. Neuromuscular versus quadriceps strengthening exercise in patients with medial knee osteoarthritis and varus malalignment: a randomized controlled trial. Arthritis Rheumatol. 2014;66:950-959. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 147] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 49. | Hinman RS, Wrigley TV, Metcalf BR, Hunter DJ, Campbell P, Paterson K, Staples MP, Bennell KL. Unloading shoes for osteoarthritis of the knee: protocol for the SHARK randomised controlled trial. BMC Musculoskelet Disord. 2014;15:48. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 20] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 50. | Moyer RF, Birmingham TB, Bryant DM, Giffin JR, Marriott KA, Leitch KM. Biomechanical effects of valgus knee bracing: a systematic review and meta-analysis. Osteoarthritis Cartilage. 2015;23:178-188. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 84] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 51. | Reinbolt JA, Haftka RT, Chmielewski TL, Fregly BJ. A computational framework to predict post-treatment outcome for gait-related disorders. Med Eng Phys. 2008;30:434-443. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 46] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 52. | Rodríguez-Merchán EC, Gómez-Cardero P. Unicompartmental knee arthroplasty: Current indications, technical issues and results. EFORT Open Rev. 2018;3:363-373. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 40] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 53. | Petterson SC, Blood TD, Plancher KD. Role of alignment in successful clinical outcomes following medial unicompartmental knee arthroplasty: current concepts. J ISAKOS. 2020;5:224-228. [RCA] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 25] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 54. | Kim TK, Mittal A, Meshram P, Kim WH, Choi SM. Evidence-based surgical technique for medial unicompartmental knee arthroplasty. Knee Surg Relat Res. 2021;33:2. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 22] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 55. | Yadav AK, Parihar M, Pawar ED, Ahuja D, Gavhale S, Khanna V. Functional Outcome of High Tibial Osteotomy in Patients with Medial Compartment Osteoarthritis Using Dynamic Axial Fixator -a prospective study. J Clin Orthop Trauma. 2020;11:S902-S908. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 56. | Tawy G, Shahbaz H, McNicholas M, Biant L. The Relationships between Coronal Plane Alignments and Patient-Reported Outcomes Following High Tibial Osteotomy: A Systematic Review. Cartilage. 2021;13:132S-146S. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 57. | Hernigou P, Medevielle D, Debeyre J, Goutallier D. Proximal tibial osteotomy for osteoarthritis with varus deformity. A ten to thirteen-year follow-up study. J Bone Joint Surg Am. 1987;69:332-354. [PubMed] |
| 58. | Yin Y, Li S, Zhang R, Guo J, Hou Z, Zhang Y. What is the relationship between the "Fujisawa point" and postoperative knee valgus angle? A theoretical, computer-based study. Knee. 2020;27:183-191. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 24] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 59. | Petersen W, Metzlaff S. Open wedge high tibial osteotomy (HTO) versus mobile bearing unicondylar medial joint replacement: five years results. Arch Orthop Trauma Surg. 2016;136:983-989. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 55] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/licenses/by-nc/4.0/
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country of origin: United Kingdom
Peer-review report’s classification
Scientific Quality: Grade A, Grade B
Novelty: Grade A, Grade C
Creativity or Innovation: Grade B, Grade B
Scientific Significance: Grade B, Grade C
P-Reviewer: DeSousa K, India; Yan ZQ, China S-Editor: Che XX L-Editor: A P-Editor: Zhao YQ