Published online May 18, 2024. doi: 10.5312/wjo.v15.i5.435
Revised: April 6, 2024
Accepted: April 16, 2024
Published online: May 18, 2024
Processing time: 160 Days and 14.2 Hours
Primary thumb carpometacarpal (CMC) osteoarthritis is one of the most common conditions encountered by hand surgeons. Of the vast number of operations that have been proposed, none have demonstrated results significantly superior to tra
The purpose of our study was to determine why surgeons opt for their technique in treating CMC arthritis.
A cross-sectional survey of active members of the American Society for Surgery of the Hand was conducted to evaluate the reasons behind their preferred technique in the treatment of isolated thumb CMC arthritis. Surgeons were contacted by e-mail once and provided with a link to a de-identified survey consisting of 5 trea
Of 950 responses were received. 40.5% of surgeons preferred trapeziectomy + ligament reconstruction tendon interposition (LRTI), followed by trapeziectomy + suspensionplasty (28.2%), suture button suspension (5.9 %), trapeziectomy alone (4.6%), prosthetic arthroplasty (3.2%), arthrodesis (1.1%), and other (6.6%). Proponents of trapeziectomy + LRTI cited familiarity (73.2%), exposure during fellowship (48.8%) and less proximal migration (60%) to be the main reasons affecting their decision. Surgeons who preferred trapeziectomy + suspensionplasty most reported simplicity (74.9%), fewer complications (45.3%), less proximal migration (43.8%), and avoidance of autogenous tissue harvest (42.7%). Advocates of suture button suspension cited avoidance of autogenous tissue harvest (80.4%), shorter immobilization (76.8%), and quicker recovery (73.2%) with their technique. Advocates of trapeziectomy alone cited simplicity (97.7%), fewer complications (86.4%), and avoidance of autogenous tissue harvest (59.1%). In their comments, 45% of surgeons choosing trapeziectomy alone cited evidence as an additional rationale. Advocates of prosthetic arthroplasty cited improved pinch strength (83.3%) and improved range of motion (63.3%), while those preferring arthrodesis cited better pinch strength (90%) and frequently in their comments, durability. Of the surgeons who preferred a technique other than LRTI, 41.8% reported they had tried LRTI in the past, citing complexity of the procedure, flexor carpi radialis harvest, and longer operative time as reasons for moving on.
Our study provides an update on current treatment trends and offers new insight into the reasons behind sur
Core Tip: Despite strong evidence from level 1 prospective randomized studies that trapeziectomy alone is sufficient for the treatment of basilar thumb osteoarthritis, surgeons continue to perform more complicated operations with more complications. After surveying 950 fellowship trained hand surgeons, it seems that the majority are still performing trapeziectomy with ligament tendon interposition arthroplasty or suspensionplasty relying more on their level 4 clinical expertise and personal observations.
- Citation: Wu EJ, Fossum BW, Voort WV, Bayne CO, Szabo RM. Surgeon preferences in the treatment of thumb carpometacarpal osteoarthritis. World J Orthop 2024; 15(5): 435-443
- URL: https://www.wjgnet.com/2218-5836/full/v15/i5/435.htm
- DOI: https://dx.doi.org/10.5312/wjo.v15.i5.435
Primary thumb carpometacarpal (CMC) osteoarthritis is the second most common site of arthritis in the hand, and the most common site of surgical reconstruction for osteoarthritis in the upper extremity[1]. It is present in 25% of men and 40% of women over the age of 75[1]. When non-operative modalities such as non-steroidal anti-inflammatory medication, activity modification, splinting, and injections fail to provide adequate relief, surgical intervention is often indicated[2].
First described in 1947 by Gervis, resection of the trapezium has remained the gold standard surgical option for management of Eaton stages II-IV CMC arthritis [3,4]. However, many variations and modifications to this procedure have since been introduced, suggesting that the optimal procedure for this condition has yet to be agreed upon[5]. Currently, hand surgeons across the United States are routinely performing procedures ranging from implant arthroplasty, arthrodesis, and trapeziectomy with or without volar ligament reconstruction, suture suspension, interposition of native or artificial soft tissue, or a combination thereof[1].
Prior randomized studies have demonstrated no statistically significant difference between trapeziectomy alone and trapeziectomy plus ligament reconstruction tendon interposition (LRTI) in pain relief, pinch strength, and patient reported outcome scores[6,7]. Multiple review studies have demonstrated similar findings. Martou et al[8] performed a systematic review of 18 comparative studies and found no single procedure to be superior. They also reported 16% fewer adverse events in trapeziectomy alone and 11% more adverse events in trapeziectomy with LRTI compared to other commonly performed procedures. Shuler et al[9] accurately summarized current knowledge on the topic, stating that although prior studies “exhibit limitations in regard to validated outcomes, power analysis, and blinded assessment, their conclusions question the clinical benefits of ligament reconstruction and tendon interposition.”
Despite current evidence, most hand surgeons in the United States still prefer trapeziectomy with LRTI for surgical management of CMC arthritis. The most recent surveys in 2010 and 2012 reported that 62% to 68% of surgeons perform trapeziectomy with LRTI for Eaton Stage III-IV basilar thumb arthritis[5,10]. These studies also reported that only 2% and 3% of respondents perform trapeziectomy alone, despite the current consensus in the literature that the addition of LRTI provides no substantial benefit to the patient. While descriptive, these studies did not offer insight into the reasons behind surgeons’ decision making. Given this treatment equipoise, we sought to determine if treatment trends have changed and to understand the reasons why surgeons opt for one technique versus another.
This cross-sectional survey study, utilizing a 10-question researcher-administered online questionnaire entitled “Thumb CMC Arthroplasty Preferences”, was developed through a professional online service to ensure confidentiality and anonymity. This de-identified questionnaire was sent to active members of the American Society for Surgery of the Hand via electronic mail. Retired, international, and candidate members were included, while respondents in residency were excluded. Only one email was sent to each member, and no follow-up or reminder emails were sent. The survey was ad
Demographic information, including primary and specialty training, years in practice, number of procedures per
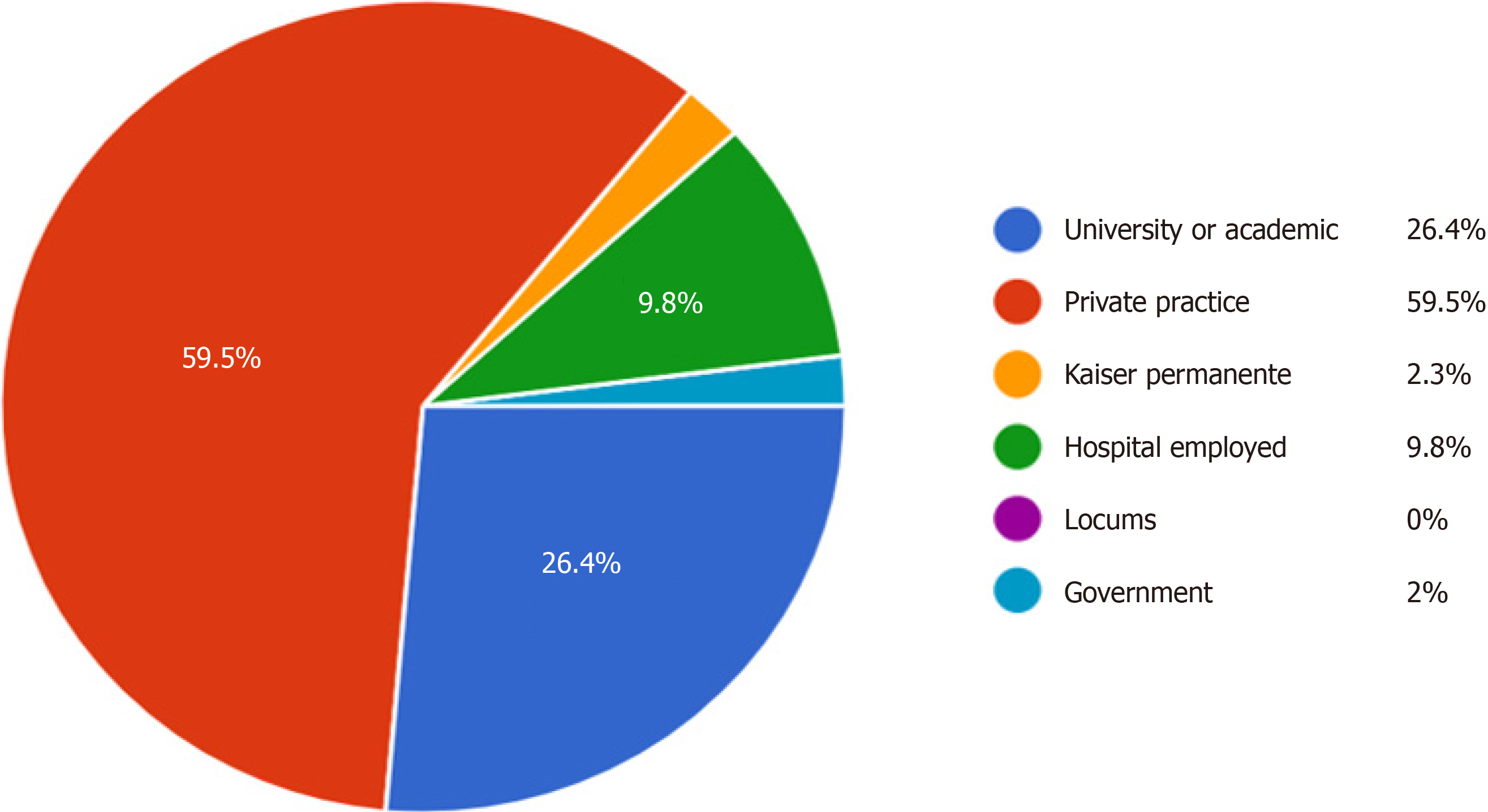
The survey was sent to a total of 4831 recipients. 950 responses were received for a total response rate of 19.7%. 795 (83.7%) of respondents were orthopedic surgeons, 121 (12.7%) were plastic surgeons, and 34 (3.6%) were general surgeons. 929 (97.8%) of these surgeons were fellowship trained in hand surgery. Most survey respondents were employed in a private practice setting (59.5%), 26.4% were employed in a university or academic setting, 9.8% were hospital employed, 2.3% were employed by Kaiser Permanente, and 2% were employed by the government (Figure 1).
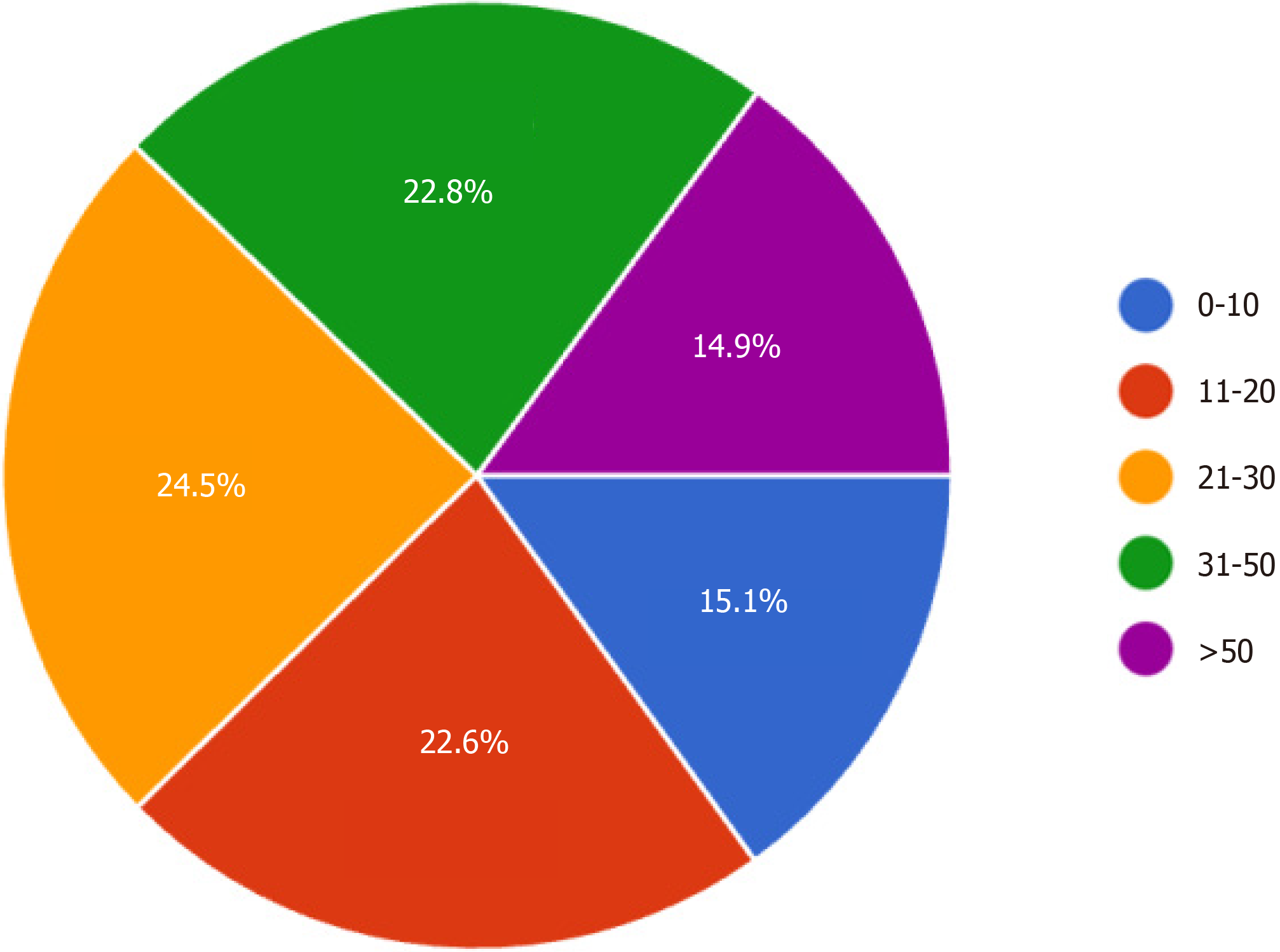
30.8% of survey respondents were in their first 10 years of practice, 21.1% had been in practice between 11 to 20 years, 28.1% had been in practice between 21 to 30 years, and 20% had greater than 30 years of experience. 14.9% reported performing greater than 50 thumb CMC arthroplasties per year, 22.8% performed 31-50 per year, 24.5% performed 21-30 annually, 22.6% performed 11-20 annually, and 15.1% surgeons performed 10 or fewer of these procedures per year (Figure 2).
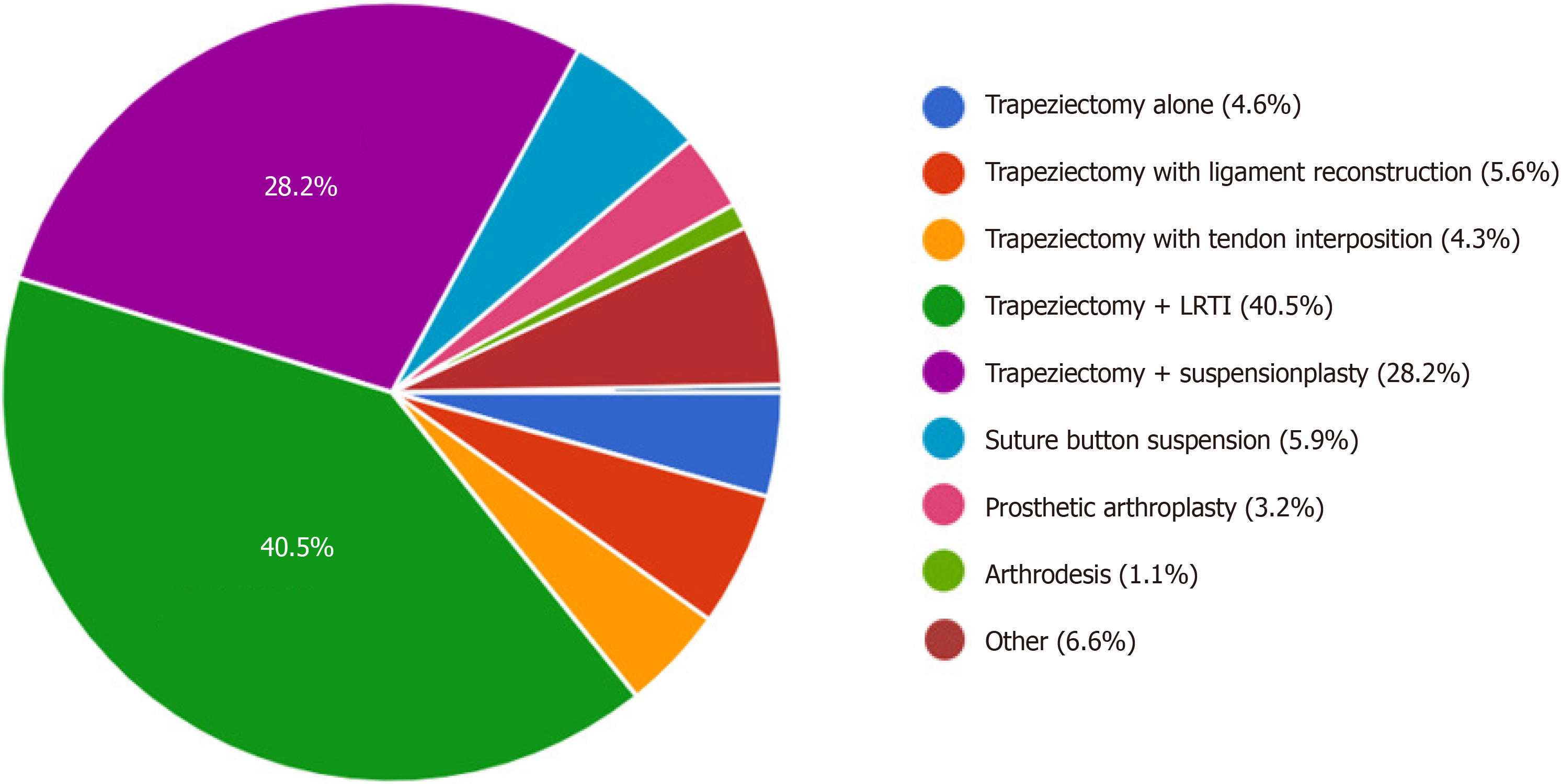
The distribution of surgeons’ preferred techniques is represented in Figure 3. Trapeziectomy + LRTI (385 responses, 40.5%) and trapeziectomy + suspensionplasty (268 responses, 28.2%) were the two most popular techniques, comprising over two-thirds (68.7%) of survey respondents. This was followed by suture button suspension (56 responses, 5.9%), and trapeziectomy with ligament reconstruction (53 responses, 5.6%), trapeziectomy with tendon interposition (41 responses 4.3%), trapeziectomy alone (44 responses, 4.6%), prosthetic arthroplasty (30 responses, 3.2%), and arthrodesis (10 responses, 1.1%). There were 63 respondents (6.6%) in the survey who selected other. They were provided the opportunity to elaborate on their techniques in free text responses, which included suspensionplasty variations using the extensor carpi radialis longus or palmaris longus tendons, arthroscopic hemi-trapeziectomy with suture button sus
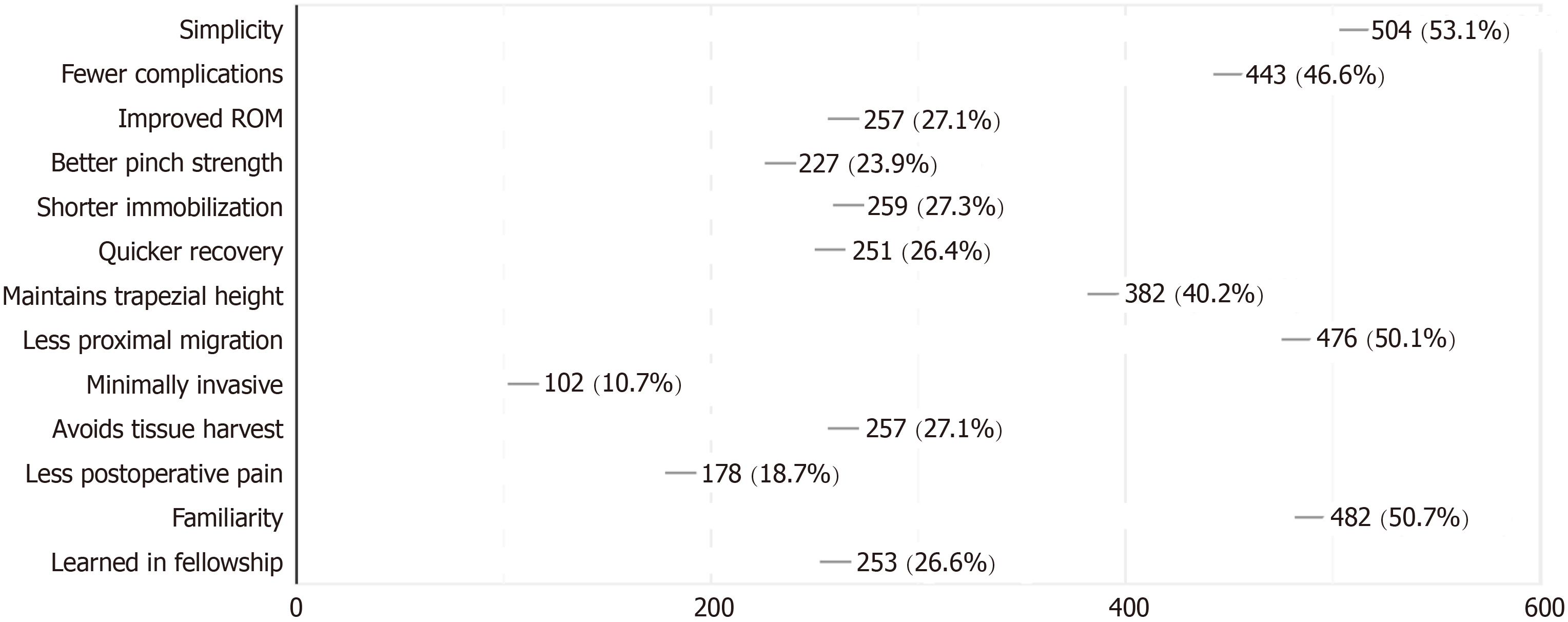
Reasons why surgeons preferred their technique and the overall percentage of respondents selecting each reason are provided in Figure 4. Simplicity (53.1%) and familiarity (50.7%) were the two most common reasons provided. 50.1% of surgeons believed that their technique provided less proximal migration of the thumb metacarpal, and 40.2% believed it maintained trapezial height. 46.6% of respondents believed that their technique was associated with fewer complications. 26.6% of respondents reported that they used their preferred technique because they learned it during their fellowship training.
A sub-analysis of each individual technique was performed. The most common reasons provided by surgeons who performed trapeziectomy + LRTI were familiarity (73.2%), exposure during fellowship (48.8%), and less proximal migration (60%). Surgeons who preferred trapeziectomy + suspensionplasty reported simplicity (74.9%), fewer complications (45.3%), less proximal migration (43.8%), and avoidance of autogenous tissue harvest (42.7%) as reasons they used this technique. Advocates of suture button suspension cited avoidance of autogenous tissue harvest (80.4%), shorter immobilization (76.8%), and quicker recovery (73.2%) with their technique. Respondents who performed trapeziectomy alone noted simplicity (97.7%), fewer complications (86.4%), and avoidance of autogenous tissue harvest (59.1%). In their comments, 45% of these surgeons cited evidence as an additional rationale. Surgeons who performed prosthetic arthroplasty cited improved pinch strength (83.3%) and improved range of motion (63.3%), while those preferring arthrodesis cited preservation of pinch strength (90%) and durability in the additional comments section. Of the surgeons who preferred a technique other than LRTI, 41.8% reported they had tried LRTI in the past, citing complexity of the procedure, flexor carpi radialis harvest, and longer operative time as reasons for no longer performing this procedure.
We further analyzed the data to determine if practice setting, specialty training, years in practice, or number of CMC arthroplasties performed per year had any influence on technique choice (Tables 1-4). Trapeziectomy + LRTI was the most frequently performed technique across specialties and practice settings, followed by trapeziectomy + suspensionplasty. Our findings demonstrate a higher tendency for younger surgeons in their first ten years of practice to perform suspensionplasty (42.1%). However, trapeziectomy + LRTI remains the most popular technique among surgeons in their second or third decade of practice. The number of surgeons in their third decade of practice performing LRTI greatly outnumbered those performing suspensionplasty (47.1% vs 17.9%, respectively). Our findings also demonstrate a positive correlation between case volume and preference for LRTI. Among surgeons performing > 50 CMC arthroplasties annually, 49.3% preferred LRTI, compared to just 31.3% of surgeons who performed 11-20 cases per year. Likewise, a negative correlation was seen between case volume and preference for suspensionplasty. Among surgeons performing > 50 CMC arthroplasties annually, only 21.8% preferred suspensionplasty, compared to 31.3% of surgeons who performed 11-20 cases per year.
| Academic | Private practice | Hospital employed | Kaiser permanente | Gov | |
| Trapeziectomy + LRTI | 34.0 | 43.5 | 40.7 | 35.0 | 42.1 |
| Trapeziectomy + suspensionplasty | 30.8 | 26.1 | 35.2 | 35.0 | 26.3 |
| Trapeziectomy + TI | 5.3 | 4.8 | 1.1 | 0.0 | 0.0 |
| Trapeziectomy + LR | 6.1 | 5.5 | 3.3 | 10.0 | 0.0 |
| Trapeziectomy (alone) | 5.3 | 3.7 | 5.5 | 5.0 | 5.3 |
| Suture button suspension | 5.7 | 5.3 | 8.8 | 10.0 | 10.5 |
| Prosthetic arthroplasty | 3.2 | 3.6 | 2.2 | 0.0 | 0.0 |
| Arthrodesis | 0.8 | 1.1 | 2.2 | 0.0 | 0.0 |
| Other | 8.9 | 6.4 | 1.1 | 5.0 | 15.8 |
| Orthopaedic surgery | Plastic surgery | General surgery | |
| Trapeziectomy + LRTI | 41.0 | 37.8 | 38.2 |
| Trapeziectomy + suspensionplasty | 28.6 | 30.3 | 17.6 |
| Trapeziectomy + TI | 3.6 | 6.7 | 14.7 |
| Trapeziectomy + LR | 5.3 | 5.9 | 5.9 |
| Trapeziectomy (alone) | 3.7 | 6.7 | 11.8 |
| Suture button suspension | 6.5 | 3.4 | 2.9 |
| Prosthetic arthroplasty | 3.0 | 3.4 | 5.9 |
| Arthrodesis | 1.0 | 1.7 | 0.0 |
| Other | 7.2 | 4.2 | 2.9 |
| 0-10 yr | 11-20 yr | 21-30 yr | > 30 yr | |
| Trapeziectomy + LRTI | 39.3 | 38.4 | 47.1 | 35.4 |
| Trapeziectomy + suspensionplasty | 42.1 | 27.3 | 17.9 | 23.3 |
| Trapeziectomy + TI | 3.1 | 3.0 | 3.8 | 8.5 |
| Trapeziectomy + LR | 2.8 | 5.1 | 7.2 | 7.4 |
| Trapeziectomy (alone) | 2.1 | 7.1 | 3.8 | 5.8 |
| Suture button suspension | 5.2 | 8.1 | 6.8 | 3.7 |
| Prosthetic arthroplasty | 1.7 | 5.1 | 3.0 | 3.7 |
| Arthrodesis | 0.3 | 0.5 | 0.8 | 3.2 |
| Other | 3.4 | 5.6 | 9.5 | 9.0 |
| 0-10 cases | 11-20 cases | 21-30 cases | 31-50 cases | > 50 cases | |
| Trapeziectomy + LRTI | 34.3 | 31.3 | 41.2 | 47.2 | 49.3 |
| Trapeziectomy + suspensionplasty | 30.0 | 31.3 | 28.5 | 28.7 | 21.8 |
| Trapeziectomy + TI | 5.7 | 4.2 | 4.4 | 3.7 | 4.2 |
| Trapeziectomy + LR | 5.0 | 6.5 | 5.3 | 4.2 | 6.3 |
| Trapeziectomy (alone) | 10.0 | 6.5 | 2.6 | 1.9 | 2.1 |
| Suture button suspension | 5.0 | 4.7 | 9.2 | 4.2 | 6.3 |
| Prosthetic arthroplasty | 2.1 | 4.7 | 2.6 | 3.7 | 2.1 |
| Arthrodesis | 2.1 | 2.3 | 0.4 | 0.0 | 0.7 |
| Other | 5.7 | 8.4 | 5.7 | 6.5 | 7.0 |
Since Gervis first introduced trapeziectomy for the treatment of thumb CMC osteoarthritis, many modifications and additions to this procedure have been described in attempts to augment its effectiveness[3,11-13]. Despite the purported advantages of these ancillary procedures, studies have repeatedly shown that they provide no significant benefit in various patient outcomes compared to trapeziectomy alone[6-8,11,12,14]. Furthermore, the Cochrane group found that patients who had just a trapeziectomy had fewer complications, whereas those who received LRTI developed more complications, including tendon adhesion or ruptures, scar tenderness, sensory disturbances, or complex regional pain syndrome[12].
Despite this strong evidence supporting trapeziectomy as a standalone procedure, our study indicates that hand surgeons continue to supplement it with additional soft tissue stabilizing techniques. Over two thirds of survey res
This apparent dichotomy between what the evidence suggests as best practice and what surgeons actually do highlight the complexities of applying evidence-based medicine (EBM). EBM is defined by three main components; current evidence-based best practice, the clinical expertise of the physician, and the values of the patient and their individual situation[15]. Our study reveals that other factors besides evidence continue to influence practice patterns with regards to the surgical management of thumb CMC osteoarthritis. Surgeons who preferred LRTI cited familiarity, less proximal migration, and exposure during fellowship as the main reasons behind their choice. Surgeons who preferred suspensionplasty felt that it was the simpler option with fewer complications, avoiding autogenous tissue harvest while also preve
Surgical treatment of thumb CMC osteoarthritis is but one example in medicine where strong evidence has failed to unify consensus on treatment. Our findings highlight several challenges against the application of evidence in daily practice. The current surgical training structure is largely based on the apprenticeship model. Indeed, familiarity and exposure during fellowship were two main reasons provided by survey respondents who used LRTI. Furthermore, because of the extensive training and experience required to develop surgical mastery, individual surgeons tend to treat specific problems with a single technique or approach. From a practical standpoint, implementing a new approach requires a significant change in professional behavior[19]. It is therefore not surprising that surgeons are reluctant to abandon a technique that “works in my hands,” especially when there is equipoise among the alternative options.
Whether or not we like to admit, surgical culture emphasizes the individualism of surgeons, and the “valorization” of clinical experience, autonomy, and authority of the individual surgeon often takes precedence over objective scientific evaluation of surgical practice[20]. Studies evaluating surgeons’ attitudes towards EBM revealed that surgeons have high confidence in their own judgment compared to low confidence in clinical practice guidelines[21]. While the results of the survey indicate that surgeons believe EBM-generated knowledge is useful, they did not feel that not using EBM adversely affected their daily practice. Another survey by the American Orthopaedic Association revealed that while 94% of respondents utilized EBM in their decision-making, only 18% believed randomized controlled trials could adequately answer most clinical questions. Two-thirds believed that evidence relevant to their clinical practice was lacking and the majority of respondents cited personal experience as the most influential in guiding their clinical decision-making, above randomized controlled trials, case-control studies, case series, and expert opinion[22].
Previous level 1 comparative studies for the surgical treatment of thumb CMC osteoarthritis are lacking in follow-up greater than a year, which could be one reason that surgeons remain convinced of the long-term benefit of other techniques to supplement trapeziectomy[23]. Even the Cochrane review suggested that the current research may be of limited quality and noted that further research may change recommendations in the future[12]. Robinson et al[24] described the limitations of generalizing results of randomized controlled trials to large populations. While a positive result in a pragmatic trial can indicate that a procedure is clinically effective, a negative result does not necessarily mean that a procedure is ineffective. Rather it may imply that the treatment works in some circumstances or subgroups and not others. Another independent study analyzed the quality of randomized controlled trials in orthopaedic journals and found that the sought-after level 1 evidence rating does not always imply high quality of reporting, and recommended that each paper’s methodological safeguards be assessed individually[25]. Therefore, when the critical appraisal of the literature indicates that all current techniques result in similarly good outcomes, the other two aspects of EBM, clinical experience and patient values, become much more important in the treatment decision. The objective of EBM is not standardization, but the assurance of optimal patient care. It also is not mechanistically applying trial results as an overall directive in patient care, nor is it the slavish adherence to guidelines. Medicine is and will remain an imperfect science, and individual surgeon skill and technical mastery cannot be discounted. In the absence of studies showing obvious superiority of a particular intervention, alternative practices such as LRTI and suspensionplasty should not be designated “evidence opposed.”
As illustrated in the surgical treatment of thumb CMC osteoarthritis, the integration of evidence, clinical expertise, and patient values often does not result in one set approach to the management of an individual patient. Several factors including familiarity, personal experience, and comfort may be more influential than Level 1 evidence when determining a surgeon’s treatment choice. Although EBM remains the ideal goal for the practice of medicine, we should remain mindful of its limitations and critically appraise its value in clinical practice. Remaining up to date on the latest evidence will prevent it from being implemented improperly. As Sackett et al[15] said, “External clinical evidence can inform, but never replace individual clinical expertise. It is this expertise that decides which external evidence applies to the indivi
This study is not without limitations, some of which are inherent to self-reported survey studies. This questionnaire was sent to all active, retired, international, and candidate members of the American Society for Surgery of the Hand, so the results may not be representative of all practicing surgeons, particularly non-members or those practicing in other countries. Non-respondent bias is also a concern, as the 80.3% who did not respond may differ in their preferred surgical techniques compared to those who participated in the survey. Additionally, responses to several questions were limited to predefined selections. We attempted to account for this by providing additional opportunities for surgeons to explain their techniques and rationale via open-ended, free text responses. While this allowed for comprehensive data gathering, it posed a challenge during the survey process as the professional online survey service could not analyze these free text responses. The strength of the professional online survey service was its ability to provide descriptive statistics of the predefined, multiple-choice selections. However, these open-ended, free text responses required individual evaluation by the study authors to ensure the accurate categorization of respondents’ techniques and rationale. Lastly, this study was not intended to be scientific by design. Therefore, statistical calculations to determine differences between techniques, practice settings, specialty, case volume, and surgeon experience were not performed, and conclusions were limited at times due to small numbers.
This survey provides an interesting perspective of the current practice patterns in the surgical treatment of basilar thumb osteoarthritis. It seems that because the current evidence demonstrates non-inferiority of additional soft tissue stabilizing techniques in conjunction with trapeziectomy, surgeons rely more on individual clinical expertise. Ultimately, this may ensure the best outcome for their patients.
| 1. | Van Heest AE, Kallemeier P. Thumb carpal metacarpal arthritis. J Am Acad Orthop Surg. 2008;16:140-151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 120] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 2. | Yao J, Park MJ. Early treatment of degenerative arthritis of the thumb carpometacarpal joint. Hand Clin. 2008;24:251-261, v. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 56] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 3. | Gervis WH. Osteo-arthritis of the Trapezio-metacarpal Joint treated by Excision of the Trapezium. Proc R Soc Med. 1947;40:492. [PubMed] |
| 4. | Weiss AC, Goodman AD. Thumb Basal Joint Arthritis. J Am Acad Orthop Surg. 2018;26:562-571. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 38] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 5. | Brunton LM, Wilgis EF. A survey to determine current practice patterns in the surgical treatment of advanced thumb carpometacarpal osteoarthrosis. Hand (N Y). 2010;5:415-422. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 72] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 6. | Davis TR, Brady O, Dias JJ. Excision of the trapezium for osteoarthritis of the trapeziometacarpal joint: a study of the benefit of ligament reconstruction or tendon interposition. J Hand Surg Am. 2004;29:1069-1077. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 225] [Cited by in RCA: 224] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 7. | Belcher HJ, Nicholl JE. A comparison of trapeziectomy with and without ligament reconstruction and tendon interposition. J Hand Surg Br. 2000;25:350-356. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 132] [Cited by in RCA: 133] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 8. | Martou G, Veltri K, Thoma A. Surgical treatment of osteoarthritis of the carpometacarpal joint of the thumb: a systematic review. Plast Reconstr Surg. 2004;114:421-432. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 126] [Cited by in RCA: 137] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 9. | Shuler MS, Luria S, Trumble TE. Basal joint arthritis of the thumb. J Am Acad Orthop Surg. 2008;16:418-423. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 27] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 10. | Wolf JM, Delaronde S. Current trends in nonoperative and operative treatment of trapeziometacarpal osteoarthritis: a survey of US hand surgeons. J Hand Surg Am. 2012;37:77-82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 119] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 11. | Gangopadhyay S, McKenna H, Burke FD, Davis TR. Five- to 18-year follow-up for treatment of trapeziometacarpal osteoarthritis: a prospective comparison of excision, tendon interposition, and ligament reconstruction and tendon interposition. J Hand Surg Am. 2012;37:411-417. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 158] [Cited by in RCA: 181] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 12. | Wajon A, Vinycomb T, Carr E, Edmunds I, Ada L. Surgery for thumb (trapeziometacarpal joint) osteoarthritis. Cochrane Database Syst Rev. 2015;2015:CD004631. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 107] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 13. | Yuan F, Aliu O, Chung KC, Mahmoudi E. Evidence-Based Practice in the Surgical Treatment of Thumb Carpometacarpal Joint Arthritis. J Hand Surg Am. 2017;42:104-112.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 99] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 14. | Li YK, White C, Ignacy TA, Thoma A. Comparison of trapeziectomy and trapeziectomy with ligament reconstruction and tendon interposition: a systematic literature review. Plast Reconstr Surg. 2011;128:199-207. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 62] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 15. | Sackett DL, Rosenberg WM, Gray JA, Haynes RB, Richardson WS. Evidence based medicine: what it is and what it isn't. BMJ. 1996;312:71-72. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8991] [Cited by in RCA: 7638] [Article Influence: 254.6] [Reference Citation Analysis (0)] |
| 16. | Salem HM, Davis TR. Degenerative change at the pseudarthrosis after trapeziectomy at 6-year followup. Clin Orthop Relat Res. 2014;472:1160-1165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 19] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 17. | Kriegs-Au G, Petje G, Fojtl E, Ganger R, Zachs I. Ligament reconstruction with or without tendon interposition to treat primary thumb carpometacarpal osteoarthritis. A prospective randomized study. J Bone Joint Surg Am. 2004;86:209-218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 113] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 18. | Yang SS, Weiland AJ. First metacarpal subsidence during pinch after ligament reconstruction and tendon interposition basal joint arthroplasty of the thumb. J Hand Surg Am. 1998;23:879-883. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 106] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 19. | Leape LL, Berwick DM. Five years after To Err Is Human: what have we learned? JAMA. 2005;293:2384-2390. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 823] [Cited by in RCA: 709] [Article Influence: 33.8] [Reference Citation Analysis (0)] |
| 20. | Katz P. The Scalpel's Edge: The Culture of Surgeons. Allyn and Bacon. 1999;. |
| 21. | Kitto S, Villanueva EV, Chesters J, Petrovic A, Waxman BP, Smith JA. Surgeons' attitudes towards and usage of evidence-based medicine in surgical practice: a pilot study. ANZ J Surg. 2007;77:231-236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 33] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 22. | Schemitsch EH, Bhandari M, McKee MD, Zdero R, Tornetta P 3rd, McGehee JB, Hawkins RJ. Orthopaedic surgeons: artists or scientists? J Bone Joint Surg Am. 2009;91:1264-1273. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 23. | Zafonte B, Szabo RM. Evidence-based medicine in hand surgery: clinical applications and future direction. Hand Clin. 2014;30:269-283, v. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 24. | Robinson AHN, Johnson-Lynn SE, Humphrey JA, Haddad FS. The challenges of translating the results of randomized controlled trials in orthopaedic surgery into clinical practice. Bone Joint J. 2019;101-B:121-123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 25. | Poolman RW, Struijs PA, Krips R, Sierevelt IN, Lutz KH, Bhandari M. Does a "Level I Evidence" rating imply high quality of reporting in orthopaedic randomised controlled trials? BMC Med Res Methodol. 2006;6:44. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 75] [Cited by in RCA: 86] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: American Society for Surgery of the Hand, 103958; American Orthopaedic Association, AOA660; American Academy of Orthopaedic Surgeons, 00022902.
Specialty type: Surgery
Country of origin: United States
Peer-review report’s classification
Scientific Quality: Grade B, Grade C
Novelty: Grade B, Grade B
Creativity or Innovation: Grade B, Grade B
Scientific Significance: Grade B, Grade B
P-Reviewer: Chen N, China; Liu Y, China S-Editor: Liu JH L-Editor: A P-Editor: Zhao YQ