INTRODUCTION
Shoulder trauma can be caused directly or indirectly. A person can injure their shoulder directly by falling on their arm. Indirect mechanisms include falling on an outstretched hand with the upper extremity mounted at a different angle to the torso or when the arm is at a fixed point and the trunk is turned sharply. Shoulder injuries can produce different types of lesions including a simple dislocation (anterior, posterior, or inferior), a proximal humerus fracture, or a fracture dislocation. Fractures of the proximal humerus are classified as two-part, three-part, or four-part fractures according to Neer[1]. His classification system was based on an observation that all proximal humerus fractures were composed of four major segments: Lesser tuberosity; greater tuberosity; articular surface; and humeral shaft[2]. Neer[1] added categories for articular surface fractures and dislocations as he correctly observed these to be important prognostic factors. He enumerated the most common injury patterns and described how characteristic patterns of displacement occur with each fracture type. In addition, he explained how these fracture types result from the attached bone segments and the deforming forces generated by the rotator cuff.
Proximal humerus fractures are among the most frequent fractures in the elderly population[3]. Dislocations have a bimodal distribution as they most often occur in young male patients and females over 50 years of age[4]. Despite the frequency of shoulder trauma, little is understood about the pathobiomechanics. The purpose of this study was to investigate the literature on the mechanisms of shoulder injuries and to ascertain correlations between different types of lesions.
HISTORY
In 1938, Bankart[5] underlined the significance of the detachment of the capsule with or without the glenoid labrum from the anterior margin of the glenoid fossa. His theory of the mechanism of shoulder trauma became widely accepted. He considered that the detachment of the anterior capsule was responsible for the installation of the anterior instability of the shoulder. This explanation was founded upon surgical findings from 27 patients with recurrent shoulder dislocation. He also refuted the existing theories and proposed a refixation operation of the anterior capsule. In the novel approach used by Bankart[5], an osteotomy of the coracoid process is performed, and a cross-section of the subscapularis near its insertion is created for a wider view of the anterior glenohumeral ligaments. His technique has since been widely discussed and is still used today with some modifications. For example, anchors with strong non-absorbable sutures instead of catgut sutures and arthroscopy without incision on the subscapularis muscle and detaching the coracoid process are used. When there is a detachment of the labrum or a bone deficit in the anterior lower part of the glenoid fossa, they are referred to as a Bankart lesion and a bony Bankart lesion, respectively.
Shortly afterwards, radiologists Hill et al[6] examined compressive fractures in the posterolateral aspect of the humeral head, which is found after shoulder dislocations and is the typical defect. According to previous data, the force is transferred from the longitudinal axis to the humeral head when the hand is in abduction and turned outward. The humeral head is extruded out of the joint as it opposes the anterior edge of the glenoid fossa. Depending on the force applied, a greater tuberosity fracture of the neck of the humerus can be caused or the soft cancellous bone at the posterolateral aspect of the humeral head can be compressed into the scapula, creating the typical defect. The study of Hill et al[6] revealed that this compression fracture in cases of habitual dislocation were found so frequently that they were described as the typical defect (Figure 1). They postulated that many of these defects are sustained at the time of the first dislocation, and they may be an etiologic factor of recurrence. The defect can be best visualized by anteroposterior radiograph with the arm adducted and internally rotated (Figure 2). A special sign of the Hill-Sachs lesion is sharp, vertical, and dense medial border of the groove known as the “line of condensation,” which is the length that correlates with the size of the defect.
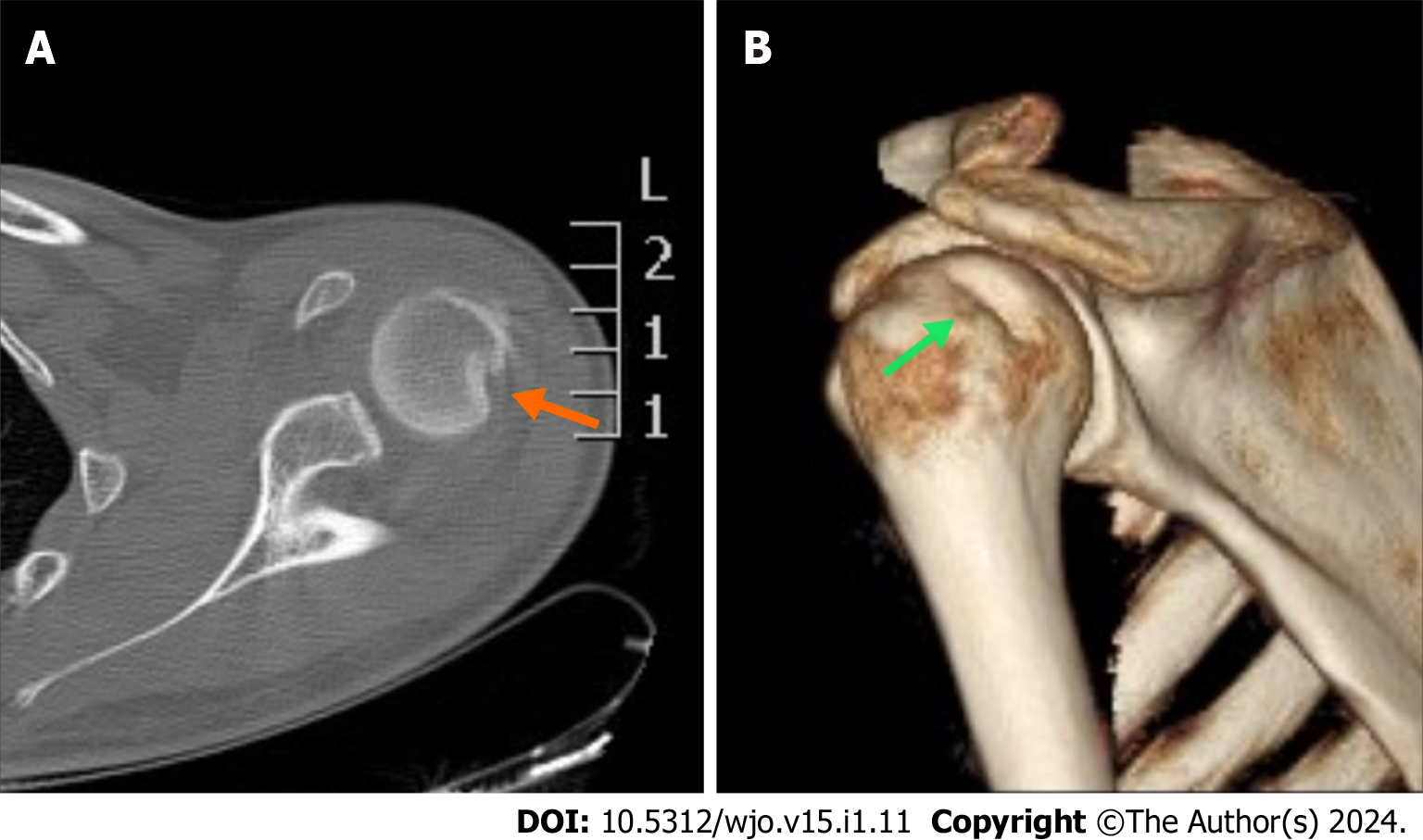
Figure 1 A 20-year-old patient after a forced abduction and hyperextension injury of his left shoulder with no support of his hand.
A: The computed tomography scan revealed an impaction fracture on the posterolateral part of the humeral head (orange arrow); B: A three-dimensional image in which the entire Hill-Sachs lesion was impressively displayed (green arrow).
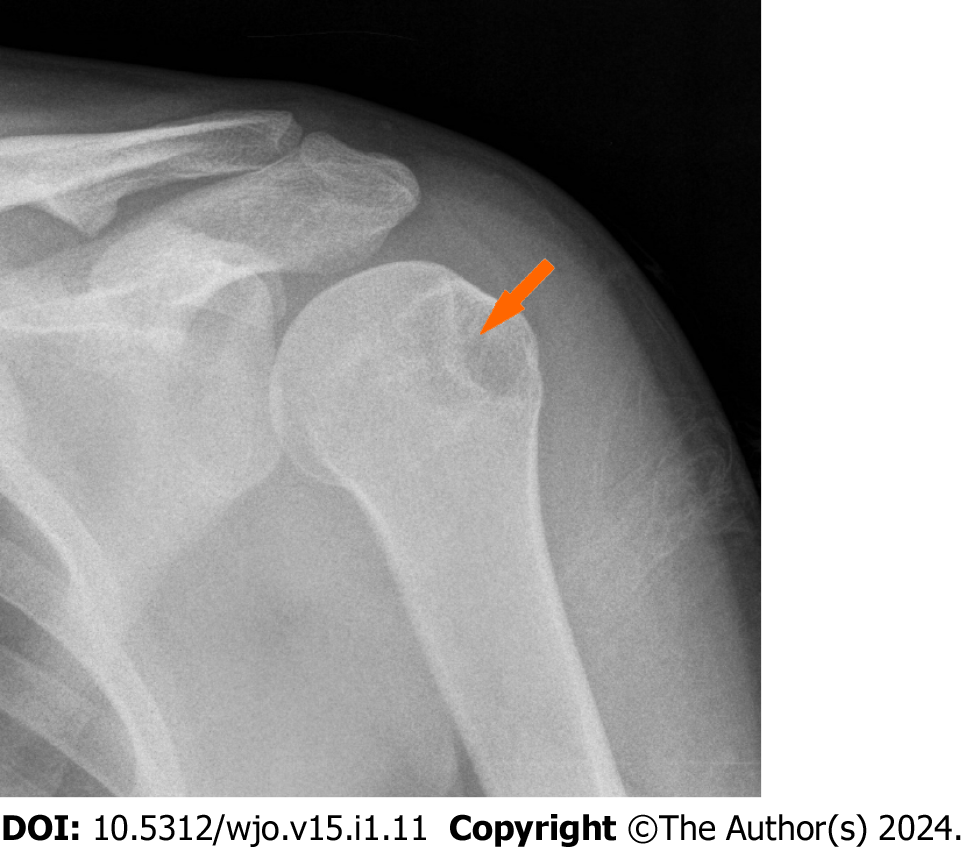
Figure 2 Left shoulder of a patient in internal rotation immediately after reduction of an anterior dislocation.
A large Hill-Sachs defect and a line of condensation was very obvious on this radiograph (orange arrow).
In 1948, Palmer et al[7] presented their results obtained with 90 patients treated with a bone block procedure, also known as the Hybbinette-Eden procedure. The augmentation of the anterior glenoid with a graft from the iliac crest was placed in a periosteal pocket at the anterior glenoid rim. They postulated that the compression fracture of the posterolateral aspect of the humerus was responsible for the development of recurrence, which was characterized as the essential lesion.
There are two theories that have become widely accepted to explain the development of instability. The first is detachment of the anterior capsule and the second is compression fracture in the posterolateral aspect of the humeral head. Other authors have attempted to investigate the role of different anatomical structures such as the anterior-medial glenohumeral ligament and the subscapularis muscle[8-10].
INCIDENCE OF SHOULDER TRAUMA
Most shoulder dislocations occur in males. The greatest incidence is observed in young and active patients, with the peak involving patients aged 16-20 years. In females, the prevalence increases after age 50, with the peak involving patients aged 61-70 years[4,11]. The risk of recurrence is lower if the primary reduction was performed by an orthopedic surgeon or was associated with a greater tuberosity fracture[12]. Older age and higher medical comorbidity score are also protective of recurrence.
About 95% of shoulder dislocations are anterior. The variants of the humeral head location after displacement are subglenoid, anterior or axillary, and subcoracoid[6]. Posterior glenohumeral dislocations represent approximately 2%-5% of all traumatic shoulder dislocations. A precise determination of the incidence remains difficult because of the frequency of undetected posterior dislocations[13].
Proximal humerus fractures account for almost 6% of all fractures in the Western world[3]. Following the fractures of the distal radius and spine fractures, it is the third most common osteoporotic fracture[14]. About 85% of these fractures occur in people over the age of 50, with the highest incidence occurring between the ages of 60 and 90 and with a female-to-male ratio of 70:30[3]. The most common fracture pattern according to the Arbeitsgemeinschaft für Osteosynthesefragen (AO) classification system is B1.1. This classification is valgus impacted and is found in 20% of cases[15]. AO types B1.1, A2.2, A3.2, and A1.2 represent over 50% of all proximal humeral fractures, while AO type C fractures occur in only 6% of cases[15].
MECHANISM OF SHOULDER DISLOCATION
Dislocations of the glenohumeral articulation and dislocations with a greater tuberosity fracture can be studied together due to similarity of the mechanism of the injuries. Gotzen et al[16] provided an alternative description for dislocations with great tuberosity fractures in their classification. In the most recent classification, Mutch et al[17] studied the morphology of these fractures and observed three fracture patterns, namely avulsion, split, and depression. These patterns may have practical implications in pathophysiology.
Symeonides[10] studied the etiology of shoulder instability and reproduced dislocations in fresh cadavers. He found that with the arm abducted, externally rotated, and extended, the posterior border of the greater tuberosity meets the posterior margin of the glenoid fossa. In this position the subscapularis muscle was in maximal tension. To permit dislocation, the subscapularis muscle had to be stretched or even partially ruptured; at the same time, the posterior border of the greater tuberosity was scratched while it was overriding the posterior margin of the glenoid. These data provided an explanation for the development of fracture dislocation of the shoulder, which is most referred to as a dislocation with greater tuberosity fracture.
When the head of the arm, which is located inside a very narrow pocket, meets the posterior margin of the glenoid fossa, creating an impression fracture on the posterolateral part of the humeral head, it was previously described as a Hill-Sachs lesion[6]. In other cases, a greater tuberosity fracture is created. In cases where the force continues without causing a fracture, the head collides with the anterior elements of the joints, which sometimes causes damage to the humerus, anterior glenoid labrum, cartilage, and subscapularis muscle. However, there is disagreement as to the part of the glenoid fossa where the collision with the humeral head takes place, with some authors suggesting the anterior margin[18,19] and others the posterior[10,20].
Bahrs et al[20] suggested that the common Hill-Sachs lesionwhich occurs in anterior shoulder dislocations and is defined as an impaction fracture at the posterolateral aspect of the proximal humeruspresents itself in its completed form as a greater tuberosity fracture. They divided their study population which consisted of patients with isolated great tuberosity fractures or dislocations with fractures into two mechanisms of injury: (1) Direct injury, sustained as a direct force or blow to the shoulder with the arm in adduction or a direct fall on the lateral aspect of the shoulder; and (2) Indirect injury, sustained as a fall on the extended arm or flexed elbow or abduction (external rotation trauma). They studied anteroposterior and axillary view radiographs before and after reduction, and they correlated the findings with the above mechanisms. Even though this study included a large number of patients, it referred to only two mechanisms of injury that led to either anterior dislocation or dislocation with greater tuberosity fracture. In addition, patients were evaluated with plain radiographs, which provide less diagnostic value than cross-sectional modalities such as computed tomography (CT) and magnetic resonance imaging (MRI). Nevertheless, the significance of this study lies in its strengthening of the theory of the mechanism of dislocation and fractures, as other authors before had suggested[6,10,21]. The important conclusion from this study was that dislocations with a greater tuberosity fracture almost never create instability as other authors had suggested[11,22]. This likely arises because the force of the impact transmitted from the humerus to the head is completely relieved in the greater tuberosity and is not enough to injure the anterior elements of the joint.
When there is a greater tuberosity fracture, the possibility of recurrence is low[11,22]. McLaughlin et al[22] postulated that recurrent and non-recurrent shoulder dislocations have little in common. They retrospectively reviewed two clinical samples to find a specific mechanism that led to instability. They observed that non-recurrent shoulder dislocations typically showed posterior joint support damage and that recurrent shoulder dislocations typically showed anterior joint support damage. It is worth noting that 5 of the patients required open reduction (all great tuberosity fractures), while 4 of the patients had dislocation of the long tendon of the biceps, which was interposed between the humerus and glenoid.
Age also plays an important role in the mechanism of shoulder injury[22-25]. In elderly patients, the posterior mechanism is predominant. The posterior elements, which consist of the rotator cuff muscles, are more prone to injury because of the weakening and degeneration associated with aging. As a result, young patients usually present with Bankart lesions, which are anterior inferior labral tears and are prone to dislocation. The rotator cuff plays a secondary role in the stability of the glenohumeral articulation. Therefore, only massive tears will increase the risk of recurrence[23] and specifically subscapularis tears[24]. In conclusion, younger patients show more shoulder instability than older patients[25].
IMAGING AFTER GLENOHUMERAL DISLOCATION
Plain anteroposterior radiographs before and after a dislocation are common practice. In most cases, anteroposterior radiographs are the only imaging conducted in an emergency. Axillary and/or transcapular projections are often performed when the direction of force producing the trauma is unknown, and there is a strong suspicion of posterior dislocation. Posterior dislocations can be missed up to 50% of the time on anteroposterior radiographs[26,27]. In the absence of other views there are several indications for diagnosis of posterior dislocation on the frontal view (Figure 3). The rim sign, which is a widening of the articular distance more than 6 mm, and the trough sign will appear on the axillary view as a sclerotic line at the site of the impaction fracture on the anterior humeral head[26].
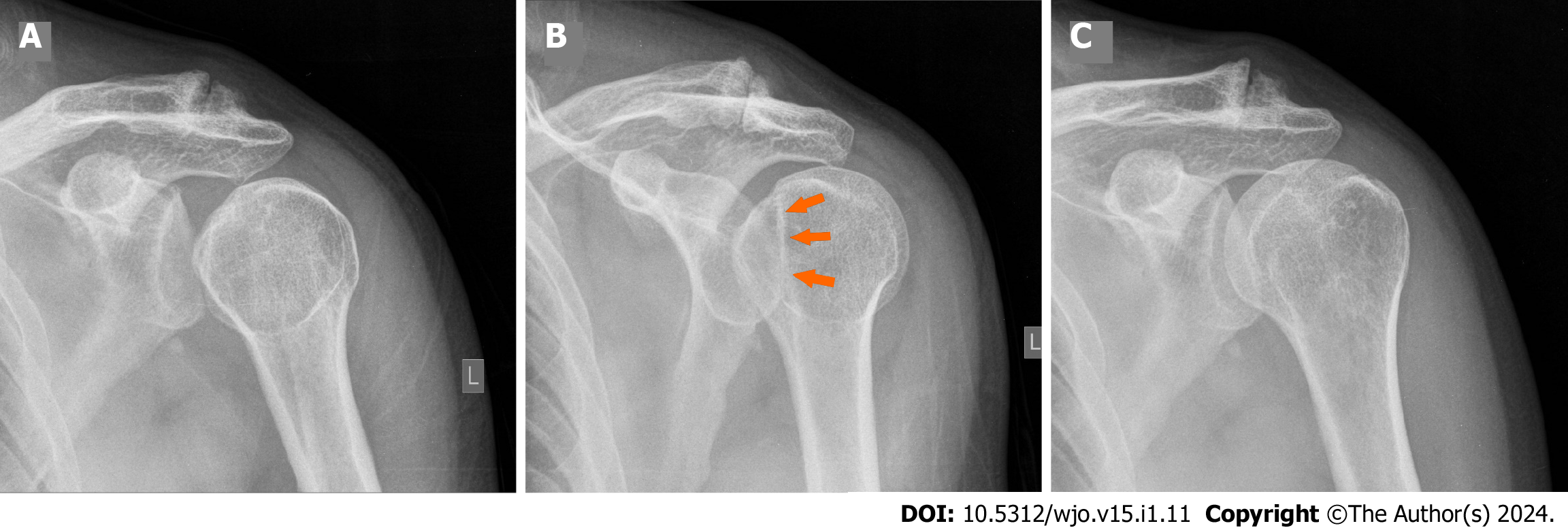
Figure 3 Posterior shoulder dislocation.
A: In the frontal view the distance of the medial cortical margin of the humeral head and the anterior glenoid rim was more than 6 mm, constituting a positive rim sign; B: A slightly oblique view with appreciable through sign (orange arrows). The humeral head was in internal rotation and hooked on the posterior rim of the glenoid fossa; C: The post reduction anteroposterior radiograph showed normal alignment and congruity of the glenohumeral articulation.
CT imaging is indicated in cases where the direction of force cannot be distinguished. In addition, it provides information regarding dislocation with a greater tuberosity fracture as well as bony-Bankart lesion (Figures 4 and 5). CT imaging is the most targeted examination for measuring the glenoid destruction with the best-fit circle technique used in the sagittal plane[28,29]. It is important to accurately diagnose glenoid bone loss as a defect of more than 20% of total glenoid surface or more than 7mm width, is very likely to lead to instability[18,26].
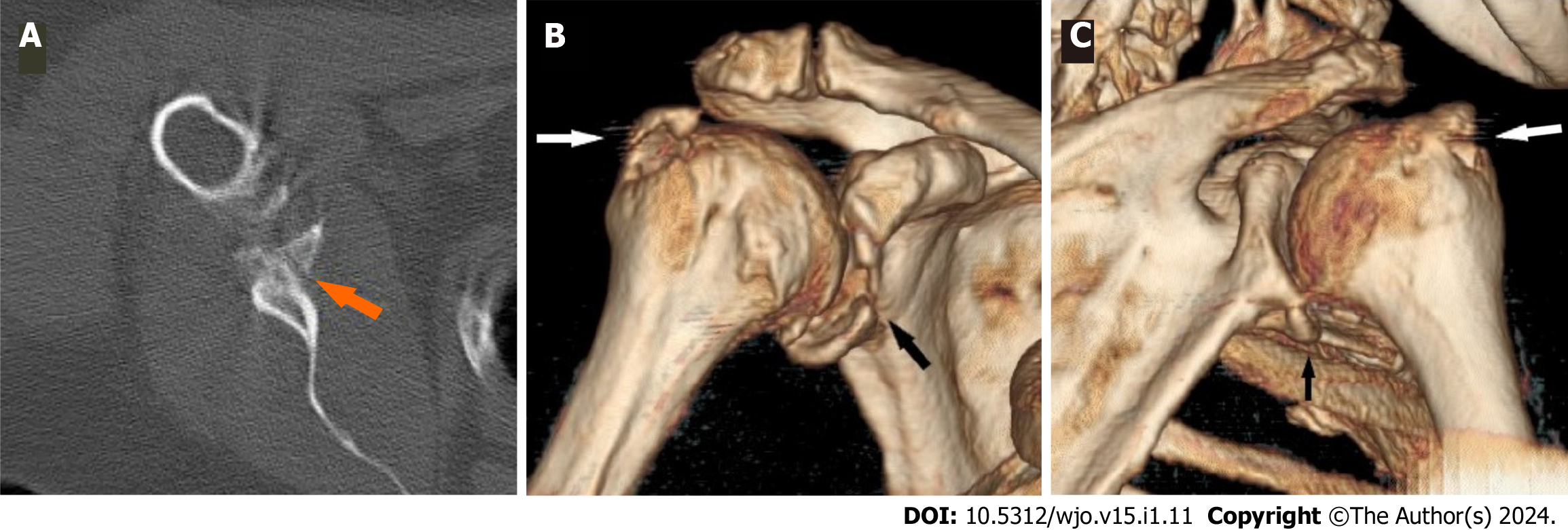
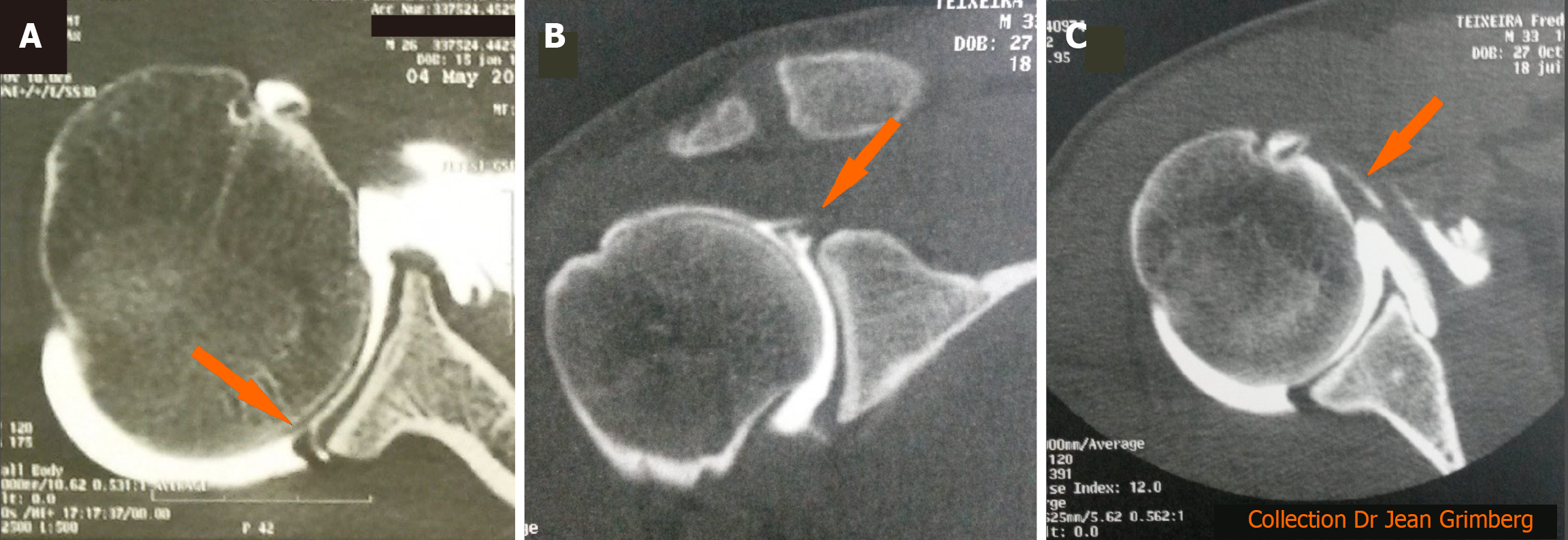
Figure 4 A 58-year-old female after a forward fall with the arm in flexion resulted in anterior dislocation with a bony Bankart lesion and greater tuberosity fracture.
A: The sagittal image illustrated a bony Bankart lesion (orange arrow); B: An anterior three-dimensional image on the same patient showed a large Bankart lesion (black arrow) and greater tuberosity fracture (white arrow); C: The absence of a Hill-Sachs lesion was evident on the posterior three-dimensional view.
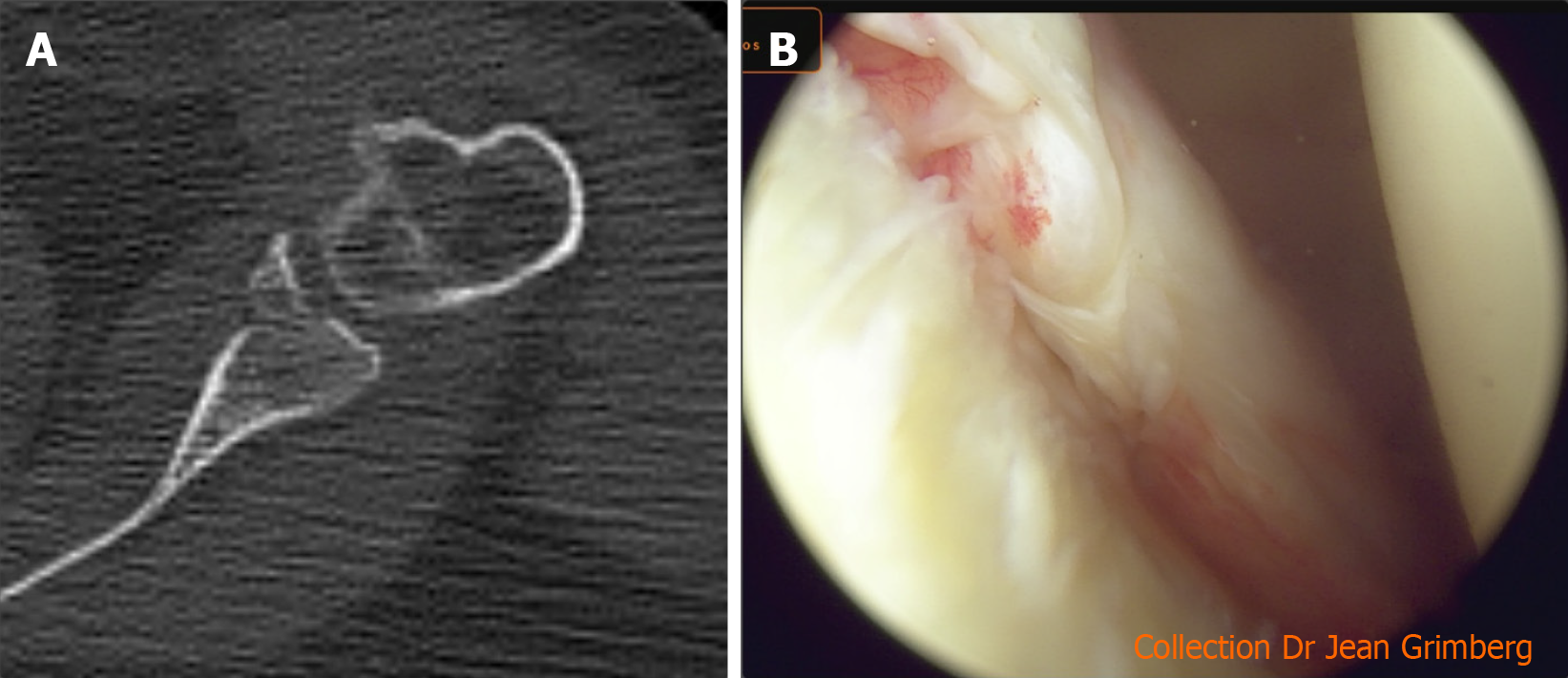
Figure 5 Bony Bankart lesion imaging.
A: Computed tomography scan of a bony Bankart lesion on the sagittal view; B: Image during arthroscopy of a Bankart lesion.
Imaging tests such as MRI are rarely considered necessary in patients with shoulder dislocation. MRI is often ordered after the early post-traumatic period, when soft tissue injury is suspected or joint instability develops. MRI is the most sensitive modality for diagnosis of soft tissue injuries such as rotator cuff ruptures, labral ruptures, and damage of the cartilage (Figure 6).
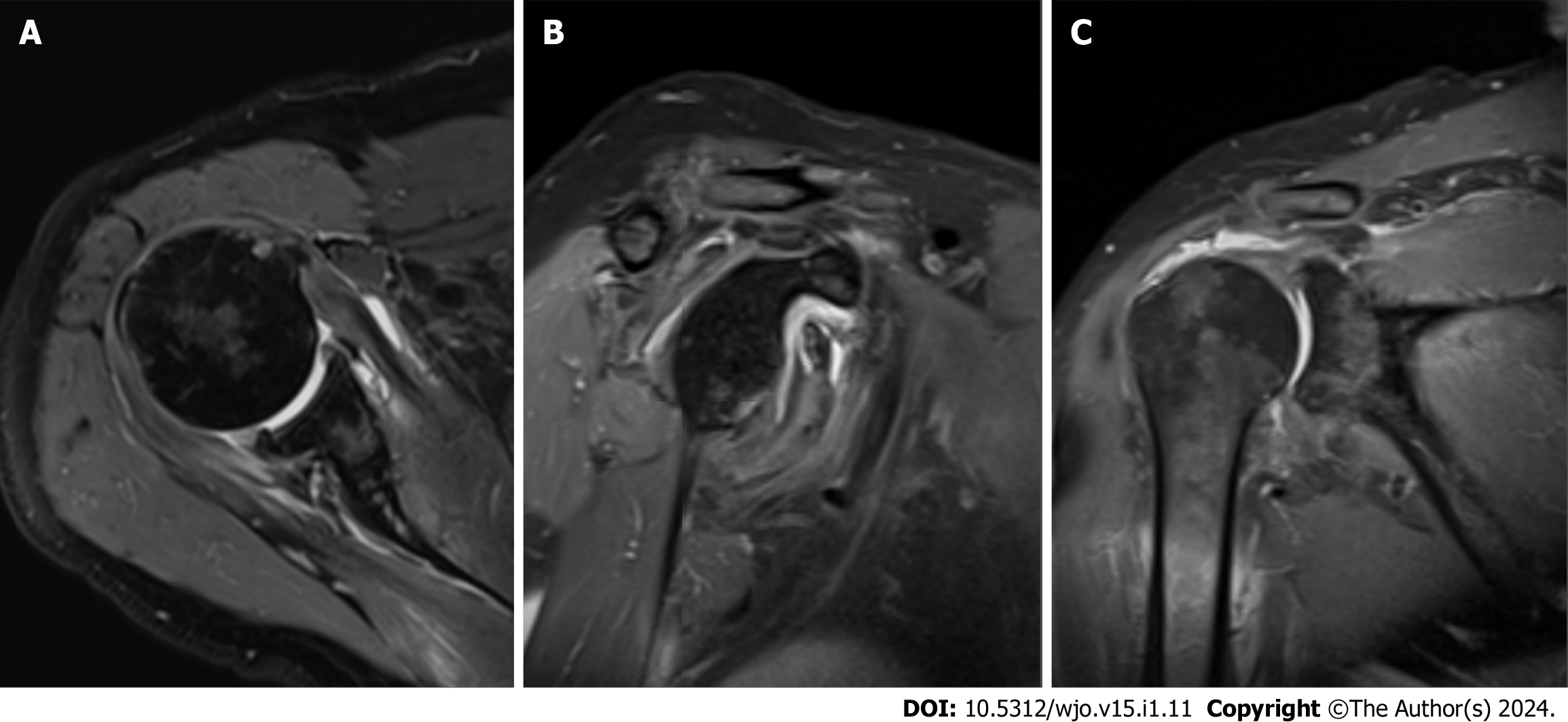
Figure 6 Magnetic resonance imaging of a 75-year-old male after a fall with forced abduction-hyperextension of the arm with support in the hand that resulted in anterior dislocation.
A: Anterior labral tears are best detected on the sagittal view; B: Bone edema on the anteroposterior margin of the glenoid; C: Magnetic resonance imaging is the modality of choice in cases of suspected rotator cuff tears.
In a study by Atef et al[30], early findings after shoulder dislocation were investigated in 240 patients using MRI and ultrasonography (US) until the 1st wk after injury. The incidence of complications was significantly higher than in previous reports[31,32]. In that study, rotator cuff tears were found in a total of 27.9% of the population and were the most common injury. Greater tuberosity fractures were found in 15.4% of patients, and axillary nerve injuries were found in 15.3% of patients. Hill-Sachs and Bankart lesions were also observed[30]. The predominant age group with rotator cuff tears was females over age 45, which was similar to previous reports[33,34]. US is also an acceptable imaging modality when a rotator cuff tear is suspected. US has the advantages of speed and the ability to compare both shoulders at one time. However, the accuracy of US evaluation of the rotator cuff depends on the experience of the ultrasonographer[35]. Invasive modalities such as MRI and CT arthrography (Figure 7) are the best modalities to detect sports-related injuries like Bankart lesions, superior labral anterior posterior lesions, Perthes lesions, anterior labral periosteal sleeve avulsion lesions, and glenolabral articular disruption cartilage ruptures[36,37].
Figure 7 Computed tomography arthrography is useful in cases of false-negative magnetic resonance imaging results.
A: Posterior labral tear on the sagittal view; B: Superior labral anterior posterior lesions are best detected on the coronal view; C: Computed tomography arthrogram is the modality of choice in cases of undetected subscapular tears. The sagittal view showed widening of the bicipital canal, which is an indirect sign of subscapularis rupture and delamination with penetration of contrast fluid into the tendon (orange arrow).
MECHANISM OF PROXIMAL HUMERUS FRACTURES
Little is understood about the pathobiomechanics that lead to proximal humerus fractures. Several theories include fractures transmitted through epiphyseal lines of the proximal humerus, deforming forces of the rotator cuff muscles on fracture fragments, and the arm position in relation to the torso at the time of impact[1,2,38]. Neer[1] refuted the existing theories of classification in proximal humerus fractures and emphasized the role of different arm rotations during injury. In addition, taking into account the size of the joint pocket that can fit up to two humeral heads when the tuberosities are detached, underlined that the articular surface of the humerus can easily be subluxated or rotated out of the glenoid fossa. To identify the role of muscle attachment on displaced fragments as well as the circulatory status and continuity of the articular surface, he adopted a classification system based on the four fracture segments (as described above)[2].
Most authors identify two mechanisms for the development of proximal humerus fractures, which can be divided into direct and indirect mechanisms. Direct fractures include a fall on the shoulder. This is represented by a direct impact of the head of the humerus on the scapula without the arm being loaded axially and is usually a high-energy injury[39,40]. Indirect fractures are usually caused by a fall onto an outstretched hand with the fracture point not directly impacted. The position of the hand can be different; sometimes it is in abduction and external rotation and sometimes in flexion and abduction. The indirect mechanism is also more frequent because the arm is subject to a large but relatively lower energy load compared to the direct mechanism[41-44]. Rare mechanisms that can cause a fracture include excessive muscle contraction by muscle groups around the shoulder, which can occur during seizures and electric shock[45].
In the indirect mechanism, the fracture is caused by an attempt to avoid an uncontrollable fall forward or sideways. Typically, a fall on an outstretched hand causes relative displacement or rotation of the trunk around the point of rotation, producing an abduction or adduction motion to the proximal humerus[46-48]. Some authors have observed that anatomical neck fractures are associated with posterior dislocations, but the mechanism has not been fully established. Anterior dislocations can be associated with a greater tuberosity fracture or Hill-Sachs lesion.
Several studies investigating this type of injury have found that both greater tuberosity fractures and Hill-Sachs lesions may be the result of the same mechanism[10,20,41,47]. With the arm abducted, externally rotated, and extended, the posterior border of the greater tuberosity comes into contact with the posterior margin of the glenoid fossa. As a result, an impaction fracture in the posterolateral part of the humerus or a greater tuberosity fracture can occur[10,20]. Hyperabduction, with impaction of the humeral head to the acromion, can produce a valgus impacted two-part proximal humeral fracture or an inferior dislocation depending on the strength of the underlying ligaments[49]. Other mechanisms that can produce two-part proximal humeral fractures and humeral head split fractures with impaction of the humeral head onto the glenoid fossa have not been fully investigated[50,51].
There is no evidence of the biomechanics of proximal humerus fractures due to the lack of interest and absence of in vivo biomechanical data[52]. A study by Majed et al[53] investigated the mechanism of proximal humerus fractures by creating a biomechanical model to examine the effect of arm position at the point of impact. The mechanisms investigated were a direct impact onto the adducted shoulder in the neutral rotation (side impact simulation) and a fall onto an outstretched hand (parachute reflex)[38], which produced district fracture patterns. Both mechanisms were reproduced by a simulator. The side impact mechanism resulted in a simple head split, which also occupied the greater tuberosity and was accompanied by valgus impaction and relative valgus displacement of an intact articular head onto the shaft. The parachute reflex with the shoulder position in 70° abduction, 20° angulation in the sagittal plane, and 30° internal rotation[40] recreated the three main fracture types, namely an undisplaced greater tuberosity fracture, a shield-type fracture, and a head split. They also found that in shield type fractures the detached greater tuberosity segment extends to the sulcus of the biceps, thus creating a butterfly fragment. This is like the three-part fracture where the extension of the greater tuberosity is the point where the nutrient arteries enter the bone and provide perfusion to the arcuate vessels. This is an important inhibitory factor for the development of aseptic necrosis[1,2,38]. Despite the importance of this study, the authors did not account for the soft tissue attaching the head of the humerus that could affect fracture pattern. Furthermore, the mechanisms of the development of proximal humerus fractures, individual greater tuberosity fractures, and fracture dislocations could be more complex than the two mentioned above.
IMAGING AFTER PROXIMAL HUMERUS FRACTURES
Proximal humerus fracture imaging is carried out with the simplest tests due to the prevailing theory of independent fragments that are displaced by the rotator cuff muscles[1]. The anteroposterior view combined with the axillary view has been shown to be superior in terms of classification accuracy[20]. Existing classifications in use, like the Neer and the AO/Orthopedic Trauma Association classifications, have poor intraobserver and interobserver reliability despite the modality of imaging used[54]. Furthermore, CΤ and two-dimensional and three-dimensional CT are widely used by surgeons for the assessment of complex fracture patterns even though they do not offer improved interobserver and intraobserver agreement, as other authors have suggested[55,56]. Thus, even shoulder specialists fail to reconcile the classification and the appropriate imaging method for the best assessment of the fracture. In addition, the Neer classification of the four segments is not a radiographic classification. It is based on pathoanatomical classification by exacting roentgen studies, interpretation of the films, and occasionally intraoperative findings[57].
Other factors like the rotation of the segments, the impaction of the humeral head, and the separation of the articular surface seem to be more important and can be best evaluated by CT. The update of the Neer[57] classification in 2002 included a supplementary type for valgus-impacted four-part fracture underlined by valgus rotation of the humeral head among separated segments of the tuberosities. In these cases, the glenohumeral articular surface is preserved rather than dislocated, as seen with the classic four-part proximal humerus fracture. An intact medial calcar, where the nutrient arteries enter the bone and provide perfusion to the arcuate vessels, carries a lower risk of post-traumatic avascular necrosis and may be treated without surgery[29,58]. Consequently, this illustrative detail, that may change management and outcome, should be distinct.
MECHANISM OF SHOULDER TRAUMA IN SPORTS
Shoulder injuries are quite common in athletes, especially in high-energy contact sports such as rugby and hockey. Many studies have investigated the mechanisms of the repetitive movements of athletes in different sports that lead to aggravation of different anatomical structures, particularly the soft tissue around the shoulder joint. Other studies have investigated the diagnosis and treatment of these lesions. Two studies elucidated and described patterns of shoulder injury mechanisms in elite rugby players. The aims were to correlate injury-producing mechanisms with specific patterns of injury. Longo et al[59] used a video tape to analyze the mechanism of injury in four rugby players who sustained a shoulder dislocation. The authors observed abduction and external rotation as the accepted mechanism of anterior dislocation and suggested that rugby players are at risk of anterior dislocation by hyperflexion with internal rotation.
Crichton et al[60] identified three mechanisms of shoulder injury from a video analysis of 24 rugby players. They included the “Try-Scorer” (characterized by hyperflexion and axial load of the outstretched arm equally when an athlete falls to score), the “Tackler” (defined as forced abduction and extension of a non-fixed to the ground hand while tackling), and the “Direct Impact” (a direct fall on the shoulder with the arm adducted and representing direct impact of the head of the humerus on the scapula without axial load to the arm). The “Try-Scorer” and “Tackler” mechanisms predominantly resulted in shoulder dislocations with Bankart, reverse Bankart, and superior labrum anterior posterior tears. In addition, the “Try-Scorer” mechanism caused the majority (83%) of rotator cuff tears. The “Direct Impact” mechanism resulted in glenohumeral dislocation and labral injury in 37.5% of players and was the only mechanism that resulted in acromioclavicular joint dislocation and scapula fractures[60]. Limitations of the above investigation were the relatively small sample and the study population of athletes with a strong muscular system and increased bone density who are injured with significantly greater energy than the general population.
CONCLUSION
The mechanism of shoulder injury has been studied primarily in distinct injuries. Thus, possible mechanisms have been studied that lead to anterior dislocation of the shoulder and dislocation with concomitant greater tuberosity fractures. However, only two mechanisms of the proximal humerus dislocations have been succinctly reported.
The biomechanics of shoulder trauma have not been fully investigated, and it seems that other factors such as age, muscle strength, and bone density play an important role in the development of different lesions. Radiological and laboratory findings of distinct types, have been studied individually and fall under common mechanisms. To our knowledge, there are no recent studies linking the mechanism of shoulder dislocation and/or proximal humerus fracture injury to post-traumatic radiological findings. Knowledge of specific injuries based on the mechanism of the injury will enable the clinician to be suspicious when there is no capability for immediate radiological imaging, or when district patterns are not evident in a simple radiological examination. In addition they will help in the treatment plan that will be followed reducing the possibility of falsely omitting negative imaging findings.
ACKNOWLEDGEMENTS
The authors would like to thank Dr Jean Grimberg for providing the images from his personal collection.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: Greece
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Iossifidis A, United Kingdom; Shibata Y, Japan S-Editor: Liu JH L-Editor: A P-Editor: Guo X