Published online Sep 5, 2025. doi: 10.4292/wjgpt.v16.i3.107148
Revised: April 30, 2025
Accepted: June 26, 2025
Published online: September 5, 2025
Processing time: 172 Days and 0.1 Hours
Obesity is a global pandemic that has been threatening the worldwide population. It has been reported to be associated with an increase in the risk of chronic diseases such as type 2 diabetes mellitus (T2DM), cardiovascular disease, and other diseases, including some malignancies. Currently, the first line of mana
Core Tip: Obesity is a global pandemic causing chronic diseases like type 2 diabetes mellitus (T2DM) and cardiovascular disease. Lifestyle modifications and bariatric surgeries are the primary management methods. Glucagon-like peptide-1 receptor agonists (GLP-1RAs) are a rising star for managing T2DM by controlling blood sugar and weight loss. However, they have side effects like nausea, vomiting, diarrhea, and gastrointestinal (GI) adverse events. More serious risks include pancreatitis, gallbladder diseases, and thyroid C-cell cancers. This review discusses GLP-1RAs' role in obesity management and GI safety considerations.
- Citation: Ismail A, Amer MS, Tawheed A. Glucagon-like peptide-1 receptor agonists: Evolution, gastrointestinal adverse effects, and future directions. World J Gastrointest Pharmacol Ther 2025; 16(3): 107148
- URL: https://www.wjgnet.com/2150-5349/full/v16/i3/107148.htm
- DOI: https://dx.doi.org/10.4292/wjgpt.v16.i3.107148
The past decade has witnessed the growing burden of obesity and related comorbidities as a major public health problem across the globe[1,2]. Obesity is the ultimate result of a continuous state of positive energy balance where energy intake exceeds energy expenditure. The surplus of energy in the form of calories is stored as fatty acids in adipose tissue leading eventually to an overweight body phenotype with a body mass index (BMI) ≥ 25 kg/m2, and ultimately to obesity, a body weight disorder, with a BMI ≥ 30 kg/m2[3]. Overall, obesity could be defined as the excessive or abnormal accumulation of body fat affecting the persons’ health-related quality of life[4-6]. Obesity was once considered a cosmetic problem, but is now considered by the American Medical Association as a multi-factorial disease where genetics, behavioral, and environmental factors play a role[3]. Obesity is an important risk factor for morbidity and mortality from type 2 diabetes mellitus (T2DM), cardiovascular diseases, stroke, dyslipidemia, hepatic steatosis, hypertension (HTN), gallbladder diseases, osteoarthritis, obstructive sleep apnoea, and some types of cancer (endometrial, breast, ovary, prostate, liver, gallbladder, kidney and colon)[7,8]. Obesity and overweight contribute to 35.8 million (2.3%) of the world's disability-adjusted life years, and to over 2.8 million deaths annually worldwide[9].
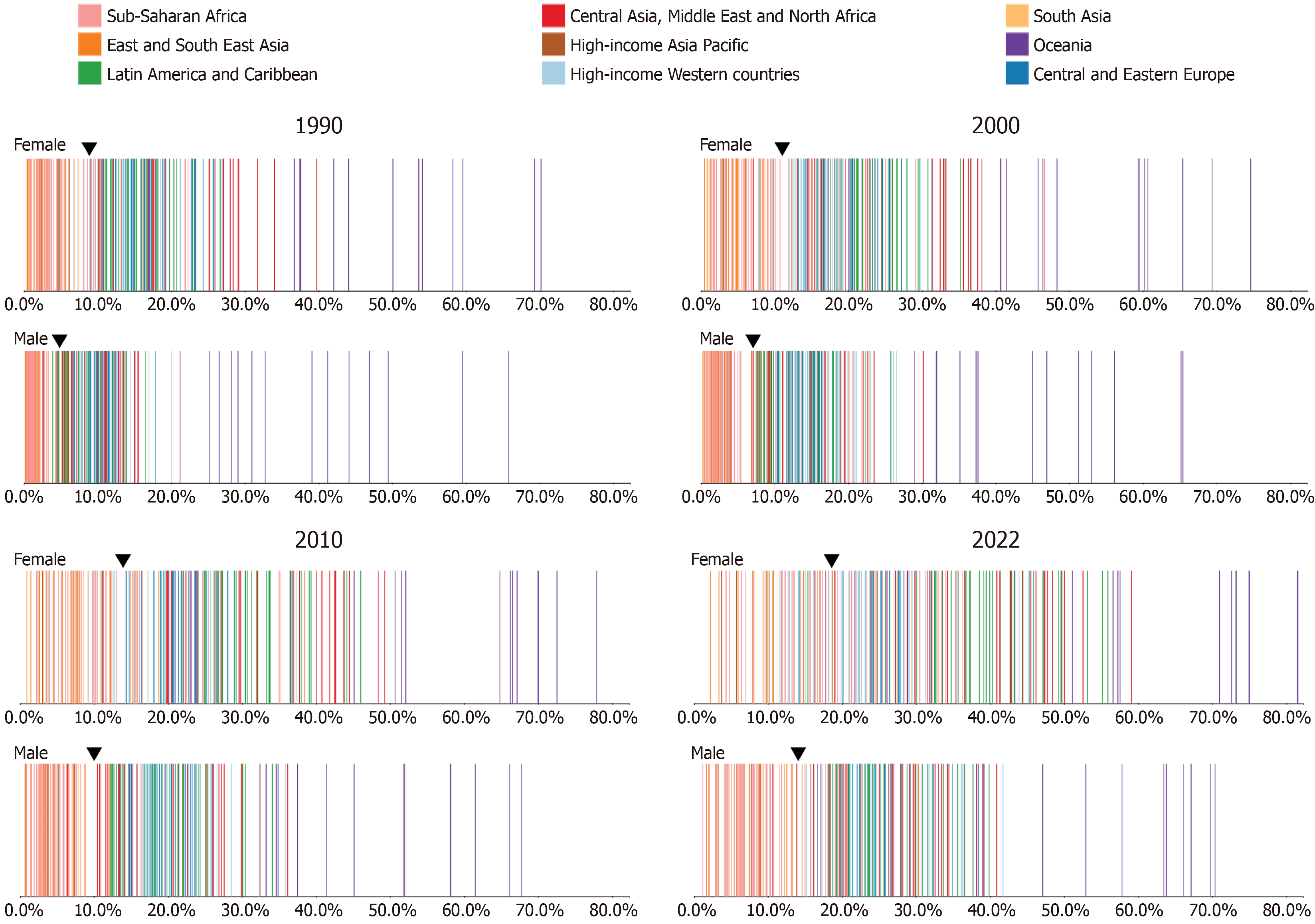
The obesity epidemic began in the United States over 40 years ago, and the obesity prevalence has increased by twofold in the United States from 1980 to 2010. Globally, obesity prevalence has doubled since 1980 to the point where one-third of the world’s population is classified as overweight or obese. In 2022, the World Health Organization reported that 890 million (16%) of the world's people aged 18 years and over were obese, and 2.5 billion (43%) were overweight[10]. If the current trends continue, it is estimated that by 2030, 57.8% of the world population will be overweight or obese[11]. The Noncommunicable Diseases Risk Factor Collaboration (NCD-RisC) expected that by 2025, the prevalence of obesity will reach 18% in men and 21% in women[12]. According to the latest statistics from the NCD-RisC, the preva
This global burden of obesity represents the domino effect triggered by globalization, rapid urbanization, and economic growth which led to substantial lifestyle changes from diets to day life activities promoting a state of positive energy balance through increased consumption of empty caloric food with more sugar and fats than nutrients, and reduced physical activity (Figure 2)[14-16]. The risk of obesity is higher in developing and developed countries compared to low-income countries. While obesity affects people of all ages and sexes in high-income nations, it is disproportionately more common in underprivileged groups. In low-income countries, obesity is typically more common among middle-aged adults from high social class, particularly women[17]. In general, across all sociodemographic groups, women are more likely than males to be obese[18].
Since energy balance is regulated by a variety of biological processes, treating obesity and maintaining weight loss afterward have proven difficult. The first-line treatment for obesity is non-pharmacological with behavioral modifications promoting healthy eating habits and regular exercise; however, non-pharmacological approaches could only lead to a weight loss of 1-6 kg, which is difficult to maintain[3,19-21]. Pharmacotherapy appears as a good adjunct when beha
Bariatric surgeries could also be done endoscopically. This is done as part of endoscopic bariatric therapies, which provide a minimally invasive, cheaper, and safer modality to mitigate obesity[28]. The various types of endoscopic bariatric therapies include space-occupying devices (intragastric balloons, botulinum toxin injection, aspiration therapy, and transpyloric shuttle, etc.), stomach procedures (primary obesity surgery endoluminal, endoscopic sleeve gastroplasty, etc.), and small bowel procedures [duodenal jejunal bypass sleeve (endobarrier), gastroduodenal-jejunal bypass (endobypass system), duodenal mucosal resurfacing, etc.][28,29]. According to current guidelines, endoscopic bariatric therapies is the standard of care in treating obesity class I[29]. Additionally, a recent systematic review and meta-analysis by Zhu et al[30] deemed endoscopic bariatric surgery as an effective and safe method for weight reduction with a better 12-month effect than the non-adjustable intragastric balloon.
Over the past decades, pharmacotherapy for obesity has made significant progress[31]. However, many drugs were withdrawn in the human clinical trials phase due to various side effects, inability to be used beyond 3 months, or a moderate short-term efficacy[32]. An example of withdrawn drugs are riconabant, a cannabinoid receptor type 1 antagonist, and sibutramine, an inhibitor of neurotransmitter re-uptake[33,34]. Anti-obesity pharmacotherapy tries to mitigate common pathways regulating energy balance and feeding behavior including the opioid system, the leptin-melanocortin axis, glucagon-like peptide-1 (GLP-1)/ GLP-1 receptor (GLP-1R) system, and fibroblast growth factor 21/its receptor complex FGFR1c/b-klotho axis. GLP-1R agonists (GLP-1RAs) have revolutionized the treatment of metabolic diseases including T2DM and obesity. Nevertheless, a focus should be put on the cumulative arising evidence regarding GLP-1RAs-induced adverse events and how to prevent such complications from arising or, if they occur, to manage them properly. While GLP-1RAs are widely used, comparative analyses of GI tolerability across agents—especially dual glucose-dependent insulinotropic polypeptide (GIP)/GLP-1RAs like tirzepatide—remain limited.
Herein, we will discuss gastrointestinal (GI) adverse events, and contraindications associated with GLP-1RAs.
When nutrients are consumed, the gut-driven incretin hormone GLP-1 is released[35]. GLP-1 is a peptide hormone that regulates glucose homeostasis after ingestion of carbohydrates or fats. GLP-1 exists in two active forms: (1) GLP-1 (7-36) amide (30 amino acids); and (2) GLP-1 (7-37) (31 amino acids). GLP-1 increases insulin production, decreases glucagon secretion, slows stomach emptying, and decreases food intake[36]. GLP-1RAs have been proved to restore insulin secretory functions, improve glycemic control, and reduce bodyweight in patients with T2DM[37].
The source of GLP-1 secretion remained an enigma till 1983, when it was found to be derived from the proglucagon gene’s transcription product and secreted from: (1) Enteroendocrine L cells as the entral GLP-1 in the periphery; (2) A-cells in the pancreatic islet; and (3) Preproglucagon neurons in the solitary tract's caudal nucleus and nearby medullary reticular formation produce GLP-1 in the central nervous system (CNS)[38-42]. Neurons that produce GLP-1 extend across the brain to the hypothalamus and other areas that regulate energy balance.
Once GLP-1 is secreted, its hypoglycemic action is mediated via the GLP-1R, a class B G-protein coupled glucagon receptor abundantly expressed in the stomach, islet B-cells, intestine, and CNS[43,44]. GLP-1 exerts its action by inhibiting hepatic glucose production through alpha cells glucagon secretion, increasing insulin secretion from pancreatic beta-cells, improving insulin resistance via upregulation of the expression of glucokinase and glucose transporter genes, increasing satiety, decreasing appetite, and inhibiting gastric emptying[45-49]. Interestingly, natural GLP-1 exerts its actions within a very short half-life of approximately 2 minutes. GLP-1 has a rapid renal clearance and inactivation via dipeptidyl peptidase IV (DPP-IV). Due to these benefits and the short half-life, drug developers have tried to synthesize exogenous GLP-1RAs[36].
Although genetic studies report a limited link between the GLP-1/GLP-1R axis T2DM, GLP-1RAs are approved as the third-line therapy following metformin and oral medications such as DPP-IV inhibitors for treating T2DM[50]. The role of GLP-1RAs in T2DM emerged from the fact that endogenous GLP-1 concentrations are decreased in response to oral glucose load in T2DM patients. The first GLP-1RA to be approved for the clinical treatment of T2DM was exenatide. Subsequently, many GLP-1RA were approved (Table 1)[51]. GLP-1RAs are effective in lowering fasting plasma glucose and glycated hemoglobin in T2DM. The greatest hypoglycemic effects were reported with tirzepatide, followed by semaglutide once weekly, dulaglutide and liraglutide, then exenatide once weekly, followed by exenatide twice daily and lixisenatide[52-54]. In pediatric patients with T2DM who are 10 years and older, liraglutide and exenatide extended-release injections are the only GLP-1RAs approved of T2DM treatment[55,56].
| Glucagon-like peptide-1 receptor agonists | Injection frequency | Manufacturer | Approval year | Dosage concerns in hepatic patients | Dosage concerns in renal patients |
| Short-acting agonists | |||||
| Exenatide | Twice daily | AstraZeneca | 2011 | Safe | Avoid if eGFR less than 30 mL/minute/1.73 m2 |
| Lixisenatide1 | Once daily | Sanofi | 2013 | Safe | Avoid if eGFR less than 15 mL/minute/1.73 m2 |
| Long-acting agonists | |||||
| Liraglutide | Once daily | Novo nordisk | 2009 | Safe | Safe |
| Exenatide extended-release | Once weekly | AstraZeneca | 2017 | Safe | Avoid if eGFR less than 45 mL/minute/1.73 m2 |
| Semaglutide | Once weekly | Novo nordisk | 2017 | Safe | Safe |
| Dulaglutide | Once weekly | Eli lilly | 2014 | Safe | Safe |
| Albiglutide | Once weekly | Glycogen synthase kinase | 2014 | Safe | Safe |
| Tirzepatide | Once weekly | Eli lilly | 2023 | Safe | Safe |
GLP-1RAs have pleiotropic actions with metabolic, renal, hepatic, and cardiovascular effects[57,58]. In addition to being effective anti-diabetic medications, GLP-1RAs also improve renal and cardiovascular outcomes, and have an anti-obesity effect[59]. Sattar et al[60] reported a reduction in major adverse cardiovascular events (i.e., cardiovascular death, non-fatal myocardial infarction, and non-fatal stroke), hospitalization for heart failure, and progression of chronic kidney disease. The currently commercialized GLP-1RAs with their uses are summarized in Table 2.
| Generic name | Trade name | Indications | Regimen | |||
| Type 2 diabetes mellitus | Obesity | Major adverse cardiovascular events reduction | ||||
| Adults | Pediatrics ≥ 10 years | |||||
| Exenatide1 | Bydureon® | Yes | Yes | Yes | 2 mg, s.c./week | |
| Byetta® | Yes | Yes | 0.01 mg s.c. twice a day | |||
| Liraglutide | Victoza® | Yes | Yes | Yes | 1.2 mg, 1.8 mg s.c. QD | |
| Saxenda® | Yes | Yes | 3 mg, s.c. QD | |||
| Semaglutide | Ozempic® | Yes | Yes | 0.5 mg, 1.0 mg, 2.0 mg, s.c./week | ||
| Rybelsus® | Yes | Yes | 7 mg, 14 mg, oral QD | |||
| Wegovy® | Yes | Yes | 2.4 mg s.c./week | |||
| Lixisenatide2 | Lyxumia® | Yes | 0.02 mg s.c. QD | |||
| Dulaglutide | Trulicity® | Yes | Yes | 0.75 mg (monotherapy), 1.5 mg (add-on therapy) s.c./week | ||
| Tirzepatide3 | Zepbound® | Yes | Yes | 2.5 mg, 5 mg, 10 mg, 15 mg, s.c./week | ||
GLP-1RAs trials in obese T2DM patients revealed a significant association between GLP-1RAs and a mean weight loss of -1 kg to -4.4 kg after 3 months to 4 months of treatment in overweight T2DM patients[37,61,62]. This opened the door for investigating the first non-oral weight loss GLP-1RA, liraglutide (saxenda) as a monotherapy for weight loss. Liraglutide was approved for the treatment of chronic weight management as an adjunct to behavioral therapy, although with a higher starting dose compared to that used in the treatment of T2DM. Liraglutide’s effect on weight is primarily mediated through decreased energy intake[63]. Anti-obesity GLP1-RAs are indicated for patients who are obese with BMI ≥ 30 kg/m2, or overweight with BMI ≥ 27 kg/m2 and at least one weight-related comorbid condition (i.e., T2DM, dyslipidemia, or HTN)[64,65]. Semaglutide is the only GLP-1RA available in both oral tablet (rybelsus) and injections[66]. Several randomized controlled trials (RCTs) investigated the effect of GLP-1RAs on weight loss in adults with obesity and without diabetes mellitus (Table 3)[67-82].
| Ref. | Design | Regimen | Number of participants | Number of centers | Duration (weeks) | BMI (kg/m2) | Glycated hemoglobin | Results and NNT for ≥ 5% weight loss | Conclusion |
| Garvey et al[67] | Phase 3 randomized, double-blind, placebo-controlled trial to evaluate the efficacy and safety of tirzepatide once weekly for chronic weight management in adults with a BMI of 27 kg/m2 of higher who have T2DM | Tirzepatide (10 mg/week, or 15 mg/week) | 938 | 77 | 72 | 36 | 8% | Change in body weight: Tirzepatide 10 mg: 12.8% (-12.9 kg); tirzepatide 15 mg: 14.7% (-14.8 kg); placebo: 3.2% (-3.2 kg). Percentage of patients that lost at least 5% of body weight: Tirzepatide 10 mg: 79%; tirzepatide 15 mg: 83%; placebo: 32%. NNT for achieving ≥ 5% weight loss: Tirzepatide 10 mg vs placebo: 3; tirzepatide 15 mg vs placebo: 2 | Tirzepatide 10 mg, or 15 mg once weekly provided substantial and clinically meaningful reductions in body weight over 72 weeks in adults with obesity and T2DM, with a safety profile that was similar to other incretin-based therapies for weight management |
| Jastreboff et al[68] | A 72-week, phase 3 randomized, double-blind, placebo-controlled trial to evaluate the efficacy and safety of tirzepatide in adults without T2DM who were obese (BMI 30 kg/m2 or greater) or overweight (BMI 27 to less than 30 kg/m2) with at least 1 weight-related comorbid condition | Tirzepatide (5 mg/week, 10 mg/week, or 15 mg/week) | 2539 | 119 | 72 | 38 | 5.6% | Change in body weight: Tirzepatide 5 mg: 15% (95%CI: -15.9 to -14.2); tirzepatide 10 mg: 19.5% (95%CI: -20.4 to -18.5); tirzepatide 15 mg: 20.9% (95%CI: -21.8 to -19.9); placebo: 3.1% (95%CI: -4.3 to -1.9). Percentage of patients that lost at least 5% of body weight: Tirzepatide 5 mg: 85% (95%CI: 82-89); tirzepatide 10 mg: 89% (95%CI: 86-92); tirzepatide 15 mg: 91% (95%CI: 88-94); placebo: 35% (95%CI: 30-39). NNT for achieving ≥ 5% weight loss: Tirzepatide 5 mg, 10 mg, 15 mg: 2 | Tirzepatide 5 mg, 10 mg, or 15 mg once weekly provided substantial reductions in body weight over 72 weeks in adults with obesity |
| Wilding et al[69] | Four 68-week randomized, double-blind control trials comparing efficacy and safety of semaglutide 2.4 mg for weight management in patients with a BMI of at least 30 without T2DM, a BMI 27 or more without T2DM with at least 1 weight-related comorbidity, or a BMI 27 or more with T2DM | Semaglutide 24 mg/week | 1961 | 129 | 68 | 38 | 5.7% | Mean change in body weight: Semaglutide vs placebo: -9.6% to | Compared to placebo, semaglutide significantly reduced overall body weight, with weight loss of at least 5% and up to 15% of initial weight. The most common adverse events with semaglutide were nausea and vomiting; a dose escalation period is required |
| Wadden et al[70] | 611 | 41 | 38 | 5.7% | |||||
| Davies et al[71] | 1210 | 149 | 36 | 8.1% | |||||
| Rubino et al[72] | 902 | 73 | 38% | 5.7% | |||||
| O'Neil et al[73] | A 52-week, double-blind, placebo and active controlled, multicenter, dose-ranging, phase 2 trial, comparing efficacy and safety of semaglutide with liraglutide and placebo for weight management in adults (≥ 18 years) without diabetes and with a BMI of 30 kg/m² or more | Semaglutide 0.4 mg/day and 0.4 mg/day fast dose escalation, liraglutide 30 mg/day | 957 | 71 | 52 | 39 | 5.5% | Mean change in body weight: Mean changes at week 59 for semaglutide escalated on the 4-weekly schedule were -4.9% (SD = 6.2; 0.05 mg) to | Compared to placebo and liraglutide, semaglutide significantly reduced overall body weight, with no new safety concerns. The most common adverse events were dose-related gastrointestinal symptoms, primarily nausea |
| Pi-Sunyer et al[74] | A 56-week, double-blind trial comparing efficacy and safety of liraglutide 3 mg for weight management in patients with a BMI of at least 30 without T2DM or a BMI of 27 or more if they had treated or untreated dyslipidemia or hypertension | Liraglutide 30 mg/day | 3731 | 191 | 56 | 38 | 5.6% | Mean weight loss: liraglutide: -5.6 kg (95%CI: -6 to -5.1) | Compared to placebo, liraglutide significantly reduced overall body weight, with weight loss of at least 5% and up to 10% or more of initial weight. The most common adverse events with liraglutide were mild or moderate nausea, diarrhea and vomiting; a dose escalation period is required. Serious events occurred in 6.2% of the patients in the liraglutide group vs 5% in the placebo group |
| le Roux et al[75] | A 160-week randomized, double-blind, placebo-controlled trial comparing liraglutide 3 mg with placebo for T2DM risk reduction and weight management in adults with prediabetes and a body-mass index of at least 30 kg/m², or at least 27 kg/m² with comorbidities | Liraglutide 30 mg/day | 2254 | 191 | 160 | 39 | 5.8% | Mean change in body weight: Mean changes at week 160 for liraglutide was -6.5 (SD = 8.1) and for placebo was -2.0 (SD = 7.3). Percentage of patients that lost at least 5% of body weight: Liraglutide vs placebo: 49.6% vs 23.7%. NNT for achieving ≥ 5% weight loss: Liraglutide vs placebo: 4 | Compared to placebo, liraglutide induced greater weight loss than placebo at week 160 [-6.1 (SD = 7.3)] vs -1.9% (SD = 6.3); estimated treatment difference -4.3%, 95%CI: -4.9 to -3.7, P < 0.0001 |
| Astrup et al[76] | A 20-week randomized, double-blind, placebo-controlled trial comparing liraglutide with placebo and orlistat for treatment of obesity in obese individuals without T2DM | Liraglutide 12 mg/day, 1.8 mg/day, 2.4 mg/day, or 3.0 mg/day | 564 | 19 | 20 | 35 | - | Mean change in body weight: Mean changes at week 20 for liraglutide 12 mg was: -4.8 | Compared to placebo and orlistat, liraglutide treatment over 20 weeks is well tolerated, induces weight loss, improves certain obesity-related risk factors, and reduces prediabetes. Nausea and vomiting occurred more often in individuals on liraglutide than in those on placebo, but adverse events were mainly transient and rarely led to discontinuation of treatment |
| Astrup et al[77] | A 52-week randomized, double-blind, placebo-controlled trial comparing liraglutide with placebo and orlistat for treatment of obesity | Liraglutide 30 mg/day | 398 | 19 | 52 | - | - | Mean change in body weight: Mean changes for liraglutide 12 mg was: -3.8; liraglutide 18 mg: | Compared to placebo and orlistat, liraglutide is well tolerated, sustains weight loss over 2 years and improves cardiovascular risk factors. The most frequent drug-related side effects were mild to moderate, transient nausea and vomiting |
| Blackman et al[78] | A 32-week randomized, double-blind, placebo-controlled trial comparing the effect of liraglutide with placebo in reducing OSA severity and treatment of obesity in non-diabetic individuals with obesity and moderate or severe OSA | Liraglutide 30 mg/day | 359 | 40 | 32 | 39 | 5.7% | Mean change in body weight: Mean change for liraglutide 3 mg: | Compared to placebo and orlistat, liraglutide 30 mg was generally well tolerated and produced significantly greater reductions than placebo. The results confirm that weight loss improves OSA-related parameters |
| Kim et al[79] | A 14-week randomized, double-blind, placebo-controlled trial to evaluate the ability of liraglutide to augment weight loss and improve insulin resistance, CVD risk factors, and inflammation in a high-risk population for T2DM and CVD | Liraglutide 18 mg/day | 68 | 1 | 14 | 32 | - | Mean change in body weight: Mean change for liraglutide 18 mg: | Compared to placebo, the addition of liraglutide 18 mg to calorie restriction significantly augmented weight loss and improved insulin resistance, systolic blood pressure, glucose, and triglyceride concentration in this population at high risk for development of T2DM and CVD |
| Rosenstock et al[80] | A 24-week randomized, placebo-controlled trial to assess the effects of exenatide on body weight and glucose tolerance in nondiabetic obese subjects with normal or IGT or IFG | Exenatide 10 μg/day | 152 | - | 24 | 39 | - | Mean change in body weight: Mean change for exenatide with nausea: -5.1 (SD = 0.5), placebo: -1.6 (SD = 0.5). Percentage of patients that lost at least 5% of body weight: Exenatide vs placebo: 32% vs 17%. NNT for achieving ≥ 5% weight loss: Exenatide vs placebo: 7 | Compared to placebo, the addition of exenatide to lifestyle modification decreased caloric intake and resulted in weight loss in nondiabetic obesity with improved glucose tolerance in subjects with IGT and IFG |
| Dushay et al[81] | A 35-week randomized, double-blind, placebo-controlled, crossover study, including two 16-week treatment periods separated by a 3-week wash-out period to investigate the effect of exenatide on weight loss and metabolic parameters in obese nondiabetic women | Exenatide 10 μg/day | 41 | 1 | 35 | 33 | - | Mean change in body weight: Mean change for exenatide: -2.49 (SD = 0.66); placebo: +0.43 (SD = 0.63). Percentage of patients that lost at least 5% of body weight: Exenatide vs placebo: 30% vs 17%. NNT for achieving ≥ 5% weight loss: Exenatide vs placebo: 8 | Compared to placebo, short-term exenatide treatment was associated with modest weight loss and decreased waist circumference in a cohort of obese nondiabetic women. A subset of individuals demonstrated robust weight loss that was detected very early in treatment. Subjects experienced more nausea during exenatide treatment compared with placebo, but the severity decreased over time and did not correlate with weight loss |
| Pratley et al[82] | A 20-week phase II, randomized, placebo-controlled, double-blind trial to evaluate the safety of efpeglenatide and its effects on body weight management in adults without diabetes | Efpeglenatide 6 mg/week | 295 | - | 20 | 35 | 5.5% | Mean change in body weight: Mean change for efpeglenatide 4 mg once weekly: -6.6 (SD = 0.6); efpeglenatide 6 mg once weekly: -7.3 (SD = 0.6); efpeglenatide 6 mg once every 2 weeks: -6.4 (SD = 0.6); efpeglenatide 8 mg once every 2 weeks: -7.1 (SD = 0.6); placebo: -0.1 (SD = 0.6). Percentage of patients that lost at least 5% of body weight: Efpeglenatide 4 mg once weekly: 48%; efpeglenatide 6 mg once weekly: 51%; efpeglenatide 6 mg once every 2 weeks: 46%; efpeglenatide 8 mg once every 2 weeks: 53%; placebo: 3%. NNT for achieving ≥ 5% weight loss: Efpeglenatide 4 mg weekly: 3; efpeglenatide 6 mg weekly: 3; efpeglenatide 6 mg every 2 weeks: 3; efpeglenatide 8 mg every 2 weeks: 2 | Efpeglenatide once weekly and once every 2 weeks led to significant body weight reduction and improved glycaemic and lipid variables vs placebo. It was also well tolerated for weight management in adults without diabetes |
The exact weight loss mechanism of GLP-1RAs is still not clear. However, it has been reported that GI adverse events associated with GLP-1RAs are likely to have desirable outcomes favoring anorexia and subsequent weight loss. Lean et al[83] reported that liraglutide-treated greater weight loss in patients who experienced at least one episode of nausea or vomiting compared to those who did not experience any such side effects. Another contributing factor to the cumulative weight loss of liraglutide was the following liraglutide-induced effects: (1) Increased satiety and fullness; (2) Decreased hunger; and (3) Slowed gastric emptying[63]. These CNS effects were postulated to be due to the activation of GLP-1RAs in satiety centers in the CNS. This was supported by the finding of radiolabeled liraglutide in the arcuate nucleus following subcutaneous liraglutide administration with higher doses than those used for T2DM treatment[84].
Tirzepatide (zepbound), a novel dual GIP/GLP-1RA has emerged. Dual GIP/GLP-1RA binds both GIP and GLP-1RAs, with more tendency to bind GIP receptors. GIP stimulates insulin secretion, inhibits lipolysis, promotes lipogenesis, and inhibits gastric secretion activity. The effects of GIP along with the satiating effects of GLP-1 add to desired weight-loss outcome[85-87]. This explains why tirzepatide is associated with greater weight loss than other anti-diabetic medications. Tirzepatide achieved greater weight loss (-20.9%) than semaglutide (-14.9%) but higher nausea rates (29% vs 15%)[54,67,88-90].
Tirzepatide is indicated for patients who are obese with BMI ≥ 30 kg/m2 or overweight with BMI ≥ 27 kg/m2 and at least one weight-related comorbid condition (i.e., T2DM, dyslipidemia, or HTN, obstructive sleep apnea or cardiovascular diseaes)[91]. The SURMOUNT-2 trial demonstrated tirzepatide’s superior weight loss (-14.7% to -20.9%) in T2DM patients[67,92,93] in the SURMOUNT-4 trial, the overall mean weight reduction from week 0 to 88 was 25.3% for tirzepatide and 9.9% for placebo[94].
With the use of GLP-1RAs in clinical practice, several adverse events have been reported, most of which were GI (Table 4)[95,96]. Other reported adverse events included acute pancreatitis, cholelithiasis and cholecystitis, angioedema/anaphylaxis, injection site reactions, acute kidney injury (AKI), drug-induced immune thrombocytopenia (DITP), and thyroid C cell tumor.
| Adverse events | Exenatide (%) | Liraglutide (%) | Semaglutide (%) | Dulaglutide (%) | Lixisenatide (%) | Tirzepatide (%) |
| Abdominal pain | Reported | 5.40 | 5.7-20 | 6.5-9.4 | 2-2.2 | 5-10 |
| Biliary diseases | 1.99 | 2.22 | 0.52 | 1.55 | 0.78 | - |
| Antibody formation | 6-64 | < 12 | 0.5-3 | 1.6-6 | 2.40 | 51-64.5 |
| Constipation | 2.10 | 4.8-19.4 | 3.1-24 | 3.7-3.9 | 2.80 | 6-17 |
| Diarrhea | 6-18 | 9.3-22.4 | 8.5-30 | 8.9-12.6 | 8 | 12-23 |
| Hypoglycemia | 1.7-5.2 | 1.6-24.2 | 1-6 | Reported | 2 | 0.3-4.2 |
| Injection site reaction | 1.6-23.9 | 2-13.9 | 0.2-1.4 | 0.5-3.9 | 4 | 3.2-8 |
| Nausea | 8-44 | 23.9-42.4 | 11-44 | 12.4-21.1 | < 25 | 12-29 |
| Vomiting | 3.4-13 | 8.7-34.4 | 5-36 | 6-12.7 | < 10 | 5-13 |
| Dizziness | 2.5-9 | 5.8-12.1 | 0.4-8 | - | 7 | 4-5 |
| Anorexia | 1-2 | 10 | - | 4.9-8.6 | - | 5-11 |
| Fatigue | - | 4.8-7.5 | 0.4-11 | 4.2-5.6 | - | 5-7 |
| Fever | - | 8 | - | - | - | - |
| Pharyngitis | - | - | 12 | - | - | - |
GI disorders were the most common side effects in GLP-1RAs clinical trials[97]. Among GI symptoms[98-102], nausea[103], diarrhea, vomiting, constipation, abdominal pain, and dyspepsia are common[104-108]. A network meta-analysis of 236 clinical studies found that GLP-1RAs were linked to severe adverse events resulting in treatment discontinuation more often than other oral anti-diabetic medications[109]. Treatment interruption has been reported in up to 12% of GLP-1RA-treated patients while treatment discontinuation has been reported in 1.6%-6% of GLP-1RA treated patients[110-112]. On contrast, Wharton et al[112] reported that the 99.5% of GLP-1RA-induced GI adverse events were non-serious. In general, GI adverse events are transient, starting during the dose-escalation period, and resolving shortly after the maintenance dose is reached.
When used as anti-obesity agents, GLP-1RAs have been associated with more severe adverse effects, including obstruction and symptomatic gastroparesis[113]. A meta-analysis reported that the most frequent adverse events with GLP-1 were pancreatitis and acute gallbladder disease[114]. Nausea is the most frequent adverse event with exenatide once weekly. Patients on short-acting GLP-1RA experience higher rates of GI adverse events than those on long-acting GLP-1RA. Studies have reported a less frequent exenatide-induced nausea with once-weekly than with twice-daily administration (26% vs 50%) and also less frequently than with liraglutide (9% vs 21%)[102,115]. Long-acting GLP-1RAs exert a sustained effect on intestinal GLP-1RAs leading to more diarrhea and less nausea and vomiting[116,117]. Patients with estimated glomerular filtration rate > 60 mL/minute/1.73 m2 and gastroparesis are more likely to suffer GI adverse effects with exenatide once weekly[118].
Regarding semaglutide, Rosenstock et al[119] reported nausea, vomiting, and diarrhea in 15%, 9%, and 12.3%, respec
Tirzepatide clinical trials for weight management showed GI adverse effects among patients receiving tirzepatide than placebo leading to higher discontinuation rates among patients receiving tirzepatide. The GI adverse effects included, nausea (25%-29%), vomiting (8%-13%), and diarrhea (19%-23%)[67,68].
The GLP-1-induced delay in gastric transit can impact the quality of bowel preparation for procedures such as colo
Several studies have indicated that delayed gastric emptying and associated GI adverse events may pose risks during endoscopic examinations. Imam et al[93] highlighted that incorporating GLP-1RAs alongside bariatric therapies has shown promise in weight loss but emphasized the necessity of considering GI motility effects when planning surgical interventions, including endoscopic examinations.
Additionally, a retrospective study by Ghazanfar et al[124] raised questions about the necessity of temporarily discontinuing GLP-1 therapy before endoscopic procedures, as long-acting GLP-1RAs, such as liraglutide and dulaglutide, have prolonged effects on GI function. This withdrawal could reduce adverse GI events that might complicate endoscopy and improve the quality of procedures.
GLP-1RAs have been associated with acute pancreatitis[113,125]. GLP-1RAs should never be initiated in patients with a history of pancreatitis, and if a patient on GLP-1RAs developed persistent severe abdominal pain, pancreatitis should be suspected and GLP-1RAs should be stopped and never restarted. Retrospective cohort studies and meta-analyses of RCTs[126] reported that GLP-1RAs-induced pancreatitis usually does not increase the risk of hospitalization[127-131]. However, a large population-based case-control study revealed that exenatide and sitagliptin were associated with an increased risk of hospitalization for acute pancreatitis (adjusted odds ratio = 2.07, 95%CI: 1.36-3.13)[132].
Some studies reported an increase in pancreatic amylase and lipase from baseline levels, although remaining within the normal ranges[121,133]. Steinberg et al[134] reported isolated elevations of lipase and amylase levels above the upper limit in the liraglutide and placebo groups (51% and 32% of participants, respectively, for lipase and 29% and 23%, respectively, for amylase) with no association with subsequent acute pancreatitis.
Some case reports showed an increased risk of pancreatic cancer, neuroendocrine tumors, and subclinical pancreatic inflammation in exenatide users[125,135-137]. However, the United States Food and Drug Administration and the European Medicines Agency concluded that there was insufficient evidence to confirm an increased risk of pancreatic cancer with the use of GLP-1-based therapies[138].
Gallbladder and biliary diseases including cholelithiasis and cholecystitis have been associated with GLP-1RAs. A meta-analysis of 76 randomized clinical trials showed an increased risk of the composite outcome of gallbladder or biliary diseases (event rate 1.58% vs 1.19%, relative risk = 1.37, 95%CI: 1.23-1.52)[139]. A post-marketing report has shown an elevated risk of acute cholecystitis with GLP-1RAs[140]. If cholelithiasis or cholecystitis are suspected, gallbladder studies are indicated.
Angioedema/anaphylaxis: There are some reports of angioedema and anaphylaxis with GLP-1RAs[141,142]. The under
Injection site reactions including abscess, cellulitis, and necrosis have been reported with GLP-1RA. When compared with insulin injections, once-weekly GLP-1RAs, especially albiglutide, and exenatide, appear to be more associated with injection site reactions compared to insulin (10% vs 1%-5%)[144,145]. Studies have shown injection site reactions were more common with exenatide once weekly or albiglutide than lirglutide[102,146].
Immunogenicity: Antibodies against GLP-1RAs have been reported. However, no significant clinical safety concerns have been confirmed[147].
Kidney: Several studies reported AKI with exenatide twice daily[121,149-151]. The AKI is usually driven by dehydration from the GI symptoms initially caused by GLP-1RAs. AKI has also been reported with liraglutide and semaglutide[152,153]. A kidney biopsy may be considered if the diagnosis remains unclear.
DITP: Exenatide has been associated with DITP[154]. In a case report, prolonged, severe thrombocytopenia resulted from the persistence of the drug at levels sufficient to permit binding of the patient's drug-dependent, platelet-reactive immunoglobulin G anti-body to platelets for more than 6 weeks after discontinuing treatment due to immune memory mechanisms[154]. Once DITP is suspected, Exenatide should be discontinued and never restarted.
Thyroid C cell tumors: Recent studies have yielded conflicting results regarding the association between GLP-1RAs and thyroid cancer risk. A Scandanavian cohort study evaluated thyroid cancer risk in patients on GLP-1RA, particularly liraglutide and semaglutide, compared to DPPI-4 and showed no association between GLP-1RA and risk of any thyroid cancer [hazard ratio (HR) = 0.93, 95%CI: 0.66-1.31] or medullary thyroid cancer (HR = 1.19, 95%CI: 0.37-3.86)[155]. In contrast, a study based on the French national health care insurance system database found an increased risk of all thyroid cancer and medullary thyroid cancer with use of GLP-1RA, in particular after 1-3 years of treatment[156].
Animal studies have shown that liraglutide and dulaglutide were associated with thyroid C cell tumors[157]. Also, exenatide and liraglutide were associated with stimulation of calcitonin release[157,158]. There is no clear evidence of similar effects in humans. This may be due to the fact that humans have fewer c with low GLP-1R expression[157]. These findings highlight the need for continued monitoring and research on this potential safety concern.
In general, GLP-1RA and dual GIP/GLP-1RA are contraindicated in patients with a personal or family history of thyroid C cell tumors such as medullar thyroid carcinoma (MTC), or in patients with multiple endocrine neoplasia syndrome type 2 (MEN 2). Routine monitoring of serum calcitonin is not recommended; however, if measured and found elevated, the patient should be referred to an endocrinologist.
GLP-1RAs share several contraindications rooted in clinical and preclinical evidence. Absolute contraindications for exenatide, liraglutide, semaglutide, dulaglutide, and tirzepatide include a personal or family history of MTC or MEN 2, conditions linked to thyroid C-cell tumorigenesis in animal studies[159]. Additionally, a history of idiopathic pancreatitis (pancreatitis of unknown etiology) precludes their use, given concerns about exacerbating pancreatic inflammation[160]. Pregnancy is considered an absolute contraindication for liraglutide, semaglutide, and trizepatide. For trizepatide, hypersensitivity reactions are considered an absolute contraindication.
Relative contraindications for liraglutide, semaglutide, and tirzepatide include gastroparesis, as their mechanism of delaying gastric emptying may worsen symptoms such as nausea and vomiting. Similarly, severe gastroesophageal reflux disease may be aggravated by slowed GI motility. For liraglutide, there is a potential increased risk of acute pancreatitis and pancreatic cancer; thus, close monitoring is required[161,162]. For semaglutide, close monitoring and risk/benefit assessment are required in patients with diabetic retinopathy, gallbladder dysfunction, and acute pancreatitis. For tirzepatide, close monitoring and risk/benefit assessment are required in patients with gallbladder dysfunction and diabetic retinopathy.
It is crucial to educate patients about the common GI side effects associated with medications such as tirzepatide, semaglutide, and liraglutide, including nausea, diarrhea, and constipation. Studies like Get-Goal-M[103], STEP-1 trial[69], STEP-3 trial[70], SURMOUNT-1[68] indicate that these side effects can lead to treatment discontinuation in a notable percentage of patients.
Encouraging patients to report any adverse effects early and reassuring them that many GI symptoms are mild to moderate and often improve over time can help manage patient expectations and improve adherence.
Initiating treatment with a lower dose and gradually increasing it can help mitigate GI side effects.
Pharmacological options: For patients experiencing nausea or diarrhea, prescribing antiemetics or antidiarrheal agents may provide relief. These medications can help manage symptoms effectively, allowing patients to continue their treatment regimen.
Non-pharmacological strategies: Dietary adjustments, such as consuming smaller, more frequent meals and avoiding high-fat or spicy foods, can alleviate GI discomfort. Behavioral modifications, including gradual dose escalation and maintaining hydration, are also beneficial in managing symptoms.
Treatment should be reconsidered if patients experience severe GI symptoms that lead to significant distress or inability to maintain adequate nutrition. For example, if nausea or diarrhea leads to dehydration or weight loss, discontinuation may be necessary.
If treatment discontinuation occurs, it is essential to evaluate alternative therapies or adjust the current treatment plan. This may involve switching to a different medication with a more favorable side effect profile or considering non-pharmacological interventions for weight management.
Potential developments in GLP-1RA formulations aimed at minimizing GI effects are critical for enhancing patient adherence and overall therapeutic outcomes.
These developments could focus on providing long-acting GLP-1RAs that necessitate less frequent dosing and have shown promise in reducing GI side effects. For instance, formulations such as semaglutide, dulaglutide, exenatide extended-release, albiglutide, and tirzepatide, which are administered once weekly, have demonstrated improved patient adherence and a more gradual onset of side effects compared to their shorter-acting counterparts. This extended-release mechanism may allow for a more stable pharmacokinetic profile, thereby mitigating the intensity of GI disturbances commonly associated with GLP-1 therapy[163]. However, complications of long acting formulations should be put into consideration including: (1) Cumulative toxicity; and (2) Immunogenicity risks.
Moreover, future research may focus on improving the bioavailability and therapeutic efficacy of GLP-1RAs via molecular modifications and targeted delivery systems[164]. This could lead to formulations that are more effective while causing fewer GI disturbances, thereby improving the overall patient experience with GLP-1 therapy. Additionally, genetic studies are needed to predict GI tolerability and personalize therapy
GLP-1RAs are novel anti-obesity medications that come with some adverse events, particularly GI adverse events. Physicians should prescribe GLP-1RAs with particular attention to the absolute and relative contraindications and possible adverse events in a patient-customized approach. In this regard, future studies are needed to enhance patient safety, mitigate side effects, and improve treatment outcomes for GLP-1RAs as anti-obesity medications.
| 1. | Misra A, Khurana L. Obesity and the metabolic syndrome in developing countries. J Clin Endocrinol Metab. 2008;93:S9-30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 618] [Cited by in RCA: 675] [Article Influence: 37.5] [Reference Citation Analysis (0)] |
| 2. | Finucane MM, Stevens GA, Cowan MJ, Danaei G, Lin JK, Paciorek CJ, Singh GM, Gutierrez HR, Lu Y, Bahalim AN, Farzadfar F, Riley LM, Ezzati M; Global Burden of Metabolic Risk Factors of Chronic Diseases Collaborating Group (Body Mass Index). National, regional, and global trends in body-mass index since 1980: systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9.1 million participants. Lancet. 2011;377:557-567. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3177] [Cited by in RCA: 2969] [Article Influence: 197.9] [Reference Citation Analysis (1)] |
| 3. | Jackson VM, Breen DM, Fortin JP, Liou A, Kuzmiski JB, Loomis AK, Rives ML, Shah B, Carpino PA. Latest approaches for the treatment of obesity. Expert Opin Drug Discov. 2015;10:825-839. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 86] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 4. | Bray GA. Evaluation of obesity. Who are the obese? Postgrad Med. 2003;114:19-27, 38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 33] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 5. | Chung W, Park CG, Ryu OH. Association of a New Measure of Obesity with Hypertension and Health-Related Quality of Life. PLoS One. 2016;11:e0155399. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 29] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 6. | Wu S, Wang R, Jiang A, Ding Y, Wu M, Ma X, Zhao Y, He J. Abdominal obesity and its association with health-related quality of life in adults: a population-based study in five Chinese cities. Health Qual Life Outcomes. 2014;12:100. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 30] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 7. | Prospective Studies Collaboration, Whitlock G, Lewington S, Sherliker P, Clarke R, Emberson J, Halsey J, Qizilbash N, Collins R, Peto R. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet. 2009;373:1083-1096. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3582] [Cited by in RCA: 3354] [Article Influence: 197.3] [Reference Citation Analysis (0)] |
| 8. | Danaei G, Ding EL, Mozaffarian D, Taylor B, Rehm J, Murray CJ, Ezzati M. The preventable causes of death in the United States: comparative risk assessment of dietary, lifestyle, and metabolic risk factors. PLoS Med. 2009;6:e1000058. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1230] [Cited by in RCA: 1285] [Article Influence: 75.6] [Reference Citation Analysis (0)] |
| 9. | World Health Organization. Obesity. 2024. [cited 23 June 2025]. Available from: https://www.who.int/data/gho/indicator-metadata-registry/imr-details/3420. |
| 10. | Vaamonde JG, Álvarez-món M. Obesidad y sobrepeso. Med Programa Form Méd Contin Acredit. 2020;13:767-776. [DOI] [Full Text] |
| 11. | Kelly T, Yang W, Chen CS, Reynolds K, He J. Global burden of obesity in 2005 and projections to 2030. Int J Obes (Lond). 2008;32:1431-1437. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1843] [Cited by in RCA: 2121] [Article Influence: 117.8] [Reference Citation Analysis (2)] |
| 12. | NCD Risk Factor Collaboration (NCD-RisC). Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 19.2 million participants. Lancet. 2016;387:1377-1396. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4095] [Cited by in RCA: 3640] [Article Influence: 364.0] [Reference Citation Analysis (0)] |
| 13. | Collaboration NRF. Data Visualisations. [cited 23 June 2025]. Available from: https://ncdrisc.org/data-visualisations.htm. |
| 14. | Hawkes C. Uneven dietary development: linking the policies and processes of globalization with the nutrition transition, obesity and diet-related chronic diseases. Global Health. 2006;2:4. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 421] [Cited by in RCA: 407] [Article Influence: 20.4] [Reference Citation Analysis (0)] |
| 15. | Kearney J. Food consumption trends and drivers. Philos Trans R Soc Lond B Biol Sci. 2010;365:2793-2807. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1260] [Cited by in RCA: 799] [Article Influence: 49.9] [Reference Citation Analysis (0)] |
| 16. | Popkin BM. Global nutrition dynamics: the world is shifting rapidly toward a diet linked with noncommunicable diseases. Am J Clin Nutr. 2006;84:289-298. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 361] [Article Influence: 18.1] [Reference Citation Analysis (0)] |
| 17. | Swinburn BA, Sacks G, Hall KD, McPherson K, Finegood DT, Moodie ML, Gortmaker SL. The global obesity pandemic: shaped by global drivers and local environments. Lancet. 2011;378:804-814. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2895] [Cited by in RCA: 3043] [Article Influence: 202.9] [Reference Citation Analysis (0)] |
| 18. | GBD 2015 Obesity Collaborators; Afshin A, Forouzanfar MH, Reitsma MB, Sur P, Estep K, Lee A, Marczak L, Mokdad AH, Moradi-Lakeh M, Naghavi M, Salama JS, Vos T, Abate KH, Abbafati C, Ahmed MB, Al-Aly Z, Alkerwi A, Al-Raddadi R, Amare AT, Amberbir A, Amegah AK, Amini E, Amrock SM, Anjana RM, Ärnlöv J, Asayesh H, Banerjee A, Barac A, Baye E, Bennett DA, Beyene AS, Biadgilign S, Biryukov S, Bjertness E, Boneya DJ, Campos-Nonato I, Carrero JJ, Cecilio P, Cercy K, Ciobanu LG, Cornaby L, Damtew SA, Dandona L, Dandona R, Dharmaratne SD, Duncan BB, Eshrati B, Esteghamati A, Feigin VL, Fernandes JC, Fürst T, Gebrehiwot TT, Gold A, Gona PN, Goto A, Habtewold TD, Hadush KT, Hafezi-Nejad N, Hay SI, Horino M, Islami F, Kamal R, Kasaeian A, Katikireddi SV, Kengne AP, Kesavachandran CN, Khader YS, Khang YH, Khubchandani J, Kim D, Kim YJ, Kinfu Y, Kosen S, Ku T, Defo BK, Kumar GA, Larson HJ, Leinsalu M, Liang X, Lim SS, Liu P, Lopez AD, Lozano R, Majeed A, Malekzadeh R, Malta DC, Mazidi M, McAlinden C, McGarvey ST, Mengistu DT, Mensah GA, Mensink GBM, Mezgebe HB, Mirrakhimov EM, Mueller UO, Noubiap JJ, Obermeyer CM, Ogbo FA, Owolabi MO, Patton GC, Pourmalek F, Qorbani M, Rafay A, Rai RK, Ranabhat CL, Reinig N, Safiri S, Salomon JA, Sanabria JR, Santos IS, Sartorius B, Sawhney M, Schmidhuber J, Schutte AE, Schmidt MI, Sepanlou SG, Shamsizadeh M, Sheikhbahaei S, Shin MJ, Shiri R, Shiue I, Roba HS, Silva DAS, Silverberg JI, Singh JA, Stranges S, Swaminathan S, Tabarés-Seisdedos R, Tadese F, Tedla BA, Tegegne BS, Terkawi AS, Thakur JS, Tonelli M, Topor-Madry R, Tyrovolas S, Ukwaja KN, Uthman OA, Vaezghasemi M, Vasankari T, Vlassov VV, Vollset SE, Weiderpass E, Werdecker A, Wesana J, Westerman R, Yano Y, Yonemoto N, Yonga G, Zaidi Z, Zenebe ZM, Zipkin B, Murray CJL. Health Effects of Overweight and Obesity in 195 Countries over 25 Years. N Engl J Med. 2017;377:13-27. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5669] [Cited by in RCA: 5382] [Article Influence: 598.0] [Reference Citation Analysis (3)] |
| 19. | Norris SL, Zhang X, Avenell A, Gregg E, Brown TJ, Schmid CH, Lau J. Long-term non-pharmacologic weight loss interventions for adults with type 2 diabetes. Cochrane Database Syst Rev. 2005;2005:CD004095. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 62] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 20. | Franz MJ, VanWormer JJ, Crain AL, Boucher JL, Histon T, Caplan W, Bowman JD, Pronk NP. Weight-loss outcomes: a systematic review and meta-analysis of weight-loss clinical trials with a minimum 1-year follow-up. J Am Diet Assoc. 2007;107:1755-1767. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 944] [Cited by in RCA: 1068] [Article Influence: 56.2] [Reference Citation Analysis (8)] |
| 21. | Gourlan MJ, Trouilloud DO, Sarrazin PG. Interventions promoting physical activity among obese populations: a meta-analysis considering global effect, long-term maintenance, physical activity indicators and dose characteristics. Obes Rev. 2011;12:e633-e645. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 48] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 22. | Li M, Cheung BM. Pharmacotherapy for obesity. Br J Clin Pharmacol. 2009;68:804-810. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 61] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 23. | Rucker D, Padwal R, Li SK, Curioni C, Lau DC. Long term pharmacotherapy for obesity and overweight: updated meta-analysis. BMJ. 2007;335:1194-1199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 572] [Cited by in RCA: 515] [Article Influence: 27.1] [Reference Citation Analysis (0)] |
| 24. | Padwal R, Li SK, Lau DC. Long-term pharmacotherapy for obesity and overweight. Cochrane Database Syst Rev. 2003;CD004094. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 35] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 25. | Padwal R, Klarenbach S, Wiebe N, Birch D, Karmali S, Manns B, Hazel M, Sharma AM, Tonelli M. Bariatric surgery: a systematic review and network meta-analysis of randomized trials. Obes Rev. 2011;12:602-621. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 170] [Cited by in RCA: 178] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 26. | Pories WJ. Bariatric surgery: risks and rewards. J Clin Endocrinol Metab. 2008;93:S89-S96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 260] [Cited by in RCA: 254] [Article Influence: 14.1] [Reference Citation Analysis (0)] |
| 27. | Pontiroli AE, Morabito A. Long-term prevention of mortality in morbid obesity through bariatric surgery. a systematic review and meta-analysis of trials performed with gastric banding and gastric bypass. Ann Surg. 2011;253:484-487. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 208] [Cited by in RCA: 185] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 28. | Reja D, Zhang C, Sarkar A. Endoscopic bariatrics: current therapies and future directions. Transl Gastroenterol Hepatol. 2022;7:21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 16] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 29. | Ibrahim Mohamed BK, Barajas-Gamboa JS, Rodriguez J. Endoscopic Bariatric Therapies: Current Status and Future Perspectives. JSLS. 2022;26:e2021.00066. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 12] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 30. | Zhu J, Yan Y, Qiu X, Lin S, Wen J. Endoscopic bariatric surgery for adults with overweight and obesity: a systematic review and network meta-analysis. Int J Obes (Lond). 2025;49:237-245. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 31. | Jackson VM, Price DA, Carpino PA. Investigational drugs in Phase II clinical trials for the treatment of obesity: implications for future development of novel therapies. Expert Opin Investig Drugs. 2014;23:1055-1066. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 32. | Folli F, Guardado Mendoza R. Potential use of exenatide for the treatment of obesity. Expert Opin Investig Drugs. 2011;20:1717-1722. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 17] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 33. | Nathan PJ, O'Neill BV, Napolitano A, Bullmore ET. Neuropsychiatric adverse effects of centrally acting antiobesity drugs. CNS Neurosci Ther. 2011;17:490-505. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 80] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 34. | Scheen AJ. Cardiovascular risk-benefit profile of sibutramine. Am J Cardiovasc Drugs. 2010;10:321-334. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 52] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 35. | Kreymann B, Williams G, Ghatei MA, Bloom SR. Glucagon-like peptide-1 7-36: a physiological incretin in man. Lancet. 1987;2:1300-1304. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1228] [Cited by in RCA: 1316] [Article Influence: 33.7] [Reference Citation Analysis (0)] |
| 36. | Nauck MA, Quast DR, Wefers J, Meier JJ. GLP-1 receptor agonists in the treatment of type 2 diabetes - state-of-the-art. Mol Metab. 2021;46:101102. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 399] [Cited by in RCA: 1040] [Article Influence: 208.0] [Reference Citation Analysis (0)] |
| 37. | Garber AJ. Long-acting glucagon-like peptide 1 receptor agonists: a review of their efficacy and tolerability. Diabetes Care. 2011;34 Suppl 2:S279-S284. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 231] [Cited by in RCA: 254] [Article Influence: 16.9] [Reference Citation Analysis (0)] |
| 38. | Larsen PJ, Tang-Christensen M, Holst JJ, Orskov C. Distribution of glucagon-like peptide-1 and other preproglucagon-derived peptides in the rat hypothalamus and brainstem. Neuroscience. 1997;77:257-270. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 452] [Cited by in RCA: 518] [Article Influence: 17.9] [Reference Citation Analysis (0)] |
| 39. | Han VK, Hynes MA, Jin C, Towle AC, Lauder JM, Lund PK. Cellular localization of proglucagon/glucagon-like peptide I messenger RNAs in rat brain. J Neurosci Res. 1986;16:97-107. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 131] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 40. | Vrang N, Grove K. The brainstem preproglucagon system in a non-human primate (Macaca mulatta). Brain Res. 2011;1397:28-37. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 32] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 41. | Zheng H, Cai L, Rinaman L. Distribution of glucagon-like peptide 1-immunopositive neurons in human caudal medulla. Brain Struct Funct. 2015;220:1213-1219. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 30] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 42. | Bell GI, Sanchez-Pescador R, Laybourn PJ, Najarian RC. Exon duplication and divergence in the human preproglucagon gene. Nature. 1983;304:368-371. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 395] [Cited by in RCA: 409] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 43. | D'Alessio D. Is GLP-1 a hormone: Whether and When? J Diabetes Investig. 2016;7 Suppl 1:50-55. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 51] [Cited by in RCA: 98] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 44. | Drucker DJ. Mechanisms of Action and Therapeutic Application of Glucagon-like Peptide-1. Cell Metab. 2018;27:740-756. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 615] [Cited by in RCA: 1311] [Article Influence: 163.9] [Reference Citation Analysis (1)] |
| 45. | Campbell JE, Drucker DJ. Pharmacology, physiology, and mechanisms of incretin hormone action. Cell Metab. 2013;17:819-837. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 918] [Cited by in RCA: 1114] [Article Influence: 85.7] [Reference Citation Analysis (0)] |
| 46. | Nauck M, Stöckmann F, Ebert R, Creutzfeldt W. Reduced incretin effect in type 2 (non-insulin-dependent) diabetes. Diabetologia. 1986;29:46-52. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 942] [Cited by in RCA: 938] [Article Influence: 23.5] [Reference Citation Analysis (0)] |
| 47. | Luque MA, González N, Márquez L, Acitores A, Redondo A, Morales M, Valverde I, Villanueva-Peñacarrillo ML. Glucagon-like peptide-1 (GLP-1) and glucose metabolism in human myocytes. J Endocrinol. 2002;173:465-473. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 91] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 48. | Holst JJ, Vilsbøll T, Deacon CF. The incretin system and its role in type 2 diabetes mellitus. Mol Cell Endocrinol. 2009;297:127-136. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 373] [Cited by in RCA: 385] [Article Influence: 22.6] [Reference Citation Analysis (0)] |
| 49. | Butler AE, Janson J, Bonner-Weir S, Ritzel R, Rizza RA, Butler PC. Beta-cell deficit and increased beta-cell apoptosis in humans with type 2 diabetes. Diabetes. 2003;52:102-110. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3031] [Cited by in RCA: 3082] [Article Influence: 134.0] [Reference Citation Analysis (0)] |
| 50. | Wessel J, Chu AY, Willems SM, Wang S, Yaghootkar H, Brody JA, Dauriz M, Hivert MF, Raghavan S, Lipovich L, Hidalgo B, Fox K, Huffman JE, An P, Lu Y, Rasmussen-Torvik LJ, Grarup N, Ehm MG, Li L, Baldridge AS, Stančáková A, Abrol R, Besse C, Boland A, Bork-Jensen J, Fornage M, Freitag DF, Garcia ME, Guo X, Hara K, Isaacs A, Jakobsdottir J, Lange LA, Layton JC, Li M, Hua Zhao J, Meidtner K, Morrison AC, Nalls MA, Peters MJ, Sabater-Lleal M, Schurmann C, Silveira A, Smith AV, Southam L, Stoiber MH, Strawbridge RJ, Taylor KD, Varga TV, Allin KH, Amin N, Aponte JL, Aung T, Barbieri C, Bihlmeyer NA, Boehnke M, Bombieri C, Bowden DW, Burns SM, Chen Y, Chen YD, Cheng CY, Correa A, Czajkowski J, Dehghan A, Ehret GB, Eiriksdottir G, Escher SA, Farmaki AE, Frånberg M, Gambaro G, Giulianini F, Goddard WA 3rd, Goel A, Gottesman O, Grove ML, Gustafsson S, Hai Y, Hallmans G, Heo J, Hoffmann P, Ikram MK, Jensen RA, Jørgensen ME, Jørgensen T, Karaleftheri M, Khor CC, Kirkpatrick A, Kraja AT, Kuusisto J, Lange EM, Lee IT, Lee WJ, Leong A, Liao J, Liu C, Liu Y, Lindgren CM, Linneberg A, Malerba G, Mamakou V, Marouli E, Maruthur NM, Matchan A, McKean-Cowdin R, McLeod O, Metcalf GA, Mohlke KL, Muzny DM, Ntalla I, Palmer ND, Pasko D, Peter A, Rayner NW, Renström F, Rice K, Sala CF, Sennblad B, Serafetinidis I, Smith JA, Soranzo N, Speliotes EK, Stahl EA, Stirrups K, Tentolouris N, Thanopoulou A, Torres M, Traglia M, Tsafantakis E, Javad S, Yanek LR, Zengini E, Becker DM, Bis JC, Brown JB, Cupples LA, Hansen T, Ingelsson E, Karter AJ, Lorenzo C, Mathias RA, Norris JM, Peloso GM, Sheu WH, Toniolo D, Vaidya D, Varma R, Wagenknecht LE, Boeing H, Bottinger EP, Dedoussis G, Deloukas P, Ferrannini E, Franco OH, Franks PW, Gibbs RA, Gudnason V, Hamsten A, Harris TB, Hattersley AT, Hayward C, Hofman A, Jansson JH, Langenberg C, Launer LJ, Levy D, Oostra BA, O'Donnell CJ, O'Rahilly S, Padmanabhan S, Pankow JS, Polasek O, Province MA, Rich SS, Ridker PM, Rudan I, Schulze MB, Smith BH, Uitterlinden AG, Walker M, Watkins H, Wong TY, Zeggini E; EPIC-InterAct Consortium, Laakso M, Borecki IB, Chasman DI, Pedersen O, Psaty BM, Tai ES, van Duijn CM, Wareham NJ, Waterworth DM, Boerwinkle E, Kao WH, Florez JC, Loos RJ, Wilson JG, Frayling TM, Siscovick DS, Dupuis J, Rotter JI, Meigs JB, Scott RA, Goodarzi MO. Low-frequency and rare exome chip variants associate with fasting glucose and type 2 diabetes susceptibility. Nat Commun. 2015;6:5897. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 168] [Cited by in RCA: 167] [Article Influence: 15.2] [Reference Citation Analysis (0)] |
| 51. | Aroda VR. A review of GLP-1 receptor agonists: Evolution and advancement, through the lens of randomised controlled trials. Diabetes Obes Metab. 2018;20 Suppl 1:22-33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 145] [Cited by in RCA: 207] [Article Influence: 25.9] [Reference Citation Analysis (0)] |
| 52. | American Diabetes Association Professional Practice Committee. 9. Pharmacologic Approaches to Glycemic Treatment: Standards of Care in Diabetes-2024. Diabetes Care. 2024;47:S158-S178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 163] [Cited by in RCA: 421] [Article Influence: 210.5] [Reference Citation Analysis (1)] |
| 53. | Inzucchi SE, Bergenstal RM, Buse JB, Diamant M, Ferrannini E, Nauck M, Peters AL, Tsapas A, Wender R, Matthews DR; American Diabetes Association (ADA); European Association for the Study of Diabetes (EASD). Management of hyperglycemia in type 2 diabetes: a patient-centered approach: position statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. 2012;35:1364-1379. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2563] [Cited by in RCA: 2625] [Article Influence: 187.5] [Reference Citation Analysis (4)] |
| 54. | Min T, Bain SC. The Role of Tirzepatide, Dual GIP and GLP-1 Receptor Agonist, in the Management of Type 2 Diabetes: The SURPASS Clinical Trials. Diabetes Ther. 2021;12:143-157. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 84] [Cited by in RCA: 183] [Article Influence: 36.6] [Reference Citation Analysis (0)] |
| 55. | Princeton N, Inc NN. Victoza (liraglutide) package insert. 2010. [cited 23 June 2025]. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/label/2010/022341lbl.pdf. |
| 56. | Wilmington D, AstraZeneca Pharmaceuticals L. Bydureon BCise (exenatide extended-release) injection package insert. 2005. [cited 23 June 2025]. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/label/2018/022200s026lbl.pdf. |
| 57. | Yin WL, Bain SC, Min T. The Effect of Glucagon-Like Peptide-1 Receptor Agonists on Renal Outcomes in Type 2 Diabetes. Diabetes Ther. 2020;11:835-844. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 36] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 58. | Aviles Bueno B, Soler MJ, Perez-Belmonte L, Jimenez Millan A, Rivas Ruiz F, Garcia de Lucas MD. Semaglutide in type 2 diabetes with chronic kidney disease at high risk progression-real-world clinical practice. Clin Kidney J. 2022;15:1593-1600. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 28] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 59. | Kristensen SL, Rørth R, Jhund PS, Docherty KF, Sattar N, Preiss D, Køber L, Petrie MC, McMurray JJV. Cardiovascular, mortality, and kidney outcomes with GLP-1 receptor agonists in patients with type 2 diabetes: a systematic review and meta-analysis of cardiovascular outcome trials. Lancet Diabetes Endocrinol. 2019;7:776-785. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 729] [Cited by in RCA: 1161] [Article Influence: 165.9] [Reference Citation Analysis (0)] |
| 60. | Sattar N, Lee MMY, Kristensen SL, Branch KRH, Del Prato S, Khurmi NS, Lam CSP, Lopes RD, McMurray JJV, Pratley RE, Rosenstock J, Gerstein HC. Cardiovascular, mortality, and kidney outcomes with GLP-1 receptor agonists in patients with type 2 diabetes: a systematic review and meta-analysis of randomised trials. Lancet Diabetes Endocrinol. 2021;9:653-662. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 198] [Cited by in RCA: 1039] [Article Influence: 207.8] [Reference Citation Analysis (0)] |
| 61. | Htike ZZ, Zaccardi F, Papamargaritis D, Webb DR, Khunti K, Davies MJ. Efficacy and safety of glucagon-like peptide-1 receptor agonists in type 2 diabetes: A systematic review and mixed-treatment comparison analysis. Diabetes Obes Metab. 2017;19:524-536. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 340] [Cited by in RCA: 331] [Article Influence: 36.8] [Reference Citation Analysis (0)] |
| 62. | Bessesen DH, Van Gaal LF. Progress and challenges in anti-obesity pharmacotherapy. Lancet Diabetes Endocrinol. 2018;6:237-248. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 154] [Cited by in RCA: 241] [Article Influence: 30.1] [Reference Citation Analysis (0)] |
| 63. | van Can J, Sloth B, Jensen CB, Flint A, Blaak EE, Saris WH. Effects of the once-daily GLP-1 analog liraglutide on gastric emptying, glycemic parameters, appetite and energy metabolism in obese, non-diabetic adults. Int J Obes (Lond). 2014;38:784-793. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 257] [Cited by in RCA: 380] [Article Influence: 29.2] [Reference Citation Analysis (0)] |
| 64. | Plainsboro NNNI. Saxenda (liraglutide) injection package insert. 2014. [cited 23 June 2025]. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/label/2014/206321Orig1s000lbl.pdf. |
| 65. | Plainsboro N, Inc. NN. Wegovy (semaglutide) injection package insert. 2017. [cited 23 June 2025]. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/label/2024/215256s011lbl.pdf. |
| 66. | Plainsboro N, Inc. NN. Rybelsus (semaglutide tablets) package insert. 2017. [cited 23 June 2025]. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/label/2019/213051s000lbl.pdf. |
| 67. | Garvey WT, Frias JP, Jastreboff AM, le Roux CW, Sattar N, Aizenberg D, Mao H, Zhang S, Ahmad NN, Bunck MC, Benabbad I, Zhang XM; SURMOUNT-2 investigators. Tirzepatide once weekly for the treatment of obesity in people with type 2 diabetes (SURMOUNT-2): a double-blind, randomised, multicentre, placebo-controlled, phase 3 trial. Lancet. 2023;402:613-626. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 419] [Article Influence: 139.7] [Reference Citation Analysis (0)] |
| 68. | Jastreboff AM, Aronne LJ, Ahmad NN, Wharton S, Connery L, Alves B, Kiyosue A, Zhang S, Liu B, Bunck MC, Stefanski A; SURMOUNT-1 Investigators. Tirzepatide Once Weekly for the Treatment of Obesity. N Engl J Med. 2022;387:205-216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 232] [Cited by in RCA: 2035] [Article Influence: 508.8] [Reference Citation Analysis (0)] |
| 69. | Wilding JPH, Batterham RL, Calanna S, Davies M, Van Gaal LF, Lingvay I, McGowan BM, Rosenstock J, Tran MTD, Wadden TA, Wharton S, Yokote K, Zeuthen N, Kushner RF; STEP 1 Study Group. Once-Weekly Semaglutide in Adults with Overweight or Obesity. N Engl J Med. 2021;384:989-1002. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 699] [Cited by in RCA: 2844] [Article Influence: 568.8] [Reference Citation Analysis (0)] |
| 70. | Wadden TA, Bailey TS, Billings LK, Davies M, Frias JP, Koroleva A, Lingvay I, O'Neil PM, Rubino DM, Skovgaard D, Wallenstein SOR, Garvey WT; STEP 3 Investigators. Effect of Subcutaneous Semaglutide vs Placebo as an Adjunct to Intensive Behavioral Therapy on Body Weight in Adults With Overweight or Obesity: The STEP 3 Randomized Clinical Trial. JAMA. 2021;325:1403-1413. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 454] [Cited by in RCA: 720] [Article Influence: 144.0] [Reference Citation Analysis (14)] |
| 71. | Davies M, Færch L, Jeppesen OK, Pakseresht A, Pedersen SD, Perreault L, Rosenstock J, Shimomura I, Viljoen A, Wadden TA, Lingvay I; STEP 2 Study Group. Semaglutide 2.4 mg once a week in adults with overweight or obesity, and type 2 diabetes (STEP 2): a randomised, double-blind, double-dummy, placebo-controlled, phase 3 trial. Lancet. 2021;397:971-984. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1031] [Cited by in RCA: 846] [Article Influence: 169.2] [Reference Citation Analysis (0)] |
| 72. | Rubino D, Abrahamsson N, Davies M, Hesse D, Greenway FL, Jensen C, Lingvay I, Mosenzon O, Rosenstock J, Rubio MA, Rudofsky G, Tadayon S, Wadden TA, Dicker D; STEP 4 Investigators. Effect of Continued Weekly Subcutaneous Semaglutide vs Placebo on Weight Loss Maintenance in Adults With Overweight or Obesity: The STEP 4 Randomized Clinical Trial. JAMA. 2021;325:1414-1425. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 584] [Cited by in RCA: 859] [Article Influence: 171.8] [Reference Citation Analysis (0)] |
| 73. | O'Neil PM, Birkenfeld AL, McGowan B, Mosenzon O, Pedersen SD, Wharton S, Carson CG, Jepsen CH, Kabisch M, Wilding JPH. Efficacy and safety of semaglutide compared with liraglutide and placebo for weight loss in patients with obesity: a randomised, double-blind, placebo and active controlled, dose-ranging, phase 2 trial. Lancet. 2018;392:637-649. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 321] [Cited by in RCA: 565] [Article Influence: 70.6] [Reference Citation Analysis (0)] |
| 74. | Pi-Sunyer X, Astrup A, Fujioka K, Greenway F, Halpern A, Krempf M, Lau DC, le Roux CW, Violante Ortiz R, Jensen CB, Wilding JP; SCALE Obesity and Prediabetes NN8022-1839 Study Group. A Randomized, Controlled Trial of 3.0 mg of Liraglutide in Weight Management. N Engl J Med. 2015;373:11-22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1103] [Cited by in RCA: 1768] [Article Influence: 160.7] [Reference Citation Analysis (0)] |
| 75. | le Roux CW, Astrup A, Fujioka K, Greenway F, Lau DCW, Van Gaal L, Ortiz RV, Wilding JPH, Skjøth TV, Manning LS, Pi-Sunyer X; SCALE Obesity Prediabetes NN8022-1839 Study Group. 3 years of liraglutide versus placebo for type 2 diabetes risk reduction and weight management in individuals with prediabetes: a randomised, double-blind trial. Lancet. 2017;389:1399-1409. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 585] [Cited by in RCA: 549] [Article Influence: 61.0] [Reference Citation Analysis (0)] |
| 76. | Astrup A, Rössner S, Van Gaal L, Rissanen A, Niskanen L, Al Hakim M, Madsen J, Rasmussen MF, Lean ME; NN8022-1807 Study Group. Effects of liraglutide in the treatment of obesity: a randomised, double-blind, placebo-controlled study. Lancet. 2009;374:1606-1616. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 743] [Cited by in RCA: 817] [Article Influence: 48.1] [Reference Citation Analysis (0)] |
| 77. | Astrup A, Carraro R, Finer N, Harper A, Kunesova M, Lean ME, Niskanen L, Rasmussen MF, Rissanen A, Rössner S, Savolainen MJ, Van Gaal L; NN8022-1807 Investigators. Safety, tolerability and sustained weight loss over 2 years with the once-daily human GLP-1 analog, liraglutide. Int J Obes (Lond). 2012;36:843-854. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 393] [Cited by in RCA: 508] [Article Influence: 33.9] [Reference Citation Analysis (1)] |
| 78. | Blackman A, Foster GD, Zammit G, Rosenberg R, Aronne L, Wadden T, Claudius B, Jensen CB, Mignot E. Effect of liraglutide 3.0 mg in individuals with obesity and moderate or severe obstructive sleep apnea: the SCALE Sleep Apnea randomized clinical trial. Int J Obes (Lond). 2016;40:1310-1319. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 169] [Cited by in RCA: 352] [Article Influence: 35.2] [Reference Citation Analysis (0)] |
| 79. | Kim SH, Abbasi F, Lamendola C, Liu A, Ariel D, Schaaf P, Grove K, Tomasso V, Ochoa H, Liu YV, Chen YD, Reaven G. Benefits of liraglutide treatment in overweight and obese older individuals with prediabetes. Diabetes Care. 2013;36:3276-3282. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 62] [Cited by in RCA: 82] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 80. | Rosenstock J, Klaff LJ, Schwartz S, Northrup J, Holcombe JH, Wilhelm K, Trautmann M. Effects of exenatide and lifestyle modification on body weight and glucose tolerance in obese subjects with and without pre-diabetes. Diabetes Care. 2010;33:1173-1175. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 154] [Cited by in RCA: 173] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 81. | Dushay J, Gao C, Gopalakrishnan GS, Crawley M, Mitten EK, Wilker E, Mullington J, Maratos-Flier E. Short-term exenatide treatment leads to significant weight loss in a subset of obese women without diabetes. Diabetes Care. 2012;35:4-11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 91] [Cited by in RCA: 109] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 82. | Pratley RE, Kang J, Trautmann ME, Hompesch M, Han O, Stewart J, Sorli CH, Jacob S, Yoon KH. Body weight management and safety with efpeglenatide in adults without diabetes: A phase II randomized study. Diabetes Obes Metab. 2019;21:2429-2439. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 39] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 83. | Lean ME, Carraro R, Finer N, Hartvig H, Lindegaard ML, Rössner S, Van Gaal L, Astrup A; NN8022-1807 Investigators. Tolerability of nausea and vomiting and associations with weight loss in a randomized trial of liraglutide in obese, non-diabetic adults. Int J Obes (Lond). 2014;38:689-697. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 112] [Cited by in RCA: 136] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 84. | Secher A, Jelsing J, Baquero AF, Hecksher-Sørensen J, Cowley MA, Dalbøge LS, Hansen G, Grove KL, Pyke C, Raun K, Schäffer L, Tang-Christensen M, Verma S, Witgen BM, Vrang N, Bjerre Knudsen L. The arcuate nucleus mediates GLP-1 receptor agonist liraglutide-dependent weight loss. J Clin Invest. 2014;124:4473-4488. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 458] [Cited by in RCA: 729] [Article Influence: 60.8] [Reference Citation Analysis (0)] |
| 85. | Cho YK, La Lee Y, Jung CH. The Cardiovascular Effect of Tirzepatide: A Glucagon-Like Peptide-1 and Glucose-Dependent Insulinotropic Polypeptide Dual Agonist. J Lipid Atheroscler. 2023;12:213-222. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 37] [Reference Citation Analysis (0)] |
| 86. | Forzano I, Varzideh F, Avvisato R, Jankauskas SS, Mone P, Santulli G. Tirzepatide: A Systematic Update. Int J Mol Sci. 2022;23:14631. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 64] [Reference Citation Analysis (0)] |
| 87. | Tall Bull S, Nuffer W, Trujillo JM. Tirzepatide: A novel, first-in-class, dual GIP/GLP-1 receptor agonist. J Diabetes Complications. 2022;36:108332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 20] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 88. | Frías JP, Davies MJ, Rosenstock J, Pérez Manghi FC, Fernández Landó L, Bergman BK, Liu B, Cui X, Brown K; SURPASS-2 Investigators. Tirzepatide versus Semaglutide Once Weekly in Patients with Type 2 Diabetes. N Engl J Med. 2021;385:503-515. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 312] [Cited by in RCA: 1258] [Article Influence: 251.6] [Reference Citation Analysis (0)] |
| 89. | Del Prato S, Kahn SE, Pavo I, Weerakkody GJ, Yang Z, Doupis J, Aizenberg D, Wynne AG, Riesmeyer JS, Heine RJ, Wiese RJ; SURPASS-4 Investigators. Tirzepatide versus insulin glargine in type 2 diabetes and increased cardiovascular risk (SURPASS-4): a randomised, open-label, parallel-group, multicentre, phase 3 trial. Lancet. 2021;398:1811-1824. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 441] [Article Influence: 88.2] [Reference Citation Analysis (0)] |
| 90. | Sattar N, McGuire DK, Pavo I, Weerakkody GJ, Nishiyama H, Wiese RJ, Zoungas S. Tirzepatide cardiovascular event risk assessment: a pre-specified meta-analysis. Nat Med. 2022;28:591-598. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 231] [Article Influence: 57.8] [Reference Citation Analysis (0)] |
| 91. | Indianapolis I, Company EL. Zepbound (tirzepatide) injection package insert. 2022. [cited 23 June 2025]. Available from: https://pi.lilly.com/us/zepbound-uspi.pdf. |
| 92. | Quast DR, Nauck MA, Schenker N, Menge BA, Kapitza C, Meier JJ. Macronutrient intake, appetite, food preferences and exocrine pancreas function after treatment with short- and long-acting glucagon-like peptide-1 receptor agonists in type 2 diabetes. Diabetes Obes Metab. 2021;23:2344-2353. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 25] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 93. | Imam A, Alim H, Binhussein M, Kabli A, Alhasnani H, Allehyani A, Aljohani A, Mohorjy A, Tawakul A, Samannodi M, Taha W. Weight Loss Effect of GLP-1 RAs With Endoscopic Bariatric Therapy and Bariatric Surgeries. J Endocr Soc. 2023;7:bvad129. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 13] [Reference Citation Analysis (0)] |
| 94. | Aronne LJ, Sattar N, Horn DB, Bays HE, Wharton S, Lin WY, Ahmad NN, Zhang S, Liao R, Bunck MC, Jouravskaya I, Murphy MA; SURMOUNT-4 Investigators. Continued Treatment With Tirzepatide for Maintenance of Weight Reduction in Adults With Obesity: The SURMOUNT-4 Randomized Clinical Trial. JAMA. 2024;331:38-48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 459] [Article Influence: 229.5] [Reference Citation Analysis (0)] |
| 95. | Elsevier Drug Information. Glucagon-like Peptide-1 (GLP-1) Receptor Agonists and Dual Agonists. 2024. |
| 96. | Sodhi M, Rezaeianzadeh R, Kezouh A, Etminan M. Risk of Gastrointestinal Adverse Events Associated With Glucagon-Like Peptide-1 Receptor Agonists for Weight Loss. JAMA. 2023;330:1795-1797. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 299] [Article Influence: 99.7] [Reference Citation Analysis (0)] |
| 97. | Sun F, Chai S, Yu K, Quan X, Yang Z, Wu S, Zhang Y, Ji L, Wang J, Shi L. Gastrointestinal adverse events of glucagon-like peptide-1 receptor agonists in patients with type 2 diabetes: a systematic review and network meta-analysis. Diabetes Technol Ther. 2015;17:35-42. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 114] [Cited by in RCA: 111] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 98. | Buse JB, Rosenstock J, Sesti G, Schmidt WE, Montanya E, Brett JH, Zychma M, Blonde L; LEAD-6 Study Group. Liraglutide once a day versus exenatide twice a day for type 2 diabetes: a 26-week randomised, parallel-group, multinational, open-label trial (LEAD-6). Lancet. 2009;374:39-47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1100] [Cited by in RCA: 1125] [Article Influence: 66.2] [Reference Citation Analysis (0)] |
| 99. | Marre M, Shaw J, Brändle M, Bebakar WM, Kamaruddin NA, Strand J, Zdravkovic M, Le Thi TD, Colagiuri S; LEAD-1 SU study group. Liraglutide, a once-daily human GLP-1 analogue, added to a sulphonylurea over 26 weeks produces greater improvements in glycaemic and weight control compared with adding rosiglitazone or placebo in subjects with Type 2 diabetes (LEAD-1 SU). Diabet Med. 2009;26:268-278. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 603] [Cited by in RCA: 636] [Article Influence: 37.4] [Reference Citation Analysis (0)] |
| 100. | Russell-Jones D, Cuddihy RM, Hanefeld M, Kumar A, González JG, Chan M, Wolka AM, Boardman MK; DURATION-4 Study Group. Efficacy and safety of exenatide once weekly versus metformin, pioglitazone, and sitagliptin used as monotherapy in drug-naive patients with type 2 diabetes (DURATION-4): a 26-week double-blind study. Diabetes Care. 2012;35:252-258. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 240] [Cited by in RCA: 281] [Article Influence: 20.1] [Reference Citation Analysis (0)] |
| 101. | Riddle MC, Aronson R, Home P, Marre M, Niemoeller E, Miossec P, Ping L, Ye J, Rosenstock J. Adding once-daily lixisenatide for type 2 diabetes inadequately controlled by established basal insulin: a 24-week, randomized, placebo-controlled comparison (GetGoal-L). Diabetes Care. 2013;36:2489-2496. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 228] [Cited by in RCA: 245] [Article Influence: 18.8] [Reference Citation Analysis (0)] |
| 102. | Nauck M, Frid A, Hermansen K, Shah NS, Tankova T, Mitha IH, Zdravkovic M, Düring M, Matthews DR; LEAD-2 Study Group. Efficacy and safety comparison of liraglutide, glimepiride, and placebo, all in combination with metformin, in type 2 diabetes: the LEAD (liraglutide effect and action in diabetes)-2 study. Diabetes Care. 2009;32:84-90. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 805] [Cited by in RCA: 875] [Article Influence: 51.5] [Reference Citation Analysis (0)] |
| 103. | Nauck M, Frid A, Hermansen K, Thomsen AB, During M, Shah N, Tankova T, Mitha I, Matthews DR. Long-term efficacy and safety comparison of liraglutide, glimepiride and placebo, all in combination with metformin in type 2 diabetes: 2-year results from the LEAD-2 study. Diabetes Obes Metab. 2013;15:204-212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 122] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 104. | Nauck MA, Duran S, Kim D, Johns D, Northrup J, Festa A, Brodows R, Trautmann M. A comparison of twice-daily exenatide and biphasic insulin aspart in patients with type 2 diabetes who were suboptimally controlled with sulfonylurea and metformin: a non-inferiority study. Diabetologia. 2007;50:259-267. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 322] [Cited by in RCA: 312] [Article Influence: 16.4] [Reference Citation Analysis (0)] |
| 105. | Garber A, Henry R, Ratner R, Garcia-Hernandez PA, Rodriguez-Pattzi H, Olvera-Alvarez I, Hale PM, Zdravkovic M, Bode B; LEAD-3 (Mono) Study Group. Liraglutide versus glimepiride monotherapy for type 2 diabetes (LEAD-3 Mono): a randomised, 52-week, phase III, double-blind, parallel-treatment trial. Lancet. 2009;373:473-481. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 752] [Cited by in RCA: 806] [Article Influence: 47.4] [Reference Citation Analysis (0)] |
| 106. | Buse JB, Nauck M, Forst T, Sheu WH, Shenouda SK, Heilmann CR, Hoogwerf BJ, Gao A, Boardman MK, Fineman M, Porter L, Schernthaner G. Exenatide once weekly versus liraglutide once daily in patients with type 2 diabetes (DURATION-6): a randomised, open-label study. Lancet. 2013;381:117-124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 374] [Cited by in RCA: 408] [Article Influence: 31.4] [Reference Citation Analysis (0)] |
| 107. | Garber A, Henry RR, Ratner R, Hale P, Chang CT, Bode B; LEAD-3 (Mono) Study Group. Liraglutide, a once-daily human glucagon-like peptide 1 analogue, provides sustained improvements in glycaemic control and weight for 2 years as monotherapy compared with glimepiride in patients with type 2 diabetes. Diabetes Obes Metab. 2011;13:348-356. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 148] [Cited by in RCA: 154] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 108. | Diamant M, Van Gaal L, Stranks S, Guerci B, MacConell L, Haber H, Scism-Bacon J, Trautmann M. Safety and efficacy of once-weekly exenatide compared with insulin glargine titrated to target in patients with type 2 diabetes over 84 weeks. Diabetes Care. 2012;35:683-689. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 70] [Cited by in RCA: 73] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 109. | Zheng SL, Roddick AJ, Aghar-Jaffar R, Shun-Shin MJ, Francis D, Oliver N, Meeran K. Association Between Use of Sodium-Glucose Cotransporter 2 Inhibitors, Glucagon-like Peptide 1 Agonists, and Dipeptidyl Peptidase 4 Inhibitors With All-Cause Mortality in Patients With Type 2 Diabetes: A Systematic Review and Meta-analysis. JAMA. 2018;319:1580-1591. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 333] [Cited by in RCA: 298] [Article Influence: 37.3] [Reference Citation Analysis (0)] |
| 110. | Aroda VR, Ahmann A, Cariou B, Chow F, Davies MJ, Jódar E, Mehta R, Woo V, Lingvay I. Comparative efficacy, safety, and cardiovascular outcomes with once-weekly subcutaneous semaglutide in the treatment of type 2 diabetes: Insights from the SUSTAIN 1-7 trials. Diabetes Metab. 2019;45:409-418. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 199] [Article Influence: 28.4] [Reference Citation Analysis (1)] |
| 111. | Grimm M, Han J, Weaver C, Griffin P, Schulteis CT, Dong H, Malloy J. Efficacy, safety, and tolerability of exenatide once weekly in patients with type 2 diabetes mellitus: an integrated analysis of the DURATION trials. Postgrad Med. 2013;125:47-57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 53] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 112. | Wharton S, Calanna S, Davies M, Dicker D, Goldman B, Lingvay I, Mosenzon O, Rubino DM, Thomsen M, Wadden TA, Pedersen SD. Gastrointestinal tolerability of once-weekly semaglutide 2.4 mg in adults with overweight or obesity, and the relationship between gastrointestinal adverse events and weight loss. Diabetes Obes Metab. 2022;24:94-105. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 46] [Cited by in RCA: 94] [Article Influence: 23.5] [Reference Citation Analysis (0)] |
| 113. | Lomeli LD, Kodali AM, Tsushima Y, Mehta AE, Pantalone KM. The incidence of acute pancreatitis with GLP-1 receptor agonist therapy in individuals with a known history of pancreatitis. Diabetes Res Clin Pract. 2024;215:111806. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 14] [Reference Citation Analysis (0)] |
| 114. | Ma H, Lin YH, Dai LZ, Lin CS, Huang Y, Liu SY. Efficacy and safety of GLP-1 receptor agonists versus SGLT-2 inhibitors in overweight/obese patients with or without diabetes mellitus: a systematic review and network meta-analysis. BMJ Open. 2023;13:e061807. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 53] [Reference Citation Analysis (0)] |
| 115. | Blevins T, Pullman J, Malloy J, Yan P, Taylor K, Schulteis C, Trautmann M, Porter L. DURATION-5: exenatide once weekly resulted in greater improvements in glycemic control compared with exenatide twice daily in patients with type 2 diabetes. J Clin Endocrinol Metab. 2011;96:1301-1310. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 320] [Cited by in RCA: 350] [Article Influence: 23.3] [Reference Citation Analysis (0)] |
| 116. | Bettge K, Kahle M, Abd El Aziz MS, Meier JJ, Nauck MA. Occurrence of nausea, vomiting and diarrhoea reported as adverse events in clinical trials studying glucagon-like peptide-1 receptor agonists: A systematic analysis of published clinical trials. Diabetes Obes Metab. 2017;19:336-347. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 148] [Cited by in RCA: 267] [Article Influence: 29.7] [Reference Citation Analysis (0)] |
| 117. | Holst JJ, Andersen DB, Grunddal KV. Actions of glucagon-like peptide-1 receptor ligands in the gut. Br J Pharmacol. 2022;179:727-742. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 47] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 118. | Guja C, Frías JP, Suchower L, Hardy E, Marr G, Sjöström CD, Jabbour SA. Safety and Efficacy of Exenatide Once Weekly in Participants with Type 2 Diabetes and Stage 2/3 Chronic Kidney Disease. Diabetes Ther. 2020;11:1467-1480. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 119. | Rosenstock J, Allison D, Birkenfeld AL, Blicher TM, Deenadayalan S, Jacobsen JB, Serusclat P, Violante R, Watada H, Davies M; PIONEER 3 Investigators. Effect of Additional Oral Semaglutide vs Sitagliptin on Glycated Hemoglobin in Adults With Type 2 Diabetes Uncontrolled With Metformin Alone or With Sulfonylurea: The PIONEER 3 Randomized Clinical Trial. JAMA. 2019;321:1466-1480. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 172] [Cited by in RCA: 316] [Article Influence: 45.1] [Reference Citation Analysis (0)] |
| 120. | Fineman MS, Shen LZ, Taylor K, Kim DD, Baron AD. Effectiveness of progressive dose-escalation of exenatide (exendin-4) in reducing dose-limiting side effects in subjects with type 2 diabetes. Diabetes Metab Res Rev. 2004;20:411-417. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 167] [Cited by in RCA: 171] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 121. | Trujillo J. Safety and tolerability of once-weekly GLP-1 receptor agonists in type 2 diabetes. J Clin Pharm Ther. 2020;45 Suppl 1:43-60. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 57] [Cited by in RCA: 94] [Article Influence: 15.7] [Reference Citation Analysis (0)] |
| 122. | Abu-Freha N, Yitzhak A, Shirin H, Nevo-Shor A, Abu-Jaffar J, Abu-Rafe S, Afianish Y, Cohen DL, Bermont A. Glucagon-like peptide-1 receptor agonists significantly affect the quality of bowel preparation for colonoscopy. Endoscopy. 2025;57:126-133. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 12] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 123. | Tong Y, Huang JQ, Chen Y, Tu M, Wang W. Impact of glucagon-like peptide 1 receptor agonist liraglutide and dipeptidyl peptidase-4 inhibitor sitagliptin on bowel cleaning and gastrointestinal symptoms in type 2 diabetes. Front Pharmacol. 2023;14:1176206. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 18] [Reference Citation Analysis (0)] |
| 124. | Ghazanfar H, Javed N, Qasim A, Sosa F, Altaf F, Khan S, Mahasamudram J, Jyala A, Kandhi SD, Shin D, Mantri N, Sun H, Hanumanthu S, Patel H, Makker J, Balar B, Dev A, Chilimuri S. Is it necessary to stop glucagon-like peptide-1 receptor agonists prior to endoscopic procedure? A retrospective study. World J Gastroenterol. 2024;30:3221-3228. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 5] [Cited by in RCA: 13] [Article Influence: 6.5] [Reference Citation Analysis (2)] |
| 125. | Elashoff M, Matveyenko AV, Gier B, Elashoff R, Butler PC. Pancreatitis, pancreatic, and thyroid cancer with glucagon-like peptide-1-based therapies. Gastroenterology. 2011;141:150-156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 596] [Cited by in RCA: 685] [Article Influence: 45.7] [Reference Citation Analysis (0)] |
| 126. | Garg R, Chen W, Pendergrass M. Acute pancreatitis in type 2 diabetes treated with exenatide or sitagliptin: a retrospective observational pharmacy claims analysis. Diabetes Care. 2010;33:2349-2354. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 233] [Cited by in RCA: 240] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 127. | Dore DD, Bloomgren GL, Wenten M, Hoffman C, Clifford CR, Quinn SG, Braun DK, Noel RA, Seeger JD. A cohort study of acute pancreatitis in relation to exenatide use. Diabetes Obes Metab. 2011;13:559-566. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 110] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 128. | Romley JA, Goldman DP, Solomon M, McFadden D, Peters AL. Exenatide therapy and the risk of pancreatitis and pancreatic cancer in a privately insured population. Diabetes Technol Ther. 2012;14:904-911. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 69] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 129. | Li L, Shen J, Bala MM, Busse JW, Ebrahim S, Vandvik PO, Rios LP, Malaga G, Wong E, Sohani Z, Guyatt GH, Sun X. Incretin treatment and risk of pancreatitis in patients with type 2 diabetes mellitus: systematic review and meta-analysis of randomised and non-randomised studies. BMJ. 2014;348:g2366. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 191] [Cited by in RCA: 181] [Article Influence: 15.1] [Reference Citation Analysis (10)] |
| 130. | Monami M, Nreu B, Scatena A, Cresci B, Andreozzi F, Sesti G, Mannucci E. Safety issues with glucagon-like peptide-1 receptor agonists (pancreatitis, pancreatic cancer and cholelithiasis): Data from randomized controlled trials. Diabetes Obes Metab. 2017;19:1233-1241. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 174] [Article Influence: 19.3] [Reference Citation Analysis (0)] |
| 131. | Storgaard H, Cold F, Gluud LL, Vilsbøll T, Knop FK. Glucagon-like peptide-1 receptor agonists and risk of acute pancreatitis in patients with type 2 diabetes. Diabetes Obes Metab. 2017;19:906-908. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 116] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 132. | Singh S, Chang HY, Richards TM, Weiner JP, Clark JM, Segal JB. Glucagonlike peptide 1-based therapies and risk of hospitalization for acute pancreatitis in type 2 diabetes mellitus: a population-based matched case-control study. JAMA Intern Med. 2013;173:534-539. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 257] [Cited by in RCA: 326] [Article Influence: 25.1] [Reference Citation Analysis (0)] |
| 133. | Nauck MA, Frossard JL, Barkin JS, Anglin G, Hensley IE, Harper KD, Milicevic Z. Assessment of Pancreas Safety in the Development Program of Once-Weekly GLP-1 Receptor Agonist Dulaglutide. Diabetes Care. 2017;40:647-654. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 28] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 134. | Steinberg WM, Buse JB, Ghorbani MLM, Ørsted DD, Nauck MA; LEADER Steering Committee; LEADER Trial Investigators. Amylase, Lipase, and Acute Pancreatitis in People With Type 2 Diabetes Treated With Liraglutide: Results From the LEADER Randomized Trial. Diabetes Care. 2017;40:966-972. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 67] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 135. | Halfdanarson TR, Pannala R. Incretins and risk of neoplasia. BMJ. 2013;346:f3750. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 136. | Cohen D. Has pancreatic damage from glucagon suppressing diabetes drugs been underplayed? BMJ. 2013;346:f3680. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 32] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 137. | Butler AE, Campbell-Thompson M, Gurlo T, Dawson DW, Atkinson M, Butler PC. Marked expansion of exocrine and endocrine pancreas with incretin therapy in humans with increased exocrine pancreas dysplasia and the potential for glucagon-producing neuroendocrine tumors. Diabetes. 2013;62:2595-2604. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 302] [Cited by in RCA: 320] [Article Influence: 24.6] [Reference Citation Analysis (0)] |
| 138. | Egan AG, Blind E, Dunder K, de Graeff PA, Hummer BT, Bourcier T, Rosebraugh C. Pancreatic safety of incretin-based drugs--FDA and EMA assessment. N Engl J Med. 2014;370:794-797. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 374] [Cited by in RCA: 378] [Article Influence: 31.5] [Reference Citation Analysis (0)] |
| 139. | He L, Wang J, Ping F, Yang N, Huang J, Li Y, Xu L, Li W, Zhang H. Association of Glucagon-Like Peptide-1 Receptor Agonist Use With Risk of Gallbladder and Biliary Diseases: A Systematic Review and Meta-analysis of Randomized Clinical Trials. JAMA Intern Med. 2022;182:513-519. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 192] [Article Influence: 48.0] [Reference Citation Analysis (0)] |
| 140. | Woronow D, Chamberlain C, Niak A, Avigan M, Houstoun M, Kortepeter C. Acute Cholecystitis Associated With the Use of Glucagon-Like Peptide-1 Receptor Agonists Reported to the US Food and Drug Administration. JAMA Intern Med. 2022;182:1104-1106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 25] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 141. | Ornelas C, Caiado J, Lopes A, Pereira Dos Santos MC, Pereira Barbosa M. Anaphylaxis to Long-Acting Release Exenatide. J Investig Allergol Clin Immunol. 2018;28:332-334. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 142. | Pradhan R, Montastruc F, Rousseau V, Patorno E, Azoulay L. Exendin-based glucagon-like peptide-1 receptor agonists and anaphylactic reactions: a pharmacovigilance analysis. Lancet Diabetes Endocrinol. 2020;8:13-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 21] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 143. | Shamriz O, NaserEddin A, Mosenzon O, Sviri S, Tal Y. Allergic Reaction to Exenatide and Lixisenatide but Not to Liraglutide: Unveiling Anaphylaxis to Glucagon-Like Peptide 1 Receptor Agonists. Diabetes Care. 2019;42:e141-e142. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 15] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 144. | Weissman PN, Carr MC, Ye J, Cirkel DT, Stewart M, Perry C, Pratley R. HARMONY 4: randomised clinical trial comparing once-weekly albiglutide and insulin glargine in patients with type 2 diabetes inadequately controlled with metformin with or without sulfonylurea. Diabetologia. 2014;57:2475-2484. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 111] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 145. | Rosenstock J, Fonseca VA, Gross JL, Ratner RE, Ahrén B, Chow FC, Yang F, Miller D, Johnson SL, Stewart MW, Leiter LA; Harmony 6 Study Group. Advancing basal insulin replacement in type 2 diabetes inadequately controlled with insulin glargine plus oral agents: a comparison of adding albiglutide, a weekly GLP-1 receptor agonist, versus thrice-daily prandial insulin lispro. Diabetes Care. 2014;37:2317-2325. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 157] [Cited by in RCA: 179] [Article Influence: 14.9] [Reference Citation Analysis (0)] |
| 146. | Pratley RE, Nauck MA, Barnett AH, Feinglos MN, Ovalle F, Harman-Boehm I, Ye J, Scott R, Johnson S, Stewart M, Rosenstock J; HARMONY 7 study group. Once-weekly albiglutide versus once-daily liraglutide in patients with type 2 diabetes inadequately controlled on oral drugs (HARMONY 7): a randomised, open-label, multicentre, non-inferiority phase 3 study. Lancet Diabetes Endocrinol. 2014;2:289-297. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 234] [Cited by in RCA: 257] [Article Influence: 21.4] [Reference Citation Analysis (0)] |
| 147. | Shyangdan DS, Royle P, Clar C, Sharma P, Waugh N, Snaith A. Glucagon-like peptide analogues for type 2 diabetes mellitus. Cochrane Database Syst Rev. 2011;2011:CD006423. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 87] [Cited by in RCA: 123] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 148. | Filippatos TD, Elisaf MS. Effects of glucagon-like peptide-1 receptor agonists on renal function. World J Diabetes. 2013;4:190-201. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 51] [Cited by in RCA: 75] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 149. | Johansen OE, Whitfield R. Exenatide may aggravate moderate diabetic renal impairment: a case report. Br J Clin Pharmacol. 2008;66:568-569. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 29] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 150. | López-Ruiz A, del Peso-Gilsanz C, Meoro-Avilés A, Soriano-Palao J, Andreu A, Cabezuelo J, Arias JL. Acute renal failure when exenatide is co-administered with diuretics and angiotensin II blockers. Pharm World Sci. 2010;32:559-561. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 27] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 151. | Weise WJ, Sivanandy MS, Block CA, Comi RJ. Exenatide-associated ischemic renal failure. Diabetes Care. 2009;32:e22-e23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 72] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 152. | Kaakeh Y, Kanjee S, Boone K, Sutton J. Liraglutide-induced acute kidney injury. Pharmacotherapy. 2012;32:e7-11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 41] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 153. | Leehey DJ, Rahman MA, Borys E, Picken MM, Clise CE. Acute Kidney Injury Associated With Semaglutide. Kidney Med. 2021;3:282-285. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 39] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 154. | Vallatharasu Y, Hayashi-Tanner Y, Polewski PJ, Bottner WA, Rosenstein LJ, Uprety D, Bista A, Farnen JP, Aster R. Severe, prolonged thrombocytopenia in a patient sensitive to exenatide. Am J Hematol. 2019;94:E78-E80. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 155. | Pasternak B, Wintzell V, Hviid A, Eliasson B, Gudbjörnsdottir S, Jonasson C, Hveem K, Svanström H, Melbye M, Ueda P. Glucagon-like peptide 1 receptor agonist use and risk of thyroid cancer: Scandinavian cohort study. BMJ. 2024;385:e078225. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 63] [Article Influence: 31.5] [Reference Citation Analysis (0)] |
| 156. | Bezin J, Gouverneur A, Pénichon M, Mathieu C, Garrel R, Hillaire-Buys D, Pariente A, Faillie JL. GLP-1 Receptor Agonists and the Risk of Thyroid Cancer. Diabetes Care. 2023;46:384-390. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 195] [Article Influence: 65.0] [Reference Citation Analysis (0)] |
| 157. | Bjerre Knudsen L, Madsen LW, Andersen S, Almholt K, de Boer AS, Drucker DJ, Gotfredsen C, Egerod FL, Hegelund AC, Jacobsen H, Jacobsen SD, Moses AC, Mølck AM, Nielsen HS, Nowak J, Solberg H, Thi TD, Zdravkovic M, Moerch U. Glucagon-like Peptide-1 receptor agonists activate rodent thyroid C-cells causing calcitonin release and C-cell proliferation. Endocrinology. 2010;151:1473-1486. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 380] [Cited by in RCA: 492] [Article Influence: 30.8] [Reference Citation Analysis (0)] |
| 158. | Madsen LW, Knauf JA, Gotfredsen C, Pilling A, Sjögren I, Andersen S, Andersen L, de Boer AS, Manova K, Barlas A, Vundavalli S, Nyborg NC, Knudsen LB, Moelck AM, Fagin JA. GLP-1 receptor agonists and the thyroid: C-cell effects in mice are mediated via the GLP-1 receptor and not associated with RET activation. Endocrinology. 2012;153:1538-1547. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 119] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 159. | Consoli A, Formoso G. Potential side effects to GLP-1 agonists: understanding their safety and tolerability. Expert Opin Drug Saf. 2015;14:207-218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 48] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 160. | Schmitz SH, Saunders KH, Aronne LJ. Cutting-Edge Approaches to Obesity Management: The Latest Pharmacological Options. Endocrinol Metab Clin North Am. 2025;54:85-102. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 161. | Egan JM, Chia CW. Incretin therapy and pancreatic pathologies: background pathology versus drug-induced pathology in rats. Diabetes. 2014;63:1174-1178. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 162. | Monami M, Dicembrini I, Nardini C, Fiordelli I, Mannucci E. Glucagon-like peptide-1 receptor agonists and pancreatitis: a meta-analysis of randomized clinical trials. Diabetes Res Clin Pract. 2014;103:269-275. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 74] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 163. | Kim D, MacConell L, Zhuang D, Kothare PA, Trautmann M, Fineman M, Taylor K. Effects of once-weekly dosing of a long-acting release formulation of exenatide on glucose control and body weight in subjects with type 2 diabetes. Diabetes Care. 2007;30:1487-1493. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 334] [Cited by in RCA: 334] [Article Influence: 17.6] [Reference Citation Analysis (0)] |
| 164. | Zhang T, Liu S, He S, Shi L, Ma R. Strategies to Enhance the Therapeutic Efficacy of GLP-1 Receptor Agonists through Structural Modification and Carrier Delivery. Chembiochem. 2025;26:e202400962. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/