Copyright
©The Author(s) 2022.
World J Gastrointest Pharmacol Ther. Mar 5, 2022; 13(2): 23-29
Published online Mar 5, 2022. doi: 10.4292/wjgpt.v13.i2.23
Published online Mar 5, 2022. doi: 10.4292/wjgpt.v13.i2.23
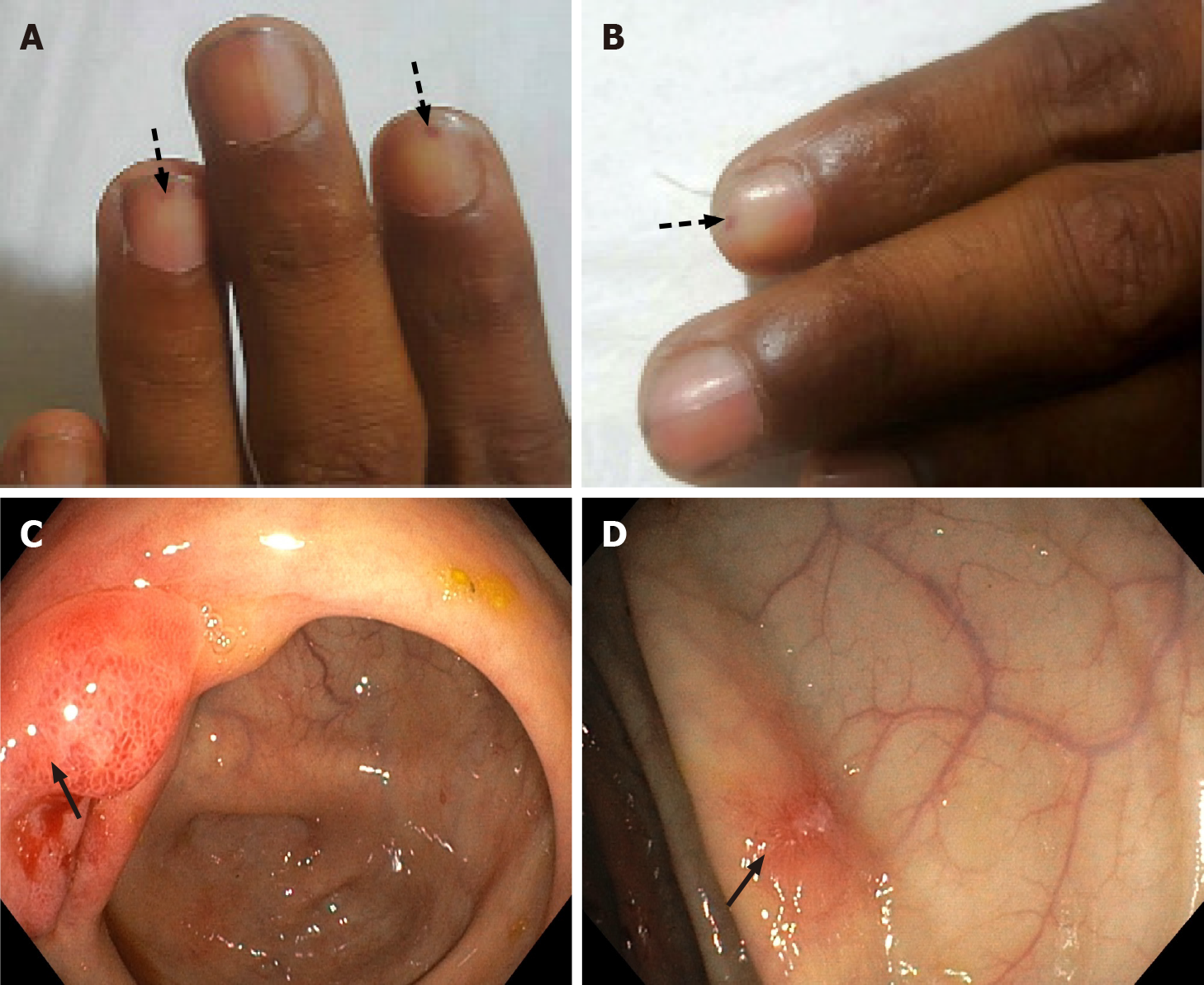
Figure 1 Cutaneous manifestations and endoscopic findings in the patient with eosinophilic gastrointestinal disorder.
A and B: Sections show splinter hemorrhages (arrows) in different nails; C and D: Show terminal ileum and colonic mucosal erythematous erosions (arrows).
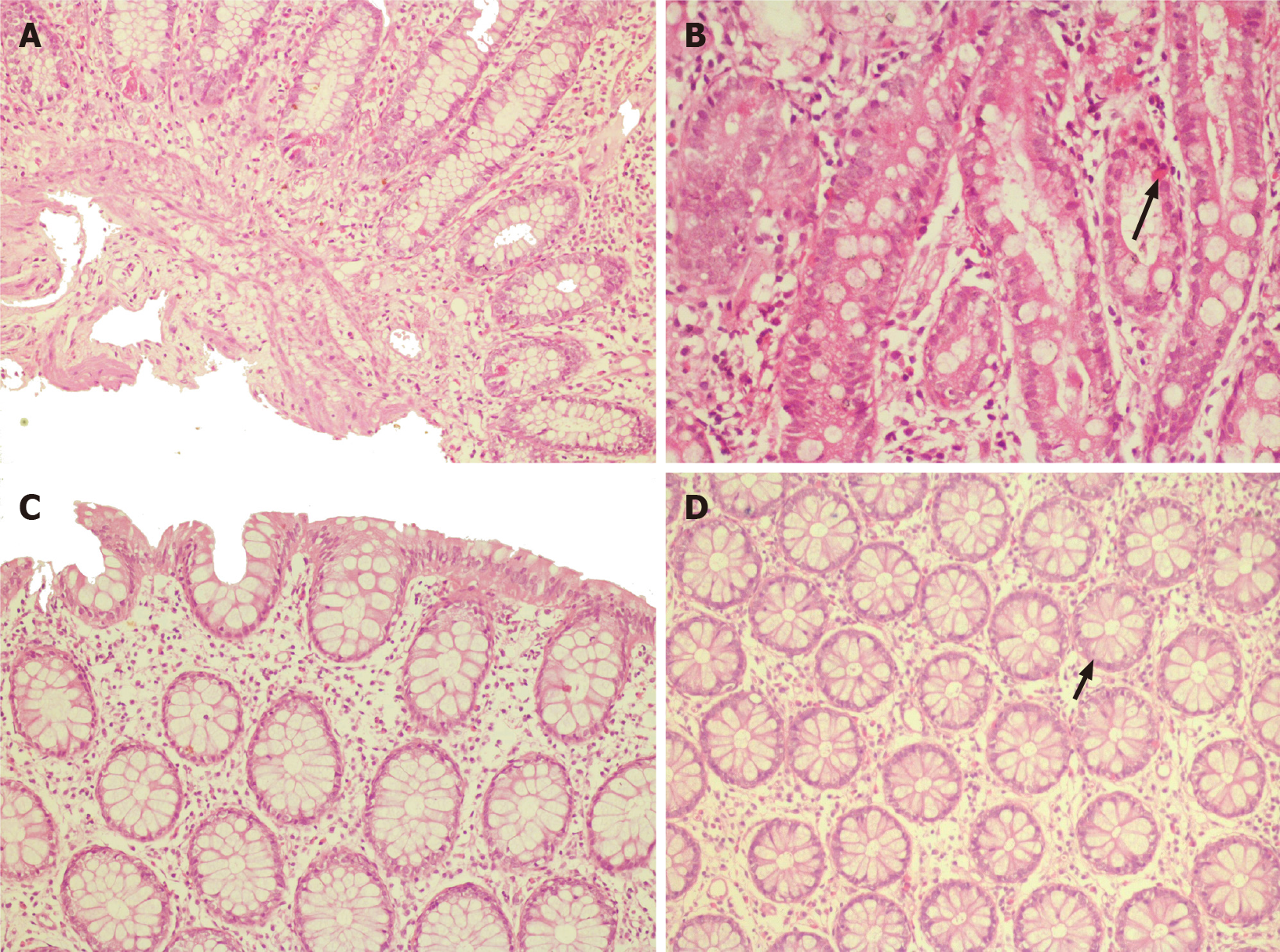
Figure 2 Histopathology images.
A: Terminal ileal/ileocecal biopsy section shows mucosal lining with marked eosinophil rich infiltrates in the lamina propria. The eosinophils infiltrate the muscularis mucosae; B: Higher magnification (400×) of the duodenum section shows the infiltration of crypt epithelium by eosinophils (arrow); C: Section from the ascending colon lamina propria shows a mild increase in eosinophils; however, no cryptitis or crypt abscess is seen; D: Higher magnification (400×) of the rectum shows crypt lining epithelium infiltrated by eosinophils (arrow).
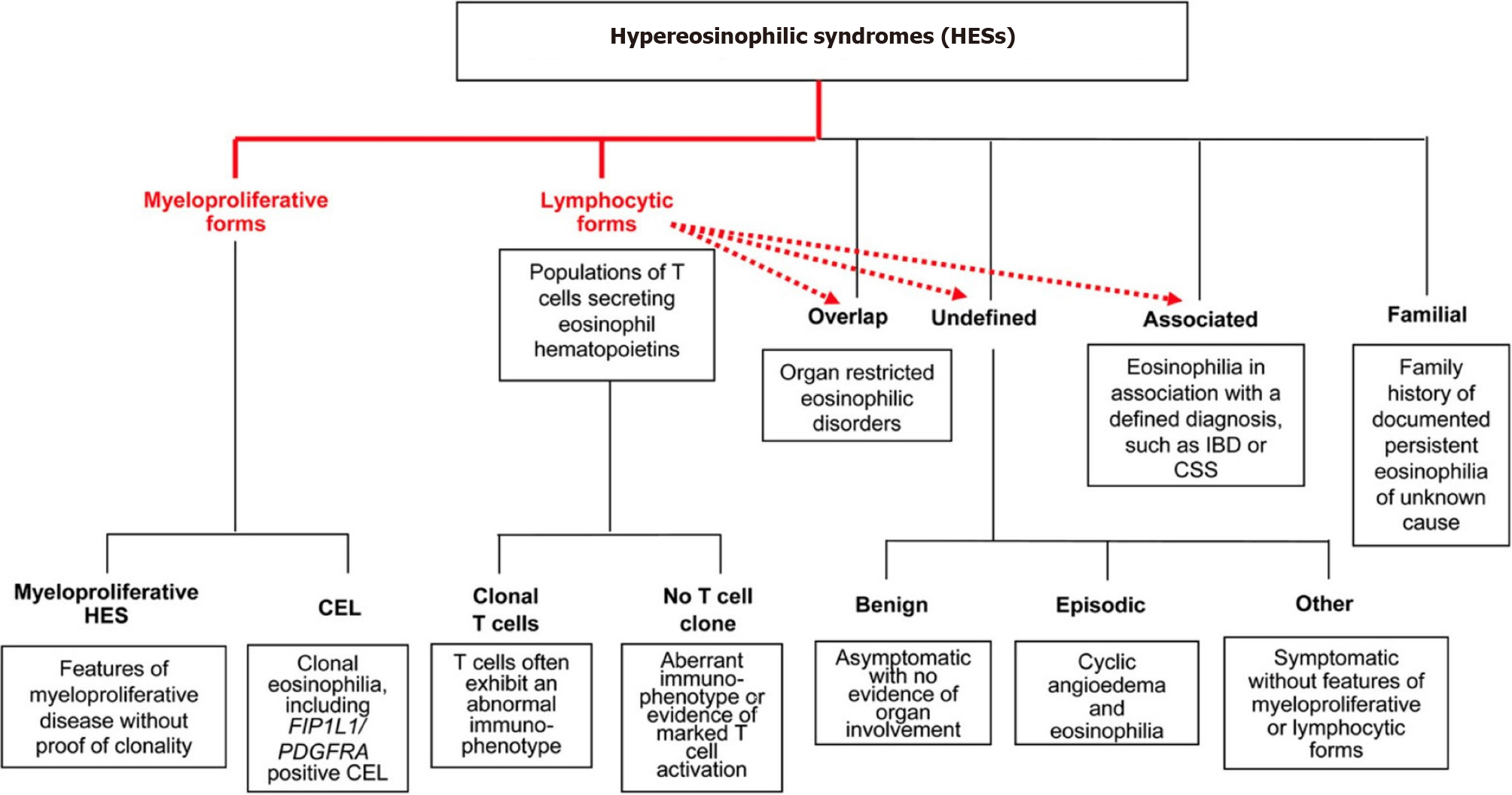
Figure 3 The classification of hypereosinophilic syndrome as per Simon et al[3].
CSS: Cyberchondria severity scale; IBD: Inflammatory bowel disease; HES: Hypereosinophilic syndrome; CEL: Carboxyl ester lipase. Citation: Simon HU, Rothenberg ME, Bochner BS, Weller PF, Wardlaw AJ, Wechsler ME, Rosenwasser LJ, Roufosse F, Gleich GJ, Klion AD. Refining the definition of hypereosinophilic syndrome. J Allergy Clin Immunol 2010; 126: 45-49.
- Citation: Bhasi A, Patnaik I, Panda PK, Singh A. Hypereosinophilic syndrome presenting as eosinophilic gastroenteritis disorder and splinter hemorrhages: A case report. World J Gastrointest Pharmacol Ther 2022; 13(2): 23-29
- URL: https://www.wjgnet.com/2150-5349/full/v13/i2/23.htm
- DOI: https://dx.doi.org/10.4292/wjgpt.v13.i2.23