Published online Aug 15, 2010. doi: 10.4291/wjgp.v1.i3.112
Revised: July 25, 2010
Accepted: August 1, 2010
Published online: August 15, 2010
Syphilitic proctitis is a rare disease. It usually presents as proctitis, ulcer and neoplasm but lacks pathognomonic clinical symptoms. It is, therefore, difficult to diagnose and is occasionally treated inappropriately. We report the case of a 51-year-old man who had a hard, ulcerated mass, which occupied the circumference of the rectal wall and which mimicked a rectal tumor. Fortunately, positive finding from routine toluidine red unheated serum test and treponema pallidum particle agglutination tests made us reevaluate the patient and led us to suspect syphilitic proctitis. This diagnosis was finally confirmed after successful penicillin G benzathine therapy which made surgery unnecessary.
- Citation: Zhao WT, Liu J, Li YY. Syphilitic proctitis mimicking rectal cancer: A case report. World J Gastrointest Pathophysiol 2010; 1(3): 112-114
- URL: https://www.wjgnet.com/2150-5330/full/v1/i3/112.htm
- DOI: https://dx.doi.org/10.4291/wjgp.v1.i3.112
Syphilitic proctitis is a rare disease. It usually presents as proctitis, ulcer and neoplasm but lacks pathognomonic clinical symptoms[1-4]. It is, therefore, difficult to diagnose and is occasionally treated inappropriately[5]. Here, we report a case of syphilitic proctitis which was initially considered to be a rectal cancer.
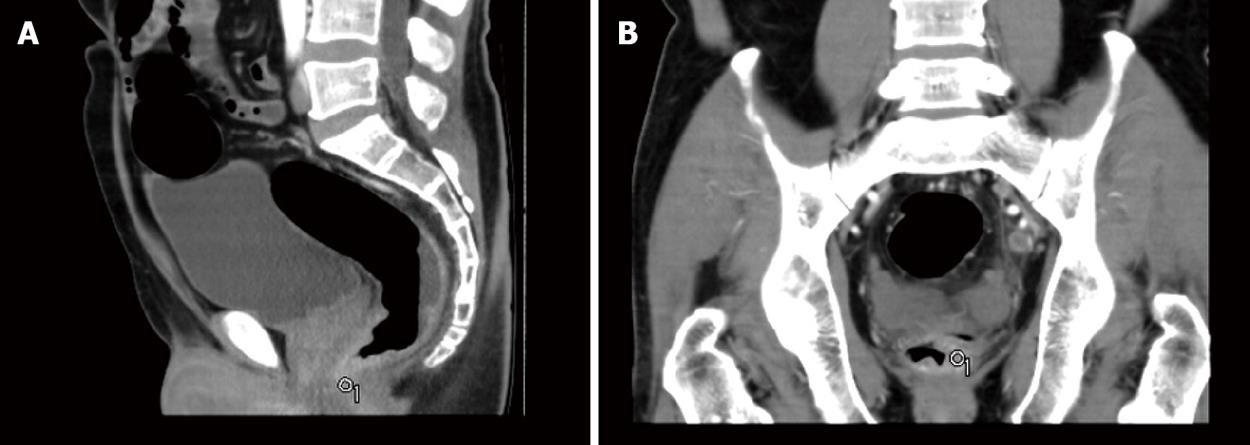
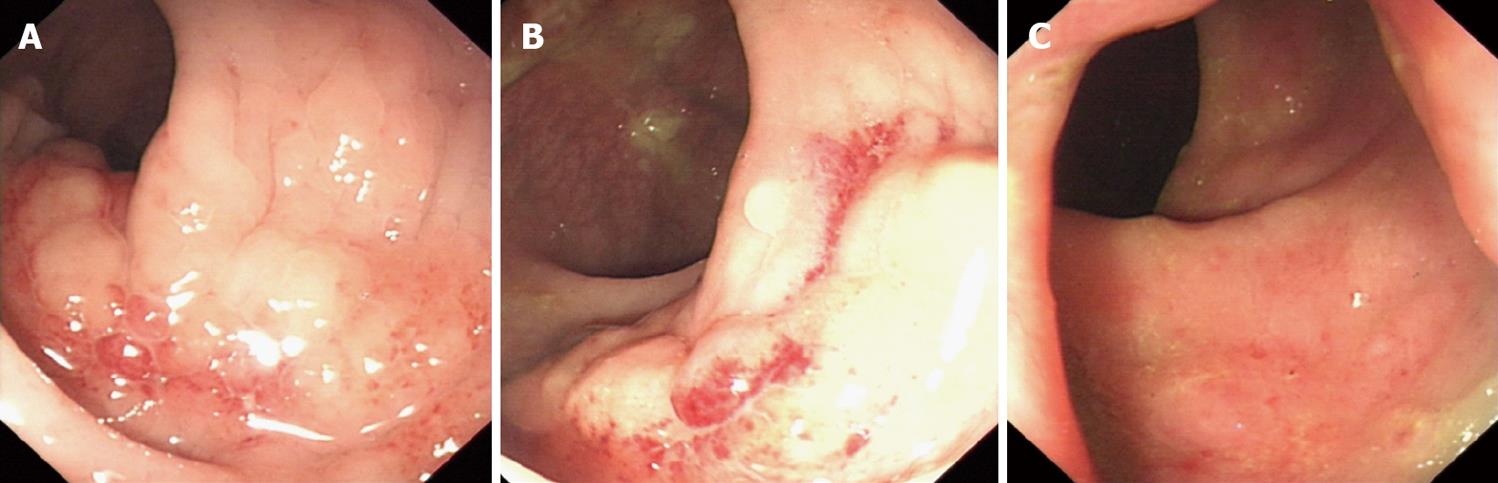
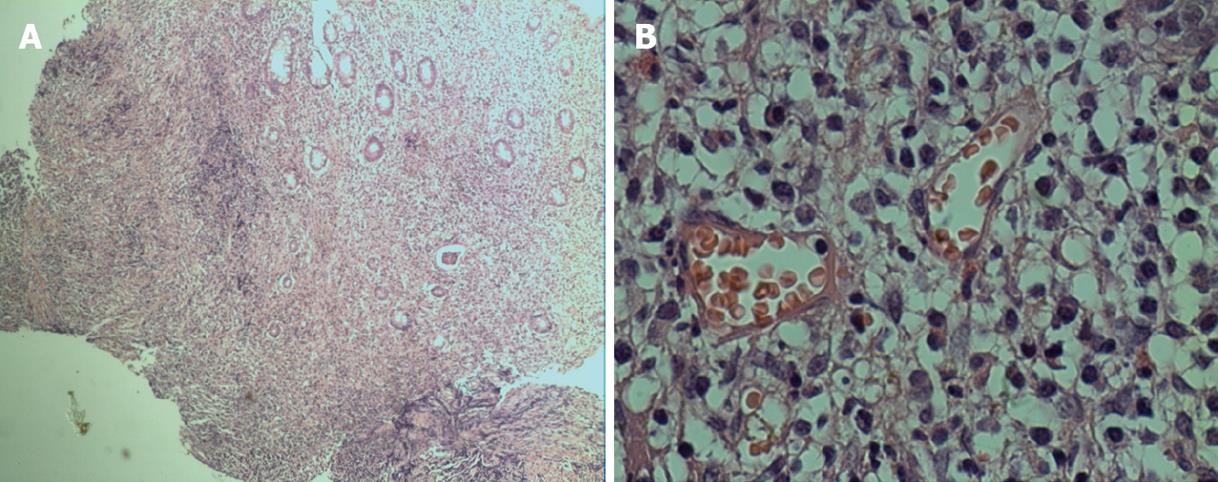
A 51-year-old man was referred to our hospital with a 2 wk history of anorectal discomfort. He complained of anorectal discomfort, tenesmus, mucous discharge, increase in the number of stools by 3-4 per day, and intermittent presence of blood in stool. He experienced a weight loss of about 2-kilogram over the previous two weeks. His past history was negative for any anorectal disease, surgery, genetically transmitted problems, or infective illness. He denied improper sexual and same-sex sexual behavior. Rectal examination revealed a hard, ulcerated mass, occupying the circumference of the rectal wall, at 3 cm to 7 cm from the anal verge. Laboratory studies revealed normal results on complete blood cell, urinalysis and serum chemistry testing. Faecal occult blood test was positive. Serum tumor markers were negative. Toluidine red unheated serum test (TRUST) was positive at a dilution of 1: 16 and treponema pallidum particle agglutination (TPPA) test was positive. A human immunodeficiency virus antibody test was negative. Hepatitis B surface antigen, hepatitis B core antibody and hepatitis e antibody were positive. The electrocardiogram and chest radiograph showed no abnormalities. The computed tomography of the abdomen demonstrated local inhomogeneous and confounded thickening of the rectal wall, about 3 cm from the anal verge which was believed to represent an infiltrating tumor (Figure 1). The colonoscopy showed an irregular ulcerated mass, 3 cm from the anal verge, with hyperemia and erosion encircling the wall of the rectum (Figure 2A and B). A biopsy specimen was obtained for confirmation of the rectal mass. Histological findings of the biopsy showed extensive infiltration of a large number of lymphocytes, plasma cells and neutrophil granulocytes with formation of lymphoid follicles and ulcer but no heterotypic cells or lymph epithelial lesions (Figure 3). The patient was treated with intramuscular penicillin G benzathine, 2.4 million units per week for 3 wk[2]. Three wk later, the patient was asymptomatic and a repeat colonoscopy showed the rectal mass completely cleared (Figure 2C).
Syphilitic proctitis is observed exceedingly infrequently both because of its low clinical incidence and because of the lack of specific signs and symptoms. It is usually diagnosed as other anorectal disease such as a neoplasm[2]. For examples, in this case, symptoms and signs suggested rectal cancer. The findings from the computed tomography, the colonoscopy and colonoscopic biopsy specimen could not confirm the diagnosis. Fortunately, the positive findings from the routine TRUST and TPPA tests made us reevaluate the patient and led us to suspect syphilitic proctitis. This diagnosis was finally confirmed after the penicillin G benzathine therapy induced a rapid and completely regression of the rectal mass and the disappearance of symptoms. In summary, a high index of suspicion is important for this disease. The clinical, endoscopic and radiological appearance of syphilitic proctitis may easily be confused with rectal neoplasm. The most common symptoms of syphilitic proctitis are hematochezia, tenesmus, mucous discharge, and changes in bowel habit. The endoscopic appearance may vary from diffuse edema, erythematic, friable or multiple erosions, to ulceration[3]. Moreover, endoscopic rectal mucosal biopsies often show nonspecific chronic inflammation. Radiological appearance is also nonspecific. Serological testing for syphilis is very important for the diagnosis of the disease. We believe that this should be routinely performed on all patients admitted to hospital. If syphilis is considered and positive findings of the test are obtained, a diagnosis can be confirmed. The patient may then be treated appropriately, and spared unnecessary surgery.
| 1. | Faris MR, Perry JJ, Westermeier TG, Redmond J 3rd. Rectal syphilis mimicking histiocytic lymphoma. Am J Clin Pathol. 1983;80:719-721. |
| 2. | Song SH, Jang I, Kim BS, Kim ET, Woo SH, Park MJ, Kim CN. A case of primary syphilis in the rectum. J Korean Med Sci. 2005;20:886-887. |
| 3. | Bassi O, Cosa G, Colavolpe A, Argentieri R. Primary syphilis of the rectum--endoscopic and clinical features. Report of a case. Dis Colon Rectum. 1991;34:1024-1026. |
| 4. | Akdamar K, Martin RJ, Ichinose H. Syphilitic proctitis. Am J Dig Dis. 1977;22:701-704. |
| 5. | Quinn TC, Lukehart SA, Goodell S, Mkrtichian E, Schuffler MD, Holmes KK. Rectal mass caused by Treponema pallidum: confirmation by immunofluorescent staining. Gastroenterology. 1982;82:135-1398. |
Peer reviewer: Shouji Shimoyama, MD, Department of Gastrointestinal Surgery, University of Tokyo, Bunkyo-ku, Tokyo 113-8655, Japan