Published online Apr 28, 2016. doi: 10.4329/wjr.v8.i4.428
Peer-review started: November 9, 2015
First decision: December 7, 2015
Revised: January 21, 2016
Accepted: February 14, 2016
Article in press: February 16, 2016
Published online: April 28, 2016
Processing time: 162 Days and 9.4 Hours
The association between continuous-flow left ventricular assist devices (CF-LVADs) and gastrointestinal (GI) bleeding from angiodysplasia is well recognized. However, the association between continuous-flow biventricular assist devices (CF-BIVADs) and bleeding angiodysplasia is less understood. We report a case of GI bleeding from a patient with a CF-BIVAD. The location of GI bleeding was identified by nuclear red blood cell bleeding scan. The vascular malformation leading to the bleed was identified and localized on angiography and then by pathology. The intensity of bleeding, reflected by number of units of packed red blood cells needed for normalization of hemoglobin, as well as the time to onset of bleeding after transplantation, are similar to that seen in the literature for CF-LVADs and pulsatile BIVADs. While angiography only detected a dilated late draining vein, pathology demonstrated the presence of both arterial and venous dilation in the submucosa, vascular abnormalities characteristic of a late arteriovenous malformation.
Core tip: Gastrointestinal (GI) bleeding from angiodysplasia is a recognized complication in patients with continuous-flow left ventricular assist devices. The pathogenesis of the association, including coagulopathy and mechanics related to blood flow through the device, remains under investigation. We review a case of GI bleeding in a patient with a continuous-flow biventricular assist device.
- Citation: Mirasol RV, Tholany JJ, Reddy H, Fyfe-Kirschner BS, Cheng CL, Moubarak IF, Nosher JL. Gastrointestinal bleeding in a patient with a continuous-flow biventricular assist device. World J Radiol 2016; 8(4): 428-433
- URL: https://www.wjgnet.com/1949-8470/full/v8/i4/428.htm
- DOI: https://dx.doi.org/10.4329/wjr.v8.i4.428
Gastrointestinal (GI) bleeding is a well-recognized complication of continuous-flow left ventricular assist devices (CF-LVADs), with little known of the relative incidence or severity in patients with continuous-flow biventricular assist devices (CF-BIVADs). We describe a case of angiodysplasia leading to GI hemorrhage in a patient with a CF-BIVAD.
A 66 years old male with a history of congestive heart failure secondary to ischemic cardiomyopathy, with automatic implantable cardioverter defibrillator placement 14 years prior, presented for management of advanced heart failure. Comorbidities included chronic kidney disease and paroxysmal atrial fibrillation treated with 81 mg aspirin for several years with no significant bleeding complications.
In the hospital he was found to have bilateral deep venous thromboses. However, anticoagulation was held due to increased bleeding from his IV sites. A drop in platelets observed 1 week after admission was believed to be secondary to heparin induced thrombocytopenia, infection and congestive hepatopathy.
A Centrimag BIVAD (Thoratec Corporation) was placed 12 d after admission for hemodynamic stabilization pending eligibility for cardiac transplantation. The postoperative period was complicated by bleeding and multiple surgical re-explorations and wound closures. In his third postoperative week he developed melena and blood loss requiring transfusion of 6 units of blood.
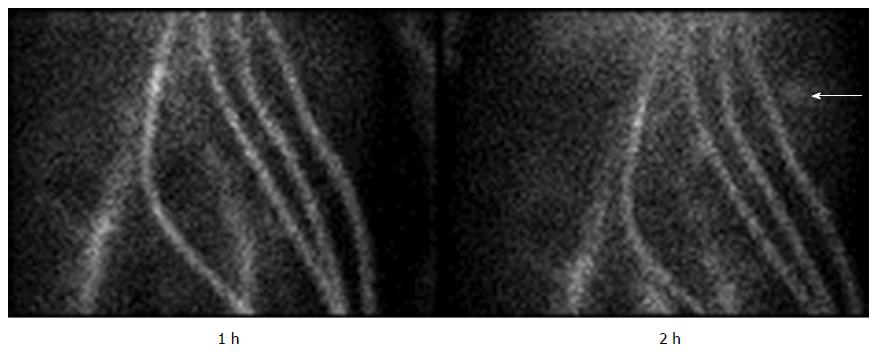
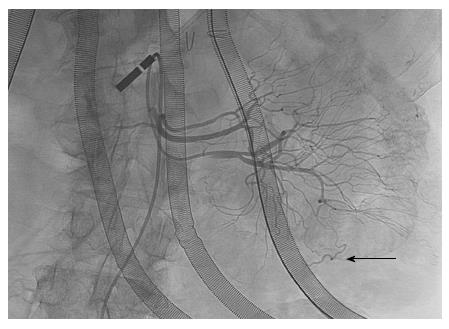
An unrevealing upper endoscopy was followed by capsule endoscopy showing fresh blood in the proximal small intestine but no obvious lesion. Superior mesenteric arteriography with selective injection of two proximal jejunal branches revealed a short venous segment with delayed washout. A red blood cell bleeding scan revealed bleeding in the left upper quadrant (Figure 1). Repeat arteriography of the superior jejunal branches redemonstrated the late draining vein (Figure 2), as well as a hypervascular jejunum.
The patient was taken to the operating room for exploratory laparotomy two days after angiography, where intraoperative upper endoscopy with telescoping past the ligament of Treitz demonstrated a large amount of blood in the small bowel and multiple small submucosal nodules in the proximal jejunum, which appeared to show stigmata of bleeding. The segment of affected bowel was resected and the remaining bowel anastomosed.
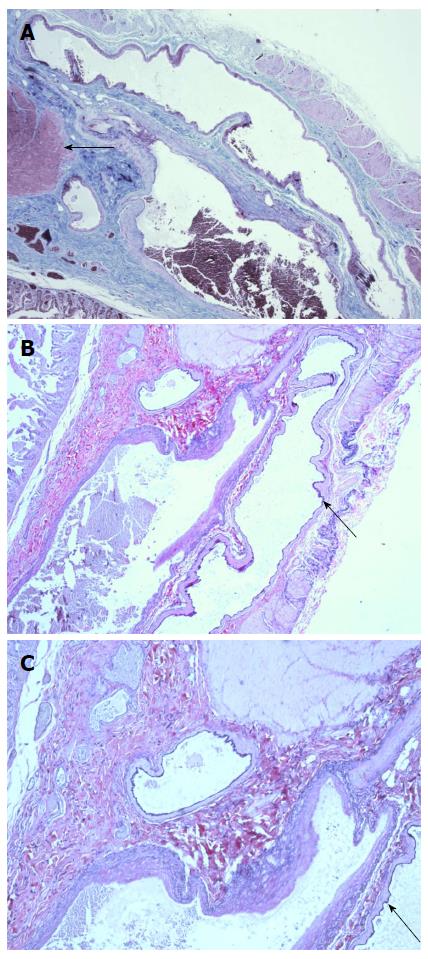
On pathological exam the resected bowel appeared grossly normal, without evidence of vascular ectasia. Paraffin sections of the small bowel were stained with hematoxylin and eosin, as well as Verhoeff-Van Gieson elastic stain. Microscopic examination showed normal mucosa, serosa, and subserosa. However, a focus of vascular ectasia involving the submucosa was noted, with attenuation of the muscularis layer (Figure 3). This vascular malformation (VM) consisted of tortuously dilated arteries and veins.
Ventricular assist devices (VADs) allow optimization of blood flow for patients either awaiting cardiac transplantation or ineligible for it. LVAD implantation involves cannulation of a ventricular inflow tract (the apex of the left ventricle) and outflow tract (the aorta). A portion of blood volume entering the left ventricle is diverted to a device that mechanically augments its flow to the systemic circulation. BIVADs require additional cannulation of the right atrium or, rarely, right ventricle, (inflow) and pulmonary artery (outflow), to similarly augment blood flow in patients with, or at high risk for, concomitant right ventricular failure[1,2].
Current VADs provide either pulsatile or continuous-flow. Pulsatile devices suffer from larger pumping units (precluding implantation in smaller patients) and, due to the multiple moving contact surfaces intrinsic to the pump design, less durability compared to continuous-flow units[3]. Consequently, continuous-flow devices are emerging as the preferred technology.
Letsou et al[3] first reported GI bleeding as a clinically significant complication specific to CF-LVADs in 3 patients receiving Jarvik 2000 devices. In all 3 patients the bleeding was attributed to VMs. Since that time, much of the literature has supported VMs as a prominent source of GI bleeding in patients with CF-LVADs[4-7]. Aquired von Willebrand deficiency, prophylactic anticoagulation, and mucosal ischemia may further predispose these patients to bleeding.
It is likely that the VMs seen in patients on CF-LVADs predate implantation of the device. Boley described GI VMs (angiodysplasias) as degenerative lesions of aging resulting from repeated bouts of muscular contraction that obstruct draining submucosal veins where they perforate the muscle layers of the bowel[8]. Over time increased intravascular pressure leads sequentially to dilation and tortuosity of superficial venous segments, dilation of the capillary ring and finally, failure of the precapillary sphincter. This ultimately results in arteriovenous shunting with the angiographic hallmark of angiodysplasia: An “early filling” or “early draining” vein associated with a cluster of abnormal vessels (dilated capillaries and venules). It’s conceivable that preexisting vascular dilation secondary to heart failure, hepatic congestion and increased portal pressure may prime the GI vasculature for such changes. Boley found 8 of 15 resected segments of colon from elderly patients with colon cancer contained large, dilated submucosal veins far from the tumor site in the absence of GI bleeding[8]. It is, therefore, not surprising that elderly patients destined for implantation with VADs may have occult GI vascular abnormalities without bleeding.
GI bleeding in CF-LVAD patients involves acquired hemostatic abnormalities, such as those seen in the context of aortic stenosis. Termed Heydes’ syndrome, the increased incidence of GI bleeding from angiodysplasia in patients with aortic stenosis has been associated with degradation of high-molecular weight multimers of von Willebrand factor (HMvWF). Blood flow across a stenotic aortic valve, as well as across the tortuous vessels of an AVM, is thought to expose HMvWF to increased sheer stress, causing conformational changes in the protein that make it susceptible to cleavage by the ADAMTS13 protease[9]. The cleaved vWF has reduced ability to induce platelet aggregation. Increased sheer stress is also thought to occur at the site of impeller movement in patients with CF-LVADS, and accordingly decreased levels of HMvWF have been observed in these patients following implantation[10]. A study by Cleveland et al[11] showed a greater than four times higher rate of any bleeding in patients with BIVADs compared to those with LVADs, even though 85% of the BIVAD patients had pulsatile (impeller-free) devices (vs 36% in the LVAD group). Similarly, Geisin et al[12] observed comparable degrees of vWF dysfunction between a small cohort of patients with pneumatically driven (impeller-free) BIVADS and CF-LVADs. Given the increased risk of bleeding for patients who are on impeller-free BIVADS, it is reasonable to speculate that recipients of BIVADS suffer comorbidities, such as congestive hepatopathy, that are absent in CF-LVAD patients and that predispose to bleeding.
Prophylactic anticoagulation regimens in post-implant patients with CF-LVADS may exacerbate coagulation defects leading to GI hemorrhage. However, anticoagulation itself may be insufficient to account for the increased rate of GI hemorrhage seen. As Crow observed, the rate of GI bleed in CF-LVAD patients was far higher than the rate of any bleeding expected in patients on anticoagulation for other reasons (e.g., 63 GI bleeds/100 patient-years in CF-LVAD patients vs 4.6 events/100 patient years in mechanical valve recipients)[5].
Our patient developed melena 3 wk after implantation, consistent with time to any bleeding event, including GI hemorrhage, in other studies assessing CF-LVADs and pulsatile BIVADs[4,5]. Furthermore, the transfusion of 6 units of blood to correct his hemoglobin prior to surgical resection of the diseased bowel was within the mode for first GI bleeding events in patients on those devices[4]. It is possible that the effect of CF-BIVAD therapy on GI bleeding may not be reflected by severity of bleeding in individual patients, but rather incidence of GI bleeding in the CF-BIVAD population.
While, Boley’s model predicted that GI AVMs were more likely to occur in the cecum, the portion of bowel with the largest diameter and presumably the highest wall tension, it has been seen that angiodysplasia may occur throughout the GI tract[1,13,14]. It is also interesting that von Willebrand disease has been associated with capillary dilation and tortuosity in the nail beds of young patients, suggesting that von Willebrand deficiency itself may have some role in growth of VMs[9].
Some authors speculate that the low pulse pressure of CF-LVADs may mimic that of aortic stenosis in that it predisposes to mucosal hypoxia and ulceration, increasing the likelihood of bleeding from angiodysplasia[3]. These pathological changes were not evident in our patient. A more compelling role for diminished pulsatility in GI bleeding after CF-VAD implantation exists in its relationship to vWF levels in the blood. Pulse pressure exposes endothelial cells to increased shear stress, which promotes release of HMvWF. It may be reasonable to assume that the narrowed pulse pressures seen with CF-VADs leads to decreased release of HMvWF and a predisposition to bleeding[15].
Tryptase released in response to antigenic components of the VAD may additionally account for the observed bleeding diathesis in VAD recipients[16]. Although tryptase levels were not measured in our patient, it is interesting to speculate that the coagulation abnormalities seen in this type of reaction may be attenuated by treatment of the anyphylactic reaction itself with anti-inflammatory medication, perhaps offering a supplemental avenue of therapy for GI bleeding in VAD recipients.
In our patient, selective angiography was the first diagnostic modality to identify an abnormality in the jejunal vasculature. While the most recognized angiographic findings in angiodysplasia are an early filling/late draining vein, nidus of VM, and supplying artery, this is a late manifestation of the disease. In our patient, angiography demonstrated the earliest manifestation of angiodysplasia, infrequently appreciated, consisting of a dilated vein with delayed drainage. However, pathology confirmed both dilated submucosal veins and associated dilated arteries, supporting the existence of angiodysplasia. It has been previously noted that the arterial, venous or nidus components of gastric angiodysplasia may be difficult to visualize on angiography - a shortcoming that may be remedied by air insufflation[17].
Patients with continuous-flow VADs are at higher risk for GI hemorrhage from angiodysplastic lesions. It should be recognized that the angiographic manifestations of these lesions include a spectrum of findings. Late lesions include an early draining vein associated with a cluster of vessels, including capillaries lacking pre- and post- capillary sphincters. Less recognized is the isolated late draining distended submucosal vein, the earliest manifestation of angiodysplasia.
We would like to thank the faculty, staff and patients at Robert Wood Johnson University Hospital for making this study possible. We would further like to thank the faculty and staff at Jersey Shore University Hospital for allowing the opportunity to complete this endeavor.
A 66-year-old male with congestive heart failure who presented with gastrointestinal (GI) bleeding after implantation of a biventricular assist device.
Arteriovenous malformation of the jejunum.
The differential diagnosis included arteriovenous malformation, coagulopathy, diverticulitis, hemorrhoids, however, localization of the bleed to the left upper quadrant, and subsequent resection of the diseased bowel and pathological identification of dilated, tortuous arteries and veins identified the etiology as an arteriovenous malformation.
Anemia by hemoglobin concentration, corrected by transfusion.
Late draining vein on mesenteric angiography, blood pooling on GI bleeding scan.
Paraffin sections of the small bowel were stained with hematoxylin and eosin, as well as Verhoeff-Van Gieson elastic stain, identifying tortuously dilated arteries and veins.
Bowel resection and anastomosis.
Ventricular assist device: Mechanical pump used to supplement blood flow from the pulmonary circulation to the systemic circulation or vice versa. Allows optimization of blood flow for patients with heart failure. Angiodysplasia: Aberrant arteriovenous connection in the GI tract. They represent a relatively uncommon source of GI bleeding.
Patients with continuous-flow HMvWFs are at risk for GI bleeding within weeks of implantation.
This is an interesting case.
| 1. | Loor G, Gonzalez-Stawinski G. Pulsatile vs. continuous flow in ventricular assist device therapy. Best Pract Res Clin Anaesthesiol. 2012;26:105-115. [PubMed] |
| 2. | Tsukui H, Teuteberg JJ, Murali S, McNamara DM, Buchanan JR, Winowich S, Stanford E, Mathier MA, Cadaret LM, Kormos RL. Biventricular assist device utilization for patients with morbid congestive heart failure: a justifiable strategy. Circulation. 2005;112:I65-I72. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 39] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 3. | Letsou GV, Shah N, Gregoric ID, Myers TJ, Delgado R, Frazier OH. Gastrointestinal bleeding from arteriovenous malformations in patients supported by the Jarvik 2000 axial-flow left ventricular assist device. J Heart Lung Transplant. 2005;24:105-109. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 175] [Cited by in RCA: 165] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 4. | French JB, Pamboukian SV, George JF, Smallfield GB, Tallaj JA, Brown RN, Smallfield MC, Kirklin JK, Holman WL, Peter S. Gastrointestinal bleeding in patients with ventricular assist devices is highest immediately after implantation. ASAIO J. 2015;59:480-485. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 5. | Crow S, John R, Boyle A, Shumway S, Liao K, Colvin-Adams M, Toninato C, Missov E, Pritzker M, Martin C. Gastrointestinal bleeding rates in recipients of nonpulsatile and pulsatile left ventricular assist devices. J Thorac Cardiovasc Surg. 2009;137:208-215. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 384] [Cited by in RCA: 376] [Article Influence: 20.9] [Reference Citation Analysis (0)] |
| 6. | Crow S, Chen D, Milano C, Thomas W, Joyce L, Piacentino V, Sharma R, Wu J, Arepally G, Bowles D. Acquired von Willebrand syndrome in continuous-flow ventricular assist device recipients. Ann Thorac Surg. 2010;90:1263-1269; discussion 1269. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 285] [Cited by in RCA: 270] [Article Influence: 16.9] [Reference Citation Analysis (0)] |
| 7. | Harvey L, Holley CT, John R. Gastrointestinal bleed after left ventricular assist device implantation: incidence, management, and prevention. Ann Cardiothorac Surg. 2014;3:475-479. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 28] [Reference Citation Analysis (0)] |
| 8. | Boley SJ, Sammartano R, Adams A, DiBiase A, Kleinhaus S, Sprayregen S. On the nature and etiology of vascular ectasias of the colon. Degenerative lesions of aging. Gastroenterology. 1977;72:650-660. [PubMed] |
| 9. | Loscalzo J. From clinical observation to mechanism--Heyde’s syndrome. N Engl J Med. 2012;367:1954-1956. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 131] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 10. | Meyer AL, Malehsa D, Budde U, Bara C, Haverich A, Strueber M. Acquired von Willebrand syndrome in patients with a centrifugal or axial continuous flow left ventricular assist device. JACC Heart Fail. 2014;2:141-145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 159] [Cited by in RCA: 170] [Article Influence: 15.5] [Reference Citation Analysis (0)] |
| 11. | Cleveland JC, Naftel DC, Reece TB, Murray M, Antaki J, Pagani FD, Kirklin JK. Survival after biventricular assist device implantation: an analysis of the Interagency Registry for Mechanically Assisted Circulatory Support database. J Heart Lung Transplant. 2011;30:862-869. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 32] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 12. | Geisen U, Heilmann C, Beyersdorf F, Benk C, Berchtold-Herz M, Schlensak C, Budde U, Zieger B. Non-surgical bleeding in patients with ventricular assist devices could be explained by acquired von Willebrand disease. Eur J Cardiothorac Surg. 2008;33:679-684. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 262] [Cited by in RCA: 265] [Article Influence: 14.7] [Reference Citation Analysis (0)] |
| 13. | Aggarwal A, Pant R, Kumar S, Sharma P, Gallagher C, Tatooles AJ, Pappas PS, Bhat G. Incidence and management of gastrointestinal bleeding with continuous flow assist devices. Ann Thorac Surg. 2012;93:1534-1540. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 143] [Cited by in RCA: 166] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 14. | Islam S, Cevik C, Madonna R, Frandah W, Islam E, Islam S, Nugent K. Left ventricular assist devices and gastrointestinal bleeding: a narrative review of case reports and case series. Clin Cardiol. 2013;36:190-200. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 28] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 15. | Baliga RR. From clinical observation to mechanism--Heyde’s syndrome. N Engl J Med. 2013;368:579. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 16. | Kounis NG, Tsigkas G, Almpanis G, Kouni SN, Kounis GN, Mazarakis A. Anaphylaxis-induced hyperfibrinogenolysis and the risk of Kounis syndrome: the dual action of tryptase. Am J Emerg Med. 2011;29:1229-1230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
P- Reviewer: Beltowski J, Kounis NG S- Editor: Ji FF L- Editor: A E- Editor: Jiao XK