Published online Jul 28, 2015. doi: 10.4329/wjr.v7.i7.180
Peer-review started: February 27, 2015
First decision: March 20, 2015
Revised: April 14, 2015
Accepted: May 7, 2015
Article in press: May 8, 2015
Published online: July 28, 2015
Processing time: 141 Days and 18.3 Hours
Echinococcosis is a zoonotic disease. Liver is the most common site of involvement. Renal involvement is seen in 2% to 3% of patients. Computed tomography findings in renal hydatid typically include: a cyst with thick or calcified wall, unilocular cyst with detached membrane, a multiloculated cyst with mixed internal density and daughter cysts with lower density than maternal matrix. Rarely type IV hydatid cysts may mimic hypovascular renal cell carcinoma. We report a case of previously asymptomatic middle aged female who presented with mild intermittent pain and a complex renal lesion on imaging which was considered to be a hypovascular renal carcinoma or urothelial neoplasm. However, by serendipity, the patient had spontaneous hydatiduria and later was definitively diagnosed and stented. Hydatid disease should always be considered amongst the top differential diagnosis of an isolated “complex” renal lesion which remains indeterminate on imaging.
Core tip: Renal hydatid is generally secondary to disseminated hydatidoses or associated with hepatic involvement. Isolated renal involvement is far less common and reported in less than 5% of all hydatid cases. Without appropriate history a subset of renal hydatid, especially type 4 cyst may simulate cystic renal/urothelial neoplasm or other complex cystic lesions such as abscess. Radiologists must harbour a high index of suspicion and look for subtle imaging signs such as calcification and non enhancing “solid” component to include this diagnosis in the differential of complex renal lesion. Absence of relevant history or hepatic involvement should not prevent diagnosticians from entertaining this rare diagnosis.
- Citation: Bhaya A, Shinde AP. Isolated renal hydatid presenting as a complex renal lesion followed by spontaneous hydatiduria. World J Radiol 2015; 7(7): 180-183
- URL: https://www.wjgnet.com/1949-8470/full/v7/i7/180.htm
- DOI: https://dx.doi.org/10.4329/wjr.v7.i7.180
Hydatid disease is mainly caused by Echinococcus granulosus[1]. It often manifests as a slow growing cystic lesion. We report a case of renal hydatid disease suspicious for complex cyst/urothelial neoplasm on computed tomography (CT) scan. The patient was extensively investigated and later presented with spontaneous hydatiduria.
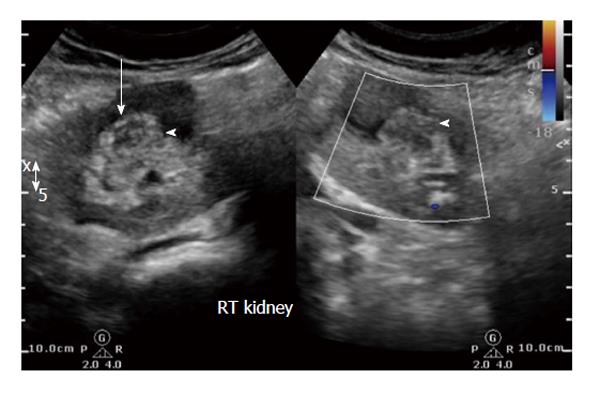
A 42-year-old female patient, resident of central India presented with mild right lumbar pain over one month. There was no dysuria, vomiting or fever. Routine laboratory investigations were within normal range except for urinary pus cells (10-12/hpf). Ultrasonography (USG) revealed a complex hetero-echoic lesion in the right kidney (Figure 1).
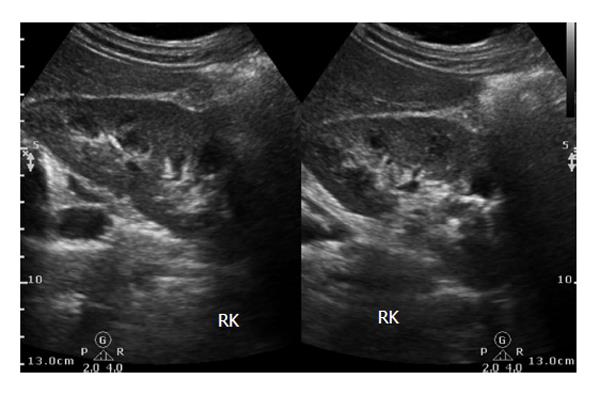
CT scan revealed a poorly demarcated lobulated, isodense lesion on plain images becoming better delineated on contrast study and measuring 2.2 (craniocaudal) cm × 2.8 (anteroposterior) cm × 3.5 (transverse) cm within interpolar region. The lesion exhibited few small irregular calcific foci and mild contrast enhancement. In addition, a hypo-attenuating, non-enhancing cystic area was noted adjacent to the lesion (Figure 2).
The right kidney revealed delayed contrast excretion. The previously noted cystic component did not opacify on the delayed scan. The left kidney was normal. The ureters and bladder were normal (Figure 3).
This was provisionally diagnosed as renal abscess possibly tubercular. The differential diagnosis of urothelial neoplasm was communicated to the referring general physician and urological consultation was strongly recommended.
A few days later she reported passage of fleshy/mucoid matter per urethra which she collected in a container. These were submitted for histopathological analysis. In view of high index of suspicion of a neoplastic lesion, the patient underwent ureteroscopy following which a double J stent was placed. Urine did not reveal any malignant cells. The patient improved clinically and was discharged on a course of antibiotics.
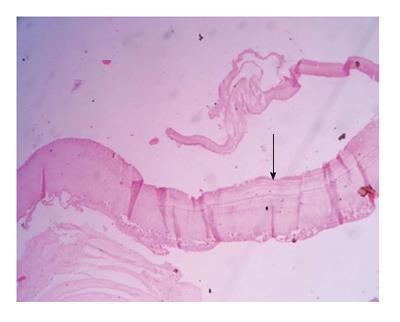
Gross examination: Multiple flat membranous pieces, the largest measuring 2 cm × 1 cm × 0.3 cm. These were greyish white, translucent and soft with smooth surfaces (Figure 4).
Microscopic examination: Lamellated layer with focal calcification and occasional brood capsules consistent with hydatid cyst (Figure 5).
Serological test for Echinococcus antibody was done and reported as positive. The patient remained asymptomatic. Follow up USG a month later revealed resolution of the lesion. The right kidney appeared normal without hydronephrosis (Figure 6). The left kidney and bladder were normal. No lesions were detected in the liver or spleen. The chest radiograph was unremarkable.
Echinococcosis is a zoonotic disease and is endemic in Mediterranean and other sheep rearing countries. However, due to increasing travel and tourism it may be found even in developed countries. In India, annual incidence of Hydatid disease per 100000 persons vary from 1 to 200[1]. The liver is most common site of involvement[2]. Renal involvement is seen in 2% to 3%[2,3].
Gharbi et al[4], classified hydatid cysts based upon sonographic morphology into five types (Table 1)[5].
| Type I | Well-defined, purely anechoic lesions that may be indistinguishable from simple renal cysts. Multiple echogenic foci due to hydatid sands may be seen in the cyst (22%) |
| Type II | Focal or diffuse detachment of the inner germinal layer results in a floating membrane inside the cyst (4%) |
| Type III | Multiseptated cysts with multiple daughter cysts (54%) |
| Type IV | Heterogeneous, solid appearance with infolded membranes, and internal echoes (12%) |
| Type V | Solid appearance, calcifications in the cyst wall, and germinative membranes (8%) |
Type 4 hydatid cysts have heterogeneous appearance similar to pseudotumor. CT scan is reportedly a problem solving modality in these cases especially as it is sensitive to calcifications and enhancement of the cyst wall[6].
Imaging spectrum of CT Renal hydatid varies and depends on stage of cyst. Typical CT findings for renal hydatidoses include a cyst with thick or calcified wall, a unilocular cyst with detached membrane, a multiloculated cyst with mixed internal density and daughter cysts with lower density than maternal matrix[4,6].
Despite multimodality imaging, in a subset of patients, no definitive diagnosis can be made and the differential diagnosis often includes infected renal cysts, abscess, pyonephrosis and neoplasms[7,8]. Rarely Type IV hydatid cysts may mimic hypo vascular renal cell carcinoma[9].
On the other hand, in endemic countries, unusual neoplasms such as mucinous cystadenoma/carcinoma may be misdiagnosed as renal hydatid[10].
Hydatiduria accompanies 10%-20% of cases of renal hydatidoses and is basically microscopic. Gross passage of hydatid cysts in urine though near diagnostic is rather uncommon and infrequently reported. We came across only two reports of gross hydatiduria in the Indian scenario - one with extensive liver and renal hydatid while the other revealed cystic renal lesion following investigation for hydatiduria. Both did not report any dilemma on imaging unlike our case[11,12].
Histologically, Hydatid cyst comprises of pericyst or fibrous layer, middle lamellated membrane and inner germinal layer which produces scolices. In patients with ruptured cysts and hydatiduria the membranes do not reveal pericyst[12].
Isolated renal hydatid involvement presents a further diagnostic challenge (as occurred in our patient). In our opinion, hydatid cyst should always be considered in the differential diagnosis of isolated complex cystic renal lesion. Absence of relevant history or hepatic involvement should not prevent diagnosticians from entertaining this rare diagnosis.
Renal hydatid may present with unusual imaging characteristics, resembling complex cyst or hypovascular solid-cystic neoplasm. This is particularly relevant in non-endemic countries wherein the Radiologists may not be aware of these unusual imaging features resulting in delayed and/or misdiagnosis.
Middle aged lady with non colicky right lumbar pain.
Neither tenderness nor any mass felt.
Chronic renal infection, renal stone disease or occult neoplasm.
Urine analysis revealed mild pyuria suggestive of urinary tract infection.
Ultrasound and computed tomography scan suspicious for urothelial cystic neoplasm.
Histopathology and microscopy suggestive of ruptured hydatid cyst.
Albendazole 15 mg/kg per day for 28 d followed by 2 wk interval and repeated total three cycles.
Enzyme-linked immunosorbent assay ELISA for detection of anti-Echinococcus antibodies (immunoglobulin G) was positive.
This is an interesting case.
| 1. | Eckert J, Deplazes P. Biological, epidemiological, and clinical aspects of echinococcosis, a zoonosis of increasing concern. Clin Microbiol Rev. 2004;17:107-135. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1121] [Cited by in RCA: 1218] [Article Influence: 55.4] [Reference Citation Analysis (1)] |
| 3. | Buckley RJ, Smith S, Herschorn S, Comisarow RH, Barkin M. Echinococcal disease of the kidney presenting as a renal filling defect. J Urol. 1985;133:660-661. [PubMed] |
| 4. | Gharbi HA, Hassine W, Brauner MW, Dupuch K. Ultrasound examination of the hydatic liver. Radiology. 1981;139:459-463. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 5. | Zmerli S, Ayed M, Horchani A, Chami I, El Ouakdi M, Ben Slama MR. Hydatid cyst of the kidney: diagnosis and treatment. World J Surg. 2001;25:68-74. [PubMed] |
| 6. | Pedrosa I, Saíz A, Arrazola J, Ferreirós J, Pedrosa CS. Hydatid disease: radiologic and pathologic features and complications. Radiographics. 2000;20:795-817. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 498] [Cited by in RCA: 501] [Article Influence: 19.3] [Reference Citation Analysis (0)] |
| 7. | Turgut AT, Altin L, Topçu S, Kiliçoğlu B, Aliinok T, Kaptanoğlu E, Karademir A, Koşar U. Unusual imaging characteristics of complicated hydatid disease. Eur J Radiol. 2007;63:84-93. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 67] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 8. | Horchani A, Nouira Y, Kbaier I, Attyaoui F, Zribi AS. Hydatid cyst of the kidney. A report of 147 controlled cases. Eur Urol. 2000;38:461-467. [PubMed] |
| 9. | Nouira K, Nouira Y, Belhiba H, Mekni A, Menif E, Horchani A. A misleading renal tumour. Tunis Med. 2007;85:535-536. [PubMed] |
| 10. | Sonmez FC, Esen HH, Tavlı L, Kılınç M. Well-Differentiated Mucinous cystadenocarcinoma of the renal pelvis. Eur J Gen Med. 2014;Suppl 1:63-65. [RCA] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 11. | Saxena S, Gupta R, Nigam DK, Tahiliani ND, Saxena KN. Hydatid cyst of kidney presenting as hydatiduria. J Assoc Physicians India. 1990;38:359-356. [PubMed] |
| 12. | Mongha R, Narayan S, Kundu AK. Primary hydatid cyst of kidney and ureter with gross hydatiduria: A case report and evaluation of radiological features. Indian J Urol. 2008;24:116-117. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 29] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
P- Reviewer: Nishio K, Schoenhagen P S- Editor: Ji FF L- Editor: A E- Editor: Liu SQ
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/