Published online Aug 28, 2013. doi: 10.4329/wjr.v5.i8.275
Revised: June 17, 2013
Accepted: July 23, 2013
Published online: August 28, 2013
Processing time: 134 Days and 12.7 Hours
Renal injuries are classified, based on the American Association for the Surgery of Trauma classification, in to five grades of injury. Several imaging modalities have been available for assessing the grade of renal injury, each with their usefulness and limitations. Currently, plain radiographs and intravenous urography have no role in the evaluation of patients with suspected renal injury. Ultrasonography (USG) has a limited role in evaluating patients with suspected retroperitoneal injury; however, it plays an important role during follow up in patients with urinoma formation. USG helps to monitor the size of a urinoma and also for the drainage procedure. The role of selective renal arteriography is mainly limited to an interventional purpose rather than for diagnostic utility. Retrograde pyelography is useful in assessing ureteral and renal pelvis integrity in suspected ureteropelvic junction injury and for an interventional purpose, like placing a stent across the site of ureteric injury. Magnetic resonance imaging has no role in acute renal injuries. Multidetector computed tomography is the modality of choice in the evaluation of renal injuries. It is also useful in evaluating traumatic injuries to kidneys with preexisting abnormalities and can help to define the extent of penetrating injuries in patients with stab wounds in the flank region. The combination of imaging findings along with clinical information is important in the management of the individual patient. This article will describe a spectrum of renal injuries encountered in a trauma setting.
Core tip: Renal trauma is frequently seen following blunt and penetrating injuries. Surgery, as a method of treatment, is frequently required in severe injuries, with most minor injuries managed conservatively. Apart from the surgical grading by the American Association, an imaging-based grading system is now frequently used and helps to decide further management. Multidetector computed tomography is now the imaging modality of choice and can depict even the severest injuries. Depending upon the imaging findings, patients may be taken for interventional procedures rather than surgery. The American Association for the Surgery of Trauma classification has been updated, with vascular injuries now included, denoting a Grade V injury.
- Citation: Dayal M, Gamanagatti S, Kumar A. Imaging in renal trauma. World J Radiol 2013; 5(8): 275-284
- URL: https://www.wjgnet.com/1949-8470/full/v5/i8/275.htm
- DOI: https://dx.doi.org/10.4329/wjr.v5.i8.275
Trauma is a leading cause of morbidity and mortality all over the world. Blunt abdominal trauma accounts for more abdominal injuries than the less frequent penetrating injuries[1]. Spleen and liver are the most common visceral organs to be affected in blunt trauma to the abdomen, followed by genitourinary injury, involved in only 3%-10% of cases[2]. The kidneys are located high up in the retroperitoneum, well protected and cushioned by the peritoneum and abdominal viscera anteriorly and by the tough musculoskeletal structures of the posterior abdominal wall posteriorly. The kidney is the most commonly injured organ of the genitourinary system and renal injuries account for only 1%-5% of all abdominal injuries[3]. Of all the incurred injuries, over 95% are minor injuries and can be managed with conservative therapy with no significant complications. It is only the more grave injuries, like renal fracture or shattering, renal pedicle injury or avulsion and severe pelvicalyceal system (PCS) injury, which require active intervention or even surgery. Contrast enhanced computed tomography (CECT) is the modality of choice for evaluation of renal injures today and can delineate the various grades of injury and associated complications[1-4].
A computed tomography (CT) scan performed with contrast enhancement is the modality of choice for evaluating renal injuries today. CT is easily available these days at most trauma centers, provides images that are easy to interpret and can demonstrate all the findings which correlate with surgical observation. Administration of contrast also provides information about renal vessels and renal function which is useful in evaluating devascularization and pelvicalyceal system injury[1-5]. Ultrasonography (USG), intravenous pyelogram (IVP), magnetic resonance imaging (MRI) and arteriography are various other imaging modalities used in radiological evaluation in a suspected renal injury, with each having its limitations. Apart from CT, USG is the other modality which has always been at hand and has evolved with time and upgrading of machines. Nowadays, portable USG machines with higher resolution and better Doppler capabilities are widely available at most centers. Because of its benefits, like portability, no radiation exposure, minimal scanning time, ease of performing at bedside while the patient is being evaluated and managed in an emergency, and contrast agents not being used, USG has become an initial screening tool performed in all patients with an abdominal injury. It has a sensitivity of 80%-90% for detecting intra-abdominal fluid but is relatively insensitive for parenchymal injuries and retroperitoneal hemorrhage[1,2,6,7].
Patients sustaining trauma undergo a total clinical and radiological evaluation. A focused assessment sonography in trauma (FAST) is done as part of this initial evaluation. FAST is done to look for the presence of intraperitoneal fluid, which in trauma settings suggests hemoperitoneum. It allows the timely diagnosis of potentially life threatening hemorrhage and acts as a decision making tool to help determine the need for transfer to the operating room, CT scanner or angiography suite. A positive FAST correlates well with associated abdominal injury[1,2,6,7]. However, USG is insensitive for retroperitoneal hemorrhage and may not pick up minor renal injuries. The presence of free fluid in a hemodynamically unstable patient warrants surgical exploration. Hemodynamically stable patients with free fluid in the abdomen or patients with hematuria, even without free fluid in the abdomen, need further evaluation with CECT[3,4].
MRI is an alternative in patients who have contraindications to administration of contrast or sometimes in pregnant patients. It provides good anatomic details but is time consuming and suffers the brunt of motion artifacts in these acutely injured patients. It provides only limited excretory information as dilution of excreted contrast leads to poor resolution, superimposed with the poor breath holding capabilities of these patients. Angiography is seldom performed for suspected renal injuries as CT can non-invasively provide all the required information. Angiography is now performed only with intent of treatment of certain conditions, like embolization for pseudoaneurysm or active bleeding and thrombolysis and stenting for revascularization of acute renal artery thrombosis. The European Association of Urology (EAU) has laid down guidelines for performing radiological evaluation in suspected renal injury.
EAU Guidelines on Radiographic Assessment[3]: (1) any patient with hematuria (macroscopic or microscopic) with hemodynamic instability (systolic blood pressure < 90 mmHg); (2) patients sustaining rapid deceleration injury and/or with significant associated injuries; and (3) renal injuries (hematuria) in hemodynamically stable patients.
The use of focused ultrasonography has now become an extension of the physical examination of the trauma patient and is conveniently used in the primary survey and triage of patients[1-5]. Mostly, kidneys are imaged as a part of the routine abdominal scan performed to look for injuries of other commonly injured abdominal viscera. It can detect renal lacerations but cannot definitely assess their depth and extent and does not help in differentiating extravasated blood from a urinoma. There is the chance one could miss a small lesion, with a retroperitoneal hemorrhage or when there is a concomitant other solid visceral injury present. In the presence of hematuria, even a negative scan does not rule out an underlying injury and a decision on further management is based on the clinical status of the patient[2,3]. The protocol for the management of patients with suspected renal injury broadly divides patients into three groups: (1) patients with hemodynamic instability usually warrants surgical exploration, whereas patients who have been stabilized after initial poor scores may undergo a CT scan or a repeat FAST and further decisions can be taken accordingly; (2) patients who are hemodynamically stable and have hematuria should undergo a CT scan; and (3) patients who are hemodynamically stable, have no hematuria and negative FAST results should be followed up with clinical observation of at least 6 h duration.
Multidetector computed tomography is considered the gold standard method for the radiographic assessment of patients with renal trauma and has completely replaced IVP[1-5,8-10].
With a short examination time, CT provides all the necessary information relating to the degree of parenchymal injury with or without involvement of PCS and renal vascular injuries and also provides information regarding the functional status of the kidneys. Doing a phasic scan also helps in differentiating active hemorrhage from urine extravasation. With the wider availability of newer CT machines and helical multislice scanners, much faster scanning, increased volume coverage and improved multiplanar reconstruction ability now can provide high quality images with shorter time on the table for the patient. As most of the patients undergoing CT scan are not so co-operative in breath holding, motion artifacts can frequently compromise the study and lead to added confusion in interpreting the scan. Faster imaging with multislice scanner and multiplanar reconstruction can help to overcome these problems and provide an accurate assessment of injury.
A CT scan should be performed after intravenous contrast administration (75-100 mL of non ionic contrast agent, 300-400 mg concentration of iodine). It helps differentiate minor injuries from those requiring aggressive management. Usually the imaging is done in the portal venous phase, 45-60 s after initiation of contrast injection. This corresponds to the early nephrographic phase of renal parenchymal enhancement which is suited for picking up the parenchymal lacerations and devascularized segments, if any[1,2,11-13]. Also, optimal contrast in the renal arteries at this time helps to evaluate renal pedicle injury. Further additional delayed scans may be needed and should be tailored according to the information required and individualized to reduce radiation dose. An immediate delayed phase scan can be added to confirm an arterial extravasation if seen in the earlier scan, which will now be seen to spread with contrast density higher than that in the adjacent arteries. If a PCS injury is suspected, a 3 to 5 min limited section low dose delayed scan can help to confirm a urinary extravasation[1,2,10,12,13].
Ever since the development of the organ injury scaling in 1987 for studying the effects of trauma on several organs, there have been several modifications, with in-depth understanding in management of these patients and with the development of several classification scales based on both imaging and surgical standards[1,2,10]. The Committee on Organ Injury Scaling of the American Association for the Surgery of Trauma (AAST) has developed a widely accepted grading scale which also ensures a common consensus between surgeons and radiologists for proper management of renal injuries[1-3,5,8]. Abdominal CT or direct renal exploration is used to accomplish injury classification. As for other injured organs, the ASST classification system is the now the standard adopted method for radiological reporting and the classification system used in renal trauma. Renal injuries are divided in to five grades.
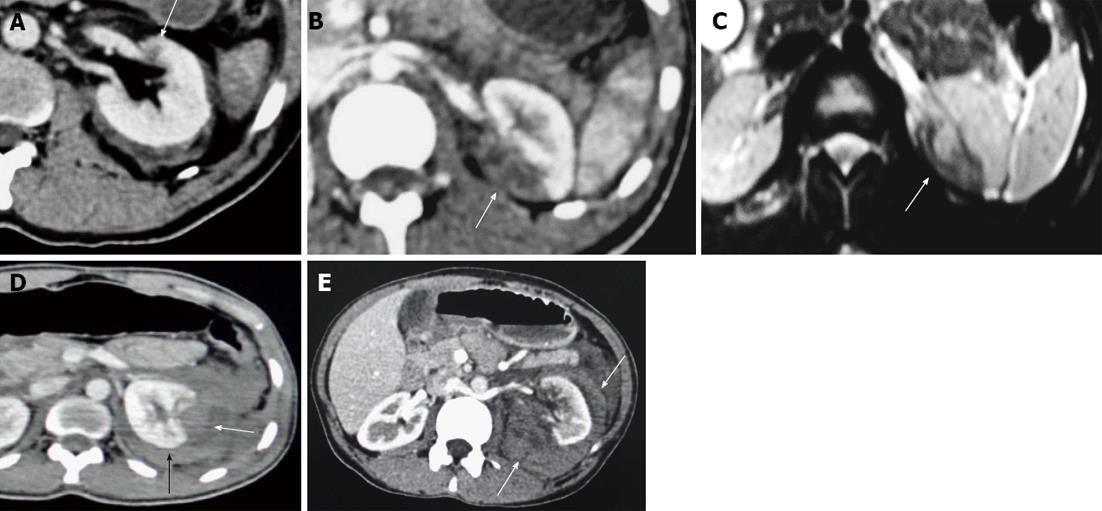
Contusion is described as an ill-defined and poorly marginated hypodense area of decreased enhancement on the nephrographic phase that may show delayed or persistent enhancement (Figure 1A).
Infarctions can be confused with contusions. Infarcts are wedge shaped, sharply marginated hypodense areas seen on the nephrographic phase and show no delayed enhancement (Figure 1B and C).
Subcapsular hematomas are seen as crescentic or biconvex area of blood collection along the renal contour, causing flattening or depression of the underlying renal surface (Figure 1D). These are differentiated from “perinephric hematoma” (Figure 1E) which is confined between the renal parenchyma and Gerota’s fascia, outlining the renal contour extending over a wider area without producing flattening or depression of renal margins, and occurs following a laceration of the renal capsule.
Lacerations are irregular linear hypodense areas of parenchymal defect reaching up to the surface, causing disruption of parenchymal continuity. It may be complex with variable width of the clefts that may be filled with blood clots. They also do not show enhancement.
Shattered kidney refers to multiple lacerations causing gross disruption and fragmentation of the renal parenchyma, often associated with renal function compromise, injuries to the collecting system with urinary extravasation and severe hemorrhage with active arterial bleeding. The fragments may retain their blood supply if spared or may be completely devascularized.
Pseudoaneurysm is a focal rounded well circumscribed lesion within the renal parenchyma or in the lacerated segment that shows intense arterial enhancement similar to that of the attenuation of the blood pool and washout synchronous to the blood pool. There is no expansion on delayed phase scans[1,2].
Active arterial extravasations: focal ill defined areas of contrast leak with different configurations with high attenuation values (85 to 370 HU)[2] on early scans and will appear as more hyper-attenuating than the blood pool and show spread and expansion in to surrounding tissue on a delayed scan[1,2].
Grade I injury
Grade I injury is characterized by contusion or nonexpanding subcapsular hematoma without parenchymal laceration. Other finding would include limited perinephric hematoma and small subsegmental infarct. Grade I injuries account for most renal injuries (approximately 80%) presenting clinically with mild or gross hematuria and are managed conservatively[1,2](Figure 2).
Grade II injury
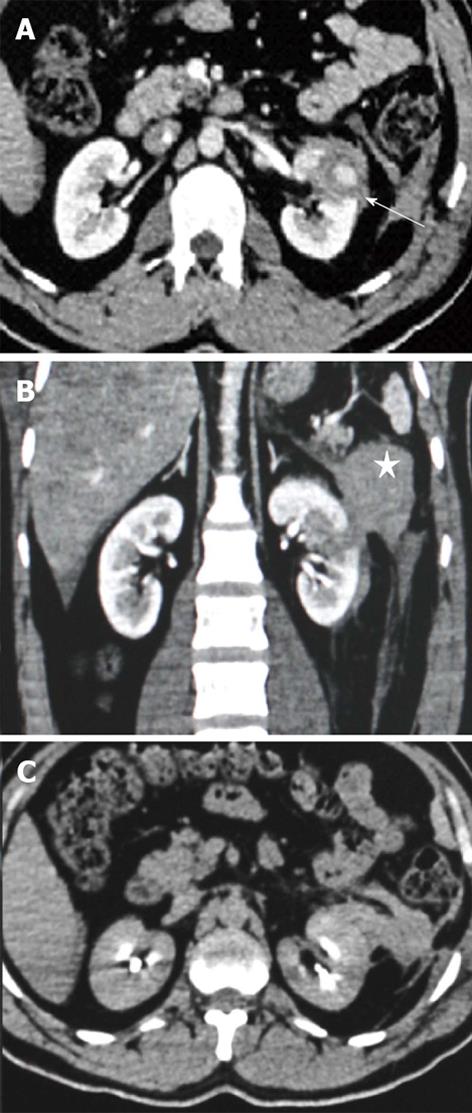
Grade II renal injuries are characterized by nonexpanding perinephric hematoma confined to the retroperitoneum or cortical laceration < 1 cm deep without involvement of the collecting system. Other associated findings are thickening of the lateroconal fascia, compression of the colon, and displacement of the kidney by the perirenal hematoma. These patients are managed conservatively (Figure 3).
Grade III injury
It is only the depth of the renal laceration which differentiates a Grade II injury from Grade III. Grade III renal injuries are characterized by nonexpanding perinephric hematoma confined to the retroperitoneum and by laceration extending more than 1 cm in depth. The laceration may involve the medulla but there is no PCS injury which is determined on the excretory phase image by demonstrating a lack of urinary extravasations (Figure 4).
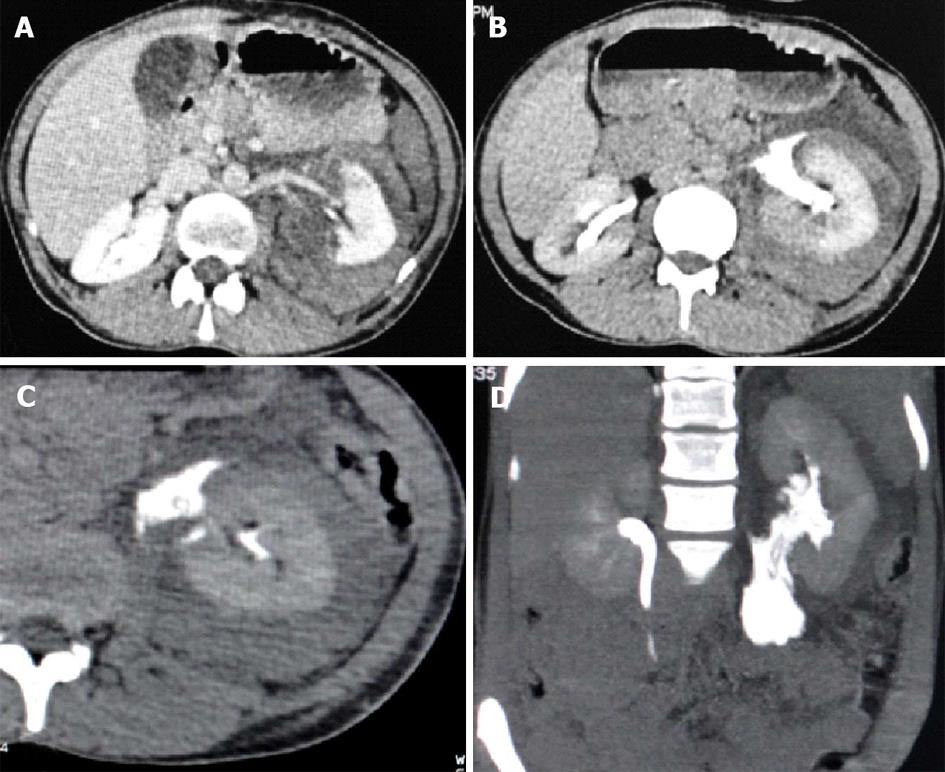
Grade IV injury
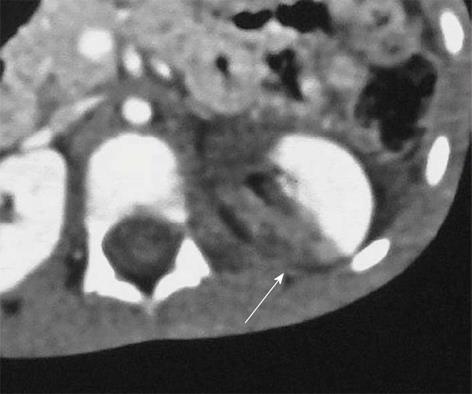
Grade IV injury includes injuries of the main renal artery or vein with contained hemorrhage and injury leading to segmental devascularization and lacerations involving the PCS. In addition, multiple renal lacerations, expanding subcapsular hematomas and fractured kidney are included in this grade. The presence of a hematoma in the perihilar location and medial aspect of the kidney or deeper lacerations extending up to the hilum should raise the possibility of PCS injury and an excretory phase scan is needed to confirm the urinary leak (Figures 5-7).
Grade V injury
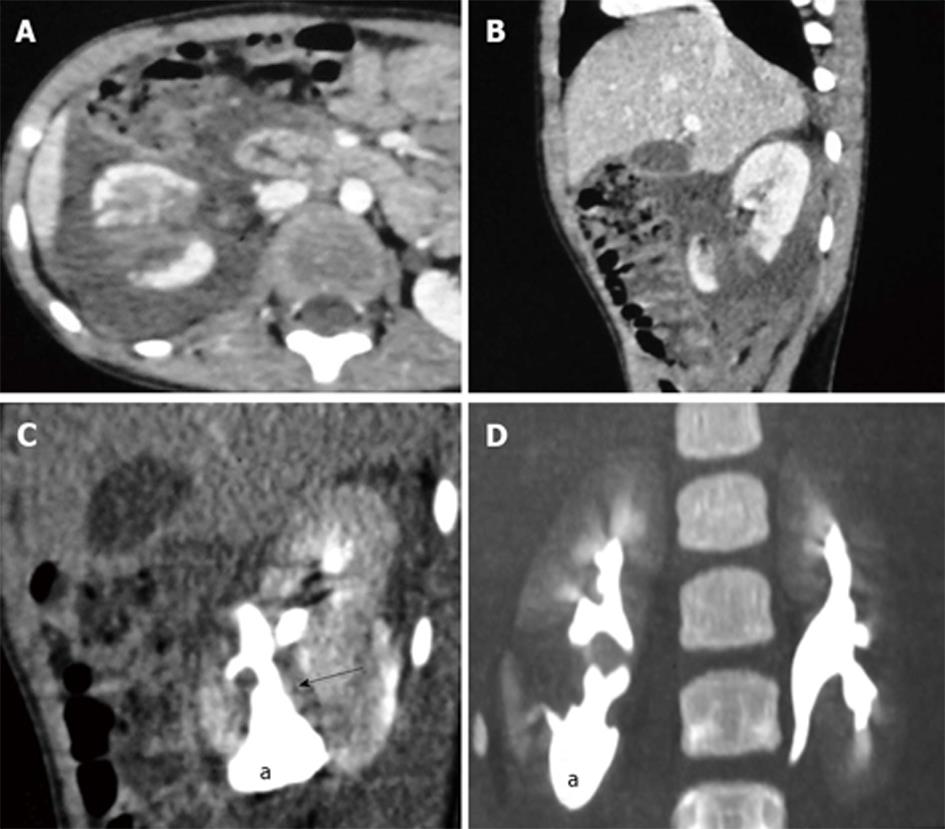
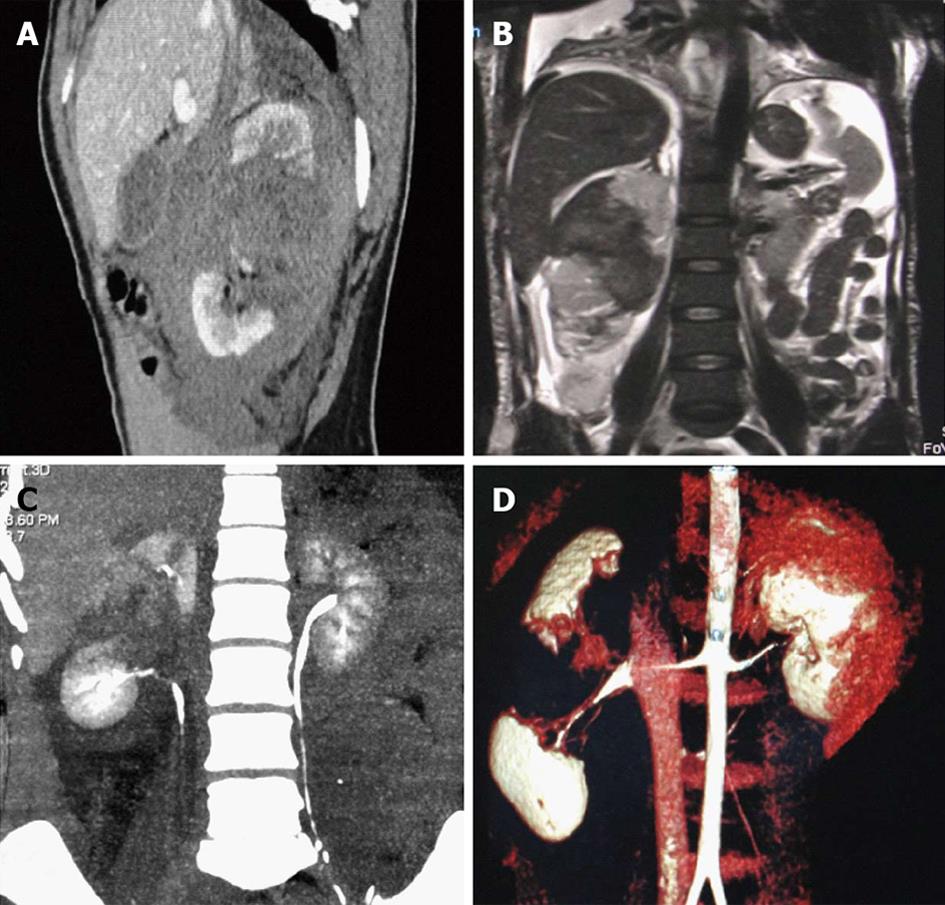
Grade V is the highest grade of renal injury, characterized by avulsion of the pelviureteric junction (Figure 8). It occurs as a result of a sheering injury at this point of fixation as it gets stretched over the transverse process and leads to PUJ disruption. They can be partial or complete, with the presence of a hematoma or urinoma in the medial and perihilar region of the kidney. Extravasation of opacified urine on excretory phase scans (Figure 8B-D) with opacification of the ureter distal to the injury helps confirm the diagnosis and differentiate complete from partial injury. In complete avulsion, no ureter beyond the injury would be seen and the patient would need a surgical repair, while in a partial tear, there will be opacification of the ureter distally and these patients could be managed by minimal invasive techniques like placing a ureteric stent across the injury site or urinary diversion through a percutaneous nephrostomy tube. Surgery may be opted for if the above conservative methods fail to heal the injury.
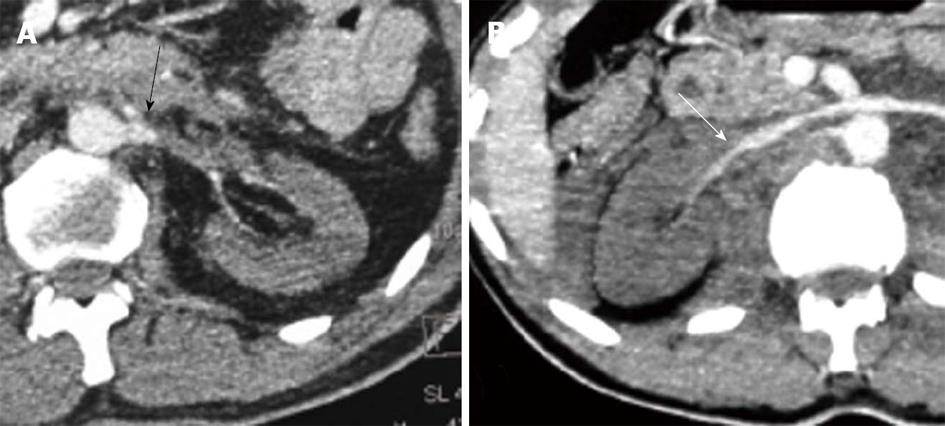
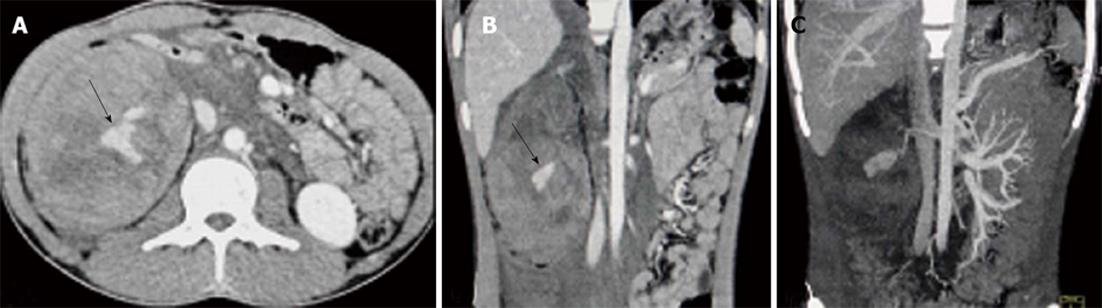
Other types of injuries include renal pedicle injury (Figure 9) and shattering of renal parenchyma (Figure 10) with or without urinary or arterial contrast extravasation. Renal pedicle injury can lead to thrombosis of the artery (Figure 9A) or vein and subsequent devascularization of the kidney or complete laceration leading to the avulsion of the renal pedicle. It is commonly seen in injuries where there is sudden deceleration injury or hyperextension of the spine leading to stretching of the renal vessels in the retroperitoneum and intimal tear with subsequent thrombus formation that occludes the main renal artery. The site of occlusion is seen as the cutoff of the main renal artery on a contrast enhanced CT scan with the absence of renal parenchymal enhancement. There would be no perinephric hematoma. In some cases, there may be an intact blood supply from capsular, peripelvic and periureteric vessels which produce a thin capsular and subcapsular enhancement, referred to as the “cortical rim sign”. Another finding that may suggest devascularization is retrograde filling of the ipsilateral renal vein (Figure 9B) from the inferior vena cava. Renal pedicle avulsion on the other hand is a complete tear of all the layers of the vessel wall and so will have a hematoma around the aorta and renal hilum with active contrast extravasation from the disrupted stump. There will be no renal perfusion. These patients show signs of hemodynamic instability and it may prove lethal if not managed in time. Renal vein injuries are extremely uncommon. On a CECT, there may be the presence of a filling defect in the enlarged renal vein or signs of back pressure changes, such as nephromegaly with differential and delayed progression on the nephrogram compared to the normal opposite kidney. A complete transaction of the renal vein may not be assessed on CT but may be suspected in the presence of a large perihilar or expanding hematoma.
The ASST does not describe pseudoaneurysm or active bleeding (Figure 11) in any of the grades as it is a surgical grading system based on the appearance at surgery, but there are several radiological grading systems which classify them into higher renal injury categories needing either close follow up or surgical or endovascular interventions[5,13]. In a well preserved renal function, a pseudoaneurysm or focal arterial extravasation could be effectively embolized, leaving surgery as an option for more severe injuries.
Grades I, II and III remain unchanged[14] (Table 1).
| Grade | Type of injury | Injury description |
| I | Contusion | Microscopic or gross hematuria, normal urological studies |
| Hematoma | Nonexpanding subcapsular hematomas with no parenchyma laceration | |
| II | Hematoma | Nonexpanding perinephric (perirenal) hematomas confined to the retroperitoneum |
| Laceration | Superficial cortical lacerations less than 1 cm in depth without pelvicalyceal system injury or urinary extravasation | |
| III | Lacerations | Deeper lacerations, more than 1 cm in depth without Pelvicalyceal system injury |
| IV | Laceration | Renal lacerations extending through the renal cortex, medulla and collecting system |
| Injuries involving the main renal artery or vein with contained hematoma | ||
| Vascular injury | Segmental infarctions without associated lacerations | |
| V | Laceration | Completely shattered kidney Ureteropelvic junction injury |
| Vascular injury | Complete laceration (avulsion) or thrombosis of the main renal artery or vein that devascularizes the kidney |
Change in Grade IV
Originally: renal lacerations involving the collecting system, injuries involving the main renal artery or vein with contained hemorrhage, and segmental renal infarctions.
Revision: adds segmental arterial and venous injury, and laceration to the renal pelvis or pelviureteric junction. Shattered kidney is now in Grade IV from Grade V.
Change in Grade V
Originally: included shattered kidney, pelviureteric junction injury and laceration or avulsion of main renal artery or vein.
Revision: now includes only vascular injury (arterial or venous), i.e., laceration, avulsion or thrombosis.
The radiological assessment and reporting of the renal injury should provide a clear insight of the grade and severity of injury following the ASST renal injury grading system that helps to decide on the treatment options for these patients. Although not detailed in the classification system, active arterial extravasation and pseudoaneurysm should suggest a higher grade injury and patients should be kept under close follow up and be provided with early intervention if needed[1,2]. Most renal injuries are low grade (Grades 1-3) and treated conservatively. However, intervention may be needed in these cases in the presence of active arterial bleeding which can, in most cases, be taken care of by angiographic embolization, with surgery needed in those with hemodynamic instability. Grade 4 injuries can also be given a trial of conservative management provided the patient is hemodynamically stable, with no expanding hematomas. The PCS injury and urinary extravasation can also be resolved with a conservative approach, sometimes assisted with stenting, percutaneous nephrostogram or drainage of urinoma. In cases resolution failure, surgical repair or nephrectomy may be warranted. Grade 5 injuries with complete ureteropelvic disruption and renal pedicle avulsion need surgical repair. However, partial ureteropelvic injury can be managed with stenting or proximal urinary divergence. Renal artery thrombosis and devascularization can be managed with thrombolysis or stenting to preserve renal function if intervention is within a few hours of injury. Others may need a nephrectomy. Partial nephrectomy remains an option in those in whom a reasonable amount of functional renal parenchyma can be preserved[1,2,3,10]. Surgical exploration has been frequently performed for penetrating wounds until recently. However, stable patients with low-velocity gunshot and stab wounds of a minor degree may be managed conservatively with wider antibiotic coverage and follow up. Penetrating wounds should be explored only if they involve the hilum or are associated with urinary leak or active bleeding[2,3].
Follow up imaging is sometimes needed to look for resolution of injuries. It is usually not indicated for Grade I-III blunt renal injuries and Grade IV renal injuries without urinary extravasation. Follow up imaging (CECT) is indicated in patients who had Grade IV injuries with urinary leak on previous scan, Grade V renal injuries that were managed conservatively, patients with signs of complications (fever, fall in hematocrit level or clinical instability) and with other associated comorbidities[3,15].
Patients with hematuria after abdominal trauma should raise suspicion for renal injury; however, hematuria may not be present in patients with main renal artery thrombosis and devascularization. Radiological evaluation is needed to further confirm and grade the injury. FAST is a rapid and well accepted tool for triage of these patients. CECT is the modality of choice to grade the renal injuries based on the AAST classification system and also to look for associated complications. CT, usually performed in a single phase (early nephrographic), provides information about parenchymal injuries and it is in this phase that other visceral organs can also be evaluated. However, to seek further information regarding renal function, PCS injury and confirming arterial extravasations, additional delayed images may be acquired. Most renal injuries can be managed conservatively. Procedures like urinary divergence, stenting for PCS or ureteric injury, and angioembolization for pseudoaneurysm or active bleeding, are minimally invasive procedures which expand the borders for conservative management and surgery is needed only in those with higher grade injuries or in those with failure of conservative management.
P- Reviewers Abdel-Razek AAK, El-Ghar MA, Nouh MR, Sijens PE, Saeed M S- Editor Gou SX L- Editor Roemmele A E- Editor Liu XM
| 1. | Lee YJ, Oh SN, Rha SE, Byun JY. Renal trauma. Radiol Clin North Am. 2007;45:581-592, ix. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 47] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 2. | Alonso RC, Nacenta SB, Martinez PD, Guerrero AS, Fuentes CG. Kidney in danger: CT findings of blunt and penetrating renal trauma. Radiographics. 2009;29:2033-2053. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 92] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 3. | Lynch TH, Martínez-Piñeiro L, Plas E, Serafetinides E, Türkeri L, Santucci RA, Hohenfellner M. EAU guidelines on urological trauma. Eur Urol. 2005;47:1-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 200] [Cited by in RCA: 189] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 4. | Sandler CM, Amis ES, Bigongiari LR, Bluth EI, Bush WH, Choyke PL, Fritzsche PJ, Holder LE, Newhouse JH, Segal AJ. Diagnostic approach to renal trauma. American College of Radiology. ACR Appropriateness Criteria. Radiology. 2000;215 Suppl:727-731. [PubMed] |
| 5. | Kawashima A, Sandler CM, Corl FM, West OC, Tamm EP, Fishman EK, Goldman SM. Imaging of renal trauma: a comprehensive review. Radiographics. 2001;21:557-574. [PubMed] |
| 6. | Poletti PA, Kinkel K, Vermeulen B, Irmay F, Unger PF, Terrier F. Blunt abdominal trauma: should US be used to detect both free fluid and organ injuries? Radiology. 2003;227:95-103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 91] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 7. | McGahan JP, Richards J, Gillen M. The focused abdominal sonography for trauma scan: pearls and pitfalls. J Ultrasound Med. 2002;21:789-800. [PubMed] |
| 8. | Smith JK, Kenney PJ. Imaging of renal trauma. Radiol Clin North Am. 2003;41:1019-1035. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 33] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 9. | Park SJ, Kim JK, Kim KW, Cho KS. MDCT Findings of renal trauma. AJR Am J Roentgenol. 2006;187:541-547. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 26] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 10. | Goldman SM, Sandler CM. Urogenital trauma: imaging upper GU trauma. Eur J Radiol. 2004;50:84-95. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 24] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 11. | Nguyen D, Platon A, Shanmuganathan K, Mirvis SE, Becker CD, Poletti PA. Evaluation of a single-pass continuous whole-body 16-MDCT protocol for patients with polytrauma. AJR Am J Roentgenol. 2009;192:3-10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 84] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 12. | Jankowski JT, Spirnak JP. Current recommendations for imaging in the management of urologic traumas. Urol Clin North Am. 2006;33:365-376. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 13. | Razali MR, Azian AA, Amran AR, Azlin S. Computed tomography of blunt renal trauma. Singapore Med J. 2010;51:468-473; quiz 474. [PubMed] |
| 14. | Buckley JC, McAninch JW. Revision of current American Association for the Surgery of Trauma Renal Injury grading system. J Trauma. 2011;70:35-37. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 68] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 15. | Davis P, Bultitude MF, Koukounaras J, Royce PL, Corcoran NM. Assessing the usefulness of delayed imaging in routine followup for renal trauma. J Urol. 2010;184:973-977. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 28] [Article Influence: 1.8] [Reference Citation Analysis (0)] |