CASE REPORT
A 75-year-old female patient, with a past medical history of type II diabetes mellitus and hypertension, was admitted to our Medical Center’s Surgical Department with a right upper quadrant (RUQ) abdominal pain, which initially presented 1 wk before she visited our hospital and was accompanied with malaise and vomiting, without any associated fever or chills. The patient was slightly anxious but in no acute distress, with normal vital signs and body temperature. Physical findings included icteric scleras and RUQ abdominal tenderness in deep palpation, without neither rebound tenderness or abdominal muscle rigidity nor palpable masses. Laboratory tests demonstrated a normal white blood cell count and hematocrit, while liver function tests reported 8.00 mg/dL total bilirubin, 6.20 mg/dL direct bilirubin, 76 U/L serum glutamic oxaloacetic transaminase, 81 U/L serum glutamic pyruvate transaminase, 327 U/L γ-glutamyltransferase, and 264 U/L alcalic phosphatase.
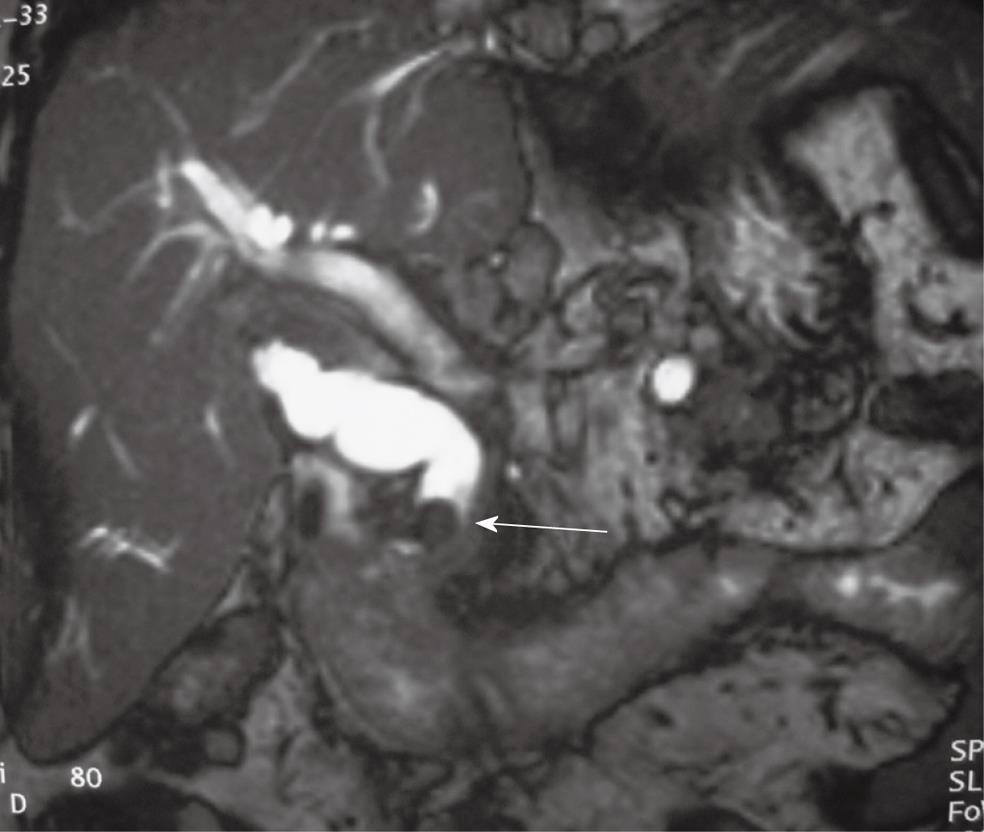
Abdominal ultrasound (US) and computer tomography (CT) showed a contracted gallbladder and stones in the CBD with an associated dilatation of the proximal biliary tree. Additionally, an abdominal magnetic resonance imaging (MRI) and retrograde cholangiopancreatography (MRCP) similarly demonstrated two stones in the CBD with a diameter of 2.2 cm and in the cystic duct, measuring 9 mm and 12 mm respectively, with dilatation of the proximal biliary tree (Figures 1 and 2).
Figure 1 Abdominal magnetic resonance imaging in a sagittal plane demonstrating two stones in common bile duct (arrow) with a diameter of 2.
2 cm and cystic duct, measuring 9 mm and 12 mm respectively, with dilatation of the proximal biliary tree.
Figure 2 Magnetic retrograde cholangio-pancreatography demonstrating stones in common bile duct and proximal dilatation of the biliary tree.
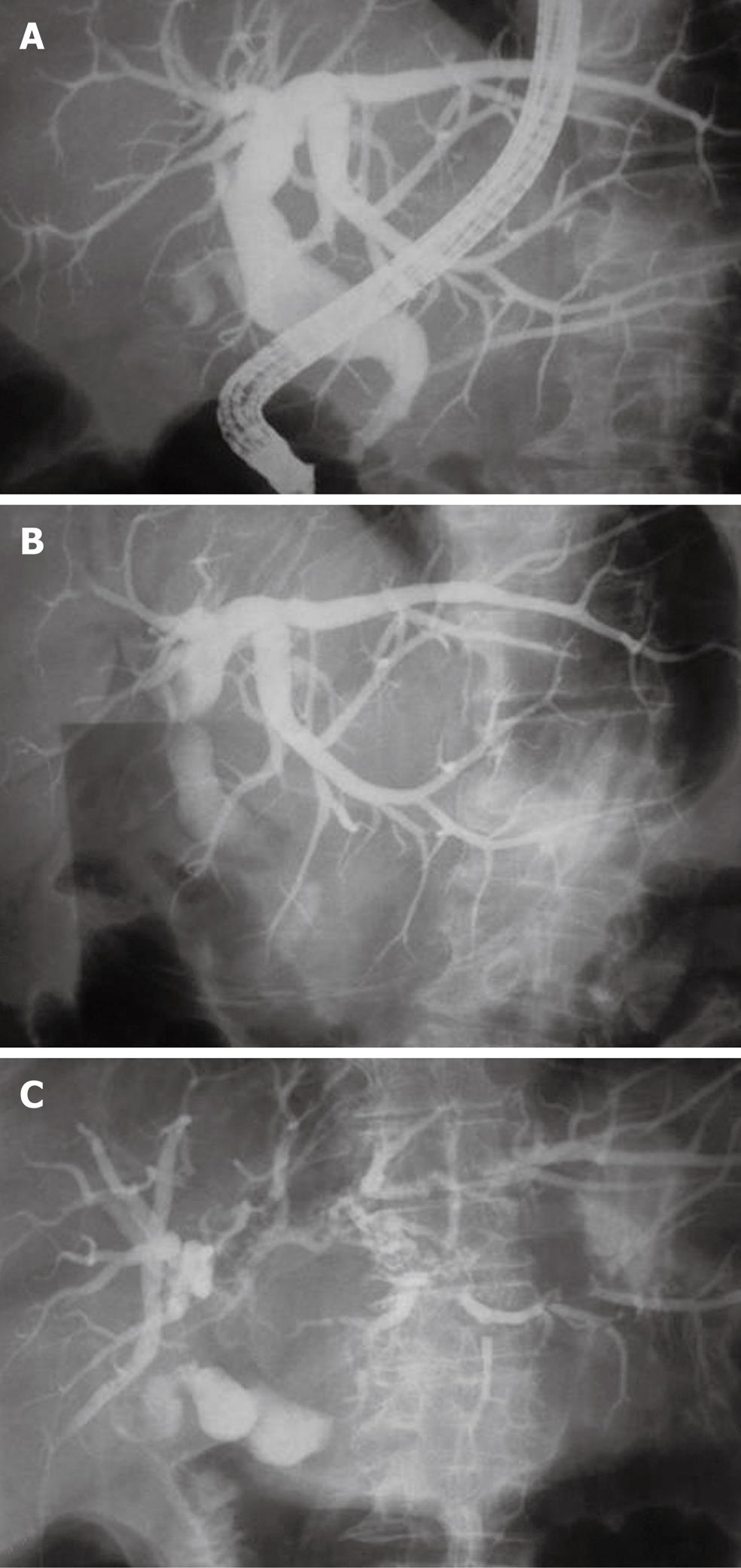
Endoscopic intervention was decided and a retrograde cholangiopancreatography (ERCP) was carried out. A balloon catheter was inserted in the dilated CBD through a wide sphincterectomy. However, several attempts to clean the CBD did not reveal any bile duct stones, and an impression of an external CBD pressed possibly by the cystic duct was demonstrated. Surprisingly, when the patient was placed in an anti-Trendelenburg position, the dilated biliary tree subsided and the diagnosis of a Mirizzi syndrome was considered more possible (Figure 3).
Figure 3 Endoscopic retrograde cholangio-pancreatography showing gradual resolve of dilated biliary tree (A) and indirect signs of Mirizzi syndrome (B and C) when the patient was placed in an anti-Trendelenburg position.
Surgical treatment was decided and an exploratory laparotomy was performed through a Kocher incision. Intraoperative findings included a contracted gallbladder that was adherently attached to the duodenum and CBD. During cholecystectomy, an impacted stone was found in the cystic duct which was firmly adhered to the CHD. After removal of the gallbladder, two defects were evident. One was on the lateral wall of the CHD involving less than 1/3 of the circumference, while the other was on the second portion of the duodenum. Both defects of the duodenum and CHD were sutured in one layer fashion. A choledochotomy was performed, the CHD was lavaged and finally a Kehr tube was inserted. The final diagnosis was a double cholecysto-choledochal and cholecysto-duodenal fistula. The patient had an uneventful postoperative course and was discharged on the 14th postoperative day.
DISCUSSION
Mirizzi syndrome is attributed to Pablo Mirizzi who was the first to describe it as a benign condition during which a stone in the cystic duct or in the Hartmann’s pouch impinges on the CBD, leading to mechanical obstruction by the stone itself or by secondary inflammation[1]. He termed this phenomenon as “functional hepatic syndrome”. In 1985, McSherry et al[2] classified Mirizzi syndrome into two types based on ERCP findings: type I Mirizzi syndrome when there is extrinsic compression of the common hepatic duct and type II Mirizzi syndrome when the gallstone erodes the common hepatic duct wall, resulting in a cholecystocholedochal fistula. In 1989, Csendes et al[3] proposed a new classification in order to clarify the definition of cholecystobiliary fistulae and to further establish an appropriate surgical treatment according to the underlying pathology. Thus, he defined the following four categories: type I: external compression of the CBD due to a stone impacted at the neck of the gallbladder or at the cystic duct (62.5%), type II: presence of a cholecystobiliary fistula (cholecystohepatic or cholecystocholedochal) due to erosion of the anterior or lateral wall of the CHD or CBD, respectively, with the fistula involving less than one-third of the circumference of the CBD (12.5%), type III: presence of a cholecystobiliary fistula with erosion of the wall of the CBD involving up to two-thirds of its circumference (12.5%), and type IV: presence of a cholecystobiliary fistula with complete destruction of the entire wall of the CBD (12.5%). In 2008, Beltran et al[4] suggested that Mirizzi syndrome may not just end with a cholecystobiliary fistula but may further complicate the clinical picture with a superimposed cholecystoenteric fistula. Thus, a modified classification was proposed as follows: any aforementioned type plus a cholecystoenteric fistula without gallstone ileus (type Va), or with gallstone ileus (type Vb). Our patient had both a cholecysto-biliary fistula and a cholecysto-enteric fistula, without any gallstone ileus. Therefore, the patient had a Mirizzi syndrome type Va, according to the latest classification.
This syndrome is a very rare cause of obstructive jaundice and occurs in 0.7%-1.4% of patients with gallstones[3-6]. It is very difficult to establish a preoperative diagnosis of intermittent jaundice, as there is no specific clinical or laboratory presentation for this syndrome. However, jaundice, abdominal pain and alternating hepatic biochemical profile can suggest Mirizzi syndrome in 80% of the cases. Ultrasonography and abdominal CT disclose a dilated CBD above the gallbladder neck, an abrupt disruption of the CHD and a decompressed gallbladder with stones[7]. Furthermore, laparoscopic US and CT scanning may rule out a tumor mass[8,9]. MRCP and MRI are the useful methods for the diagnosis of Mirizzi syndrome as they can precisely demonstrate the presence and degree of dilatated biliary tree, and can also reveal extrinsic narrowing of the CHD as well as anatomical variations and malformations[10].
ERCP remains the gold standard for preoperative diagnosis of Mirizzi syndrome in jaundiced patients, although it cannot often document the presence of a fistula. ERCP provides indirect signs such as lateral filling gap of the CHD, central dilatation of the biliary tree and insertion of the cystic duct at the point of obstruction and/or complete obliteration of the cystic duct[11]. In our case, an interesting finding during ERCP suggesting indirectly Mirizzi syndrome, was the fact that biliary tree dilatation subsided when the patient was placed in an anti-Trendelenburg position. To our knowledge, such an indirect sign has never been reported in the English literature. Preoperative diagnosis of Mirizzi syndrome by ERCP is important to prevent complications[12]. At last, a recent study demonstrated that MRCP as a noninvasive alternative to ERCP is a useful preoperative diagnostic modality for Mirizzi syndrome when combined with CT, with a higher accuracy and better inter-observer agreement compared with CT alone[13].
Management of patients with Mirizzi syndrome is a real challenge, especially if a fistula is present. Several minimal invasive techniques have been proposed. Percutaneous treatment with electrohydraulic lithotripsy under cholangioscopic control with a mother-daughter endoscope system has been reported to successfully fragment and clear all stones in 38 cases[14]. These advanced endoscopic approaches cannot be applied to all hospital settings but they are definite treatment modalities that might prove helpful in the future. Moreover, the impacted stone cannot be extracted endoscopically and therefore surgery is the only chance for cure. Although successful attempts of laparoscopic treatment have been reported, conversion to laparotomy is most commonly required with an overall conversion rate of 31.7%-100%[15,16]. Thus, several open surgical procedures are described for the treatment of different types of Mirizzi syndrome. Surgical strategy, however, should be based on three basic principles: removal of the obstructing stone and gallbladder, restoration of the integrity of biliary tree and in case of type V, closure of the gastrointestinal tract defect.
More specifically, the usual surgical treatment of type I Mirizzi syndrome is laparoscopic or open cholecystectomy and exploration of the CBD. In case of type II Mirizzi’s syndrome, most studies favor open techniques, although Binnie et al[17] reported successful laparoscopic treatment of type II Mirizzi’s syndrome after previous endoscopic biliary stenting. Choledochoplasty with gallbladder flap, cholecystoduodenostomy and Roux-en-Y hepaticojejunostomy are the possible surgical approaches to the treatment of type II Mirizzi’s syndrome[10]. Additionally, partial cholecystectomy with primary closure using the gallbladder remnant and T-tube insertion though the fistula opening are options for the treatment of type II Mirizzi syndrome[18,19]. However, T-tube insertion into the CBD rather than the fistula opening reduces the risk of stenosis[20,21]. Roux-en-Y hepaticojejunostomy is recommended as a safe approach in cases of wider CBD defects (types III and IV) in order to avoid complications such as biliary leakage and stricture formation[3,9,18,20]. Finally, a surgeon must be aware that Mirizzi syndrome coexists with cancer in 27% of the cases[22], as it requires a totally different approach.
The co-existence of double cholecysto-biliary and cholecysto-enteric fistulae is rare. Mirizzi syndrome should be highly suspected in cases of unexplained intermittent obstructive jaundice. Several imaging modalities for the diagnosis of Mirizzi syndrome exist and have been proved useful preoperatively. Treatment of Mirizzi syndrome is considered challenging and determined by the type of Mirizzi syndrome.