Published online Oct 28, 2010. doi: 10.4329/wjr.v2.i10.399
Revised: August 23, 2010
Accepted: August 30, 2010
Published online: October 28, 2010
AIM: To assess radiologists reporting rates of incidental vertebral compression fractures in imaging studies.
METHODS: We performed a review of the current literature on the prevalence and reporting rates of incidental vertebral compression fractures in radiologic examinations.
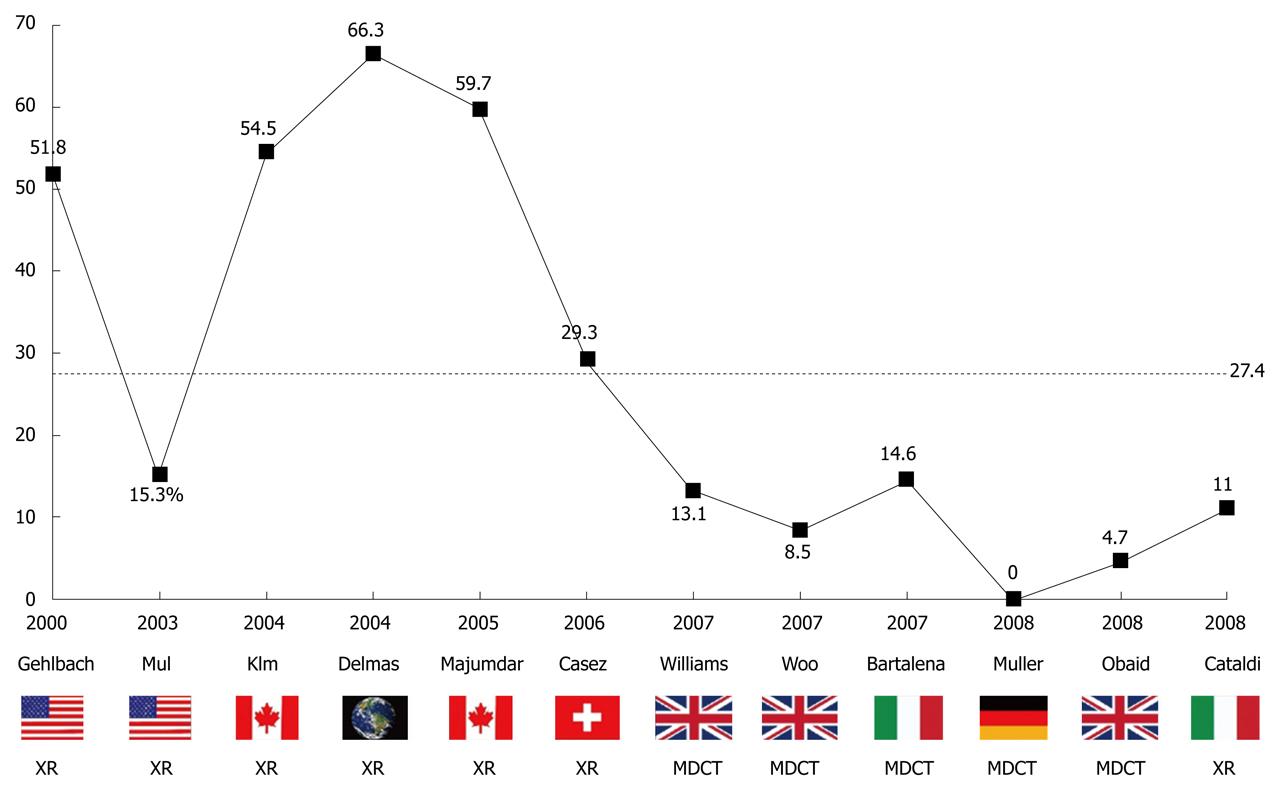
RESULTS: The bibliographic search revealed 12 studies: 7 studies using conventional radiology and 5 using multidetector computed tomography (MDCT). The loss of height cut-off to define a vertebral fracture varied from 15% to 25%. Fracture prevalence was high (mean 21.1%; range 9.5%-35%) in both radiographic and MDCT studies (mean 21.6% and 20.2%, respectively). Reporting rates were low with a mean value of 27.4% (range 0%-66.3%) and were significantly lower in MDCT than in radiographic studies (mean 8.1% vs 41.1%). Notably, recent studies showed lower reporting rates than older studies.
CONCLUSION: Many scientific studies have confirmed a high prevalence of vertebral compression fractures as incidental findings on imaging studies. However, the underreporting of these fractures, as determined in our study, may negatively affect patient care.
- Citation: Bartalena T, Rinaldi MF, Modolon C, Braccaioli L, Sverzellati N, Rossi G, Rimondi E, Busacca M, Albisinni U, Resnick D. Incidental vertebral compression fractures in imaging studies: Lessons not learned by radiologists. World J Radiol 2010; 2(10): 399-404
- URL: https://www.wjgnet.com/1949-8470/full/v2/i10/399.htm
- DOI: https://dx.doi.org/10.4329/wjr.v2.i10.399
Osteoporosis is a chronic progressive disease leading to decreased bone mass and skeletal fragility, which predisposes individuals to fractures. Vertebral fractures are the most common osteoporotic fractures, affecting 20% of postmenopausal women[1].
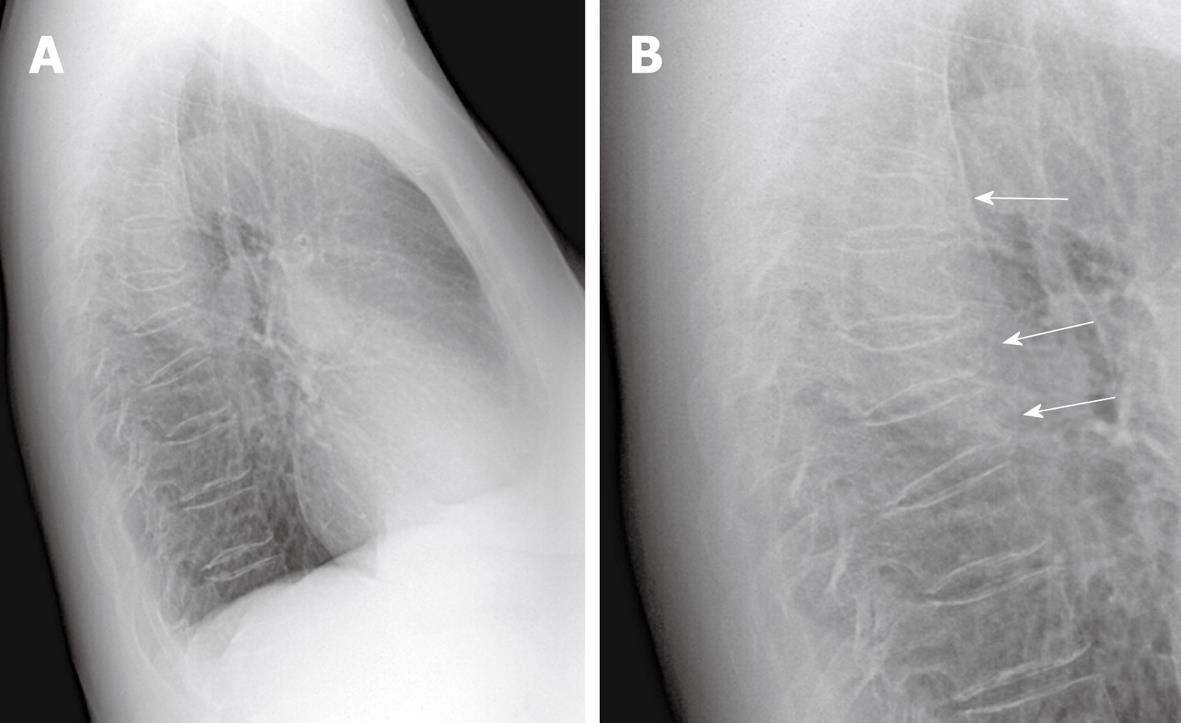
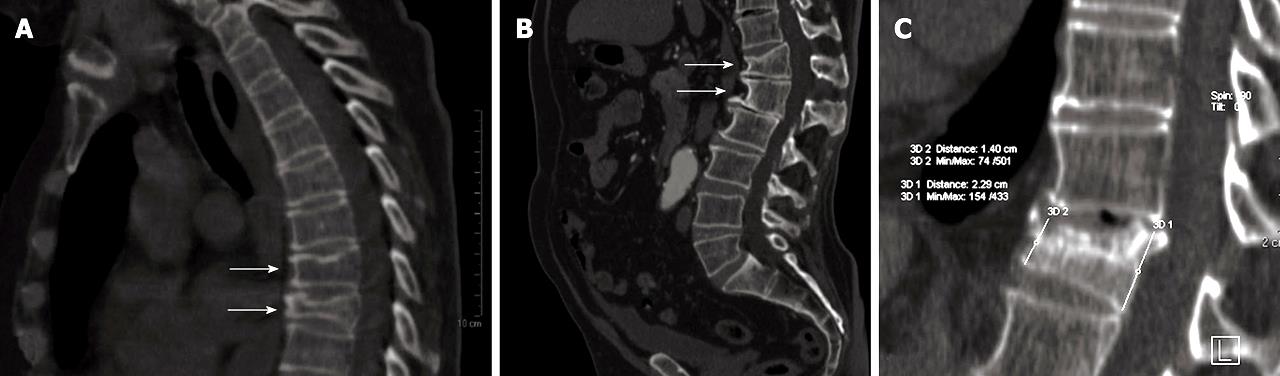
Most of these fractures are undiscovered and not recognized by physicians. It has been estimated that 66% of patients with osteoporotic vertebral fractures are asymptomatic[2], and symptoms, when present, may have a misleading location[3]. As a consequence, patients may ignore their condition and fail to seek therapy to reduce bone density loss and possible subsequent serious fractures[4]. However, imaging studies performed for various clinical indications may disclose spinal fractures leading to incidental recognition and diagnosis of this problem (Figures 1 and 2).
Thereby, radiologists may play a pivotal role in obtaining an earlier diagnosis of osteoporosis and related asymptomatic fractures[5].
A literature review of studies dealing with the prevalence of incidental vertebral compression fractures in imaging studies and their reporting rates was performed.
Multiple queries, including terms such as “vertebral fractures”, “osteoporotic” and “incidental” were performed in PubMed. Eligible studies were assessed and reviewed and their references were also analyzed for additional similar papers. The type of imaging modality used and the anatomical region studied were noted along with demographic data of the patients (sex and age). The morphometric criteria and cut-off to define a vertebral fracture were noted. Finally, prevalence and reporting rates of vertebral fractures were analyzed.
Twelve studies published from 2000 to date were identified and reviewed[6-17].
The imaging modality was radiography in 7 (58.3%) studies and multidetector CT (MDCT) in the remaining 5 (41.7%) studies. The anatomical region of interest of the radiologic and MDCT examinations included chest, spinal column and abdomen. Four studies included only women while other studies focused on particular age groups of patients (Table 1).
| Scientific study | Patients demographics | Vertebral fractures (%) | |||||||||
| Year and author1 | Imaging modality | Anatomical region | Total(n) | Sex (%) | Age (yr) | Method of assessment | Morphometric cut-off | Fractures prevalence | Reporting rate | ||
| Male | Female | Range | mean | ||||||||
| 2000-Gehlbach | X-Rays | Chest | 934 | 0.0 | 100 | 60-97 | 75.9 | SQM | 25 | 14.1 | 51.8 |
| 2003-Mui | X-Rays | Chest | 106 | 0.0 | 100 | 55-89 | 65.0 | SQM | 25 | 24.5 | 15.3 |
| 2004-Kim | X-Rays | Chest | 100 | 53.0 | 47 | > 60 | 75.2 | SQM | 25 | 22.0 | 54.5 |
| 2004-Delmas | X-Rays | Spine | 2451 | 0.0 | 100 | 65-80 | 71.3 | SQM and QM | 20 | 32.1 | 66.3 |
| 2005-Majumdar | X-Rays | Chest | 459 | 52.3 | 47.7 | > 60 | 75.2 | SQM | 25 | 15.6 | 59.7 |
| 2006-Casez | X-Rays | Chest or Spine | 464 | 54.0 | 46 | 60-97 | 75.9 | SQM | 20 | 30.8 | 29.3 |
| 2007-Williams | MDCT | Chest | 192 | 50.5 | 49.5 | 55-93 | 70.1 | SQM | 25 | 19.7 | 13.1 |
| 2007-Woo | MDCT | Chest | 200 | 52.0 | 48 | 18-92 | 61.0 | SQM | 20 | 35.0 | 8.5 |
| 2007-Bartalena | MDCT | Chest and/or Abdomen | 323 | 60.7 | 39.3 | 20-88 | 62.6 | Mixed | 15 | 9.5 | 14.6 |
| 2008-Muller | MDCT | Chest and/or Abdomen | 112 | 0.0 | 100 | 55-87 | 67.4 | SQM | 20 | 24.1 | 0.0 |
| 2008-Obaid | MDCT | Abdomen | 307 | 51.5 | 48.5 | 18-90 | 65.0 | SQM | 20 | 13.6 | 4.7 |
| 2008-Cataldi | X-Rays | Chest | 145 | 50.3 | 49.7 | 50-86 | 67.5 | SQM | 25 | 12.4 | 11.0 |
The definition criteria of an osteoporotic vertebral fracture varied among studies. According to Kleerekoper criteria, a vertebral body is considered fractured when at least one of its 3 heights is reduced by 15%[18]. Genant set the height loss cut-off at 20% and the degree of deformity was graded as mild (20%-24%), moderate (25%-39%) or severe (more than 40%)[19]. Furthermore, some of the studies using Genant’s criteria considered only moderate grade (> 25%) deformities and decided to overlook mild grade fractures. The method of assessing vertebral fractures varied from vertebral morphometry using the 6 point technique described by Hurxthal[20], to Genant’s semiquantitative visual grading, to a combined method by means of preliminary visual grading followed by focused morphometry on vertebral bodies with apparently abnormal heights[14].
Despite the above mentioned differences in demographics, imaging modality, morphometric criteria and assessment methods, the prevalence of incidental vertebral fractures on imaging studies was quite high, ranging from 9.5% to 35% (mean 21.1%). Furthermore, the true prevalence is likely higher because some studies did not take into account mild grade fractures.
Intriguingly, there are no significant differences in fracture prevalence between radiographic and MDCT case series, with a fracture rate of 21.6% and 20.2%, respectively. On the other hand, reporting rates in MDCT studies were constantly lower than those using conventional radiology (8.1% vs 41.1%).
Recognition of these incidental findings by radiologists has proved to be low with a mean reporting rate of just 27.4% with only 4 studies reporting a rate over 50% and a high score of 66.3%. Notably, we observed that reporting rates of recent studies were lower than those of older investigations (Figure 3).
The studies reviewed in this paper were derived from different countries showing that underreporting of vertebral fractures is a worldwide problem. Single center studies from North America had better reporting rates than those from Europe, with a highest reporting rate of 29.3%. Conversely, in a study by Delmas[9], which was the only multicentric study on this issue, geographical differences were encountered but showed higher rates of false-negative fractures in the Americas compared with other regions (Europe/South Africa/Australia). Our results showed that radiologists had a lower reporting rate with MDCT in comparison with conventional radiology. This is an apparent paradox because CT may better analyze and visualize vertebral bodies with sagittal multiplanar reconstructions (MPRs)[21] while evaluation of the spine on lateral plain films may be impaired by inadequate positioning, scoliosis, suboptimal exposure of the radiograph and superimposition of other structures, such as shoulder girdles and diaphragmatic domes. All these limitations may be easily overcome with the use of adequately oriented multiplanar reformations on MDCT. A possible explanation is that images in MDCT studies are natively acquired in the axial plane and, in many instances, the interpreting radiologists did not perform any sagittal reformation despite the availability of a thin collimation dataset. This results in lack of sensitivity since axial images are suboptimal in the assessment of vertebral heights and even careful review of the axial images by an expert musculoskeletal radiologist results in identification of just 35% of fractures[12].
We therefore suggest reconstruction and review of at least one sagittal midline MPR of the spine in every MDCT study. We think that, in the era of MDCT, radiologists should use all planes to confirm findings met in a particular plane for any body part examined.
There are some instances in which sagittal MPRs are already routinely performed, especially in CT angiographic studies of the aorta. Underreporting of vertebral fractures in these cases cannot be explained by an inadequate visualization plane. Radiologists probably underrate the clinical importance of these findings since recognition of vertebral fractures on lateral radiographs or in MDCT sagittal reformatted images is usually not a difficult task.
In a study by Williams, a novice observer (medical student) correctly identified 21 of 22 patients with fractures, with a sensitivity of 0.95 and a specificity of 0.85[12].
Moreover in another study, general internists exposed to a brief teaching program on vertebral fractures recognized more fractures than radiologists, who tended to overlook those findings[11].
A higher level of expertise is probably required only in the identification of mild grade fractures and in the differential diagnosis between osteoporotic vertebral fracture and non-osteoporotic deformities, such as Cupid’s bow, Scheuermann disease and degenerative wedging[22].
We suspect that some radiologists do not routinely perform an accurate analysis of bony structures while reading chest radiographs and do not review MDCT studies using a specific bone window level. Another possible explanation is that some radiologists tend to focus their report only on the clinical indication of the exam.
Underreporting has been noted also in spinal radiographs in which images are collimated to the spine and attention is focused on the vertebral bodies[9]. In these cases, the chronic appearance of osteoporotic deformities may be considered as unimportant.
The steady increase in the workload of radiologists could, in some way, explain this tendency towards low reporting rates, since busy radiologists tend to pass over incidental findings during dictation in order to save time. Vertebral morphometry with the 6 point technique is a time consuming method and cannot feasibly be applied to routine reporting of chest radiographs or MDCT studies. However, semiquantitative visual grading methods could represent a good balance between speed and accuracy, allowing recognition of the majority of fractures of moderate and severe degree in a limited time.
Speech recognition computer systems may also afford a solution since the software used allows recording and reproduction of templates for entire reports or specific sentences that may be triggered by means of a hotkey or speech macro, considerably shortening the dictation time. A line regarding presence or absence of vertebral deformities could be easily added to radiological reports with this method. Regarding this specific point, we have noticed that in the vast majority of the institutions of our country, no specific remarks about the vertebral column are usually present in standard reports for chest radiographs or MDCT studies. This may contribute to the tendency of overlooking spinal findings.
Another issue is inconsistency of terminology used to report these findings. In the IMPACT study, a consistent portion of false negatives (27%) was due to ambiguous terms used in the radiologic reports[9]. Radiologists should learn how to communicate findings consistently and to use language that is understandable by referring physicians, avoiding equivocal sentences, since ineffective communication of an identified finding has the same effect as a missed diagnosis. It is likely that the main reason for ignoring incidental fractures in imaging studies is lack of awareness by radiologists of their clinical implications.
The presence of vertebral fractures may lead to neurological symptoms in the case of retropulsed bony fragments narrowing the spinal canal[23]. Moreover, even if asymptomatic, spinal compression fractures represents a negative prognostic factor for osteoporotic patients and increases their likelihood of subsequent fracturing events, including femoral neck fracture[4].
This leads to a decline of the quality of life of these patients together with an increased risk of mortality[24,25]. All these data and the availability of pharmacological therapies that may reduce either bone mass loss or the incidence of fracturing events[26], should underscore the importance of early, consistent incidental, recognition and diagnosis.
Unfortunately, patients with correctly diagnosed compression fractures do not always receive therapeutic intervention, showing that underrating of osteoporosis does not just affect radiologists but may occur among orthopedic surgeons, emergency room physicians and primary care providers[27].
The incidence of osteoporosis and its complications are likely to represent an important health-care concern because of the expected increase in the median age of the population in the years to come. To give an idea of the proportion and the costs of this disease, we cite a study by Lippuner who showed that the cumulative number of days of hospitalization related to osteoporosis over one year in Switzerland was equal to the number of hospital days due to chronic obstructive pulmonary disease and heart failure combined[28].
Moreover, osteoporosis does not just affect elderly women but is also emerging as a common complication in patients with chronic lung diseases[29], prolonged steroid therapy[30], organ transplantation[31] and HIV infection[32], which clearly represents categories of patients who often undergo imaging studies during their clinical course.
Osteoporotic vertebral fractures are frequent incidental findings in imaging studies and have been underrated and unreported by radiologists. Even worse, reporting rates of radiologists do not seem to improve, as shown by the negative trend despite many considerations in the literature. Radiologists should understand the clinical relevance of osteoporosis. Accurate review of the spine on lateral radiographs and sagittal MDCT reconstructions is recommended, as is the inclusion of a comment regarding the presence or absence of vertebral fractures at the end of any radiological report.
Vertebral fractures are a hallmark of osteoporosis but may be clinically silent for a long time. These findings may, however, be incidentally visualized on imaging studies performed for other clinical indications. Identification of this finding may lead to an earlier diagnosis of the disease and bring it to clinical attention.
This is the first review about underreporting incidental vertebral fractures on imaging studies. It analyzes 12 different papers written in the last 10 years in different countries of the world on this topic. Patient demographics, fractures prevalence and reporting rates on different imaging modalities are compared.
The current review disclosed an unchanged and even apparently worsening tendency of radiologists to overlook incidental spinal column findings in their medical reports, especially in multidetector computed tomography studies. The review discusses the reasons for this common behavior among radiologists throughout the world.
Remark on the need for better understanding of the clinical importance of osteoporosis among radiologists and suggest ways to revert the underreporting tendency.
The authors reviewed relevant ex-literature (between years 2000-2010) discussing the topic of reporting spinal osteoporotic fracture on a variety of radiographic examinations by reporting radiologists. Underreporting is a known fact, and has been discussed in the last 10 years, but the situation has not improved according to the authors’ statements. In this respect, it is a worthwhile review paper.
| 1. | Eastell R, Cedel SL, Wahner HW, Riggs BL, Melton LJ 3rd. Classification of vertebral fractures. J Bone Miner Res. 1991;6:207-215. |
| 2. | Ross PD. Clinical consequences of vertebral fractures. Am J Med. 1997;103:30S-42S; discussion 42S-43S. |
| 3. | Friedrich M, Gittler G, Pieler-Bruha E. Misleading history of pain location in 51 patients with osteoporotic vertebral fractures. Eur Spine J. 2006;15:1797-1800. |
| 4. | Melton LJ 3rd, Atkinson EJ, Cooper C, O'Fallon WM, Riggs BL. Vertebral fractures predict subsequent fractures. Osteoporos Int. 1999;10:214-221. |
| 5. | Link TM, Adams JE. The radiologist's important roles and responsibilities in osteoporosis. Eur J Radiol. 2009;71:385-387. |
| 6. | Gehlbach SH, Bigelow C, Heimisdottir M, May S, Walker M, Kirkwood JR. Recognition of vertebral fracture in a clinical setting. Osteoporos Int. 2000;11:577-582. |
| 7. | Mui LW, Haramati LB, Alterman DD, Haramati N, Zelefsky MN, Hamerman D. Evaluation of vertebral fractures on lateral chest radiographs of inner-city postmenopausal women. Calcif Tissue Int. 2003;73:550-554. |
| 8. | Kim N, Rowe BH, Raymond G, Jen H, Colman I, Jackson SA, Siminoski KG, Chahal AM, Folk D, Majumdar SR. Underreporting of vertebral fractures on routine chest radiography. AJR Am J Roentgenol. 2004;182:297-300. |
| 9. | Delmas PD, van de Langerijt L, Watts NB, Eastell R, Genant H, Grauer A, Cahall DL. Underdiagnosis of vertebral fractures is a worldwide problem: the IMPACT study. J Bone Miner Res. 2005;20:557-563. |
| 10. | Majumdar SR, Kim N, Colman I, Chahal AM, Raymond G, Jen H, Siminoski KG, Hanley DA, Rowe BH. Incidental vertebral fractures discovered with chest radiography in the emergency department: prevalence, recognition, and osteoporosis management in a cohort of elderly patients. Arch Intern Med. 2005;165:905-909. |
| 11. | Casez P, Uebelhart B, Gaspoz JM, Ferrari S, Louis-Simonet M, Rizzoli R. Targeted education improves the very low recognition of vertebral fractures and osteoporosis management by general internists. Osteoporos Int. 2006;17:965-970. |
| 12. | Williams AL, Al-Busaidi A, Sparrow PJ, Adams JE, Whitehouse RW. Under-reporting of osteoporotic vertebral fractures on computed tomography. Eur J Radiol. 2009;69:179-183. |
| 13. | Woo EK, Mansoubi H, Alyas F. Incidental vertebral fractures on multidetector CT images of the chest: prevalence and recognition. Clin Radiol. 2008;63:160-164. |
| 14. | Bartalena T, Giannelli G, Rinaldi MF, Rimondi E, Rinaldi G, Sverzellati N, Gavelli G. Prevalence of thoracolumbar vertebral fractures on multidetector CT: underreporting by radiologists. Eur J Radiol. 2009;69:555-559. |
| 15. | Müller D, Bauer JS, Zeile M, Rummeny EJ, Link TM. Significance of sagittal reformations in routine thoracic and abdominal multislice CT studies for detecting osteoporotic fractures and other spine abnormalities. Eur Radiol. 2008;18:1696-1702. |
| 16. | Obaid H, Husamaldin Z, Bhatt R. Underdiagnosis of vertebral collapse on routine multidetector computed tomography scan of the abdomen. Acta Radiol. 2008;49:795-800. |
| 17. | Cataldi V, Laporta T, Sverzellati N, De Filippo M, Zompatori M. Detection of incidental vertebral fractures on routine lateral chest radiographs. Radiol Med. 2008;113:968-977. |
| 18. | Olmez N, Kaya T, Gunaydin R, Vidinli BD, Erdogan N, Memis A. Intra- and interobserver variability of Kleerekoper’s method in vertebral fracture assessment. Clin Rheumatol. 2005;24:215-218. |
| 19. | Genant HK, Wu CY, van Kuijk C, Nevitt MC. Vertebral fracture assessment using a semiquantitative technique. J Bone Miner Res. 1993;8:1137-1148. |
| 20. | Hurxthal LM. Measurement of anterior vertebral compressions and biconcave vertebrae. Am J Roentgenol Radium Ther Nucl Med. 1968;103:635-644. |
| 21. | Bauer JS, Müller D, Ambekar A, Dobritz M, Matsuura M, Eckstein F, Rummeny EJ, Link TM. Detection of osteoporotic vertebral fractures using multidetector CT. Osteoporos Int. 2006;17:608-615. |
| 22. | Abdel-Hamid Osman A, Bassiouni H, Koutri R, Nijs J, Geusens P, Dequeker J. Aging of the thoracic spine: distinction between wedging in osteoarthritis and fracture in osteoporosis--a cross-sectional and longitudinal study. Bone. 1994;15:437-442. |
| 23. | Kaplan PA, Orton DF, Asleson RJ. Osteoporosis with vertebral compression fractures, retropulsed fragments, and neurologic compromise. Radiology. 1987;165:533-535. |
| 24. | Adachi JD, Ioannidis G, Olszynski WP, Brown JP, Hanley DA, Sebaldt RJ, Petrie A, Tenenhouse A, Stephenson GF, Papaioannou A. The impact of incident vertebral and non-vertebral fractures on health related quality of life in postmenopausal women. BMC Musculoskelet Disord. 2002;3:11. |
| 25. | Kado DM, Duong T, Stone KL, Ensrud KE, Nevitt MC, Greendale GA, Cummings SR. Incident vertebral fractures and mortality in older women: a prospective study. Osteoporos Int. 2003;14:589-594. |
| 26. | Silverman SL, Christiansen C, Genant HK, Vukicevic S, Zanchetta JR, de Villiers TJ, Constantine GD, Chines AA. Efficacy of bazedoxifene in reducing new vertebral fracture risk in postmenopausal women with osteoporosis: results from a 3-year, randomized, placebo-, and active-controlled clinical trial. J Bone Miner Res. 2008;23:1923-1934. |
| 27. | Freedman BA, Potter BK, Nesti LJ, Giuliani JR, Hampton C, Kuklo TR. Osteoporosis and vertebral compression fractures-continued missed opportunities. Spine J. 2008;8:756-762. |
| 28. | Lippuner K, Golder M, Greiner R. Epidemiology and direct medical costs of osteoporotic fractures in men and women in Switzerland. Osteoporos Int. 2005;16 Suppl 2:S8-S17. |
| 29. | Caplan-Shaw CE, Arcasoy SM, Shane E, Lederer DJ, Wilt JS, O'Shea MK, Addesso V, Sonett JR, Kawut SM. Osteoporosis in diffuse parenchymal lung disease. Chest. 2006;129:140-146. |
| 30. | Iqbal F, Michaelson J, Thaler L, Rubin J, Roman J, Nanes MS. Declining bone mass in men with chronic pulmonary disease: contribution of glucocorticoid treatment, body mass index, and gonadal function. Chest. 1999;116:1616-1624. |
| 31. | Stein E, Ebeling P, Shane E. Post-transplantation osteoporosis. Endocrinol Metab Clin North Am. 2007;36:937-963; viii. |
| 32. | Tampellini L, Biagetti C, D'Aquino P, Borderi M, Chiodo F. HIV-HAART and Bone metabolism: prevalence of the osteopenia and osteoporosis among the HIV population. HAART Corr Pathol. 2008;N°0:9-12. |
Peer reviewers: Shigeru Ehara, MD, Professor and Chair, Iwate Medical University School of Medicine, Morioka 020-8505, Japan; Mohamed Ragab Nouh, MD, Radiodiagnosis Department, Faculty of medicine, Alexandria University, 1 Kolya El-Teb Streeet, Mohata El-Raml, Alexandria, 21521, Egypt; Sudsriluk Sampatchalit, MD, Lieutenant Colonel, Radiology, Phramongutglao Royal Thai Army Hospital, 315 Ratchawithi Road, Ratchathewi, Bangkok 10400, Thailand
S- Editor Cheng JX L- Editor Lutze M E- Editor Ma WH