Published online Jul 28, 2025. doi: 10.4329/wjr.v17.i7.107486
Revised: April 19, 2025
Accepted: June 26, 2025
Published online: July 28, 2025
Processing time: 123 Days and 0.2 Hours
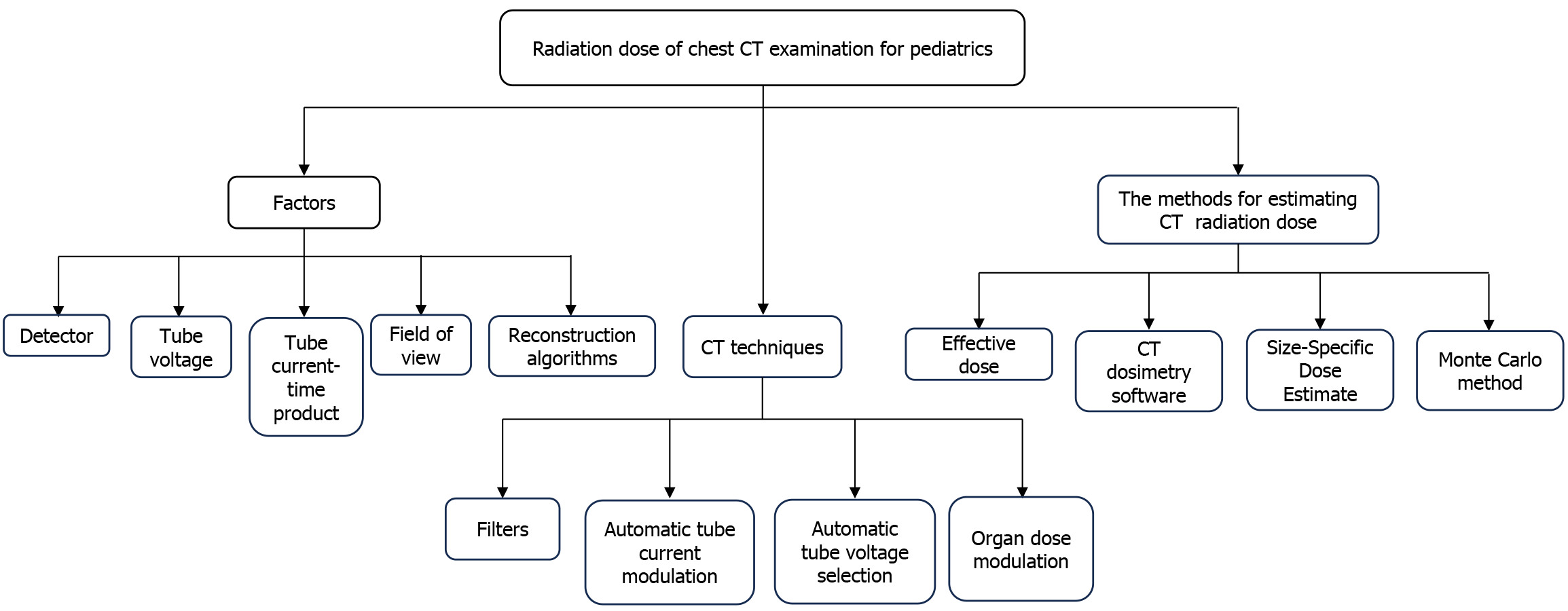
With the rapid development of computed tomography (CT) technology, the widespread use of CT examinations in the evaluation of chest diseases in pediatrics has raised extensive concerns about radiation issues. This review first systematically summarizes the factors influencing radiation dose (detector, tube voltage, tube current-time product, field of view, and reconstruction algorithms) in pediatric chest computed tomography examinations. Methods to reduce radia
Core Tip: Chest computed tomography (CT) is a common examination for diagnosing diseases in pediatrics, providing accurate clinical evidence, but is also a source of radiation exposure. In terms of optimizing dose, the selection of CT scan parameters is challenging and relies upon individual characteristics. This review summarizes multiple factors affecting CT radiation dose (detector, tube voltage, tube current-time product, field of view, and reconstruction algorithms), and introduces CT technologies that reduce radiation dose. Methods for dose calculation, including effective dose, CT dosimetry software, size-specific dose estimate, and the Monte Carlo method are also discussed.
- Citation: Sun QT, Fan YH, Liang BH. Advances in radiation protection related to pediatric chest computed tomography examinations. World J Radiol 2025; 17(7): 107486
- URL: https://www.wjgnet.com/1949-8470/full/v17/i7/107486.htm
- DOI: https://dx.doi.org/10.4329/wjr.v17.i7.107486
Computed tomography (CT) has the advantages of immediacy, accuracy and efficiency, and in terms of pediatric chest examinations, CT can be used for various local or systemic diseases, such as the evaluation of mediastinal masses and the diagnosis of diffuse lung diseases. Therefore, pediatric CT examinations have significantly increased in most countries[1-5]. Between 1996 and 2005, the usage rate of CT doubled in children under 5 years old and tripled in those aged 5 to 14 years. In 2011, pediatrics accounted for 5% to 11% of the 85 million CT examinations in the United States. Furthermore, there was a 50% increase in chest CT examinations in pediatrics from 1996 to 2010[6]. Factually, the ionizing radiation dose from CT scans is 100 to 500 times higher than that of conventional radiography[7,8], and the radiation dose is positively related to the risk of cancer[2,7]. It should be noted that pediatrics are more sensitive to radiation-induced carcinogenesis and have sufficient time to express these effects compared with adults[9]. Therefore, it is necessary to provide an individualized scan protocol and assess radiation risk in radiological examinations. According to the principle of "as low as reasonably possible"[10], many researchers hope to find the balance point between radiation dose and image quality[11]. This review aims to comprehensively describe the effects of different parameters on radiation dose and the optimization techniques in CT scanning, as well as the applications of personalized dose estimation methods (Figure 1).
Clinical CT commonly uses energy-integrating detectors (EIDs), where X-rays are absorbed and converted into visible light in the upper layer of the detector (scintillator). The photodiode measures the amount of incident light and generates electrical signals. However, the EID measures and integrates the total energy deposited during the measurement interval, such as electronic noise, which significantly reduces image quality, especially during low-dose imaging[12]. Currently, photon-counting detector CT (PCD-CT) is an emerging technology whose mechanism differs from EID-CT. PCD-CT directly converts individual X-ray photons into electrical signals without the additional step of converting photons into visible light. Thus, PCD-CT can count individual X-ray photons and measure the energy of photons[12]. Compared with conventional EID-CT, the image noise level of PCD-CT is lower under the same X-ray exposure level, as PCD-CT minimizes electronic noise and achieves the optimal X-ray photon energy weighting, which can reduce radiation dose by about 30%-60%[12,13], and in vivo human studies have demonstrated that the dose decrease can reach up to 34% for chest PCD-CT examinations[14]. Therefore, low-dose examinations in pediatric chest CT can be achieved by using PCD-CT[12,15,16].
In pediatric chest CT scans, tube voltage is one of the key variables affecting radiation dose. Increasing the tube voltage will enhance the mean energy of X-ray photons, thereby increasing the radiation dose[17,18]. Therefore, it is necessary to reasonably choose a lower tube voltage (< 120 kV) according to the attenuation of X-rays for pediatric patients while ensuring image quality[17,19]. Studies[20] have found that decreasing the tube voltage from 120 kV to 100 kV, and then to 80 kV, reduces radiation dose by 33% and 65%, respectively. It is noteworthy that the contrast improvement obtained by reducing the tube voltage for lesion detection may be offset by increased image noise[21]. Based on the study of phantom (Catphan®), Klink et al[22] proved that by lowering the tube voltage from 120 kV to 80 kV without altering other scanning parameters, the noise of the CT image increased by approximately 64%. Therefore, the reduction in kV must be paired with a moderate increase in the product of tube current and exposure time. Although the increased mAs compensate for the decreased photon flux, low tube voltage scanning can still reduce the radiation dose on most children's CT scans[17]. The optimization of tube voltage should be done according to patient size, with small infants generally scanned at 80 kV, while larger pediatrics require 100 to 120 kV[23]. Additionally, clinical indications need to be considered in tube voltage selection[23,24]. For example, the use of iodine in CT angiography helps decrease the tube voltage due to the specific absorption characteristics of iodine at different photon energies while improving the contrast-to-noise ratio (CNR)[25-27].
The product of the tube current and exposure time (tube current-time product) is one of the main factors affecting radiation dose. Increasing mAs will increase the photon flux, thereby increasing the radiation dose[17,18,28,29]. Dong et al[21] used ion chambers to record the radiation dose at the center and 12 o'clock locations of the CT dose index (CTDI) phantoms and measured exposure dose with 50 mAs, 100 mAs, 200 mAs, 300 mAs, and 400 mAs. The results showed that the radiation dose increased linearly with the increase in mAs. Additionally, reports indicate that the mAs value required for children to maintain the same CNR as adults is only 0.196 of the latter, and the radiation dose received by reducing mAs according to the standard is only 0.287 of the adult radiation dose[18]. Consequently, low mAs scanning is more suitable for pediatric CT examinations, but the tube current and exposure time need to be reasonably selected according to the adjustment of other parameters[17]. In summary, lowering the tube current can help save radiation exposure or optimize the image quality of low-dose pediatric CT, which can be applied to children's CT examinations.
Unlike other scanning parameters, reducing the field of view (FOV) has no negative effect on image quality under the condition that all the anatomical structures required for diagnosis are covered[28]. Commonly, with the change in the size of the FOV, the cone-beam geometry of the X-ray beam changes. The maximum angle of the cone corresponding to the smaller FOV is smaller, which reduces radiation dose by reducing overlap[30]. Therefore, it is necessary to choose the smallest possible FOV (including all anatomical structures required for chest examination) for children with smaller body sizes. Muenzel et al[31] set up a large FOV group (250-400 mm) and a small FOV group (< 250 mm) to research the effect of FOV size on radiation dose. The results showed that the radiation dose of the small FOV group was decreased by an average of 19.4% compared with the large FOV group. Moreover, the image spatial resolution of the latter was improved, and the cone-beam artifacts were optimized. Thus, the region of interest is precisely controlled to prevent unnecessary radiation exposure during the chest CT examination in children.
Image reconstruction techniques profoundly influence radiation dose and image quality[17]. Based on its simplicity, rapidity, and reliability, filtered back projection (FBP) has long been widely used as a standard algorithm for CT slice image reconstruction in clinical practice, continuously providing high-quality images for medical diagnosis. However, with the demand for low-dose CT imaging, the limitations of FBP are beginning to emerge[17,32]. As FBP is unable to handle complicated factors such as scattering, image deterioration is caused by the lowered radiation dose, making it unsuitable for pediatric low-dose CT examinations[17,33].
With the advent of iterative reconstruction (IR), the problem of image quality has been improved. As the IR algorithm involves multiple iterations, it allows the same image quality level to be achieved at a low radiation dose[33,34]. Consequently, IR is recommended for low-dose CT scans in children. Through the analysis of 49 studies on the impact of IR application on radiation dose, Willemink et al[35] believe that IR has the ability to optimize radiation dose (up to 76%) while ensuring image quality. Based on the phantom (Catphan500), Omotayo et al[36] objectively evaluated the image quality of IR on four different multidetector CT scanners with conventional FBP. The results showed that the IR algorithm was used to reduce the image noise and increase the CNR compared to FBP. The noise reduction range using the IR algorithm was 11%-51% for GE Discovery CT 750 HD, 10%-52% for Siemens Somatom Definition AS+, 49%-62% for Toshiba Aquilion 64, and 13%-44% for Philips Incident iCT 256 with the dose range of 1.3-1.5 mGy. The corresponding CNR increases with GE, Siemens, Toshiba and Philips were 11%-105%, 11%-106%, 85%-145% and 13%-77%, respectively. Currently, all major CT vendors have developed their own IR technology. Most commercially available IR algorithms are not entirely iterative but combine IR and FBP. The combination of IR and FBP is also called hybrid IR (HIR)[37,38]. Although progress has been made in HIR, the effects of over smoothing and noise texture changes are still visible as the percentage of IR increases. They may affect the distinctness of anatomic structures[39,40]. Therefore, it is essential to review the algorithms of different vendors[41] (Table 1) and optimize HIR, considering the patient’s weight and the clinical indications[42]. Radiologists tend to use lower levels of HIR in pediatrics with a lower body weight (< 35 kg) and higher levels in pediatrics with a larger body weight (average 72.5 kg)[43]. In general, the chest is the most extensively studied body region for children IR, and the radiation dose of IR chest CT is significantly lower than that of abdominal CT, which further contributes to the choice of a slightly more aggressive IR setting[41,42]. In addition, radiologists should set the IR algorithm in combination with other scanning parameters in clinical practice. Recently, deep learning reconstruction (DLR) has been introduced, which not only contributes to the optimization of radiation dose but also reconstructs high-quality images faster in low-dose CT examinations. Using the DLR algorithm to obtain the same quality image as FBP or IR, the radiation dose can be reduced by 30% to 71% and more than 50%, respectively[32]. In summary, combining IR and low tube voltage can reduce radiation dose and ensure image quality. The DLR algorithm has the potential to be superior to the current reconstruction technology for pediatric low-dose CT examinations.
| Vendors | GE | Toshiba | Siemens | Philips |
| Hybrid iterative reconstruction | Adaptive statistical iterative reconstruction | Adaptive iterative dose reduction 3D | Iterative reconstruction in image space; Sinogram-affirmed iterative reconstruction; advanced modeled iterative reconstruction | iDose 4 |
Advanced CT technologies, including filters, automatic tube current modulation (ATCM), automatic tube voltage selection (ATVS), and organ dose modulation (ODM), have been introduced. The methods mentioned above provide a convenient solution for reducing radiation dose in pediatric chest CT.
The low-energy photons contained in the X-ray beam are absorbed by the patient in CT scanning, which contributes to the radiation dose but does not have much effect on the image quality. The use of filters can remove low-energy photons from the beam to harden it, resulting in improved dose efficiency and reduced radiation dose[44]. Therefore, in pediatric chest CT examinations, the filter is used in combination with low kV, which can increase the average photon energy.
The degree of dose optimization caused by using filters of various materials is due to their differences in atomic number, K-edge energy, etc[45]. Currently, the types of filters include copper filters, silver filters, tin filters, etc. Of these, copper filters have become the standard[46]. Compared to standard copper filters, using silver filters reduces radiation dose by 74%. On the other hand, this technology also results in greater image noise. Fortunately, studies have shown that image quality issues can be improved through the use of silver filters combined with DLR[47,48]. Additionally, tin filters are widespread and an important method for lowering pediatric radiation doses. Using tin filters, PCD-CT reduces doses by up to 83% for non-contrast pediatric CT scans[44]. The protocol for the new "ultralow-dose" (ULD) is increasingly used in clinical practice. The ULD schemes for the chest, spine, and other parts show that using tin filters reduces the radiation dose greatly compared with the traditional protocols. Sn-100 kV is widely used in various ULD schemes, but for overweight patients, Sn-150 kV is chosen; for pediatric patients, protocols below Sn-100 kV are selected[49-51]. Using a filter is an important method for achieving low radiation doses in pediatric CT examinations, and its combination with other techniques (low kV, PCD-CT, DLR) is better for meeting diagnostic needs.
Using localizer images, the technology of ATCM adjusts mAs based on the patient’s anatomy. Patients are positioned at the center of rotation during CT scanning to ensure image quality and to minimize radiation dose[52]. Several studies[53] have reported the contribution of ATCM in optimizing radiation dose in children. Papadakis et al[53] used four physical anthropomorphic phantoms to represent children at the ages of 0, 1, 5, and 10 years, and the results showed that the application of ATCM for examination could reduce the radiation dose to various body regions while ensuring image quality, with the radiation dose to the chest potentially reduced by up to 39%. However, the application of ATCM technology in pediatric CT scans is not yet mature and still requires careful adjustment and use[54].
ATVS technology selects the corresponding kV value with the lowest radiation dose based on X-ray attenuation of patients with different body sizes and diagnostic requirements to minimize radiation exposure without compromising image quality[55]. The application of ATVS can reduce radiation dose in most body regions. With ATVS, more than 90% of CT scans have been performed at tube voltages below 100 kV, resulting in a significant change in tube voltage selection, greatly reducing radiation dose. Spearman et al[56] observed that the average volume CT dose index (CTDIvol) was reduced by 14.7% with ATVS for examination compared to without ATVS, based on the analysis of 164323 CT examinations worldwide. Additionally, Papadakis et al[53] used four physical anthropomorphic phantoms of different age groups, the dose reduction caused by ATVS varied due to clinical indications, with a reduction of 34% in the chest dose but an increase of 21% in the head dose. Therefore, the researchers advise that ATVS needs to be activated for all scans except for non-contrast head examinations. However, the increase of kV in the ATVS system will increase radiation dose when CT scans are performed on children with larger or overweight body sizes. The combination of ATVS and ATCM technology is a more effective method, preventing manual tube voltage error settings and unnecessary high radiation exposure to children with larger body sizes. This strategy can significantly reduce the radiation dose of non-contrast children’s chest CT, ensuring image quality. In liver CT, the combination of ATVS and ATCM achieved a dose reduction of 20% to 31% without compromising image quality compared to ATCM alone (fixed tube potential of 120 kV)[55,57]. The implementation of ATVS can achieve dose optimization and is suitable for pediatric CT examinations (except for head non-contrast examinations). In addition, the combination of ATCM and ATVS is conducive to further optimizing the pediatric CT examination protocol.
Conventional methods to reduce radiation dose, such as decreasing tube voltage and current, cannot achieve targeted protection for sensitive organs on the surface of the body[58]. Thus, the new ODM technology has been introduced, which adjusts the mAs to reduce by 40% on an approximately 180° arc anterior to the patients, without a corresponding increase posteriorly, thereby achieving an optimized dose for radiation-sensitive organs[59].
Due to clinical requirements, Zhao et al[58] used ODM to multiple organs in a female patient with cervical-thoracic-abdominal-pelvic contrast-enhanced CT scans across the entire scan area and found that the application of ODM reduced the tube currents to the thyroid, breast, and ovary layers on the anterior, left, posterior, and right aspects by 14.6%, 23.9%, and 22.8%, respectively. Due to the positive correlation between radiation dose and tube current, and radiation-sensitive glands are mostly located at the front of the body, ODM can effectively reduce the radiation dose to these organs. The application of ODM in body CT minimizes the radiation dose in the region to which ODM is applied and reduces the radiation dose outside the region[60]. The use of ODM may affect image quality[61], and image reconstruction is used to overcome this effect by utilizing full 360-degree signal acquisition. This methodology strategically employs the enhanced posterior signal intensity to offset the diminished anterior signal components[58]. As a new technology, ODM is beneficial for the protection of radiation-sensitive organs, and the lower signal can be compensated through image reconstruction to obtain the desired quality image.
The dose-length product (DLP) is derived from the CTDIvol product and the scanning length (L). CTDIvol is the local average radiation dose of CTDI phantom, and DLP is the overall radiation burden of the patient over the entire CT scanning[62,63]. Most scanners directly display the CTDIvol and DLP values, and the product of the DLP and the conversion factor can be used to estimate the effective dose (ED), which is expressed by the calculation formula (1): ED=k·DLP (1).
Where k represents the conversion factor[64]. The k value relies upon various factors, including the patient's age, gender, region, tube voltage, etc[64]. The corresponding k values for the head, neck, chest, abdomen, and pelvis of patients in different age groups are shown in Table 2[65].
| Head | Neck | Chest | Abdomen | Pelvis | |
| Adult | 0.0019 | 0.0052 | 0.0146 | 0.0153 | 0.0129 |
| 10-year-old | 0.0027 | 0.0094 | 0.0237 | 0.0249 | 0.0219 |
| 5-year-old | 0.0035 | 0.0121 | 0.0323 | 0.0357 | 0.0300 |
| 1-year-old | 0.0054 | 0.0168 | 0.0482 | 0.0530 | 0.0446 |
| Newborn | 0.0087 | 0.0210 | 0.0739 | 0.0841 | 0.0701 |
A study[63] compared the ED method using the conversion factors published by Shrimpton and Deak, respectively. The European Commission Concerted Action on CT established the Shrimpton conversion factor and derived it from the mathematic phantoms family representing newborns to adult ages through Monte Carlo simulation; the Deak conversion factor was updated based on the influence of modern scanners and different kV values. The results showed that the average calculation results of the Deak method were 10.2% ± 10.1% lower than those of the Shrimpton method. Although the Deak method has been updated, and the calculated ED value is slightly lower than the former, both ED methods corresponding to the two conversion factors are inaccurate in clinical applications due to the significant age gaps between the conversion factors. Individual factors such as the patient’s body size and age will be ignored using ED methods. In particular, for estimating pediatric radiation doses, the calculation is more complex than for adults, and the k value also varies greatly. If the k value for adults is used in the pediatric ED method calculation, it will greatly underestimate the radiation dose received by children[62,66,67]. The method used to calculate ED is simple, but the k value can significantly affect personalized ED estimates, especially for children's dose estimation.
The CTDIvol is the output radiation dose of the CT scanner based on a 16 cm or 32 cm standard phantom[68]. The calculation of radiation dose for pediatrics using 32 cm phantoms is often underestimated[69]. Therefore, the standard phantom with a diameter of 16 cm is usually used to represent the adult head and pediatric body, and the standard phantom with a diameter of 32 cm is used to define the adult body[70]. However, there is a certain difference between the patient’s body size and the examination region’s tissue structure density. Therefore, using CTDIvol to evaluate patients' radiation dose is inaccurate[68,71]. To assess the radiation dose accurately, the American Association of Physicists in Medicine (AAPM) proposed a size-specific dose estimation method based on effective diameter (SSDEED) to correct CTDIvol in 2011[72]. The SSDE method based on water equivalent diameter (SSDEWED) was proposed in 2014, which uses WED instead of DE to adequately consider the size and tissue structure of the scan region[73]. Studies[74] have shown that SSDEWED is more accurate than SSDEED in assessing CT radiation dose.
Compared with CTDIvol, the use of SSDEWED provides a more accurate reflection of the actual radiation dose in children, and there is a strong correlation with age[75]. Döwich et al[74] analyzed 133 pediatric chest CT scans, generating a SSDE for each patient based on WED and ED and compared them with CTDIvol. It was found that CTDIvol consistently underestimated the radiation dose compared to SSDE. Specifically, the radiation dose was underestimated by 54.7% compared to SSDEWED. In pediatric chest CT examinations, using SSDEWED can more accurately reflect the actual radiation dose in pediatrics.
In terms of accuracy, the Monte Carlo (MC) simulation is considered the gold standard for radiation dose estimation because it can accurately simulate the transmission of particles in media, providing the closest estimate for individual patient dose measurement[76,77]. There are more prominent MC tools, including Monte Carlo N-Particle Transport Code[78], GEometry ANd Tracking 4[79], GATE[77], etc. However, the method requires a large amount of computational effort and takes a longer time to simulate complex geometries, which limits the possibility of use in real-time dose planning[80,81]. Therefore, the MC method still requires further improvement in terms of time-saving.
CT dosimetry software computes radiation dose by inputting patient information and scan parameters[82]. Currently, commercially available software includes ImPACT, CT-Expo, NCICT2.0, etc.
ImPACT: The type of scanner, location and range of scanning on a phantom, kV, average tube current, gantry rotation time, slice thickness, collimation, and pitch are input into the ImPACT calculator to calculate CTDIvol, adult DLP, and adult ED. This software greatly simplifies the calculation of more specific effective doses. However, the ImPACT calculator is suitable for adults, and the calculation of pediatric dose requires the application of correction factors, which can be scanner-specific or location-specific (chest), but there is still a wide range based on age. Additionally, the accuracy of the radiation dose calculated by the ImPACT calculator is questionable[66,83,84].
CT-Expo: CT-Expo not only calculates all practical dose values (axial dose free-in-air, weighted CTDI, DLP, ED, and organ dose) but also allows for the calculation of age-specific dose values (adults, children, neonates) and gender-specific dose values, suitable for calculating pediatric radiation dose[85].
NCICT2.0: Based on the reference-size phantoms, the NCICT 1.0 provides batch dose calculation functionality for the convenience of dose calculation for many patients. NCICT 2.0 is an extension of NCICT 1.0 (a comprehensive dose library and longitudinal TCM profiles were created using the phantoms and then applied to the NCICT 2.0), where users can select age groups, gender, height, and weight. With the tube voltage, tube current, rotation time, TCM strength, and pitch inputted, NCICT 2.0 automatically calculates the average CTDIvol. Then, the scan range is defined, and the organ dose panel displays the absolute organ dose and ED. The software can significantly reduce the potential dosimetric errors caused by using only the reference-size phantoms[86].
CT dose measurement software can calculate radiation doses (including organ dose) based on patient characteristics, but there is still room for improvement in calculating CT doses for pediatrics.
This review summarizes the main factors that affect radiation dose in pediatric chest CT examination, such as detector, tube voltage, tube current-time product, FOV and reconstruction algorithms. Secondly, the technologies of filters, ATCM, ATVS, and ODM, etc., applied to CT examinations to optimize the scanning protocol were introduced. The introduction of emerging technologies has facilitated the development of CT scan schemes and contributed to the reduction of radiation dose in pediatrics. Finally, the article describes four methods for estimating radiation doses. The ED method is the simplest to calculate, but due to the large age gap between the conversion factors, the calculation results of the organ dose ED for pediatrics are inaccurate. CT dosimetry software, the SSDE method, and MC method can integrate the individualized characteristics of the patient for estimation. In summary, this review describes the influencing factors, CT techniques, and dose calculation methods, aiming to provide a theoretical foundation for clinicians to optimize the CT scan scheme in pediatrics and provide a basis for subsequent development and research in the field of radiation protection.
| 1. | Budoff M. Cardiac CT: benefits outweigh the risks. J Cardiovasc Comput Tomogr. 2011;5:275-276. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 2. | Pearce MS, Salotti JA, Little MP, McHugh K, Lee C, Kim KP, Howe NL, Ronckers CM, Rajaraman P, Sir Craft AW, Parker L, Berrington de González A. Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: a retrospective cohort study. Lancet. 2012;380:499-505. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2528] [Cited by in RCA: 2728] [Article Influence: 194.9] [Reference Citation Analysis (1)] |
| 3. | Lobo L, Antunes D. Chest CT in infants and children. Eur J Radiol. 2013;82:1108-1117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 4. | Pearce MS. Patterns in paediatric CT use: an international and epidemiological perspective. J Med Imaging Radiat Oncol. 2011;55:107-109. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 30] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 5. | Brink JA, Morin RL. Size-specific dose estimation for CT: how should it be used and what does it mean? Radiology. 2012;265:666-668. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 71] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 6. | Miglioretti DL, Johnson E, Williams A, Greenlee RT, Weinmann S, Solberg LI, Feigelson HS, Roblin D, Flynn MJ, Vanneman N, Smith-Bindman R. The use of computed tomography in pediatrics and the associated radiation exposure and estimated cancer risk. JAMA Pediatr. 2013;167:700-707. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1033] [Cited by in RCA: 1082] [Article Influence: 83.2] [Reference Citation Analysis (0)] |
| 7. | Health Risks from Exposure to Low Levels of Ionizing Radiation: BEIR VII, Phase I, Letter Report (1998). Washington (DC): National Academies Press (US); 1998 . [PubMed] |
| 8. | Preston DL, Ron E, Tokuoka S, Funamoto S, Nishi N, Soda M, Mabuchi K, Kodama K. Solid cancer incidence in atomic bomb survivors: 1958-1998. Radiat Res. 2007;168:1-64. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1224] [Cited by in RCA: 1248] [Article Influence: 65.7] [Reference Citation Analysis (0)] |
| 9. | Hauptmann M, Byrnes G, Cardis E, Bernier MO, Blettner M, Dabin J, Engels H, Istad TS, Johansen C, Kaijser M, Kjaerheim K, Journy N, Meulepas JM, Moissonnier M, Ronckers C, Thierry-Chef I, Le Cornet L, Jahnen A, Pokora R, Bosch de Basea M, Figuerola J, Maccia C, Nordenskjold A, Harbron RW, Lee C, Simon SL, Berrington de Gonzalez A, Schüz J, Kesminiene A. Brain cancer after radiation exposure from CT examinations of children and young adults: results from the EPI-CT cohort study. Lancet Oncol. 2023;24:45-53. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 147] [Article Influence: 49.0] [Reference Citation Analysis (0)] |
| 10. | Kalender WA. Dose in x-ray computed tomography. Phys Med Biol. 2014;59:R129-R150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 127] [Cited by in RCA: 127] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 11. | Frush DP, Donnelly LF, Rosen NS. Computed tomography and radiation risks: what pediatric health care providers should know. Pediatrics. 2003;112:951-957. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 440] [Cited by in RCA: 407] [Article Influence: 17.7] [Reference Citation Analysis (0)] |
| 12. | Willemink MJ, Persson M, Pourmorteza A, Pelc NJ, Fleischmann D. Photon-counting CT: Technical Principles and Clinical Prospects. Radiology. 2018;289:293-312. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 326] [Cited by in RCA: 837] [Article Influence: 104.6] [Reference Citation Analysis (0)] |
| 13. | Schmidt TG. CT energy weighting in the presence of scatter and limited energy resolution. Med Phys. 2010;37:1056-1067. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 44] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 14. | Symons R, Pourmorteza A, Sandfort V, Ahlman MA, Cropper T, Mallek M, Kappler S, Ulzheimer S, Mahesh M, Jones EC, Malayeri AA, Folio LR, Bluemke DA. Feasibility of Dose-reduced Chest CT with Photon-counting Detectors: Initial Results in Humans. Radiology. 2017;285:980-989. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 155] [Article Influence: 17.2] [Reference Citation Analysis (0)] |
| 15. | Fletcher JG, Inoue A, Bratt A, Horst KK, Koo CW, Rajiah PS, Baffour FI, Ko JP, Remy-Jardin M, McCollough CH, Yu L. Photon-counting CT in Thoracic Imaging: Early Clinical Evidence and Incorporation Into Clinical Practice. Radiology. 2024;310:e231986. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 33] [Article Influence: 16.5] [Reference Citation Analysis (0)] |
| 16. | Horst KK, Yu L, McCollough CH, Esquivel A, Thorne JE, Rajiah PS, Baffour F, Hull NC, Weber NM, Thacker PG, Thomas KB, Binkovitz LA, Guerin JB, Fletcher JG. Potential benefits of photon counting detector computed tomography in pediatric imaging. Br J Radiol. 2023;96:20230189. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 24] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 17. | Nagayama Y, Oda S, Nakaura T, Tsuji A, Urata J, Furusawa M, Utsunomiya D, Funama Y, Kidoh M, Yamashita Y. Radiation Dose Reduction at Pediatric CT: Use of Low Tube Voltage and Iterative Reconstruction. Radiographics. 2018;38:1421-1440. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 52] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 18. | Boone JM, Geraghty EM, Seibert JA, Wootton-Gorges SL. Dose reduction in pediatric CT: a rational approach. Radiology. 2003;228:352-360. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 209] [Cited by in RCA: 176] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 19. | Yu L, Bruesewitz MR, Thomas KB, Fletcher JG, Kofler JM, McCollough CH. Optimal tube potential for radiation dose reduction in pediatric CT: principles, clinical implementations, and pitfalls. Radiographics. 2011;31:835-848. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 152] [Cited by in RCA: 172] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 20. | Sigal-Cinqualbre AB, Hennequin R, Abada HT, Chen X, Paul JF. Low-kilovoltage multi-detector row chest CT in adults: feasibility and effect on image quality and iodine dose. Radiology. 2004;231:169-174. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 313] [Cited by in RCA: 290] [Article Influence: 13.2] [Reference Citation Analysis (0)] |
| 21. | Dong F, Davros W, Pozzuto J, Reid J. Optimization of kilovoltage and tube current-exposure time product based on abdominal circumference: an oval phantom study for pediatric abdominal CT. AJR Am J Roentgenol. 2012;199:670-676. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 24] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 22. | Klink T, Obmann V, Heverhagen J, Stork A, Adam G, Begemann P. Reducing CT radiation dose with iterative reconstruction algorithms: the influence of scan and reconstruction parameters on image quality and CTDIvol. Eur J Radiol. 2014;83:1645-1654. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 43] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 23. | Singh S, Kalra MK, Moore MA, Shailam R, Liu B, Toth TL, Grant E, Westra SJ. Dose reduction and compliance with pediatric CT protocols adapted to patient size, clinical indication, and number of prior studies. Radiology. 2009;252:200-208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 158] [Cited by in RCA: 154] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 24. | Singh S, Kalra MK, Thrall JH, Mahesh M. Pointers for optimizing radiation dose in pediatric CT protocols. J Am Coll Radiol. 2012;9:77-79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 25. | Nakayama Y, Awai K, Funama Y, Hatemura M, Imuta M, Nakaura T, Ryu D, Morishita S, Sultana S, Sato N, Yamashita Y. Abdominal CT with low tube voltage: preliminary observations about radiation dose, contrast enhancement, image quality, and noise. Radiology. 2005;237:945-951. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 344] [Cited by in RCA: 344] [Article Influence: 16.4] [Reference Citation Analysis (0)] |
| 26. | Iezzi R, Santoro M, Marano R, Di Stasi C, Dattesi R, Kirchin M, Tinelli G, Snider F, Bonomo L. Low-dose multidetector CT angiography in the evaluation of infrarenal aorta and peripheral arterial occlusive disease. Radiology. 2012;263:287-298. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 48] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 27. | Kalva SP, Sahani DV, Hahn PF, Saini S. Using the K-edge to improve contrast conspicuity and to lower radiation dose with a 16-MDCT: a phantom and human study. J Comput Assist Tomogr. 2006;30:391-397. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 128] [Cited by in RCA: 125] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 28. | Moser JB, Sheard SL, Edyvean S, Vlahos I. Radiation dose-reduction strategies in thoracic CT. Clin Radiol. 2017;72:407-420. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 21] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 29. | Wu D, Wang G, Bian B, Liu Z, Li D. Benefits of Low-Dose CT Scan of Head for Patients With Intracranial Hemorrhage. Dose Response. 2020;19:1559325820909778. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 30. | Hsieh J, Londt J, Vass M, Li J, Tang X, Okerlund D. Step-and-shoot data acquisition and reconstruction for cardiac x-ray computed tomography. Med Phys. 2006;33:4236-4248. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 181] [Cited by in RCA: 175] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 31. | Muenzel D, Noel PB, Dorn F, Dobritz M, Rummeny EJ, Huber A. Coronary CT angiography in step-and-shoot technique with 256-slice CT: impact of the field of view on image quality, craniocaudal coverage, and radiation exposure. Eur J Radiol. 2012;81:1562-1568. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 32. | Koetzier LR, Mastrodicasa D, Szczykutowicz TP, van der Werf NR, Wang AS, Sandfort V, van der Molen AJ, Fleischmann D, Willemink MJ. Deep Learning Image Reconstruction for CT: Technical Principles and Clinical Prospects. Radiology. 2023;306:e221257. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 227] [Article Influence: 75.7] [Reference Citation Analysis (0)] |
| 33. | den Harder AM, Willemink MJ, de Ruiter QM, Schilham AM, Krestin GP, Leiner T, de Jong PA, Budde RP. Achievable dose reduction using iterative reconstruction for chest computed tomography: A systematic review. Eur J Radiol. 2015;84:2307-2313. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 57] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 34. | Yang CC. Evaluation of Impact of Factors Affecting CT Radiation Dose for Optimizing Patient Dose Levels. Diagnostics (Basel). 2020;10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 35. | Willemink MJ, Leiner T, de Jong PA, de Heer LM, Nievelstein RA, Schilham AM, Budde RP. Iterative reconstruction techniques for computed tomography part 2: initial results in dose reduction and image quality. Eur Radiol. 2013;23:1632-1642. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 201] [Cited by in RCA: 203] [Article Influence: 15.6] [Reference Citation Analysis (0)] |
| 36. | Omotayo A, Elbakri I. Objective performance assessment of five computed tomography iterative reconstruction algorithms. J Xray Sci Technol. 2016;24:913-930. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 37. | Raman SP, Johnson PT, Deshmukh S, Mahesh M, Grant KL, Fishman EK. CT dose reduction applications: available tools on the latest generation of CT scanners. J Am Coll Radiol. 2013;10:37-41. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 103] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 38. | Willemink MJ, de Jong PA, Leiner T, de Heer LM, Nievelstein RA, Budde RP, Schilham AM. Iterative reconstruction techniques for computed tomography Part 1: technical principles. Eur Radiol. 2013;23:1623-1631. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 283] [Cited by in RCA: 314] [Article Influence: 24.2] [Reference Citation Analysis (0)] |
| 39. | Miéville FA, Gudinchet F, Rizzo E, Ou P, Brunelle F, Bochud FO, Verdun FR. Paediatric cardiac CT examinations: impact of the iterative reconstruction method ASIR on image quality--preliminary findings. Pediatr Radiol. 2011;41:1154-1164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 59] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 40. | Brady SL, Yee BS, Kaufman RA. Characterization of adaptive statistical iterative reconstruction algorithm for dose reduction in CT: A pediatric oncology perspective. Med Phys. 2012;39:5520-5531. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 44] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 41. | den Harder AM, Willemink MJ, Budde RP, Schilham AM, Leiner T, de Jong PA. Hybrid and model-based iterative reconstruction techniques for pediatric CT. AJR Am J Roentgenol. 2015;204:645-653. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 36] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 42. | Singh S, Kalra MK, Shenoy-Bhangle AS, Saini A, Gervais DA, Westra SJ, Thrall JH. Radiation dose reduction with hybrid iterative reconstruction for pediatric CT. Radiology. 2012;263:537-546. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 104] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 43. | Karmazyn B, Liang Y, Ai H, Eckert GJ, Cohen MD, Wanner MR, Jennings SG. Optimization of hybrid iterative reconstruction level in pediatric body CT. AJR Am J Roentgenol. 2014;202:426-431. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 44. | Rajendran K, Voss BA, Zhou W, Tao S, DeLone DR, Lane JI, Weaver JM, Carlson ML, Fletcher JG, McCollough CH, Leng S. Dose Reduction for Sinus and Temporal Bone Imaging Using Photon-Counting Detector CT With an Additional Tin Filter. Invest Radiol. 2020;55:91-100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 114] [Article Influence: 19.0] [Reference Citation Analysis (0)] |
| 45. | Atak H, Shikhaliev PM. Photon counting x-ray imaging with K-edge filtered x-rays: A simulation study. Med Phys. 2016;43:1385-1400. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 46. | Golbus AE, Steveson C, Schuzer JL, Rollison SF, Worthy T, Jones AM, Julien-Williams P, Moss J, Chen MY. Ultra-low dose chest CT with silver filter and deep learning reconstruction significantly reduces radiation dose and retains quantitative information in the investigation and monitoring of lymphangioleiomyomatosis (LAM). Eur Radiol. 2024;34:5613-5620. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 9] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 47. | Nomura K, Fujii K, Goto T, Tsukagoshi S, Ota H, Iwabuchi Y, Suzuki H, Muramatsu Y, Kobayashi T. Radiation Dose Reduction for Computed Tomography Localizer Radiography Using an Ag Additional Filter. J Comput Assist Tomogr. 2021;45:84-92. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 48. | Oshima Y, Ohno Y, Takenaka D, Ito Y, Kimata H, Fujii K, Akino N, Hamabuchi N, Matsuyama T, Nagata H, Ueda T, Ikeda H, Ozawa Y, Yoshikawa T, Toyama H. Capability for dose reduction while maintaining nodule detection: Comparison of silver and copper X-ray spectrum modulation filters for chest CT using a phantom study with different reconstruction methods. Eur J Radiol. 2023;166:110969. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 49. | Gordic S, Morsbach F, Schmidt B, Allmendinger T, Flohr T, Husarik D, Baumueller S, Raupach R, Stolzmann P, Leschka S, Frauenfelder T, Alkadhi H. Ultralow-dose chest computed tomography for pulmonary nodule detection: first performance evaluation of single energy scanning with spectral shaping. Invest Radiol. 2014;49:465-473. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 173] [Cited by in RCA: 199] [Article Influence: 18.1] [Reference Citation Analysis (0)] |
| 50. | Greffier J, Pereira F, Hamard A, Addala T, Beregi JP, Frandon J. Effect of tin filter-based spectral shaping CT on image quality and radiation dose for routine use on ultralow-dose CT protocols: A phantom study. Diagn Interv Imaging. 2020;101:373-381. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 44] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 51. | Lee SM, Choo HJ, Lee SJ, Kim SK, Lee IS, Kim DW, Baek JW, Heo YJ. Cervical Spine CT Using Spectral Shaping: Can It Be a Solution to Overcome Artifacts in the Lower Cervical Spinal Region? Korean J Radiol. 2019;20:469-478. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 16] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 52. | Nelson TR. Practical strategies to reduce pediatric CT radiation dose. J Am Coll Radiol. 2014;11:292-299. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 43] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 53. | Papadakis AE, Damilakis J. Automatic Tube Current Modulation and Tube Voltage Selection in Pediatric Computed Tomography: A Phantom Study on Radiation Dose and Image Quality. Invest Radiol. 2019;54:265-272. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 57] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 54. | Nievelstein RA, van Dam IM, van der Molen AJ. Multidetector CT in children: current concepts and dose reduction strategies. Pediatr Radiol. 2010;40:1324-1344. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 151] [Cited by in RCA: 142] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 55. | Lee KH, Lee JM, Moon SK, Baek JH, Park JH, Flohr TG, Kim KW, Kim SJ, Han JK, Choi BI. Attenuation-based automatic tube voltage selection and tube current modulation for dose reduction at contrast-enhanced liver CT. Radiology. 2012;265:437-447. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 79] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 56. | Spearman JV, Schoepf UJ, Rottenkolber M, Driesser I, Canstein C, Thierfelder KM, Krazinski AW, De Cecco CN, Meinel FG. Effect of Automated Attenuation-based Tube Voltage Selection on Radiation Dose at CT: An Observational Study on a Global Scale. Radiology. 2016;279:167-174. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 36] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 57. | Hojreh A, Homolka P, Gamper J, Unterhumer S, Kienzl-Palma D, Balassy C, Wrba T, Prosch H. Automated tube voltage selection in pediatric non-contrast chest CT. PLoS One. 2018;13:e0204794. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 58. | Zhao Y, Geng X, Li D, Zhang T, Xu Y. Application of full-field organ dose modulation on cervical- thoraco-abdominopelvic contrast-enhanced computed tomography. Jpn J Radiol. 2021;39:254-260. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 59. | Fu W, Sturgeon GM, Agasthya G, Segars WP, Kapadia AJ, Samei E. Breast dose reduction with organ-based, wide-angle tube current modulated CT. J Med Imaging (Bellingham). 2017;4:031208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 60. | Inoue Y, Itoh H, Koizumi K, Sekimoto S, Hata H, Miyatake H, Yamane T, Mitsui K. Effects of organ dose modulation applied to a part of the scan range on radiation dose in computed tomography of the body. J Radiol Prot. 2024;44. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 61. | Dixon MT, Loader RJ, Stevens GC, Rowles NP. An evaluation of organ dose modulation on a GE optima CT660-computed tomography scanner. J Appl Clin Med Phys. 2016;17:380-391. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 25] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 62. | Thomas KE, Wang B. Age-specific effective doses for pediatric MSCT examinations at a large children's hospital using DLP conversion coefficients: a simple estimation method. Pediatr Radiol. 2008;38:645-656. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 161] [Cited by in RCA: 164] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 63. | Newman B, Ganguly A, Kim JE, Robinson T. Comparison of different methods of calculating CT radiation effective dose in children. AJR Am J Roentgenol. 2012;199:W232-W239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 27] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 64. | Saltybaeva N, Jafari ME, Hupfer M, Kalender WA. Estimates of effective dose for CT scans of the lower extremities. Radiology. 2014;273:153-159. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 99] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 65. | The 2007 Recommendations of the International Commission on Radiological Protection. ICRP publication 103. Ann ICRP. 2007;37:1-332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 206] [Cited by in RCA: 1133] [Article Influence: 62.9] [Reference Citation Analysis (0)] |
| 66. | Shrimpton PC, Hillier MC, Lewis MA, Dunn M. National survey of doses from CT in the UK: 2003. Br J Radiol. 2006;79:968-980. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 404] [Cited by in RCA: 431] [Article Influence: 22.7] [Reference Citation Analysis (0)] |
| 67. | Deak PD, Smal Y, Kalender WA. Multisection CT protocols: sex- and age-specific conversion factors used to determine effective dose from dose-length product. Radiology. 2010;257:158-166. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 612] [Cited by in RCA: 629] [Article Influence: 39.3] [Reference Citation Analysis (0)] |
| 68. | Gabusi M, Riccardi L, Aliberti C, Vio S, Paiusco M. Radiation dose in chest CT: Assessment of size-specific dose estimates based on water-equivalent correction. Phys Med. 2016;32:393-397. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 29] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 69. | Miyazaki O, Horiuchi T, Masaki H, Nosaka S, Miyasaka M, Tsutsumi Y, Okada Y, Kitamura M. Estimation of adaptive computed tomography dose index based on body weight in pediatric patients. Radiat Med. 2008;26:98-103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 70. | McCollough CH, Leng S, Yu L, Cody DD, Boone JM, McNitt-Gray MF. CT dose index and patient dose: they are not the same thing. Radiology. 2011;259:311-316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 304] [Cited by in RCA: 317] [Article Influence: 21.1] [Reference Citation Analysis (0)] |
| 71. | Abuhaimed A, Martin CJ. Estimation of size-specific dose estimates (SSDE) for paediatric and adults patients based on a single slice. Phys Med. 2020;74:30-39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 27] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 72. | Li B, Behrman RH. Comment on the "report of AAPM TG 204: size-specific dose estimates (SSDE) in pediatric and adult body CT examinations" [report of AAPM TG 204, 2011]. Med Phys. 2012;39:4613-4; author reply 4615. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 18] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 73. | McCollough C, Bakalyar DM, Bostani M, Brady S, Boedeker K, Boone JM, Chen-Mayer HH, Christianson OI, Leng S, Li B, McNitt-Gray MF, Nilsen RA, Supanich MP, Wang J. Use of Water Equivalent Diameter for Calculating Patient Size and Size-Specific Dose Estimates (SSDE) in CT: The Report of AAPM Task Group 220. AAPM Rep. 2014;2014:6-23. [PubMed] |
| 74. | Döwich V, Torres FS, Nietto AL, Timm VS, Anés M, Bacelar A, Maróstica PJC. Radiation dose assessment of pediatric computed tomography of the chest: the need to consider patient size. Radiat Prot Dosimetry. 2024;200:2008-2013. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 75. | Zhang J, Zhang X. Size specific dose estimation in pediatric CT: preliminary study and conversion factors. Radiat Prot Dosimetry. 2024;200:677-686. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 76. | Zobrist B, Bertholet J, Frei D, Volken W, Amstutz F, Stampanoni MFM, Manser P, Fix MK, Loebner HA. Monte Carlo dose calculation for photon and electron radiotherapy on dynamically deforming anatomy. Med Phys. 2025;52:1281-1292. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 77. | Sarrut D, Arbor N, Baudier T, Borys D, Etxebeste A, Fuchs H, Gajewski J, Grevillot L, Jan S, Kagadis GC, Kang HG, Kirov A, Kochebina O, Krzemien W, Lomax A, Papadimitroulas P, Pommranz C, Roncali E, Rucinski A, Winterhalter C, Maigne L. The OpenGATE ecosystem for Monte Carlo simulation in medical physics. Phys Med Biol. 2022;67. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 43] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 78. | Goorley T, James M, Booth T, Brown F, Bull J, Cox L, Durkee J, Elson J, Fensin M, Forster R, Hendricks J, Hughes H, Johns R, Kiedrowski B, Martz R, Mashnik S, Mckinney G, Pelowitz D, Prael R, Sweezy J, Waters L, Wilcox T, Zukaitis T. Features of MCNP6. Ann Nucl Energy. 2016;87:772-783. [RCA] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 75] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 79. | Carrier JF, Archambault L, Beaulieu L, Roy R. Validation of GEANT4, an object-oriented Monte Carlo toolkit, for simulations in medical physics. Med Phys. 2004;31:484-492. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 127] [Cited by in RCA: 102] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 80. | Waeleh N, Saripan MI, Musarudin M, Ahmad Saad FF, Mashohor S, Hashim S. Towards efficient Monte Carlo N-Particle simulation of a positron emission tomography (PET) via source volume definition. Appl Radiat Isot. 2022;189:110418. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 81. | Chen W, Kolditz D, Beister M, Bohle R, Kalender WA. Fast on-site Monte Carlo tool for dose calculations in CT applications. Med Phys. 2012;39:2985-2996. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 68] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 82. | Huda W, Ogden KM, Khorasani MR. Converting dose-length product to effective dose at CT. Radiology. 2008;248:995-1003. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 391] [Cited by in RCA: 401] [Article Influence: 22.3] [Reference Citation Analysis (0)] |
| 83. | Groves AM, Owen KE, Courtney HM, Yates SJ, Goldstone KE, Blake GM, Dixon AK. 16-detector multislice CT: dosimetry estimation by TLD measurement compared with Monte Carlo simulation. Br J Radiol. 2004;77:662-665. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 64] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 84. | Khursheed A, Hillier MC, Shrimpton PC, Wall BF. Influence of patient age on normalized effective doses calculated for CT examinations. Br J Radiol. 2002;75:819-830. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 151] [Cited by in RCA: 146] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 85. | Stamm G, Nagel HD. [CT-expo--a novel program for dose evaluation in CT]. Rofo. 2002;174:1570-1576. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 264] [Cited by in RCA: 278] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 86. | Lee C, Yeom YS, Folio L. CT organ dose calculator size adaptive for pediatric and adult patients. Biomed Phys Eng Express. 2022;8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 12] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/