Published online Apr 28, 2025. doi: 10.4329/wjr.v17.i4.105960
Revised: March 15, 2025
Accepted: March 26, 2025
Published online: April 28, 2025
Processing time: 69 Days and 22.4 Hours
Traumatic hemothorax is a common complication of chest trauma; however, the timeline for its resolution, even with chest tube thoracostomy, remains unclear.
To determine the time to resolution of the hemothorax to ensure safe discharge based on chest radiography (CXR) findings.
A retrospective observational study was conducted at Hamad General Hospital, Qatar, from June 2014 to October 2019, including all patients with hemothorax diagnosed via computed tomography (CT) following chest trauma. Based on the initial imaging study, the hemothorax was divided into right, left, and bilateral.
The study included 422 patients. Of the total, 57.82% (n = 244/422) resolved their hemothorax within three days of admission. Among these, 44 patients required chest tube insertion (CTI) and 200 were cleared without it. Between days 3 and 7, an additional 16.83% (n = 71 /422) of cases were resolved, of which 28 required chest tubes. By days 8 to 14, another 11.37% (n = 48/422) were cleared, with 15 patients requiring chest tubes. After 14 days, 13.98% (n = 59/422) of patients still had hemothorax, 14 of whom required CTI.
This study showed that a subset of patients continued to experience retained hemothorax despite early tube thoracostomy. Patients with a larger hemothorax, particularly on the left side, showed prolonged resolution times. Regular imaging such as CXR or CT is recommended for up to 14 days post-intervention. After this period, outpatient follow-up is generally safe, although some patients may still have a persistent hemothorax beyond two weeks.
Core Tip: Traumatic hemothorax often requires chest tube insertion for resolution. However, the duration of follow-up for small or retained hemothorax (RH) remains uncertain. We aimed to determine the appropriate follow-up duration by using chest radiography (CXR) or computed tomography (CT). The study included 422 patients. Of these, 75% resolved their hemothorax within 7 days and 11% on days 8 to 14 post-admission. A subset of patients continued to experience RH despite early tube insertion. Patients with larger hemothoraces, particularly on the left side, exhibited prolonged resolution times. Regular imaging using CXR or CT is recommended for up to 14 days post-intervention.
- Citation: Ahmed K, Al-Hassani A, El-Menyar A, Nabir S, Ahmed MN, Almadani A, Mahmood I, Mekkodathil A, Peralta R, Rizoli S, Al-Thani H. Time to resolution of radiologically detected hemothorax in trauma patients: A retrospective observational study. World J Radiol 2025; 17(4): 105960
- URL: https://www.wjgnet.com/1949-8470/full/v17/i4/105960.htm
- DOI: https://dx.doi.org/10.4329/wjr.v17.i4.105960
Thoracic injuries are common in patients with blunt trauma and rank as the third most prevalent cause of trauma after head and limb injuries. Thoracic trauma entails significant morbidity and mortality, accounting for approximately 25% of trauma-related fatalities, second only to head trauma[1]. The estimated annual incidence of thoracic trauma in the United States is 300000 individuals. Within the emergency department (ED), chest radiography (CXR) serves as the primary diagnostic modality for patients with blunt chest trauma, detecting significant injuries in 6.3% to 12.4% of cases[2]. Currently, chest computed tomography (CT) is the standard imaging tool in ED settings, with a substantial increase in its utilization for the initial assessment of patients with chest trauma[3].
Thoracic injuries commonly lead to the accumulation of blood in the pleural space, known as hemothorax, with an estimated incidence of approximately 21.8%[4]. Traditional hemothorax management involves chest tube placement as advised by the guidelines of the Eastern Association for the Surgery of Trauma guidelines[5]. Despite the effective management of hemothorax with tube thoracostomy (chest tube), this intervention presents potentially serious complications such as iatrogenic injury, retained hemothorax (RH), and empyema in up to 22% of patients[6]. Even after chest tube removal, some patients may continue to exhibit RH and require further intervention or hospital admission.
A retrospective study[7] observed a 3% resolution of RH during a clinical follow-up 1 to 2 weeks after discharge in patients with blunt chest trauma. Asymptomatic patients were discharged from the trauma service. Another study[8] reported a diagnosis of hemothorax in 7.4% of outpatients with at least one rib fracture within 14 days. Moreover, app
Given the absence of Level I data, a protocolized approach was proposed to enhance patient outcomes and cost-effectiveness in the management of posttraumatic RH[11]. Careful consideration of the potential benefits and limitations of all available therapy modalities is essential for individual patients[9]. The time required to resolve RH after chest tube thoracostomy remains inadequately understood, highlighting the need for further research to address this knowledge gap.
This study aimed to evaluate the timeline required to resolve traumatic hemothorax after proper intervention, and to consider an appropriate time for safe discharge and/or follow-up of these patients.
In this retrospective study, we analyzed the data retrieved from the medical records and trauma registry of the Level I Trauma Center at Hamad General Hospital. This study included adult trauma patients who exhibited hemothorax on their first CT scan upon admission to the hospital between June 2014 and October 2019. The exclusion criteria were pediatric patients and individuals without confirmed chest trauma, as indicated by CT imaging (only blunt chest trauma, not penetrating chest trauma).
Our study focused on various parameters, including demographic information (age, sex, and nationality), mechanism of injury, associated injuries (chest, spine, pelvis, abdomen, and extremities), Glasgow coma score, injury severity score, chest abbreviated injury score (AIS), intubation, intensive care unit (ICU) admission, CT findings of hemothorax, pneu
RH was defined as residual pleural blood exceeding 500 mL in volume, blood occupying more than one-third of the thoracic cavity, or any residual blood that could not be drained 72 hours after thoracotomy treatment[12].
As appropriate, data are presented as proportions, medians, or mean ± SD. The patients were divided into two groups based on the intervention: Chest tube or conservative treatment. Baseline demographic characteristics, management, and outcomes were compared according to management (CTI vs conservative treatment) using the student’s-t test for continuous variables and Pearson χ2 test for categorical variables. For skewed continuous data, a non-parametric Mann-Whitney U test was performed. Two-tailed P values of < 0.05. were considered significant. Data analysis was conducted using the Statistical Package for Social Sciences version 18 (SPSS Inc., Chicago, IL United States).
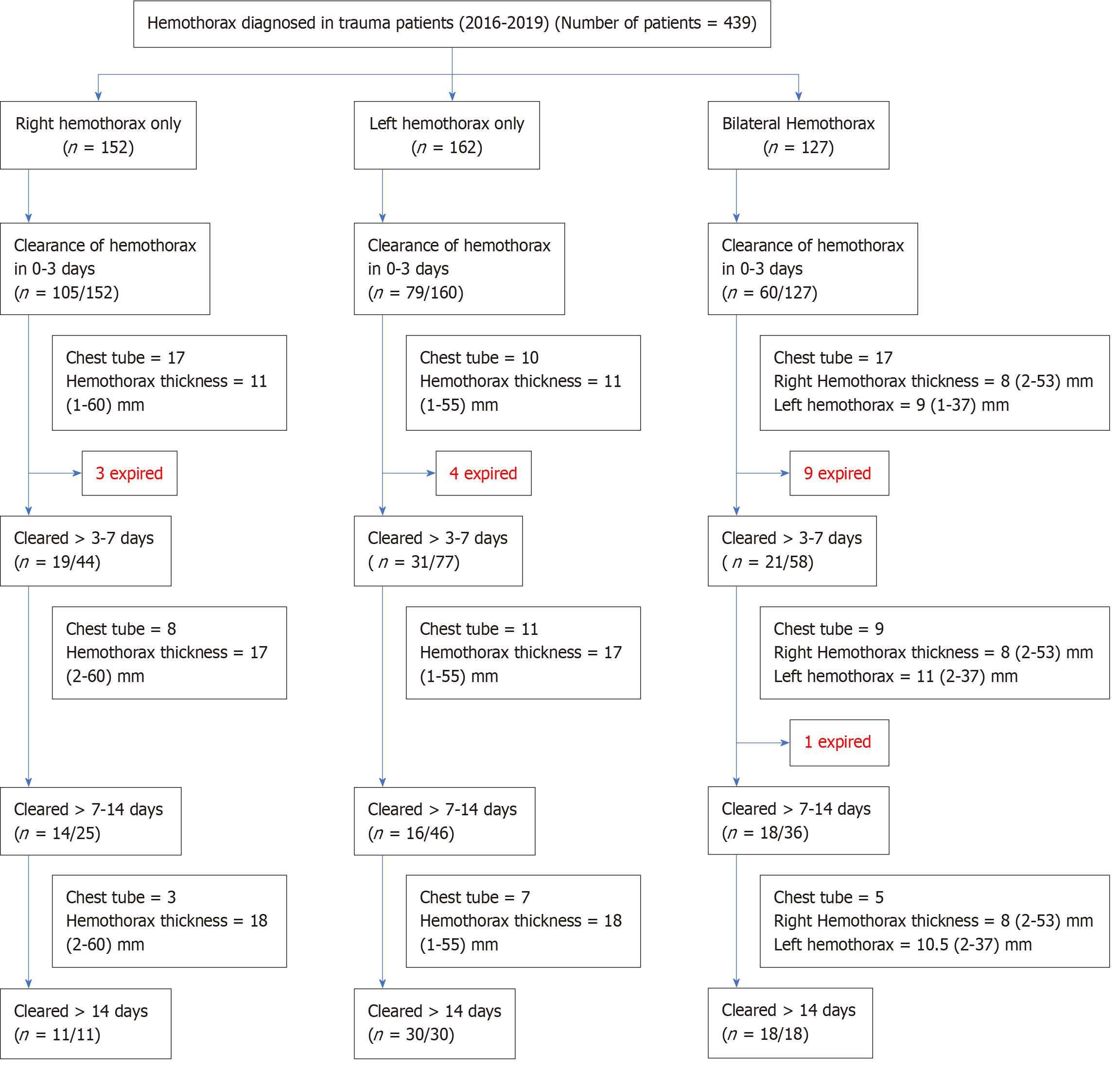
A total of 439 patients were included in the study. After excluding 17 patients who died (within the 1st week), 422 patients were included in the analysis. Figure 1 shows a flowchart of the hemothorax management including classification based on laterality, hemothorax clearance time, and outcomes. The mean age was 38.56 years (SD 15.06), and 91% were males. Motor vehicle crashes were the most common mode of injury (36.5%), followed by falls (27.7%) and pedestrian collisions (12.8%). Most patients had polytrauma, with head (28.2%), abdominal (34.4%), spinal (41.7%), and pelvic (23.5%) injuries. The mean ISS was 20.3. Pneumothorax was present in 63% of patients, 48.1% had lung contusion, and 87.2% had rib fractures. Endotracheal intubation was required in 30.1% of patients, whereas chest tubes were inserted in 23.9%. The median ICU length of stay was 5 days (2-14), with a mortality rate of 1.2%. Of the total, 152 were right-sided, 160 were left-sided, and 127 cases were bilateral hemothorax. Table 1 shows a description of trauma patients diagnosed with hemothorax on admission.
| Demographic information | Value |
| Mean age (SD) years | 38.6 (15.06) |
| Males | 384 (90.9) |
| Mechanism of injury | |
| Motor vehicle crashes | 154 (36.5) |
| Fall | 117 (27.7) |
| Pedestrian | 54 (12.8) |
| Associated injuries | |
| Head | 119 (28.2) |
| Abdomen | 145 (34.4) |
| Spine | 176 (41.7) |
| Pelvis | 99 (23.5) |
| Injury scores; mean (SD) | |
| Chest AIS | 3.1 (0.26) |
| Head AIS | 3.6 (0.99) |
| Abdomen AIS | 2.9 (1.08) |
| Spine AIS | 2.2 (0.68) |
| ISS | 20.3 (11.26) |
| Other chest injuries | |
| Pneumothorax | 266 (63.0) |
| Lung contusion | 203 (48.1) |
| Rib fracture | 368 (87.2) |
| Interventions | |
| Intubation | 127 (30.1) |
| Chest tube insertion | 101 (23.9) |
| Outcomes | Days |
| ICU LOS; Median (IQR) | 5 (2-14) |
| Mortality (after clearance) | 5 (1.2) |
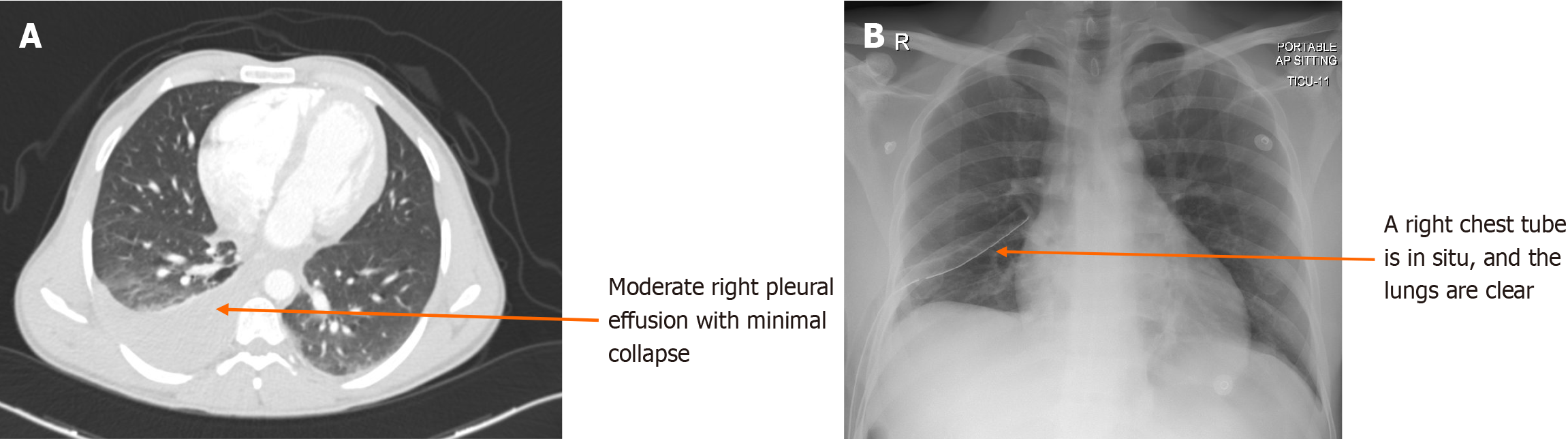
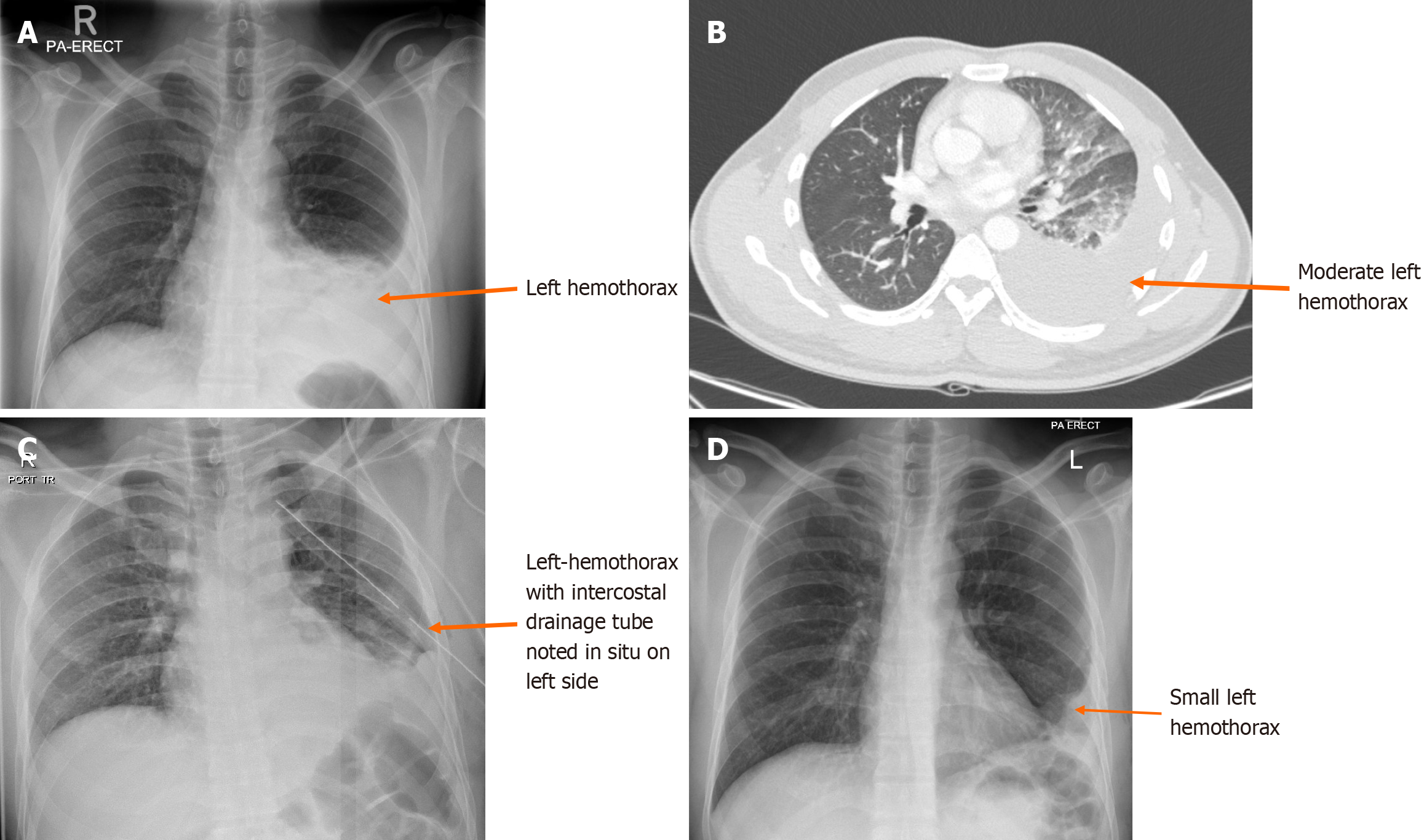
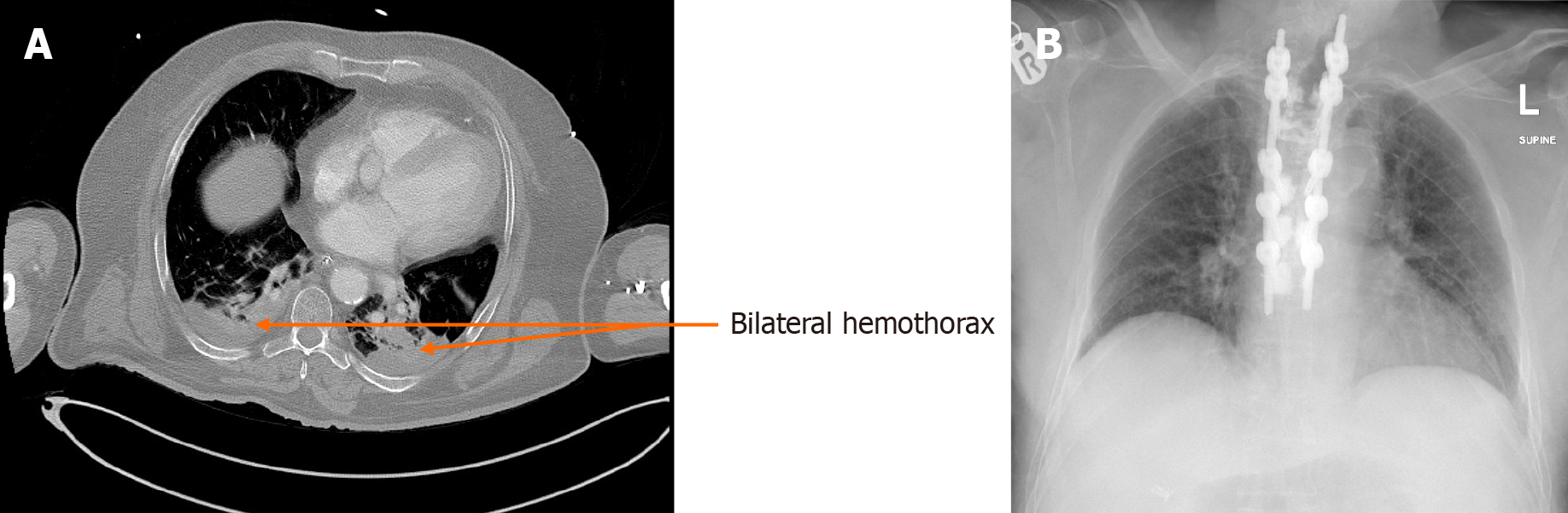
Of all the hemothorax cases, 57.82% were cleared within 0-3 days, and 18% required chest tubes. Results showed that 16.83% were cleared between 3-7 days, with 39.4% requiring chest tubes. Furthermore, 11.37% were cleared between 8-14 days, with 31.25% requiring chest tubes, while 13.98% persisted over 14 days, with 23.7% requiring chest tubes. Figures 2, 3 and 4 show examples of three cases of traumatic hemothorax.
A total of 152/439 traumatic hemothorax cases were identified. Three patients died within the first three days and were excluded from the study. In the surviving group, 64.4% of patients had pneumothorax, 43.6% had lung contusion, and 83.9% had rib fractures. A total of 105/149 (70.5%) hemothorax cases were cleared radiologically with a follow-up CT scan or chest X-ray between 0-3 days post-hospital admission. The median hemothorax size was 11 mm (range, 1-60 mm). While 17/105 (16.20 %) patients required a chest tube, the remaining patients were treated conservatively. Clearance without a chest tube occurred in 88/105 (83.80%) cases.
Of the remaining 44/149 (29.53%) cases, 19/149 (12.7%) were cleared radiologically within the 4th to 7th days post-trauma. The hemothoraces in this group were larger than those in the earlier group, with a median size of 17 mm (range: 2-60 mm). Moreover, CTI was required in 8/19 (42.10%) patients, while the remaining 11/19 (57.90%) patients did not receive CTI.
Right-sided hemothorax persisted in 25/149 (16.78 %) cases after 1 week, with only 14/149 (9.4%) cases resolved between 8 and 14 days. Furthermore, 3/14 (21.43%) cases required a CTI, and11/14 (78.57%) cases were cleared without it. The median size of the hemothorax in this group was 18 mm (2-60 mm). After 14 days, 11/149 (7.4%) patients with hemothorax persisted on imaging follow-up, and only 2/11 (18.2%) patients received CTI. Furthermore, 9/11 (81.8%) cases were subsequently cleared on the follow-up imaging scans.
In total, 160/439 cases of left-sided traumatic hemothorax were identified. Four patients died and were excluded from the study. In this group, 60.3% of patients had pneumothorax, 50% had lung contusion, and 85.3% had rib fractures. Of 156 cases, 79/156 (50.6%) were cleared radiologically between 0-3 days from hospital admission. The median hemothorax size was 11 mm (range, 1-55 mm). While 10/79 (12.66%) patients required a chest tube, the remaining patients were treated conservatively with no chest tube. Clearance without a chest tube was observed in 69/79 (87.34%) cases.
In the remaining 77/156 (49.0 %) cases, 31/156 (19.9 %) hemothoraces were cleared radiologically within day 4-7 days post-trauma. The hemothoraces in these cases were larger than those in the earlier group, with a median size of 17 mm (range, 1-55 mm). Furthermore, CTI was needed in 11/31 (35.48%) patients, while the remaining 20/31 (64.52%) patients did not receive chest tubes.
Left-sided hemothorax persisted in 46/156 (29.5%) cases after 1 week, and only 16/156 (10.3%) cases resolved between 8 and 14 days. Moreover, 7/16 (43.75%) cases required a chest tube, while 9/16 (56.25%) cases cleared the hemothorax without tubes. The median hemothorax size was 18 mm (1-55 mm). After 14 days, 30/156 (19.2%) cases persisted during follow-up, and only 5/30 (16.67%) cases were treated with CTI. Furthermore, 25/30 (83.33%) cases were cleared up on follow-up.
A total of 117/439 patients with bilateral traumatic hemothorax were identified. Ten patients died and were excluded from the study. Nearly all patients had severe polytrauma, which required the insertion of bilateral chest tubes. In this group, 65% of cases had pneumothorax, 51.3% had lung contusion, and 94% had rib fractures. Table 2 shows a com
| Hemothorax right (n = 149; 35.3) | Hemothorax left (n = 156; 37.0) | Bilateral hemothorax (n = 117; 27.7) | P value | |
| Chest injuries | ||||
| Pneumothorax | 96 (64.4) | 94 (60.3) | 76 (65.0) | 0.661 |
| Lung contusion | 65 (43.6) | 78 (50.0) | 60 (51.3) | 0.388 |
| Rib fracture | 125 (83.9) | 133 (85.3) | 110 (94.0) | 0.032 |
| Clearance by days | ||||
| 0-3 days | 105 (70.5) | 79 (50.6) | 60 (51.3) | 0.004 for all |
| > 3-7 days | 19 (12.7) | 31 (19.9) | 21 (17.9) | |
| > 7-14 days | 14 (9.4) | 16 (10.3) | 18 (15.4) | |
| > 14 days | 11 (7.4) | 30 (19.2) | 18 (15.4) | |
| Clearance with tube thoracostomy (chest tube) insertion | n = 30 (20.1) | n = 33 (21.2) | n = 38 (32.5) | |
| Chest tube 0-3 days | 17 (56.7) | 10 (30.3) | 17 (44.7) | 0.389 for all |
| Chest tube > 3-7 days | 8 (26.7) | 11 (33.3) | 9 (23.7) | |
| Chest tube > 7-14 days | 3 (10.0) | 7 (21.2) | 5 (13.2) | |
| > 14 days | 2 (6.7) | 5 (15.2) | 7 (18.4) | |
| Clearance without chest tube insertion | n = 119 (79.9) | n = 123 (78.8) | n = 79 (67.5) | |
| 0-3 days | 88 (73.9) | 69 (56.1) | 43 (54.4) | 0.007 for all |
| > 3-7 days | 11 (9.2) | 20 (16.3) | 12 (15.2) | |
| > 7-14 days | 11 (9.2) | 9 (7.3) | 13 (16.5) | |
| > 14 days | 9 (7.6) | 25 (20.3) | 11 (13.9) |
In the remaining 57/117 (48.7%) patients, 21/117 (17.9%) hemothoraces were cleared within 4-7 days post-trauma. The hemothoraces in these cases were larger, with a median size of 8 mm (2-53 mm) on the right side and 11 mm (2-37 mm) on the left side. A chest tube was inserted in 9/21 (42.85%) cases, while 12/21 (57.15%) patients did not undergo CTI.
Bilateral hemothorax persisted in 36/117 (30.76%) cases after 1 week, with 18/117(15.4%) resolved of hemothorax between days 8 and 14, 5/18 (27.78%) cases requiring CTI, and 13/18 (72.22%) cases cleared without CTI. The median hemothorax size was 8 mm (2-53 mm) on the right side and 10.5 mm (2-36 mm) on the left side.
After 14 days, 18/117 (15.4 %) cases with hemothorax persisted on follow-up, 7/18 (38.89%) were treated with CTI, and 11/18 (61.11%) cases were cleared on the follow-up imaging scans. Table 3 demonstrates the time to clearance of hemo
| Total clearance (n = 539) | Clearance with TT (n = 139) | Clearance without TT (n = 400) | P value | |
| Time of clearance | ||||
| Clearance 0-3 days | 304 (56.4) | 61 (43.9) | 243 (60.8) | 0.001 for all |
| Clearance 3-7 days | 92 (17.1) | 37 (26.6) | 55 (13.8) | |
| Clearance > 7-14 days | 66 (12.2) | 20 (14.4) | 46 (11.5) | |
| > 14 days | 77 (14.2) | 21 (15.1) | 56 (14.0) |
Hemothorax is characterized by the accumulation of blood in the pleural space or a pleural fluid hematocrit exceeding 50%[13]. In the context of evaluating thoracic injury in the ED, CXR has traditionally been used as the first-line diagnostic tool. However, for the assessment of traumatic hemothorax and the identification of additional injuries, chest CT has emerged as the preferred imaging modality, as approximately 14% of patients can be expected to have an occult hemo/pneumothorax found on CT after a normal CXR[3].
RH is defined as blood that occupies at least one-third of the pleural space and cannot be drained by thoracostomy within 72 hours or as clots of at least 500 mL in volume[14]. RH can develop as early as 24 hours after chest tube placement[15]. The incidence of RH is estimated to range from 5% to 30%, with a significant proportion of patients requiring surgical evacuation[16]. Although these RH may spontaneously reabsorb 4-6 weeks after trauma, excessive RH may lead to additional complications[15]. Reports show several risk factors for RH including a high chest AIS score, low hematocrit rate, initial hemothorax volume (with an increased risk of 15% every 100 mL/day of hemothorax), low Glasgow Coma Scale, number of chest tubes placed, and length of time with thoracostomy. The median reported size of hemothorax was 353 mL (233-397), and as described by Prakash et al[17], the development of an RH increased in moderate and large initial hemothorax with 44.3% and 39.1% RH risk rates, respectively. The mean age of the study cohort was approximately 38.5 years, which was consistent with previous findings[18].
In our study, hemothorax clearance was evaluated radiologically using CT or CXR. Each group was further stratified based on the time taken for radiological clearance within specific intervals following diagnosis and use of CTI. Earlier clearance was associated with smaller hemothorax sizes and lower chest tube requirements. Conversely, delayed hemothorax clearance or persistence was linked to larger hemothorax sizes and increased chest tube requirements.
The size of the hemothorax plays a crucial role in determining the appropriate management strategy, thus influencing the necessity of CTI[19]. Notably, in our study, the median hemothorax sizes for patients who cleared the condition within 72 h were the same on the right and left sides (11 mm), with a small bilateral decrease in hemothorax size (8-9 mm).
Our study revealed that the majority of hemothorax cases (58%) were resolved within the first 72 hours. Given the pivotal role of hemothorax size in decision-making regarding CTI, only 44/244 (18%) cases required early intervention in the form of CTI due to significant hemothorax size within three days of diagnosing traumatic hemothorax, and 82 % of patients cleared the hemothorax without the need for CTI. Hemothorax resolution is also influenced by various factors, including patient age, comorbidities, and associated injuries[20]. In our study, not all patients achieved hemothorax clea
As previously discussed, the size of the hemothorax is an important factor in resolution[20]. As the size increases, the chances of RH increase (17), which is consistent with our study where patients who did not clear their hemothorax within 3 days had a larger hemothorax (median size of 17 mm) as opposed to those who cleared in the first 72 hours (median size of 11 mm). In our study, 71/422 (16.83%) cases cleared the hemothorax between 4-7 days, resulting in approximately 74.65% of cases cleared by the end of the 1st week.
After 7 days, approximately 1/4 of all the patients (25.35%) failed to resolve on follow-up imaging despite appropriate management with either conservative treatment or with CTI. One of the reasons for the delayed resolution in these cases may be related to the fact that these patients were mostly polytrauma patients[21] with high ISS and Chest AIS scores, despite having nearly the same hemothorax sizes which resolved within a week.
This study also reported a higher prevalence of persistent hemothorax after 14 days (14%). Notably, it was more prevalent in patients with left-sided hemothorax (19.2%). This observation suggests a potential correlation between the persistence of hemothorax and the severity of associated injuries, particularly in the context of left-sided traumatic hemothorax. However, the available data are insufficient to conclusively support this hypothesis.
The criteria used for discharge of these patients included being clinically asymptomatic on room air, stable vital signs, and a last chest radiograph before discharge showing only minimal blunting of the CP angle (in case the hemothorax was not entirely resolved and still visible on imaging with no clinical signs or symptoms). Of note, our hospital has no strict protocol for follow-up of these patients. Nevertheless, these patients are generally administered on a case-by-case basis every 1-2 weeks until complete resolution of the hemothorax on outpatient visits.
None of these patients required additional intervention during this period, which is consistent with the findings of a follow-up hemothorax study[7] also showing no intervention during the follow-up of these patients.
This study had several limitations. Because of the small sample size, identifying significant predictors was challenging. Also, this was a retrospective study and data collection was limited to the amount of information available on patient charts. Therefore, many aspects could not be explained based on the available information. The decision to insert a chest tube was mainly clinical; however, based on clinical judgment, a chest tube was inserted in all patients who required it. Moreover, we do not have an explanation for why a subset of hemothoraces did not resolve and persisted beyond 14 days.
Finally, the monocentric nature of this study should be considered, and our results should be confirmed by further multicenter studies conducted on larger populations.
Patients with RH were discharged based on clinical assessment (i.e., asymptomatic, maintaining saturation on room air, good incentive, and satisfactory radiography before discharge, including minimal hemothorax, not warranting drainage). Follow-ups were performed weekly after discharge, especially in the first two weeks. Subsequently, follow-ups continued at the clinician’s discretion and judgment. We did not report any complications in patients discharged with a returned hemothorax (i.e., symptomatic presentation or requirement for hemothorax drainage).
RH persisted in a subset of patients, despite early CTI intervention. Our findings showed that patients with large hemothoraces tended to experience prolonged left-sided as opposed to right-sided hemothoraces. We recommend regular imaging, such as CXR or CT, for up to 14 days (2 weeks) postintervention to monitor patients. After this period, out
The authors thank the Medical Research Center and the Qatar National Trauma Registry at HMC, Qatar.
| 1. | Chardoli M, Hasan-Ghaliaee T, Akbari H, Rahimi-Movaghar V. Accuracy of chest radiography versus chest computed tomography in hemodynamically stable patients with blunt chest trauma. Chin J Traumatol. 2013;16:351-354. [PubMed] |
| 2. | Calderon G, Perez D, Fortman J, Kea B, Rodriguez RM. Provider perceptions concerning use of chest x-ray studies in adult blunt trauma assessments. J Emerg Med. 2012;43:568-574. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 3. | Plurad D, Green D, Demetriades D, Rhee P. The increasing use of chest computed tomography for trauma: is it being overutilized? J Trauma. 2007;62:631-635. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 58] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 4. | Chrysou K, Halat G, Hoksch B, Schmid RA, Kocher GJ. Lessons from a large trauma center: impact of blunt chest trauma in polytrauma patients-still a relevant problem? Scand J Trauma Resusc Emerg Med. 2017;25:42. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 60] [Cited by in RCA: 104] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 5. | Mowery NT, Gunter OL, Collier BR, Diaz JJ Jr, Haut E, Hildreth A, Holevar M, Mayberry J, Streib E. Practice management guidelines for management of hemothorax and occult pneumothorax. J Trauma. 2011;70:510-518. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 115] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 6. | DuBose J, Inaba K, Okoye O, Demetriades D, Scalea T, O'Connor J, Menaker J, Morales C, Shiflett T, Brown C, Copwood B; AAST Retained Hemothorax Study Group. Development of posttraumatic empyema in patients with retained hemothorax: results of a prospective, observational AAST study. J Trauma Acute Care Surg. 2012;73:752-757. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 74] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 7. | Golden P. Follow-up chest radiographs after traumatic pneumothorax or hemothorax in the outpatient setting: a retrospective review. Int J Trauma Nurs. 1999;5:88-94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 8. | Misthos P, Kakaris S, Sepsas E, Athanassiadi K, Skottis I. A prospective analysis of occult pneumothorax, delayed pneumothorax and delayed hemothorax after minor blunt thoracic trauma. Eur J Cardiothorac Surg. 2004;25:859-864. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 62] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 9. | DuBose J, Inaba K, Demetriades D, Scalea TM, O'Connor J, Menaker J, Morales C, Konstantinidis A, Shiflett A, Copwood B; AAST Retained Hemothorax Study Group. Management of post-traumatic retained hemothorax: a prospective, observational, multicenter AAST study. J Trauma Acute Care Surg. 2012;72:11-22; discussion 22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 92] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 10. | Plourde M, Émond M, Lavoie A, Guimont C, Le Sage N, Chauny JM, Bergeron É, Vanier L, Moore L, Allain-Boulé N, Fratu RF, Dufresne M. [Cohort study on the prevalence and risk factors of late pulmonary complications in adults following a closed minor chest trauma]. CJEM. 2013;15:337-344. [PubMed] |
| 11. | Morrison CA, Lee TC, Wall MJ Jr, Carrick MM. Use of a trauma service clinical pathway to improve patient outcomes for retained traumatic hemothorax. World J Surg. 2009;33:1851-1856. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 28] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 12. | Smith JW, Franklin GA, Harbrecht BG, Richardson JD. Early VATS for blunt chest trauma: a management technique underutilized by acute care surgeons. J Trauma. 2011;71:102-5; discussion 105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 52] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 13. | O׳Keeffe M, Clark S, Khosa F, Mohammed MF, McLaughlin PD, Nicolaou S. Imaging Protocols for Trauma Patients: Trauma Series, Extended Focused Assessment With Sonography for Trauma, and Selective and Whole-body Computed Tomography. Semin Roentgenol. 2016;51:130-142. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 16] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 14. | Carrillo EH, Richardson JD. Thoracoscopy in the management of hemothorax and retained blood after trauma. Curr Opin Pulm Med. 1998;4:243-246. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 27] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 15. | Chou YP, Lin HL, Wu TC. Video-assisted thoracoscopic surgery for retained hemothorax in blunt chest trauma. Curr Opin Pulm Med. 2015;21:393-398. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 33] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 16. | Morales Uribe CH, Villegas Lanau MI, Petro Sánchez RD. Best timing for thoracoscopic evacuation of retained post-traumatic hemothorax. Surg Endosc. 2008;22:91-95. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 39] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 17. | Prakash PS, Moore SA, Rezende-Neto JB, Trpcic S, Dunn JA, Smoot B, Jenkins DH, Cardenas T, Mukherjee K, Farnsworth J, Wild J, Young K, Schroeppel TJ, Coimbra R, Lee J, Skarupa DJ, Sabra MJ, Carrick MM, Moore FO, Ward J, Geng T, Lapham D, Piccinini A, Inaba K, Dodgion C, Gooley B, Schwartz T, Shraga S, Haan JM, Lightwine K, Burris J, Agrawal V, Seamon MJ, Cannon JW. Predictors of retained hemothorax in trauma: Results of an Eastern Association for the Surgery of Trauma multi-institutional trial. J Trauma Acute Care Surg. 2020;89:679-685. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 27] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 18. | El-Menyar A, Abdelrahman H, Al-Hassani A, Ellabib M, Asim M, Zarour A, Al-Thani H. Clinical Presentation and Time-Based Mortality in Patients With Chest Injuries Associated With Road Traffic Accidents. Arch Trauma Res. 2016;5:e31888. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 11] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 19. | Wells BJ, Roberts DJ, Grondin S, Navsaria PH, Kirkpatrick AW, Dunham MB, Ball CG. To drain or not to drain? Predictors of tube thoracostomy insertion and outcomes associated with drainage of traumatic hemothoraces. Injury. 2015;46:1743-1748. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 26] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 20. | Hanafi M, Al-Sarraf N, Sharaf H, Abdelaziz A. Pattern and presentation of blunt chest trauma among different age groups. Asian Cardiovasc Thorac Ann. 2011;19:48-51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 21. | Scott MF, Khodaverdian RA, Shaheen JL, Ney AL, Nygaard RM. Predictors of retained hemothorax after trauma and impact on patient outcomes. Eur J Trauma Emerg Surg. 2017;43:179-184. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/