Published online Feb 28, 2025. doi: 10.4329/wjr.v17.i2.101932
Revised: December 16, 2024
Accepted: January 23, 2025
Published online: February 28, 2025
Processing time: 147 Days and 20.7 Hours
Liver cirrhosis patients can develop various complications including bacteremia as the intestinal flora is heterologous. In those with low immunity, trauma, or following surgery, etc., the body is susceptible to concurrent systemic or local in
A male patient with decompensated cirrhosis experienced multiple episodes of gastrointestinal bleeding and hypersplenism. He was admitted to hospital due to voluntary remedial TIPS. The patient developed a numerous intrahepatic liver abscess postoperatively. Following initial conservative treatment with intra
Attention should be paid to decreased blood cell counts, especially low leukocyte levels in patients with liver cirrhosis as the presence of intestinal microbiota dysregulation and portal pyemia can result in liver abscess and sepsis during invasive diagnostic and therapeutic procedures like TIPS. The addition of pro
Core Tip: Transjugular intrahepatic portosystemic shunt (TIPS) is currently used for the treatment of portal hypertension and its complications though numerous liver abscesses induced by such interventional minimally invasive treatment is uncom
- Citation: Luo SH, Wang ZH, Chen J, Chen JY. Numerous liver abscesses after transjugular intrahepatic portosystemic shunt for decompensated liver cirrhosis: A case report. World J Radiol 2025; 17(2): 101932
- URL: https://www.wjgnet.com/1949-8470/full/v17/i2/101932.htm
- DOI: https://dx.doi.org/10.4329/wjr.v17.i2.101932
Patients with decompensated cirrhosis frequently have splenomegaly and hypersplenism, presenting with low white blood cell, red blood cell and platelet counts[1]. In particular, patients with a low white blood cell count are prone to develop concurrent abdominal infections, peritonitis, and other infections. Intestinal dysbiosis and inflammation in cirrhosis can also cause bacteremia leading to portal pyemia[2]. Even minimally invasive treatment methods for patients with liver cirrhosis can also be complicated by infectious lesions in various organs[3]. However, numerous liver abscesses induced by interventional minimally invasive treatment are uncommon.
Transjugular intrahepatic portosystemic shunt (TIPS) is currently used for the treatment of portal hypertension and its complications, such as variceal bleeding and refractory ascites, and achieves good clinical results[4]. Here, we report TIPS in a patient with decompensated cirrhosis, who developed numerous hepatic abscesses postoperatively. Following prolonged conservative treatment with intravenous antibiotics and supportive therapy, the liver abscesses disappeared, and the patient recovered fully.
A 47-year-old male patient who was admitted to our hospital for voluntary remedial TIPS for the management of decompensated liver cirrhosis. He presented without any gastrointestinal bleeding symptoms and was promptly assessed. A timely endoscopic examination was performed, and acid suppression was initiated.
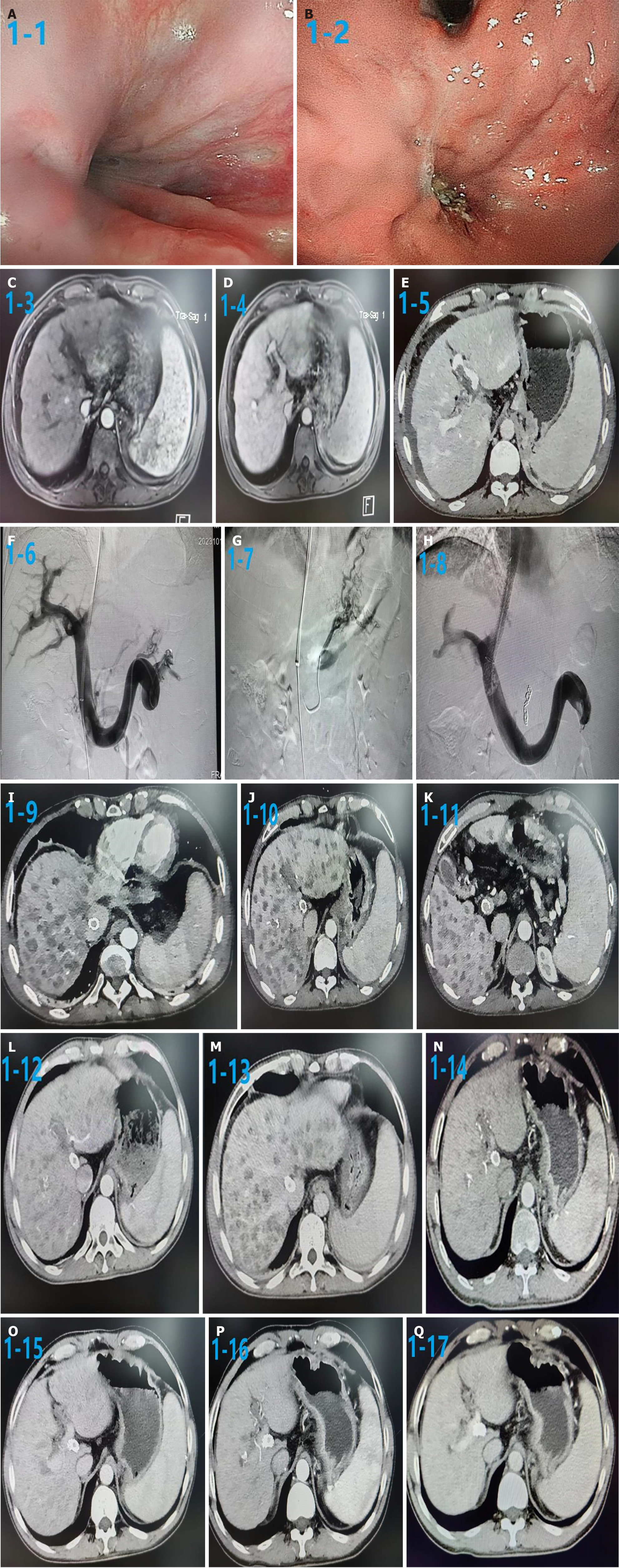
Gastroscopy revealed esophageal-gastric varices, no visible bleeding but an ulcer scar was identified in the varicose veins at the base of the stomach. Abdominal computed tomography (CT) revealed liver cirrhosis and esophageal-gastric varices, splenomegaly, and a small amount of ascites.
Gastrointestinal bleeding in this patient was treated with medication, multiple endoscopic bands and sclerotherapy over the past three years.
The patient has no relatives with similar illnesses or any family history of cirrhosis.
The patient presents with facial features of chronic liver disease and anemia. Examination of the heart and lungs were unremarkable, and the abdomen was flat and soft. The liver was not palpable and the spleen was palpable subcostally (three finger breadths). There was no edema in the lower limbs.
Laboratory tests showed that he had low white blood cell, red blood cell and platelet counts (Table 1).
| Characteristics | Pre-TIPS | Three days post-TIPS |
| Viral hepatitis | B | B |
| Child–Pugh A/B/C | A | B |
| MELD score | 6 | 15 |
| Laboratory tests | ||
| Alanine transaminase (U/L) | 22 | 1531 |
| Aspartate transaminase (U/L) | 39 | 1776 |
| Alkaline phosphatase (U/L) | 93 | 140 |
| Total bilirubin (mol/L) | 8.7 | 26.1 |
| Albumin (g/L) | 35.9 | 26.3 |
| Prothrombin time (s) | 14.0 | 21.5 |
| White cell count (109/L) | 1.70 | 3.50 |
| Red cell count (1012/L) | 4.01 | 2.78 |
| Hemoglobin (g/L) | 106 | 73 |
| Platelet count (109/L) | 58 | 54 |
| Clinical presentation | ||
| Jaundice | No | No |
| Splenomegaly | Large | Large |
| Lower limb edema | No | No |
| Ascites | Moderate | No |
| Pleural fluid | No | No |
| Varices | Moderate | Moderate |
This patient underwent gastroscopy examination that revealed esophageal-gastric varices, no visible bleeding but there was an ulcer scar in the varicose veins at the base of the stomach. Abdominal magnetic resonance imaging and CT portal venous phase showed cirrhosis, splenomegaly, and left portal vein thrombosis in the liver. After 3 days of TIPS, abdominal CT showed multiple small abscesses in the liver. After 45 days, liver CT showed multiple small abscesses, with a significant reduction in number. After 60 days, abdominal CT arterial and venous phases showed that the intrahepatic abscesses had disappeared and the TIPS shunt was patent (Figure 1).
The patient was diagnosed with decompensation of cirrhosis and gastrointestinal bleeding.
Following prompt administration of antibiotic medications, the patient was generally stable. Comprehensive evaluation of liver function showed Child-Pugh class B, and the Model for End-stage Liver Disease score was 9. According to current guidelines, the patient was treated with TIPS for managing portal hypertension. TIPS was performed under local anesthesia as previously described[5]. The RUPS-100 puncture system was introduced into the right hepatic vein, and successfully punctured to the left branch of the intrahepatic portal vein. All varicose veins were embolized with coils, and the intrahepatic puncture tract was dilated with a balloon. A covered stent (Viatorr; 8 ´ 60 ´ 20 mm) was implanted in the shunt tract. After stent implantation, follow-up portal angiography showed good intrahepatic portal venous perfusion, and the portal gradient was reduced to less than 12 mmHg. Two distinct gastroesophageal collateral vessels observed during TIPS were coiled (Cook Inc., Bloomington, IL, United States) Subsequently, direct angiography was performed to assess whether the portal system was completely patent.
After the TIPS procedure, intravenous heparin (4000 U/day; Sanofi Pharma Co., Ltd., France) was administered for 3 days. Oral warfarin was not administered due to low platelet count.
TIPS decreased the portosystemic gradient from 40 to 12 mmHg. There were no intraoperative bleeding procedure-associated complications. There were no symptoms of recurrent gastrointestinal bleeding after TIPS and the hemostasis rate was 100%.
Three days after TIPS, the patient presented with fever and cough, and laboratory tests showed that he had lower white blood cell and platelet counts than pre-TIPS. Chest and abdominal CT revealed no other infectious lesions, but ultrasound and abdominal CT showed multiple small abscesses in the liver.
Due to the small size of these abscesses, transhepatic puncture biopsy was unsuitable, and incubation of bacteria in multiple blood cultures failed. Sulperazon (Cefoperazone + Sulbactam) was administered pre-TIPS, the patient then underwent conservative treatment with intravenous Tienam (Imipenem + Cilastatin sodium), parenteral nutrition, infusion of plasma, and infusion of coagulation factors periodically. After three days, fever and cough symptoms had disappeared, and did not recur. Thereafter, there was a consistent pattern of weakness, lassitude, and intermittent lower limb edema without ascites.
A CT of the upper abdomen one and a half months later revealed small, sparse foci of abscess in the liver. At 2 months postoperatively, outpatient re-examination of the abdominal CT showed that the liver abscesses had disappeared, and his general condition had improved. Transient minor hepatic encephalopathy occurred one month postoperatively, and the symptoms disappeared after oral administration of ornithine aspartate. At an outpatient follow-up visit, the patient’s overall condition was good.
We report a patient with decompensated cirrhosis and recurrent gastrointestinal bleeding who underwent TIPS placement and subsequently developed numerous liver abscesses. The patient was treated with antibiotic therapy, supportive care and subsequently recovered.
Comlpications of TIPS included TIPS procedure itself, the stent, portosystemic shunting, and so on[6]. These complications are rare and can include arrhythmias, hemoperitoneum, liver capsule rupture, stent migration, kinking, hemolytic anemia, hepatic ischemia, and infarction which compromise liver function and are also recognized[7].
However, cases of numerous hepatic abscesses after TIPS are rare. The patient in this study who had decompensated cirrhosis and recurrent gastrointestinal bleeding developed numerous hepatic abscesses after the TIPS procedure. Chest and abdominal CT revealed no other infectious lesions, but numerous small abscesses were identified in the liver. With nearly three months of antibiotic therapy and supportive care, the patient recovered, and this experience has provided some important lessons.
Cirrhosis is a well-known pro-inflammatory state, and it has been shown that in patients with cirrhosis, intestinal microflora imbalance (increased number of Enterobacter species, decreased number of Clostridium species) and displacement may promote the inflammatory reaction[8]. Thus, in this circumstance, the patient is prone to local or systemic infection. Interventional therapy such as minimally invasive treatment methods for patients with liver cirrhosis can also result in complications such as infectious lesions[9], and TIPS, which involves surgery, alters the hemodynamics of the liver and portal venous system and has been implicated in a catastrophic hepatic complication in our case.
This patient had cirrhosis, splenomegaly and hypersplenism with low preoperative blood cell levels, especially leukocytes before TIPS placement. After the TIPS procedure, the white blood cell count was lower, but we did not find any symptoms of rebleeding. We also reviewed the gastroscopy results and did not find any signs of rebleeding. This may have been due to factors such as sepsis which caused the decreased hemoglobin level. We only focused on the patient's postoperative recurrent gastrointestinal bleeding and reviewed the gastroscopy, but did not focus on the low level of white blood cells and hemoglobin, and whether this was due to infection.
The intestinal flora is dysregulated in cirrhosis, and often displaced[10]. TIPS, which aggravates dysregulation of the intestinal flora, particularly by the opening of the hepatic shunt, may also aggravate the displacement of harmful flora in the intestine[11]. In addition, reduced white blood cells in hypersplenism and lower immune function in cirrhosis could have led onto the development of extensive hepatic abscesses.
In this patient, a transhepatic biopsy of the intrahepatic lesion was not performed, and the causative agent was not identified following blood culture. Due to the small size of the intrahepatic abscesses and the concerns regarding the possibility of additional infection resulting from the needle biopsy, we decided to treat the patient with intravenous Tienam empirically with an improvement of his condition.
This case highlights the importance of considering serious infections including liver abscess in patients with cirrhosis following invasive treatments including TIPS. Preoperatively, attention should be paid to decreased blood cell counts, especially low leukocyte levels. In addition, the presence of intestinal microbiota dysregulation and displacement should be considered, and whether to add probiotics has become a topic of discussion for such patients.
The authors would like to thank the patients who participated in this study as well as their colleagues at our hospital for their contribution in the data collection process.
| 1. | Lu H, Zheng C, Xiong B, Xia X. Efficacy and safety of heparin plus dexamethasone after partial splenic embolization for liver cirrhosis with massive splenomegaly. BMC Gastroenterol. 2022;22:470. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 2. | Wang J, Wu S, Zhang Y, Yang J, Hu Z. Gut microbiota and calcium balance. Front Microbiol. 2022;13:1033933. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 29] [Reference Citation Analysis (0)] |
| 3. | Halpenny DF, Torreggiani WC. The infectious complications of interventional radiology based procedures in gastroenterology and hepatology. J Gastrointestin Liver Dis. 2011;20:71-75. [PubMed] |
| 4. | Larrue H, D'Amico G, Olivas P, Lv Y, Bucsics T, Rudler M, Sauerbruch T, Hernandez-Gea V, Han G, Reiberger T, Thabut D, Vinel JP, Péron JM, García-Pagán JC, Bureau C. TIPS prevents further decompensation and improves survival in patients with cirrhosis and portal hypertension in an individual patient data meta-analysis. J Hepatol. 2023;79:692-703. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 68] [Article Influence: 22.7] [Reference Citation Analysis (1)] |
| 5. | Luo SH, Zhou MM, Cai MJ, Han SL, Zhang XQ, Chu JG. Reduction of portosystemic gradient during transjugular intrahepatic portosystemic shunt achieves good outcome and reduces complications. World J Gastroenterol. 2023;29:2336-2348. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 6. | Khan A, Maheshwari S, Gupta K, Naseem K, Chowdry M, Singh S. Rate, reasons, predictors, and burden of readmissions after transjugular intrahepatic portosystemic shunt placement. J Gastroenterol Hepatol. 2021;36:775-781. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 15] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 7. | Horhat A, Bureau C, Thabut D, Rudler M. Transjugular intrahepatic portosystemic shunt in patients with cirrhosis: Indications and posttransjugular intrahepatic portosystemic shunt complications in 2020. United European Gastroenterol J. 2021;9:203-208. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 29] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 8. | Nie Y, Liu Q, Zhang W, Wan Y, Huang C, Zhu X. Ursolic acid reverses liver fibrosis by inhibiting NOX4/NLRP3 inflammasome pathways and bacterial dysbiosis. Gut Microbes. 2021;13:1972746. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 66] [Article Influence: 13.2] [Reference Citation Analysis (0)] |
| 9. | Obri MS, Kamran W, Almajed MR, Eid D, Venkat D. Splenic Artery Embolism in Liver Transplant Patients: A Single-Center Experience. Cureus. 2023;15:e38599. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 10. | Trebicka J, Macnaughtan J, Schnabl B, Shawcross DL, Bajaj JS. The microbiota in cirrhosis and its role in hepatic decompensation. J Hepatol. 2021;75 Suppl 1:S67-S81. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 179] [Article Influence: 35.8] [Reference Citation Analysis (0)] |
| 11. | Gitto S, Vizzutti F, Baldi S, Campani C, Navari N, Falcini M, Venturi G, Montanari S, Roccarina D, Arena U, Pallecchi M, Di Bonaventura C, Bartolucci G, Ramazzotti M, Citone M, Fanelli F, Amedei A, Marra F. Transjugular intrahepatic Porto-systemic shunt positively influences the composition and metabolic functions of the gut microbiota in cirrhotic patients. Dig Liver Dis. 2023;55:622-628. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 8] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/