Published online Jan 28, 2025. doi: 10.4329/wjr.v17.i1.103111
Revised: December 24, 2024
Accepted: January 17, 2025
Published online: January 28, 2025
Processing time: 69 Days and 1.3 Hours
The incidence of multiple pregnancies has increased worldwide recently and women with a twin pregnancy are at higher risk of adverse outcomes compared with women with a singleton pregnancy. It is important to understand the risk factors for adverse fetal outcomes in twin pregnancy in order to guide clinical management.
To identify the independent risk factors, including maternal personal and family medical histories and first trimester ultrasound screening findings, for adverse fetal outcomes of twin pregnancy before 28 weeks of gestation.
The data of 126 twin pregnancies in our hospital, including pregnancy outcomes, first trimester ultrasound screening findings and maternal medical history, were retrospectively collected. Twenty-nine women with adverse outcomes were included in the abnormal group and the remaining 97 women were included in the control group.
Patients in the abnormal group were more likely to be monochorionic diamniotic (13/29 vs 20/97, P= 0.009), with a higher mean pulsatility index (PI, 1.57 ± 0.55 vs 1.28 ± 0.42, P = 0.003; cutoff value: 1.393) or a higher mean resistance index (0.71 ± 0.11 vs 0.65 ± 0.11, P = 0.008; cutoff value: 0.683) or early diastolic notch of bilateral uterine arteries (UtAs, 10/29 vs 15/97, P = 0.024) or with abnormal ultrasound findings (13/29 vs 2/97, P < 0.001), compared with the control group. Monocho
First trimester ultrasound screening for twin pregnancy identifies independent risk factors and is useful for the prediction of fetal outcomes.
Core Tip: Recently, the incidence of twin pregnancy has increased worldwide. Understanding the risk factors for adverse fetal outcomes in twin pregnancy would be helpful for clinical management. We retrospectively analyzed the data of 126 twin pregnancies in the first trimester, including first trimester ultrasound screening findings. Our results showed that monochorionic diamnioticity, higher mean pulsatility index of bilateral uterine arteries and abnormal ultrasound findings during first trimester screening were independent risk factors for adverse fetal outcomes. First trimester ultrasound screening in twin pregnancy is useful for predicting fetal outcomes.
- Citation: Zhang HP, Bao L, Wu JJ, Zhou YQ. Independent risk factors for twin pregnancy adverse fetal outcomes before 28 gestational week by first trimester ultrasound screening. World J Radiol 2025; 17(1): 103111
- URL: https://www.wjgnet.com/1949-8470/full/v17/i1/103111.htm
- DOI: https://dx.doi.org/10.4329/wjr.v17.i1.103111
The incidence of multiple pregnancy has recently increased worldwide with a reported twin birth rate of 3.21% in the United States and 3.69% in China in 2019[1,2]. Women with a twin pregnancy are at higher risk of adverse outcomes compared to women with a singleton pregnancy, including miscarriage, congenital abnormalities, intrauterine fetal death, hypertension disorders, preterm delivery, etc.[3-5].
It is important to understand the risk factors for adverse fetal outcomes in twin pregnancies in order to guide clinical management. However, the risk factors for adverse outcomes in twin pregnancies are still unclear. Clinical guidance for twin pregnancy is usually based on studies related to singleton pregnancy. The probable risk factors reported include chorionicity, maternal age, body mass index (BMI), smoking, use of assisted conception, gestational diabetes, and hypertensive disorders of pregnancy[6-8]. Also, crown-rump length (CRL) discordance at 11-13 weeks gestation is considered to be associated with adverse outcomes, but its value has not been confirmed[2,9,10]. Higher pulsatility index (PI) and resistance index (RI) of the uterine artery (UtA) in the first trimester are considered to be related to a higher risk of pregnancy losses in singleton pregnancy[11]. However, the role of UtA parameters for adverse outcomes in twin pregnancy is still unknown.
In this study, we retrospectively analyzed maternal personal and family medical history, first trimester ultrasound screening results and pregnancy outcomes in twin pregnancies before 28 weeks of gestation. Our aim was to explore the independent risk factors for adverse fetal outcomes in twin pregnancies before 28 weeks of gestation.
This was a retrospective study and was approved by the Ethics Committee of our hospital (No. CNFBLLKTY-IEC-2023-023). Written informed consent was obtained from each patient before ultrasound examination.
We retrospectively collected the data of women with twin pregnancies at outpatient department of our hospital from January 2019 to December 2022. Inclusion criteria were: (1) Confirmed twin pregnancy before 10 weeks gestation with two heart beats using transvaginal ultrasound; (2) Prenatal ultrasound screening performed at 11-13 weeks gestation including fetal biometry, assessment of fetal anatomy and detection of double uterine arteries; and (3) Complete data on pregnancy outcome, personal history and family history. Exclusion criteria were: (1) Induced abortion for non-medical reasons; and (2) Intrauterine fetal death of one or both twins after 28 weeks of gestation.
The participants with adverse pregnancy outcomes before 28 weeks of gestation including one or both intrauterine fetal death, spontaneous abortion, induced abortion for fetal anomaly and selective fetal reduction for fetal anomaly were assigned to the abnormal group. The participants who had two live births after 28 weeks of gestation were assigned to the control group.
Height and weight of the participants before pregnancy were recorded in order to calculate BMI (kg/m2) = weight/hei
Prenatal ultrasound screening at 11-13 weeks of gestation followed the practice guideline of the International Society of Ultrasound in Obstetrics and Gynecology (ISUOG)[12-14]. All the examinations were performed by radiologists with a certificate of competence for the 11-13 week scan offered by the Fetal Medicine Foundation using a VolusonTM E8 diagnostic ultrasound system (GE HealthCare) and a transabdominal C4-8 probe. Twin chorionicity and amnionicity were determined using ultrasound following the ISUOG practice guideline. The parameters of bilateral UtAs including PI, RI and notch were measured and recorded. The mean PI and mean RI were calculated. CRL discordance was defined as (CRLlarge - CRLsmall)/CRLlarge ≥ 10%[15]. Nuchal translucency (NT) ≥ 3.0 mm was considered abnormal. Any fetal structural anomalies were observed and recorded.
SPSS version 24.0 software (IBM Corporation, Chicago, IL, United States) was used for statistical analysis. P < 0.05 was considered statistically significant. Numerical variables are presented as mean ± standard error and the independent sample t-test was used for the comparisons if they showed normal distribution (using the Kolmogorov-Smirnov test). The cut-off points for PI and RI were calculated by a receiver operating characteristic (ROC) curve. Enumeration data are presented as a number (percentile) and compared in the two groups using the χ2 test. Bivariate logistic regression analysis was performed to determine independent risk factors for abnormal pregnancy outcome.
One hundred and twenty-eight twin pregnancies were included in this study. One was excluded as one fetus died in utero at 30 weeks of gestation; another was excluded because of induced abortion for non-medical reasons at 15 weeks of gestation.
In total, 126 twin pregnancies were included in the study; 29 in the abnormal group and 97 in the control group. Pregnancy outcomes in the abnormal group are shown in Table 1.
| Pregnancy outcomes | n |
| One of the twins died in utero | 9 |
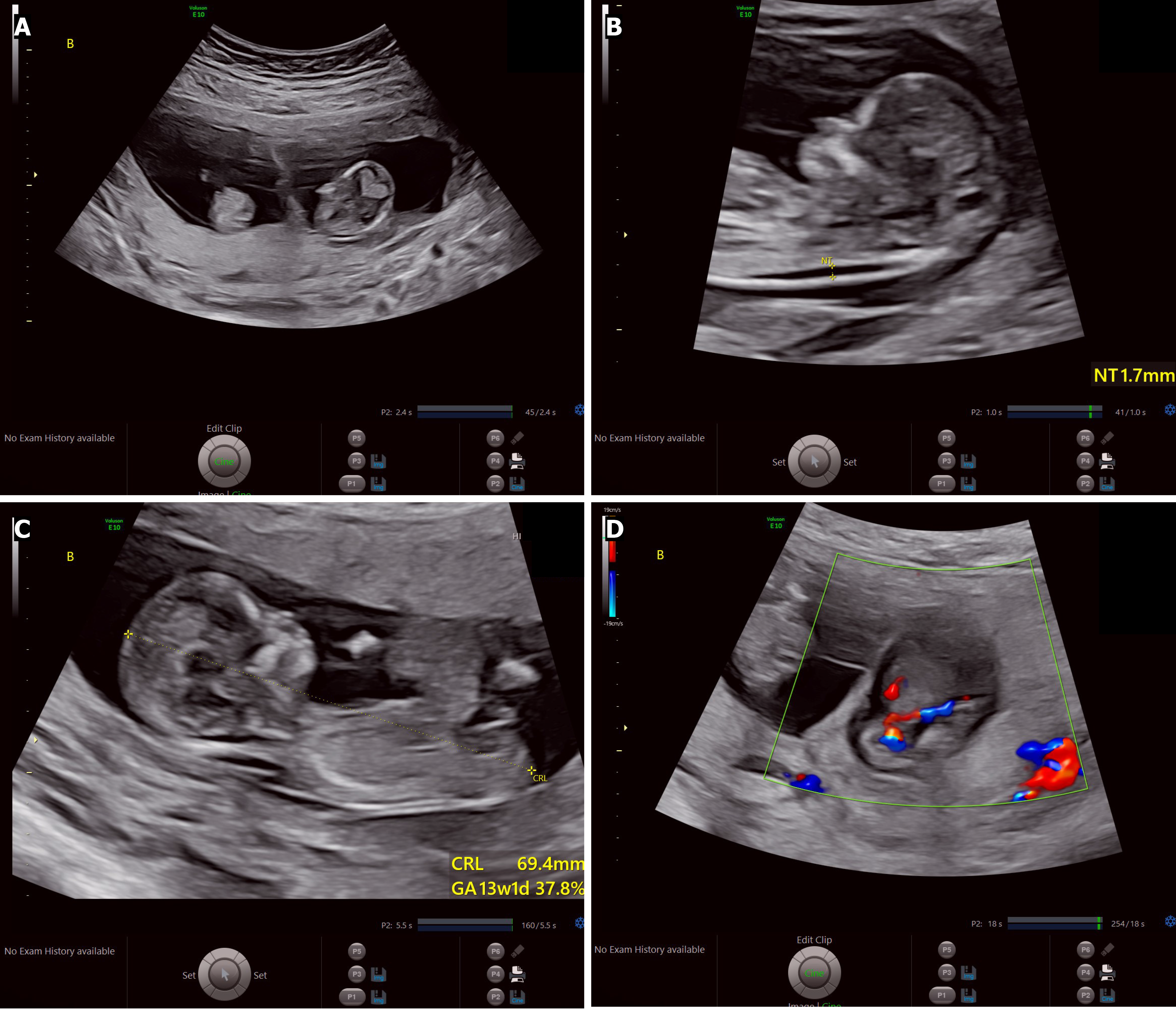
| Selective fetal reduction, for one fetus with omphalocele (Figure 1) | 1 |
| Both of the twins died in utero | 1 |
| Spontaneous abortion | 14 |
| Induced abortion for fetal anomaly | 4 |
Abnormal ultrasound findings in the first trimester screening are shown in Table 2 and Figure 1.
| Abnormal group | Control group |
| Seven cases of one intrauterine fetal death | One case with one fetus showing NT ≥ 3.0 mm |
| One case of twin reversed arterial perfusion sequence | One case with both fetuses showing NT ≥ 3.0 mm |
| One case of one fetus with omphalocele | |
| One case of one fetus with gastroschisis | |
| One case of one fetus with hydrops fetalis | |
| One case of one fetus with NT ≥ 3.0 mm | |
| One case of one intrauterine fetal death and the other with NT ≥ 3.0 mm |
None of the women in both groups were smokers or had a history of pre-eclampsia, diabetes or systemic lupus erythematosus. Only 1 patient in the control group had a history of hypertension.
Personal history and first trimester screening findings between the abnormal group and the control group are shown in Table 3. The mean PI of bilateral UtAs and mean RI of bilateral UtAs in the abnormal group were significantly higher than those in the control group. The patients in the abnormal group were more likely to be monochorionic diamniotic, with early diastolic notch in bilateral UtAs or abnormal ultrasound findings in the first trimester screening, compared with patients in the control group.
| Characteristics | Abnormal group (n = 29) | Control group (n = 97) | P value |
| Maternal age (years) | 32.39 ± 3.65 | 31.62 ± 4.07 | 0.333 |
| Maternal age (≥ 35 years) | 6 (20.69) | 28 (28.87) | 0.384 |
| Assisted conception | 11 (37.93) | 46 (47.42) | 0.368 |
| Systolic blood pressure | 113.17 ± 9.74 | 111.24 ± 9.77 | 0.351 |
| Diastolic blood pressure | 73.00 ± 7.40 | 71.82 ± 8.01 | 0.482 |
| Mean arterial pressure | 86.39 ± 7.59 | 84.96 ± 7.74 | 0.383 |
| High blood pressure | 3 (10.34) | 8 (8.25) | 0.714 |
| BMI (kg/m2) | 22.42 ± 3.40 | 22.21 ± 3.13 | 0.753 |
| BMI ≥ 24 kg/m2 | 6 (20.69) | 30 (30.93) | 0.284 |
| BMI ≥ 30 kg/m2 | 1 (3.44) | 2 (2.06) | 0.547 |
| History of hysteroscopy | 8 (27.59) | 29 (29.90) | 0.811 |
| History of anti-phospholipid syndrome | 2 (6.90) | 2 (2.06) | 0.333 |
| Family history of high blood pressure | 6 (20.69) | 30 (30.93) | 0.284 |
| Nulliparous | 16 (55.17) | 47 (48.45) | 0.525 |
| Chorionicity | 0.009 | ||
| Dichorionic diamniotic | 16 (55.17) | 77 (79.38) | |
| Monochorionic diamniotic | 13 (44.83) | 20 (20.62) | |
| Mean PI of bilateral uterine arteries | 1.57 ± 0.55 | 1.28 ± 0.42 | 0.003 |
| Mean RI of bilateral uterine arteries | 0.71 ± 0.11 | 0.65 ± 0.11 | 0.008 |
| Early diastolic notch in bilateral uterine arteries | 10 (34.48) | 15 (15.46) | 0.024 |
| Early diastolic notch in at least one uterine artery | 15 (51.72) | 39 (40.21) | 0.271 |
| Abnormal ultrasound findings during first trimester screening | 13 (44.83) | 2 (2.06) | < 0.001 |
| Crown-rump length discordance ≥ 10% | 3 (3/20, 15) | 6 (6.19) | 0.181 |
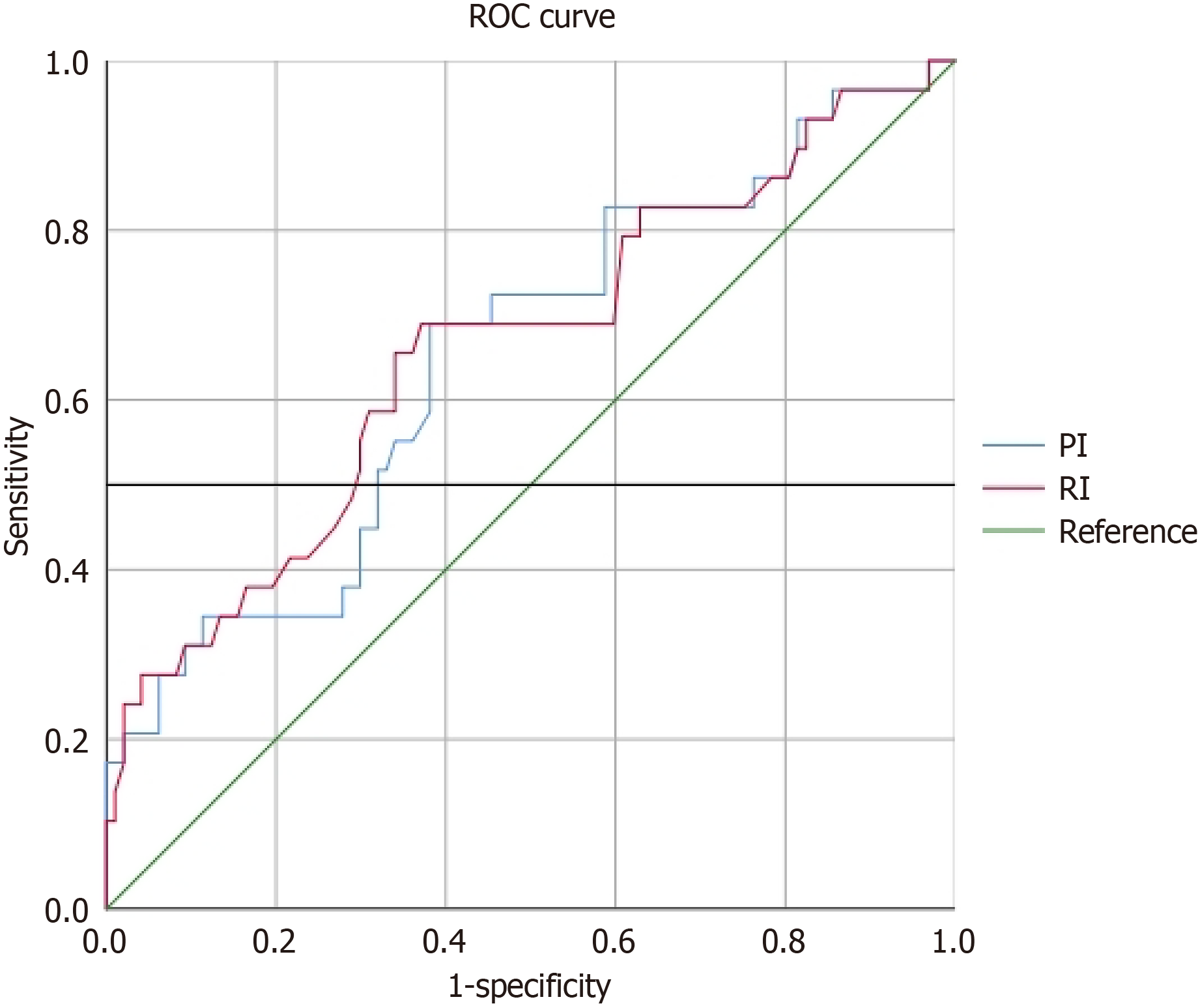
The area under the ROC curve of mean PI of bilateral UtAs was 0.650 with a Youden index of 0.309 and the cutoff value was 1.393. Twenty-one cases (21/29, 72.4%) in the abnormal group had a PI higher than the cutoff value and 60 cases (60/97, 61.9%) in the control group had a PI lower than the cutoff value. The area under the ROC curve of mean RI of bilateral UtAs was 0.661 with a Youden index of 0.319 and the cutoff value was 0.683 (Figure 2). Twenty cases (20/29, 96.0%) in the abnormal group had a RI higher than the cutoff value and 61 cases (61/97, 62.9%) in the control group had a RI lower than the cutoff value.
The results of bivariate logistic regression analysis are shown in Table 4. Monochorionic diamniotic, higher mean PI of bilateral UtAs and abnormal ultrasound findings during first trimester screening were independent risk factors for adverse pregnancy outcomes (P < 0.05).
| Characteristics | Odd ratios | 95% confidence interval | P value |
| Mean PI of bilateral uterine arteries | 3.524 | 1.015-12.236 | 0.047 |
| Abnormal ultrasound findings during first trimester screening | 56.146 | 10.086-312.547 | < 0.001 |
| Chorionicity | 0.276 | 0.088-0.862 | 0.027 |
Our study results showed that the first trimester ultrasound screening findings, including monochorionic diamniotic, higher mean PI of bilateral UtAs and abnormal ultrasound findings were independent risk factors in twin pregnancy for adverse pregnancy outcomes before 28 weeks gestation. Personal and family medical history were not independent risk factors for adverse pregnancy outcomes.
Monochorionic twin pregnancies are associated with a high risk of adverse pregnancy outcomes, including sponta
Uterine spiral artery remodeling during normal pregnancy can transform the narrow myometrial arteries into uterine placental vessels with low resistance and a large caliber and impairment in maternal uterine spiral artery remodeling could lead to abnormal placental function[18]. UtA parameters by Doppler ultrasound including PI, RI and early diastolic notch may reflect the changes in uteroplacental circulation during the remodeling process and are usually used as predictors of fetal growth restriction or pre-eclampsia[19,20]. UtA parameters may be independent risk factors for adverse pregnancy outcomes[21,22]. The study by Bao et al[21] showed that the increase in uterine radial artery RI at 8 weeks gestation was associated with spontaneous abortion in women with recurrent pregnancy losses and thrombophilia; the study by Awor et al[22] showed that bilateral end-diastolic notch in UtAs at 16-24 weeks gestation was a predictor of stillbirth at 24 + weeks. Although UtA parameters in twin pregnancies were lower than in singletons, studies showed that increased UtA PI in the first trimester was still useful for the identification of early-onset pre-eclampsia and small-for-gestational age of both twins, but not useful for the identification of late-onset pre-eclampsia and small-for-gestational age of one twin[23,24]. However, the value of UtA parameters for the prediction of adverse pregnancy outcomes before 28 weeks gestation in twin pregnancies is still uncertain. Our study showed that twin pregnancies with adverse pregnancy outcomes before 28 weeks gestation were more likely to have higher UtA PI, higher UtA RI and bilateral UtA early diastolic notch than those with normal pregnancy outcomes. Our results suggest that higher UtA PI was an independent risk factor for adverse pregnancy outcomes in twin pregnancy.
First trimester ultrasound between 11 and 13 weeks gestation for twin pregnancy is very important and does not only establish gestational age and determine the chorionicity and amnionicity accurately, but also evaluates fetal anatomy, risk of aneuploidy and unique complications in twin pregnancy[12-14]. In our study, we detected eight cases of one intrauterine fetal death, one case of twin reversed arterial perfusion sequence, three cases of one fetal structural abnormality as omphalocele, gastroschisis and hydrops fetalis and two cases of one fetal NT thickening. The early detection of fetal abnormalities by first trimester ultrasound was an independent risk factor for adverse pregnancy outcomes in twins and was helpful for further management and prognosis.
CRL discordance at 11-13 weeks gestation is usually defined as (larger CRL - smaller CRL)/larger CRL ≥ 10%[15]. The study by Janssen et al[9] showed that CRL discordance at 11-14 weeks gestation was associated with a high risk of stillbirth or miscarriage. However, our study showed that CRL discordance did not predict adverse pregnancy outcomes. The value of CRL discordance still requires further large sample studies to confirm this association[2].
Some maternal personal factors were considered risk factors for adverse outcomes in twin pregnancy[6-8]. In our study, none of the patients in both groups had a history of pre-eclampsia, diabetes or systemic lupus erythematosus. Only 1 patient in the control group had a history of hypertension. None of the patients were smokers. These factors may have been associated with the better socio-economic and educational status of the patients. In addition, these factors were not evaluated in this study. Our results showed higher maternal age, higher BMI, higher blood pressure, assisted conception and family history of hypertension were not associated with adverse outcomes in twin pregnancy.
Our study showed that monochorionic diamnioticity, higher mean PI of bilateral UtAs and abnormal ultrasound findings during first trimester screening were independent risk factors for adverse pregnancy outcomes. These results highlighted the importance of first trimester ultrasound screening and when above-mentioned results are detected, adverse pregnancy outcomes should be considered and measures should be taken to monitor the fetuses closely for early diagnosis of adverse pregnancy outcomes or preventing the adverse pregnancy outcomes.
Our study had some limitations. First, patient numbers were insufficient, especially in the abnormal group. Second, the participants in our study may deviate from the general population as the proportion of severe maternal abnormalities, such as BMI ≥ 30 kg/m2 or high blood pressure, was very low. Further prospective larger studies are needed to verify our results.
Monochorionic diamnioticity, higher mean PI of bilateral UtAs and abnormal ultrasound findings during first trimester screening were independent risk factors for adverse pregnancy outcomes. First trimester ultrasound screening is important and the findings were useful for predicting pregnancy outcomes and for guiding clinical management.
| 1. | Martin JA, Hamilton BE, Osterman MJK, Driscoll AK. Births: Final Data for 2019. Natl Vital Stat Rep. 2021;70:1-51. [PubMed] |
| 2. | Wei J, Liu CX, Cui H, Zhang LJ, Chen J, Liu SS, Chang L, Zheng DM. [Guidelines for diagnosis, treatment and health care of premature twin birth (2020 edition)]. Zhongguo Shiyong Fukeyuchanke Zazhi. 2020;36:949-956. [DOI] [Full Text] |
| 3. | Gibson JL, Castleman JS, Meher S, Kilby MD. Updated guidance for the management of twin and triplet pregnancies from the National Institute for Health and Care Excellence guidance, UK: What's new that may improve perinatal outcomes? Acta Obstet Gynecol Scand. 2020;99:147-152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 22] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 4. | Mor N, Machtinger R, Yinon Y, Toussia-Cohen S, Amitai Komem D, Levin M, Sivan E, Meyer R. Outcome of two sequential singleton pregnancies and twin pregnancies among primiparous women at advanced age undergoing IVF. Arch Gynecol Obstet. 2020;302:1113-1119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 5. | Southwest Thames Obstetric Research Collaborative (STORK). Prospective risk of late stillbirth in monochorionic twins: a regional cohort study. Ultrasound Obstet Gynecol. 2012;39:500-504. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 35] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 6. | Whittaker M, Greatholder I, Kilby MD, Heazell AEP. Risk factors for adverse outcomes in twin pregnancies: a narrative review. J Matern Fetal Neonatal Med. 2023;36:2240467. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 16] [Reference Citation Analysis (0)] |
| 7. | D'Antonio F, Odibo A, Berghella V, Khalil A, Hack K, Saccone G, Prefumo F, Buca D, Liberati M, Pagani G, Acharya G. Perinatal mortality, timing of delivery and prenatal management of monoamniotic twin pregnancy: systematic review and meta-analysis. Ultrasound Obstet Gynecol. 2019;53:166-174. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 58] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 8. | Ram M, Berger H, Lipworth H, Geary M, McDonald SD, Murray-Davis B, Riddell C, Hasan H, Barrett J, Melamed N; DOH-Net (Diabetes, Obesity and Hypertension in Pregnancy Research Network) and SOON (Southern Ontario Obstetrical Network) Investigators. The relationship between maternal body mass index and pregnancy outcomes in twin compared with singleton pregnancies. Int J Obes (Lond). 2020;44:33-44. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 29] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 9. | Janssen MK, Levine LD, Bromley B, Chasen ST, Russo ML, Roman AS, Limaye MA, Ranzini AC, Clifford CM, Biggio JR Jr, Subramanian A, Seasely A, Patil AS, Weed S, Page JM, Nicholas S, Idler J, Rao R, Crowder A, Shree R, McLennan G, Dugoff L; Twin Cell-Free DNA Study Consortium. Clinical implications of crown-rump length discordance at 11 to 14 weeks in dichorionic twins. Am J Obstet Gynecol. 2024;230:83.e1-83.e11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 10. | Bhide A, Sankaran S, Sairam S, Papageorghiou AT, Thilaganathan B. Relationship of intertwin crown-rump length discrepancy to chorionicity, fetal demise and birth-weight discordance. Ultrasound Obstet Gynecol. 2009;34:131-135. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 47] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 11. | Özkan MB, Ozyazici E, Emiroglu B, Özkara E. Can we measure the spiral and uterine artery blood flow by real-time sonography and Doppler indices to predict spontaneous miscarriage in a normal-risk population? Australas J Ultrasound Med. 2015;18:60-66. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 12. | Khalil A, Rodgers M, Baschat A, Bhide A, Gratacos E, Hecher K, Kilby MD, Lewi L, Nicolaides KH, Oepkes D, Raine-Fenning N, Reed K, Salomon LJ, Sotiriadis A, Thilaganathan B, Ville Y. ISUOG Practice Guidelines: role of ultrasound in twin pregnancy. Ultrasound Obstet Gynecol. 2016;47:247-263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 352] [Cited by in RCA: 421] [Article Influence: 42.1] [Reference Citation Analysis (0)] |
| 13. | International Society of Ultrasound in Obstetrics and Gynecology, Bilardo CM, Chaoui R, Hyett JA, Kagan KO, Karim JN, Papageorghiou AT, Poon LC, Salomon LJ, Syngelaki A, Nicolaides KH. ISUOG Practice Guidelines (updated): performance of 11-14-week ultrasound scan. Ultrasound Obstet Gynecol. 2023;61:127-143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 139] [Article Influence: 46.3] [Reference Citation Analysis (0)] |
| 14. | Syngelaki A, Hammami A, Bower S, Zidere V, Akolekar R, Nicolaides KH. Diagnosis of fetal non-chromosomal abnormalities on routine ultrasound examination at 11-13 weeks' gestation. Ultrasound Obstet Gynecol. 2019;54:468-476. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 137] [Cited by in RCA: 197] [Article Influence: 28.1] [Reference Citation Analysis (0)] |
| 15. | Li X, Xuan Y, Wang J, Wang L, Papageorghiou AT, Wu Q. Crown-Rump Length Discordance, Increased Nuchal Translucency, and Detection of Fetal Structural Anomalies in Twin Pregnancies in the First Trimester: 5 Years of Experience in a Tertiary Hospital in China. J Ultrasound Med. 2022;41:971-982. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 16. | Glinianaia SV, Rankin J, Khalil A, Binder J, Waring G, Sturgiss SN, Thilaganathan B, Hannon T. Prevalence, antenatal management and perinatal outcome of monochorionic monoamniotic twin pregnancy: a collaborative multicenter study in England, 2000-2013. Ultrasound Obstet Gynecol. 2019;53:184-192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 31] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 17. | Lewi L, Van Schoubroeck D, Gratacós E, Witters I, Timmerman D, Deprest J. Monochorionic diamniotic twins: complications and management options. Curr Opin Obstet Gynecol. 2003;15:177-194. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 155] [Cited by in RCA: 148] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 18. | Allerkamp HH, Leighton S, Pole T, Clark AR, James JL. Synergistic regulation of uterine radial artery adaptation to pregnancy by paracrine and hemodynamic factors. Am J Physiol Heart Circ Physiol. 2023;325:H790-H805. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 19. | Lee NMW, Chaemsaithong P, Poon LC. Prediction of preeclampsia in asymptomatic women. Best Pract Res Clin Obstet Gynaecol. 2024;92:102436. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 20. | Springer S, Worda K, Franz M, Karner E, Krampl-Bettelheim E, Worda C. Fetal Growth Restriction Is Associated with Pregnancy Associated Plasma Protein A and Uterine Artery Doppler in First Trimester. J Clin Med. 2023;12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 21. | Bao SH, Chigirin N, Hoch V, Ahmed H, Frempong ST, Zhang M, Ruan JL, Kwak-Kim J. Uterine Radial Artery Resistance Index Predicts Reproductive Outcome in Women with Recurrent Pregnancy Losses and Thrombophilia. Biomed Res Int. 2019;2019:8787010. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 22. | Awor S, Byanyima R, Abola B, Kiondo P, Orach CG, Ogwal-Okeng J, Kaye D, Nakimuli A. Prediction of stillbirth low resource setting in Northern Uganda. BMC Pregnancy Childbirth. 2022;22:855. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 23. | Filipecka-Tyczka D, Pokropek A, Kajdy A, Modzelewski J, Rabijewski M. Uterine Artery Doppler Reference Ranges in a Twin Caucasian Population Followed Longitudinally From 17 to 37 Weeks Gestation Compared to That of Singletons. J Ultrasound Med. 2021;40:2421-2429. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 24. | Rizzo G, Pietrolucci ME, Aiello E, Capponi A, Arduini D. Uterine artery Doppler evaluation in twin pregnancies at 11 + 0 to 13 + 6 weeks of gestation. Ultrasound Obstet Gynecol. 2014;44:557-561. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 25] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/