Published online May 28, 2024. doi: 10.4329/wjr.v16.i5.109
Revised: April 24, 2024
Accepted: April 28, 2024
Published online: May 28, 2024
Processing time: 58 Days and 12.3 Hours
Effective communication and collaboration among healthcare professionals are crucial for delivering high-quality patient care. Interdepartmental miscommunication poses a significant challenge to healthcare systems, potentially under
Core Tip: Successful collaboration across healthcare disciplines is vital for delivering the best patient care. Miscommunication between departments and challenges in communication between referring physicians and radiologists can compromise radiology services, risking both patient outcomes and the overall quality of healthcare services provided. This article emphasizes these ongoing communication challenges, prompting readers to recognize potential pitfalls in their daily clinical practice. Additionally, practical solutions are provided that should be tailored to the specific needs and challenges faced by each individual healthcare institution.
- Citation: Arkoudis NA, Karofylakis E, Moschovaki-Zeiger O, Prountzos S, Efthymiou E, Samonis G, Koutserimpas C. Interdepartmental miscommunication regarding radiology: Addressing chronic challenges and exploring solutions. World J Radiol 2024; 16(5): 109-114
- URL: https://www.wjgnet.com/1949-8470/full/v16/i5/109.htm
- DOI: https://dx.doi.org/10.4329/wjr.v16.i5.109
Interdepartmental collaboration in healthcare is of paramount importance to ensure accurate diagnosis and treatment. However, miscommunication among healthcare professionals may lead to errors and compromise patients’ effective treatment[1]. The field of radiology relies heavily on clear communication between radiologists and other healthcare practitioners. Lack of effective communication may lead to misunderstandings and misinterpretations of imaging findings, leading to incorrect or missed diagnoses, which in turn negatively impact therapeutic decisions[2] and harbor medicolegal implications as well[3]. If crucial information has been overlooked, it may affect the patient’s management and treatment based on suboptimal radiology reports, while delays in receiving imaging results containing diagnoses hinder appropriate treatment and may delay the patient’s care. Inadequate communication between radiology departments and other healthcare units may lead to redundant or unnecessary imaging studies, causing patients’ discomfort, wasting time and resources, and increasing costs.
Several converging factors may contribute to miscommunication, yielding unpleasant and, at times, dangerous results.
Attending physicians often deal with vast amounts of information given by the patient or his or her companions, making it difficult to prioritize and accurately convey critical details to other healthcare professionals. In addition, patients, at times, struggle to effectively inform about their complete medical history and express their symptoms, unintentionally skipping important details. Depending on the patient’s and the attending physician’s personalities, the physician may also face difficulties eliciting the necessary details, potentially leading to an incomplete understanding of the patient’s condition. Hence, physicians might unintentionally overlook documenting essential facts, either due to forgetfulness or a lack of awareness regarding the relevance of certain details important for radiological assessment. As a result of the above, when requesting an imaging examination, there is a significant risk that vital information may not reach the radiologist and that the information provided on the radiologist’s request form may suffer from suboptimal quality since it becomes progressively diluted. This issue becomes particularly critical in emergency departments, where the workload, the strict time limits for diagnostic and therapeutic decisions, and the hard-working conditions may lead to extra misunderstandings. Under such circumstances, incomplete communication may be exacerbated as the probability of oversight of essential patient data significantly increases, leading to potential diagnostic limitations. However, providing insufficient information not only impacts the interpretation of results by attending radiologists but may also influence the choice of the selected imaging protocol, which is often tailored to address a specific clinical question at hand.
Therefore, ensuring that accurate and necessary information is communicated by the referring physicians is crucial for obtaining reliable and meaningful results from radiological examinations.
On the other hand, issues occurring as a result of the radiologist’s workflow can also inadvertently lead to miscommunications and subpar outcomes.
Radiologists may also frequently experience a heavy workload, needing to interpret a large volume of imaging studies within a limited time frame. The pressure to process numerous cases efficiently may result in hurried assessments and the potential oversight of key findings. Consequently, radiologists may encounter challenges in effectively communicating all pertinent imaging results to the referring physician. These challenges may manifest either during the initial verbal communication, which is typically concise and conducted over the phone, or in the final written report, where funda
Moreover, there has been a progressively increased dependence on digital communication throughout the past few years due to the use of the picture archiving and communication system (PACS), which has inevitably resulted in a decline of face-to-face interactions, raising concerns regarding potential negative effects on the feedback loop between referring physicians and radiologists[2,5].
In addition, the use of different electronic health record systems and the limited integration among the various platforms used in different institutions and health care centers may impede the seamless sharing of patient information. As a result, when patients visit a new healthcare provider or undergo imaging tests at a different facility, there is no guarantee that their previous medical imaging data will be readily accessible to the current physician. In such cases, physicians may rely on patients to remember and bring physical copies or digital files of their prior imaging examinations, while regarding hospitalized patients, radiologists may subsequently rely on the referring physicians to bring those examinations to their attention. Unfortunately, this process is far from being foolproof, as patients may forget or encounter difficulties obtaining their medical records, rendering critical information missing or inaccessible and limiting the accuracy of the current examination. The consequences of this fragmented approach may be detrimental, as radiologists and subsequently treating physicians may struggle to accurately interpret the novelty and clinical relevance of current imaging findings without the context provided by previous studies.
In certain instances, physicians may seek advice from radiologists who are not the reporting specialists because they share a pre-existing relationship and therefore feel comfortable. These informal consultations may involve the exchange of new medical information regarding the case that was not initially available and may also include informal assessments of the examination. The latter scenario, of course, could even occur when a second look at a previously interpreted examination takes place by the same radiologist. However, such practices pose potential risks to patient safety, especially when discrepancies leading to alterations in patient management arise between the informal consultation and the official written report[6].
On another note, an often-overlooked factor contributing to interdepartmental miscommunication are the hierarchical structures within healthcare settings that can hinder effective communication. The reluctance, especially of younger or less experienced physicians, to challenge or seek clarification from higher-ranking professionals may lead to incorrect initiatives regarding the appropriate steps for patient management. This includes insufficient selections regarding which radiological examinations might be most indicated and suitable to perform on a case; thus, further augmenting misunderstandings and misinterpretations.
To address these issues, it is crucial to identify and develop practical solutions.
Implementing standardized and comprehensive radiology request forms that guide both patients and referring physicians to provide the necessary patient information, medical history, and symptoms reduces the risk of omitting critical details. On a similar note, educating patients on the importance of accurately conveying their medical history when, or prior to, seeking imaging examinations is crucial, as patient involvement in their own healthcare can mitigate communication gaps. In those cases where patients are unable to, or find difficulties, in gathering and conveying their medical records for various reasons, patient advocates or specifically allocated coordinators within healthcare settings can provide assistance, especially in cases of transitions between different healthcare institutions or providers.
Organizing regular interdisciplinary meetings that bring together radiologists, referring physicians, and other healthcare professionals to discuss complex cases, share insights, and improve mutual understanding could also aid in dispelling the issues of misunderstandings and miscommunication. Arranging training sessions on effective communication and the importance of clear and concise information exchange for both referring physicians and radiologists might also prove helpful.
Second reads by radiologists or formal consultations in cases where there is uncertainty or discrepancies may also be encouraged; however, the results of these consultations should be well-documented, leading to a consensus on the findings. Alternatively, this may also be achieved if it takes place during well-organized interdisciplinary meetings.
During these meetings, it’s important to discuss relevant and targeted updates from the literature, as well as recent significant publications. Continuous knowledge transfer across various specialties is vital for radiologists, especially given the swift advancements in medical devices and treatment materials. Without this interdisciplinary awareness, radiologists may misinterpret normal findings as pathological, leading to unnecessary workups, examinations, and possibly interventions. Additionally, valuable insights for radiological practice can often emerge from journals specializing in other disciplines due to the collaborative nature of subspecialties. Similarly, advancements in radiology must be effectively communicated to clinicians to ensure an accurate understanding of their benefits, limitations, and actual clinical applicability and relevance. Therefore, maintaining up-to-date knowledge across different medical fields is essential for radiologists to interpret imaging findings accurately and collaborate productively with referring physicians. This broader perspective enhances interdisciplinary communication and ensures more comprehensive patient care.
In addition, the integration of electronic health record systems across healthcare institutions should be encouraged to facilitate seamless sharing of patient information that would ensure that relevant medical data, including prior imaging studies, are readily accessible. Training sessions may also include updates on these electronic systems as well as other relevant technologies, including PACS, ensuring that these digital tools are employed in the most efficient way for communication and information exchange.
Integration of digital communication tools within healthcare systems (i.e., secure messaging platforms) could enable enhanced real-time communication between radiologists and referring physicians. When communications take place over the phone, developing standardized protocols for discussing findings (i.e., structured verbal communications) may be invaluable, particularly in time-sensitive cases where the most important and relevant findings need to be communicated.
In cases of uncertainty regarding the most suitable imaging modality for a particular clinical scenario, referring physicians should be encouraged to seek guidance from the attending radiologist. This collaborative consultation may ensure the early involvement of the radiologist in the patient’s management, promoting an inclusive approach. Such engagement is likely to increase the possibility of an optimized imaging examination protocol and the quality of the end report.
To avoid ineffective communication as a result of hierarchy within healthcare, it is necessary to promote a culture of open communication where all team members, regardless of their level of experience, feel comfortable seeking clarification and questioning decisions when necessary. This approach not only has the potential to improve outcomes through thorough double-checking but also encourages physicians of higher stature to articulate their thought processes. This, in turn, promotes staying up-to-date and ensuring that decisions adhere to the highest standards.
Establishing quality assurance programs for radiology departments that focus on the accuracy and completeness of radiology reports can help improve their quality. Regular audits and feedback from clinicians may assist in this process and help identify areas that can benefit from improvement.
Finally, educating and raising awareness on the potential medicolegal implications of miscommunication leading to suboptimal quality of healthcare services can further push those involved towards improvement.
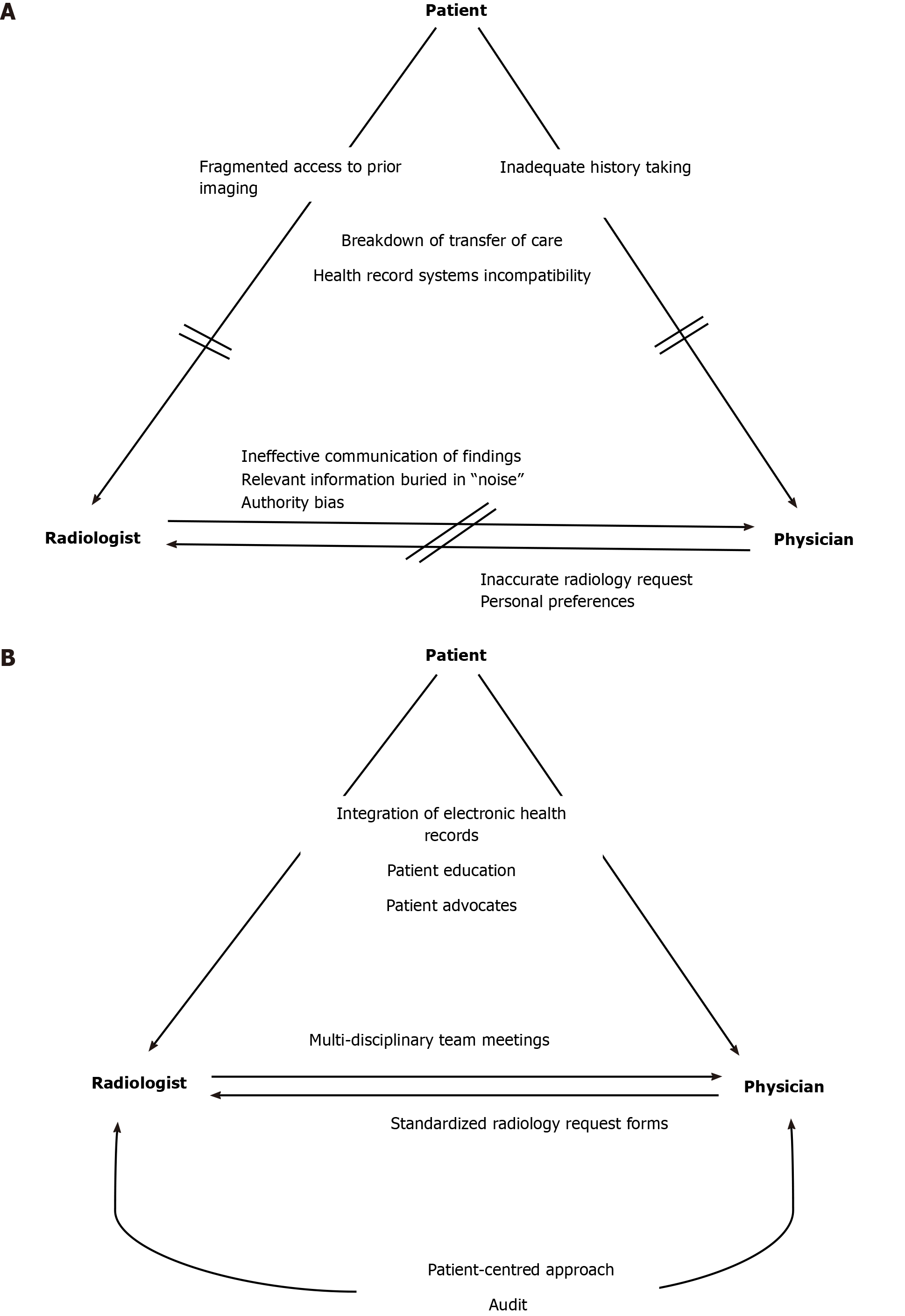
In conclusion, addressing interdisciplinary miscommunication among radiologists and collaborating physicians is essential to achieving accurate and timely diagnosis and avoiding preventable errors in patient management. Identifying the various root causes of suboptimal communications is an imperative step towards generating practical solutions. However, it is important to note that not all healthcare institutions face the same issues; therefore, solutions should be tailored to the specific needs and challenges of each one. Continuous observation and feedback are essential to ensure that the implemented strategies are effective and to identify which areas may require further adjustments to improve interdisciplinary collaboration and communication in radiology and, consequently, in healthcare as a whole. A summary of the most pertinent and important etiologies of interdisciplinary miscommunication and possible proposed solutions is provided in Figure 1.
| 1. | Rajendran L. "Teamwork makes the dream work"- interdisciplinary team dynamics within the operating room. Can Med Educ J. 2022;13:108. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 2. | Reiner B, Siegel E, Protopapas Z, Hooper F, Ghebrekidan H, Scanlon M. Impact of filmless radiology on frequency of clinician consultations with radiologists. AJR Am J Roentgenol. 1999;173:1169-1172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 82] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 3. | Pinto F, Capodieci G, Setola FR, Limone S, Somma F, Faggian A, Romano L. Communication of findings of radiologic examinations: medicolegal considerations. Semin Ultrasound CT MR. 2012;33:376-378. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 4. | Fatahi N, Krupic F, Hellström M. Difficulties and possibilities in communication between referring clinicians and radiologists: perspective of clinicians. J Multidiscip Healthc. 2019;12:555-564. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 20] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 5. | Tillack AA, Breiman RS. Renegotiating expertise: an examination of PACS and the challenges to radiology using a medical anthropologic approach. J Am Coll Radiol. 2012;9:64-68. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 6. | Won E, Rosenkrantz AB. JOURNAL CLUB: Informal Consultations Between Radiologists and Referring Physicians, as Identified Through an Electronic Medical Record Search. AJR Am J Roentgenol. 2017;209:965-969. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 10] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Radiology, nuclear medicine and medical imaging
Country of origin: Greece
Peer-review report’s classification
Scientific Quality: Grade C
Novelty: Grade B
Creativity or Innovation: Grade B
Scientific Significance: Grade B
P-Reviewer: Au SCL, China S-Editor: Chen YL L-Editor: A P-Editor: Zheng XM