Published online Oct 28, 2024. doi: 10.4329/wjr.v16.i10.608
Revised: September 19, 2024
Accepted: October 15, 2024
Published online: October 28, 2024
Processing time: 152 Days and 14.5 Hours
The extraction of maxillary impacted teeth is a common procedure in oral surgery, frequently complicated by oroantral communications. For less-experienced cli
We present a case involving disparate outcomes following bilateral extraction of maxillary third molars. Using cone-beam computed tomography and three-di
This case highlights the potential utility of predictive analysis in guiding the ma
Core Tip: This case report presents unexpected findings in bilateral maxillary third molar extractions. Using cone-beam computed tomography (CBCT) and three-dimensional software, we digitally evaluated factors influencing extraction difficulty and risk, accounting for potential confounders. Key variables analyzed included alveolar bone volume, bone quality, crown-root angulation, and maxillary sinus mucosal thickness. Notably, variations in "tegmen bone" volume between the tooth and maxillary sinus emerged as a critical determinant. We propose a simplified CBCT-based measurement method to enhance risk assessment and extraction planning of impacted tooth.
- Citation: Liu H, Wang F, Tang YL, Yan X. Asymmetric outcomes in bilateral maxillary impacted tooth extractions: A case report. World J Radiol 2024; 16(10): 608-615
- URL: https://www.wjgnet.com/1949-8470/full/v16/i10/608.htm
- DOI: https://dx.doi.org/10.4329/wjr.v16.i10.608
In clinical practice, the extraction of maxillary impacted teeth is a common surgical procedure, with oroantral com
Radiological variables are crucial for the analysis of third molar extractions[5]. Traditionally, the distance between the tooth root and the maxillary sinus is measured, but this approach is often inaccurate due to potential intermittent contact between the horizontally impacted tooth crown and the maxillary sinus mucosa[6]. The tegmen bone (TB) between the maxillary sinus floor and the tooth may fracture under the forces exerted during tooth extraction, making it essential to define and measure the TB region[7]. Studies have shown that alveolar bone stability is only maintained when bone thickness reaches 2 mm[8]. Sun et al’s research further suggests that the alveolar bone thickness should exceed 0.6 mm[9]; otherwise, CT values in this area reflect the average density of both the alveolar bone and the adjacent periodontal ligament, rather than the alveolar bone itself[9]. Establishing precise parameters and methodologies for quantifying TB mass remains a significant challenge in current research.
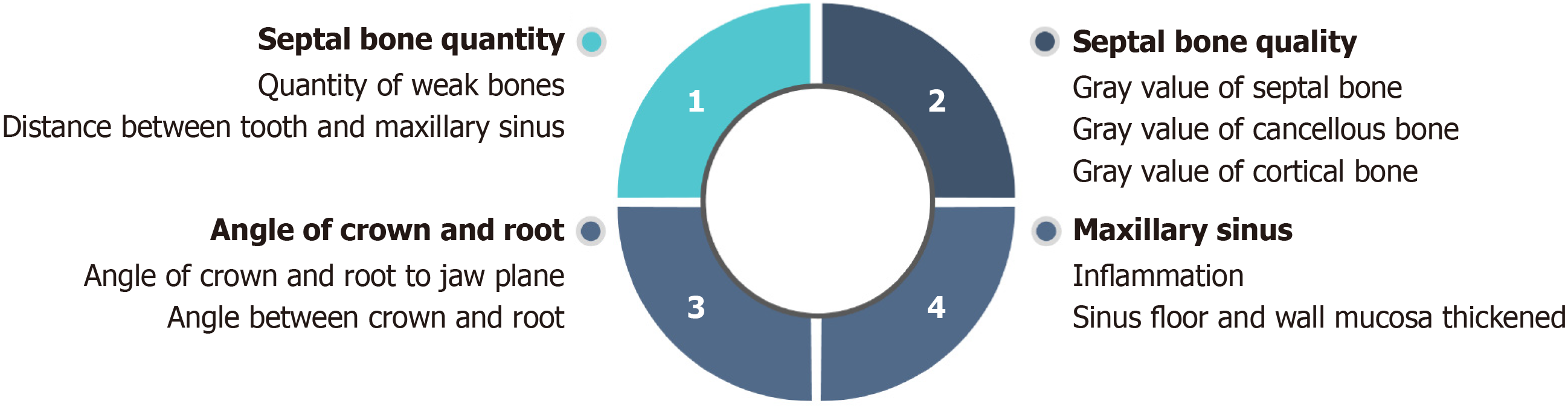
This article presents and compares the outcomes of bilateral maxillary impacted tooth extractions in a single case. We categorized the radiological variables into four groups: Alveolar bone quantity, alveolar bone quality, crown-root angle, and maxillary sinus mucosal condition (Figure 1). Through our analysis, we identified alveolar bone quantity as the primary radiological factor influencing the observed differences in risk in this case. Based on radiological data, we introduced the novel concept of TB quantity for quantitative analysis and comparison. In this case, the TB measurement was defined as a bone volume of less than 1 mm between the maxillary sinus floor and the tooth root. This method offers a practical approach for evaluating the complexity and risk of tooth extractions by utilizing CBCT-derived radiological data, thereby contributing to the scientific understanding of extraction procedures.
A 26-year-old woman was referred for the extraction of bilateral maxillary impacted third molars as part of her or
A 26-year-old woman was referred for the extraction of bilateral maxillary impacted third molars as part of her or
The patient had no history of trauma, hypertension, or other medical conditions.
Her history, personal history, and family history were unremarkable.
The impacted teeth were not visible upon clinical examination.
Laboratory examinations were normal.
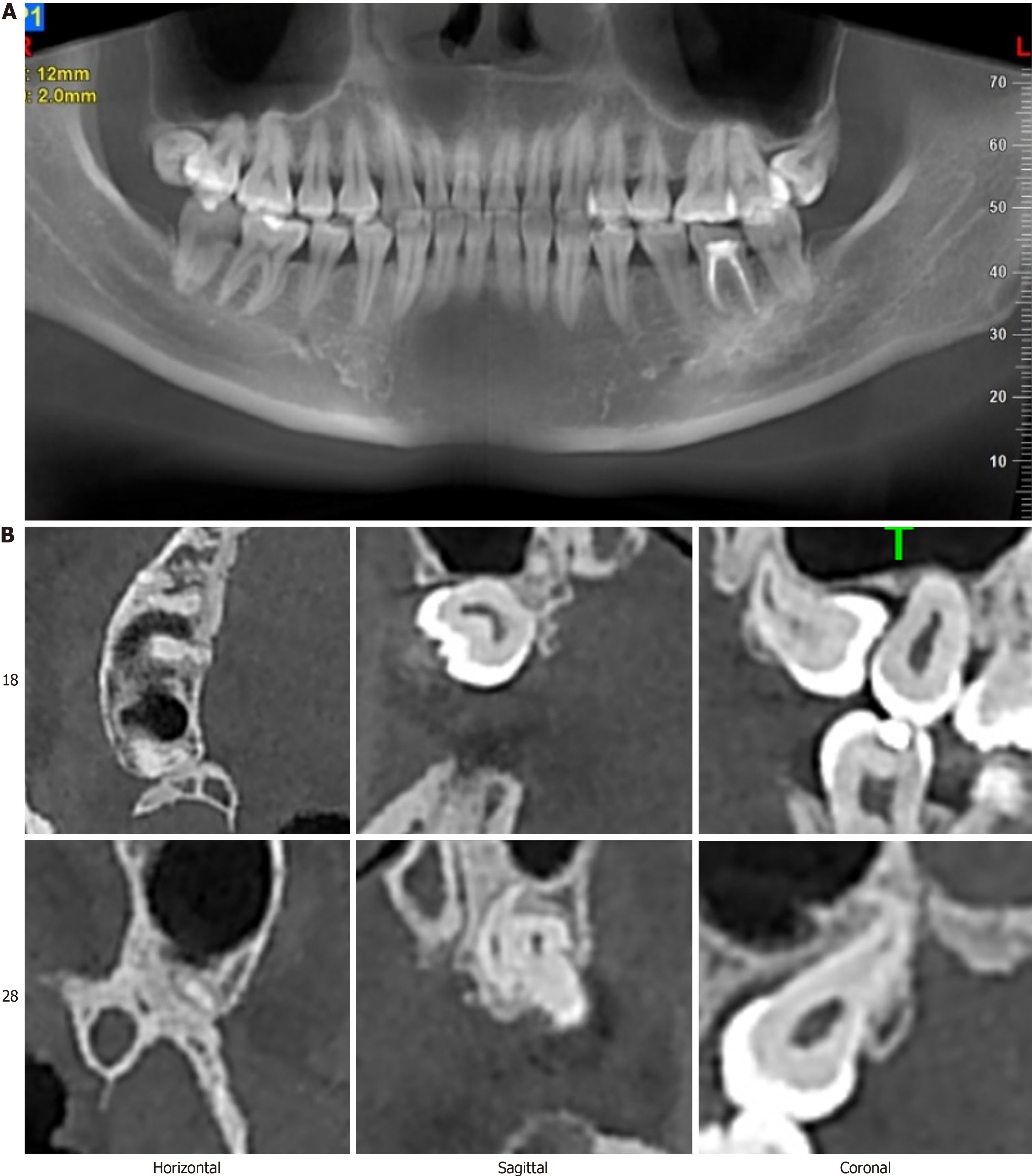
CBCT (NewTom 5G Version FP, Italy) revealed that both teeth were deeply embedded in the maxilla and in close proximity to the maxillary sinus floor, exhibiting a mesial median impaction pattern (Figure 2).
Impacted teeth 18 and 28.
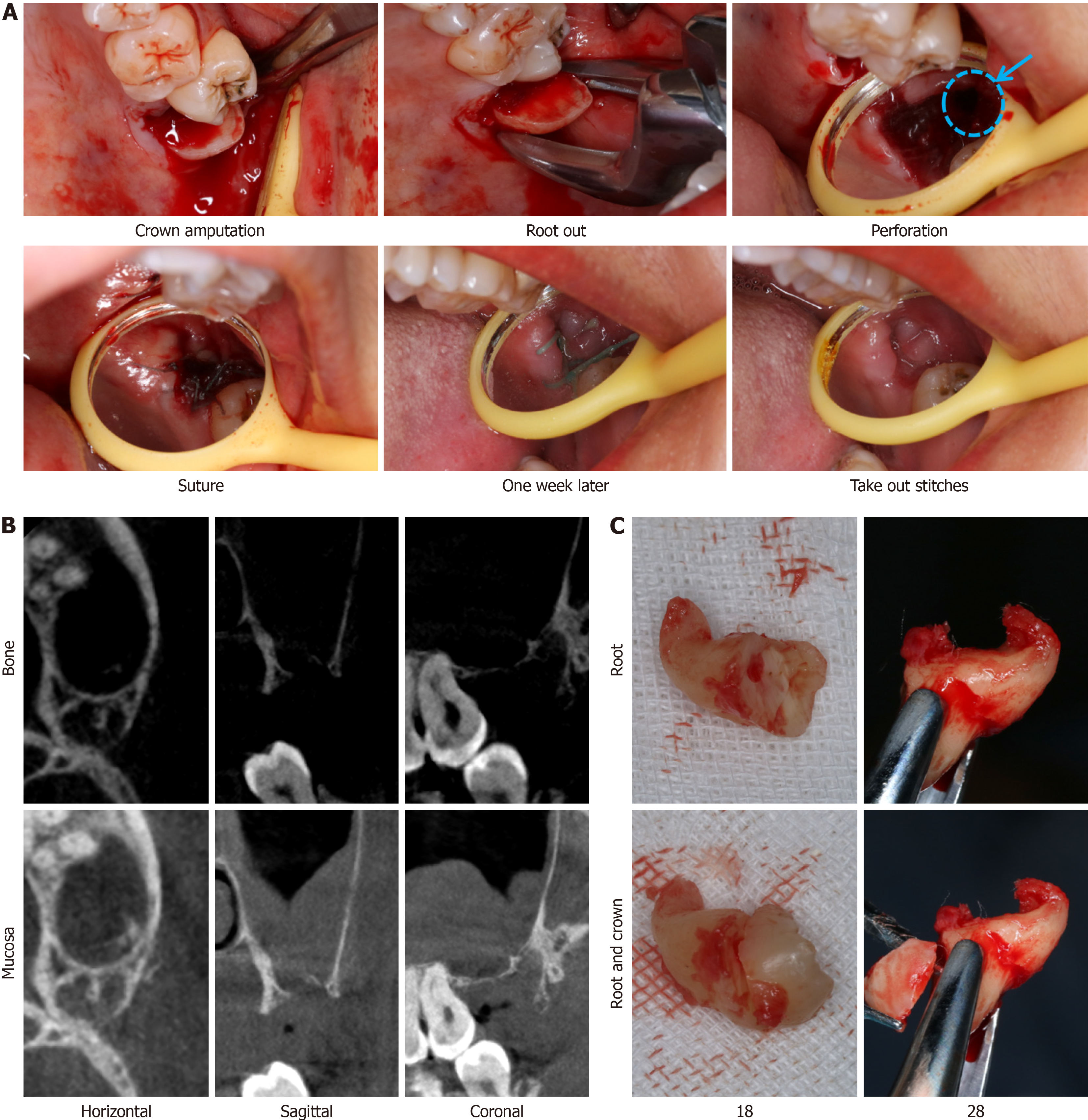
Minimally invasive tooth extraction.
The same oral and maxillofacial surgeon employed a standardized extraction technique (Figure 3) for both teeth but encountered disparate outcomes. While the extraction of tooth 18 was uneventful, removal of tooth 28 resulted in the formation of an oroantral communication. This perforation was managed using collagen application and primary closure of the wound (Figure 3A). Two weeks postoperatively, complete mucosal healing was observed. Nevertheless, on the left side, a postoperative mucosal reaction was detected in the maxillary sinus. Despite the comparable difficulty of bilateral extractions, there is an imperative to develop more precise preoperative assessment tools to accurately gauge the risk of complications associated with tooth extraction (Figure 3).
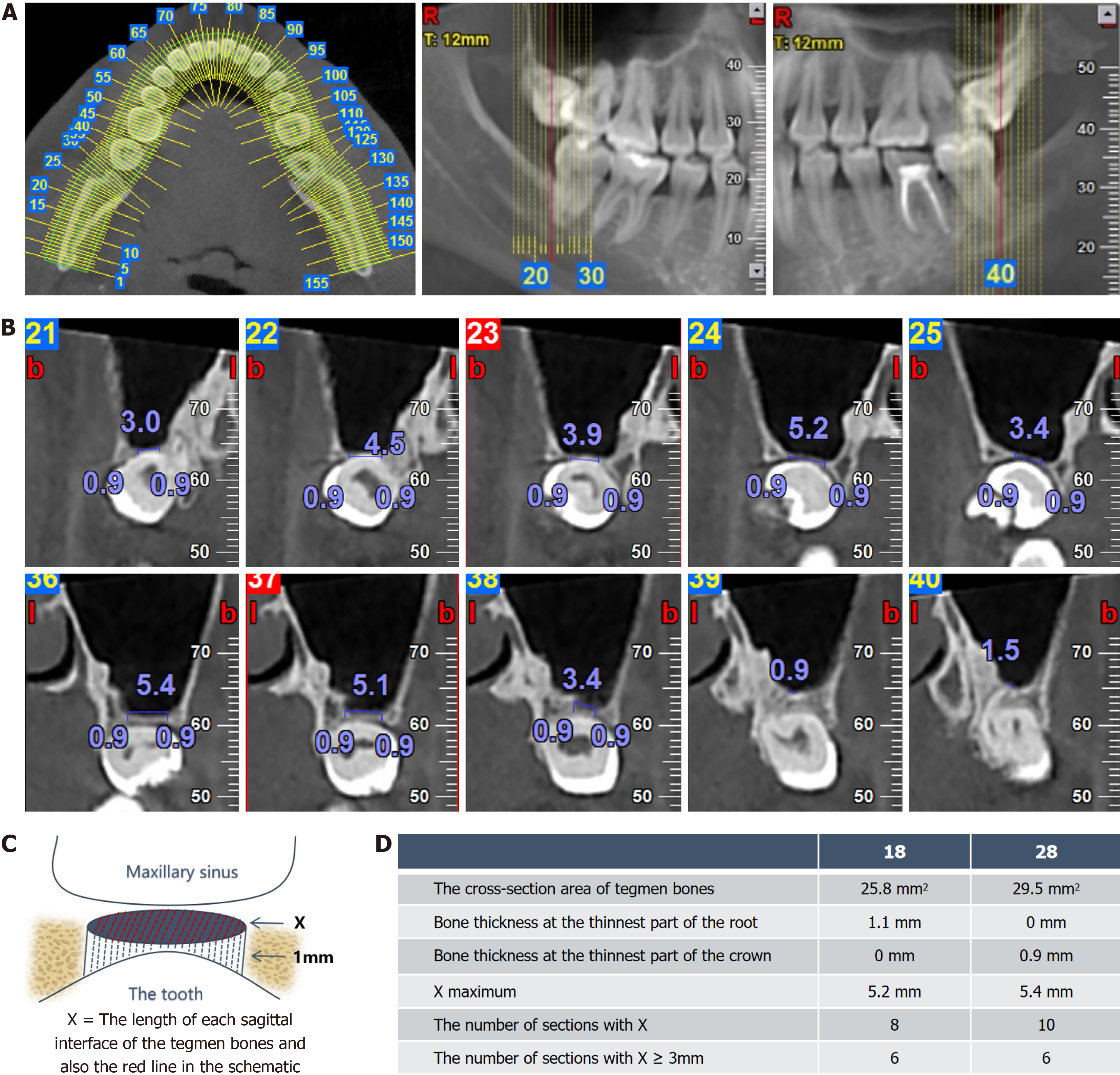
A numerical analysis of preoperative CBCT was conducted to assess extraction risk. The NNT viewer 5.6.0 (NNT QR S.r.l, United States) was used for segmentation of the CBCT data, with an axial slice thickness of 1 mm (Figure 4A). The impacted maxillary teeth were divided into 15 Layers based on the sagittal plane. Numerical analysis was performed for each layer, and the central five layers were selected for detailed evaluation (Figure 4B). To quantify the bone separating the maxillary sinus from the teeth, we introduced the concept of TB, which represents the volume of bone measuring less than 1 mm between the maxillary sinus floor and the tooth root, illustrated as a circular shape in the diagram (Figure 4). For TB measurement, the parameter X was defined, representing the length of each sagittal TB. The TB measurement methodology and corresponding data are depicted in Figure 4C and D.
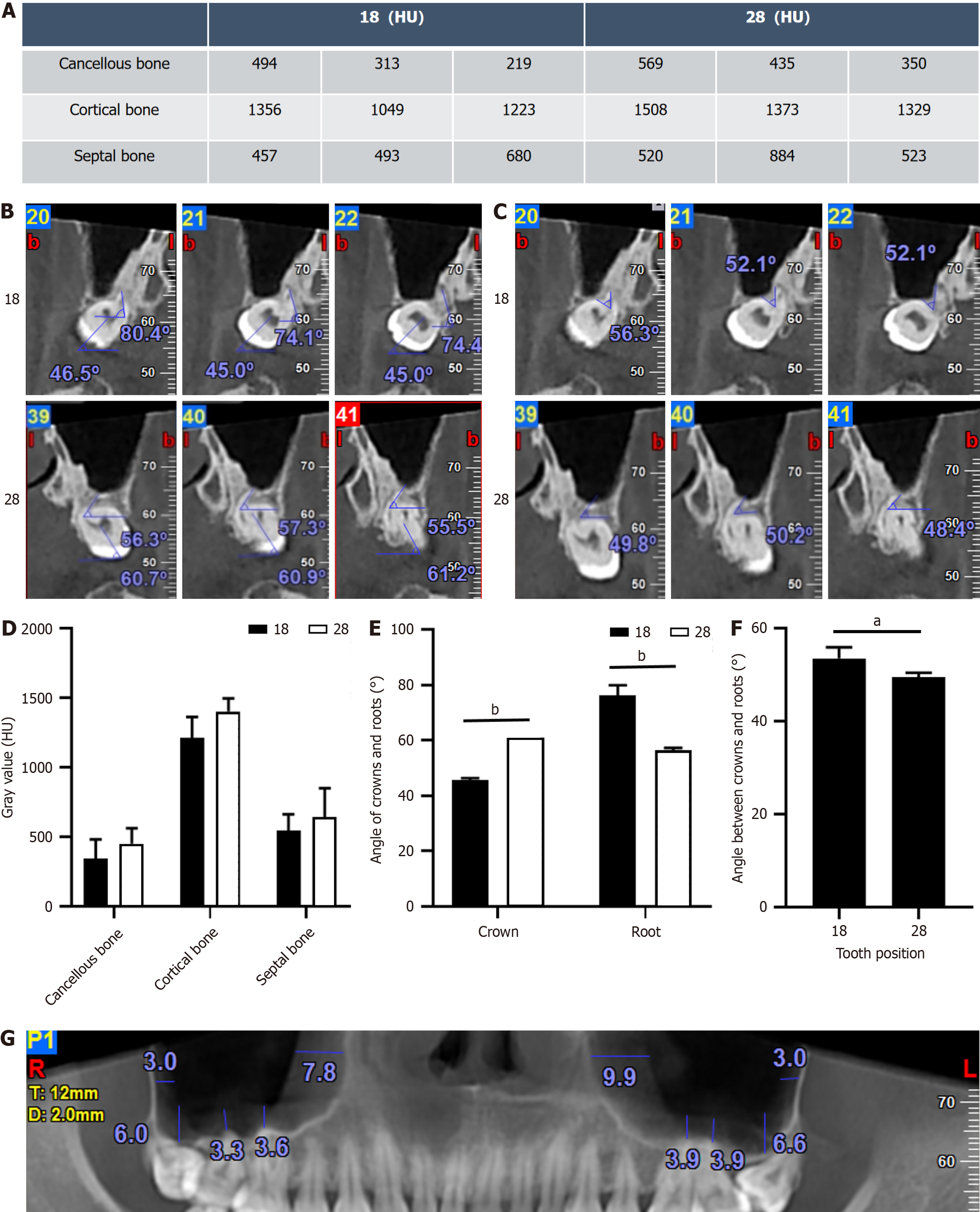
In addition to quantifying septal bone quantity, we assessed septal bone quality by analyzing the gray values of trabecular bone, cortical bone, and the alveolar bone septum. We also measured the angles between the crown and root relative to the jaw plane, and various parameters associated with the maxillary sinus mucosa (Figure 5).
The analysis revealed that the primary difference between the two impacted teeth was in septal bone quantity. As shown in the table in Figure 4D, the bone thickness at the thinnest point of both tooth 28 and tooth 18 is identical at 0 mm. The cross-sectional area of TB for tooth 18 was 25.8 mm², compared to 29.5 mm² for tooth 28, suggesting a lower risk of perforation for tooth 18. Further radiological assessment supported this finding. Additionally, the angle between the crown and root relative to the Frankfort plane differed, with tooth 28 exhibiting a smaller angle, thus increasing the extraction difficulty. No significant differences were observed in septal bone quality or maxillary sinus mucosa between the two sides.
Several key factors influence the risk associated with maxillary third molar extractions[10,11]. First, the position of the maxillary third molars is determined by variables such as the depth within the alveolar bone, the angulation between the root and crown, and the proximity to the maxillary sinus floor. Second, the condition of the alveolar bone and maxillary sinus plays a critical role, including parameters like alveolar bone density, inflammation of the bone, maxillary sinus pathology, and the state of the maxillary sinus mucosa. The third factor is the surgeon's clinical expertise, which encompasses factors such as the direction and magnitude of the force applied during extraction, including the type of force used (e.g., wedge force or axial force). Lastly, patient-specific clinical variables, including mouth opening capacity, age, sex, weight, the position of adjacent teeth, and the presence of dental caries, must be considered.
In this case, the comparison of the maxillary third molars on both sides of the same patient allows us to control for patient-specific factors. Moreover, as the extractions were performed by the same surgeon, potential variability due to operative technique was minimized. Consequently, the primary determinant of extraction difficulty and postoperative risk in this case was the position of the maxillary third molars within the alveolar bone. To quantify the minimal bone volume between the maxillary sinus and the teeth, we introduce the concept of the TB, which refers to the bone volume less than 1 mm between the floor of the maxillary sinus and the tooth roots. The shape of TB is irregular, making it difficult to calculate quantitatively. To address this, we introduced the concept of X, which involves dividing the irregular shape into small rectangles. As the number of subdivisions increases, the sum of the rectangular areas more closely approximates the actual area of the shape. In this case, we used a 1 mm width for the subdivisions to ensure calculability. The X measurement was taken directly from the sagittal plane of the segmented sections. TB has proven to be a precise and valuable tool for predicting the surgical difficulty of maxillary third molar extraction in this case, offering a practical reference for assessing the complexity and risks associated with such procedures. However, further validation across a larger cohort is required.
The data obtained in this study necessitated extensive manual post-processing, introducing challenges such as subjectivity and reproducibility concerns. Thus, exploring the use of computer algorithms to enhance data consistency and to advance CT data segmentation and measurement toward automation and greater precision remains a worthwhile endeavor[12,13]. Additionally, there is a need for further refinement in stress analysis of the alveolar bone during tooth extraction[14]. As research progresses, measurement accuracy will continue to improve.
In summary, this article presents an intriguing case report. The experienced clinician initially assessed the CBCT scans and concluded that tooth 18 was more likely to perforate, yet the outcome revealed no perforation in tooth 18, but rather in tooth 28. We find this paradox particularly interesting: Why did tooth 18, which appeared to have a greater degree of curvature, not perforate? Were there radiographic data that we overlooked, leading to an incorrect prediction? Given that this case rules out variations in patient anatomy and operator skill, we conducted a thorough analysis of all potential factors evident in the CBCT scans and compared them. Our findings suggest that the critical determinant was the tegmental bone volume between the tooth and the floor of the maxillary sinus. Additionally, we propose a simplified measurement method, aiming to provide a feasible approach for evaluating extraction risks and difficulty based on radiographic data.
| 1. | Qu H, Yang Y, Tian Y, Li Z, Sun L, Chen F, Tian B. Third molar-related knowledge, attitudes, behaviors, and medical history of 904 Chinese adults: a cross-sectional survey. J Zhejiang Univ Sci B. 2023;24:896-904. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 2. | Miclotte I, Agbaje JO, Spaey Y, Legrand P, Politis C. Incidence and treatment of complications in patients who had third molars or other teeth extracted. Br J Oral Maxillofac Surg. 2018;56:388-393. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 16] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 3. | Martu C, Martu MA, Maftei GA, Diaconu-Popa DA, Radulescu L. Odontogenic Sinusitis: From Diagnosis to Treatment Possibilities-A Narrative Review of Recent Data. Diagnostics (Basel). 2022;12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 28] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 4. | Roy I, Baliga SD, Louis A, Rao S. Importance of Clinical and Radiological Parameters in Assessment of Surgical Difficulty in Removal of Impacted Mandibular 3rd Molars: A New Index. J Maxillofac Oral Surg. 2015;14:745-749. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 19] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 5. | Klatt JC, Sorowka T, Kluwe L, Smeets R, Gosau M, Hanken H. Does a preoperative cone beam CT reduce complication rates in the surgical removal of complex lower third molars? A retrospective study including 486 cases. Head Face Med. 2021;17:33. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 6. | Hermann L, Wenzel A, Schropp L, Matzen LH. Impact of CBCT on treatment decision related to surgical removal of impacted maxillary third molars: does CBCT change the surgical approach? Dentomaxillofac Radiol. 2019;48:20190209. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 24] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 7. | Hermann L, Nørholt SE, Wenzel A, Taneja P, Matzen LH. Does cone beam CT change the treatment decision for maxillary second and third molars? A prospective study. Dentomaxillofac Radiol. 2023;52:20230128. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 8. | Şen S, Erber R. Neuronal Guidance Molecules in Bone Remodeling and Orthodontic Tooth Movement. Int J Mol Sci. 2022;23. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 9. | Sun R, Zheng LW, Sun YQ, Li TT, Ren JG, Zhao JH. Is it safe and effective to extract impacted maxillary tooth adjacent to maxillary sinus via submaxillary sinus membrane space approach?-a randomized controlled trial. Clin Oral Investig. 2023;27:6081-6087. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 10. | Bedoya MM, Park JH. A review of the diagnosis and management of impacted maxillary canines. J Am Dent Assoc. 2009;140:1485-1493. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 135] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 11. | de Carvalho RW, de Araújo Filho RC, do Egito Vasconcelos BC. Assessment of factors associated with surgical difficulty during removal of impacted maxillary third molars. J Oral Maxillofac Surg. 2013;71:839-845. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 17] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 12. | Kubota S, Imai T, Nishimoto A, Amekawa S, Uzawa N. External validation of cone-beam computed tomography- and panoramic radiography-featured prediction models for inferior alveolar nerve injury after lower third molar removal: proposal of a risk calculator. Odontology. 2023;111:178-191. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 13. | Chen P, Zhang J, Jiang Y, Li Y, Song L, Hu F, Yu Y. A new dataset of oral panoramic x-ray images and parallel network using transformers for medical image segmentation. J Stomatol Oral Maxillofac Surg. 2024;125:101700. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 14. | Pollock TI, Panagiotopoulou O, Hocking DP, Evans AR. Taking a stab at modelling canine tooth biomechanics in mammalian carnivores with beam theory and finite-element analysis. R Soc Open Sci. 2022;9:220701. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 12] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/