Published online May 28, 2023. doi: 10.4329/wjr.v15.i5.136
Peer-review started: December 19, 2022
First decision: February 20, 2023
Revised: March 21, 2023
Accepted: April 10, 2023
Article in press: April 10, 2023
Published online: May 28, 2023
Processing time: 154 Days and 15.8 Hours
Prostate cancer (Pca; adenocarcinoma) is one of the most common cancers in adult males and one of the leading causes of death in both men and women. The diagnosis of Pca requires substantial experience, and even then the lesions can be difficult to detect. Moreover, although the diagnostic approach for this disease has improved significantly with the advent of multiparametric magnetic resonance, that technology has certain unresolved limitations. In recent years artificial intelligence (AI) has been introduced to the field of radiology, providing new software solutions for prostate diagnostics. Precise mapping of the prostate has become possible through AI and this has greatly improved the accuracy of biopsy. AI has also allowed for certain suspicious lesions to be attributed to a given group according to the Prostate Imaging-Reporting & Data System classification. Finally, AI has facilitated the combination of data obtained from clinical, laboratory (prostate-specific antigen), imaging (magnetic resonance), and biopsy examinations, and in this way new regularities can be found which at the moment remain hidden. Further evolution of AI in this field is inevitable and it is almost certain to significantly expand the efficacy, accuracy and efficiency of diagnosis and treatment of Pca.
Core Tip: The peer reviewed literature has provided sufficient support for the continued application and development of artificial intelligence (AI) in prostate cancer clinical care. In addition, the expanding introduction of various AI-based software products created by leading companies is providing practical benefits to radiologists for improved prostate cancer diagnosis. Certainly, the known complexity of the disease and its consequential difficult diagnosis supports the continued development of new approaches for earlier and more accurate detection, such as could be provided through AI technologies.
- Citation: Chervenkov L, Sirakov N, Kostov G, Velikova T, Hadjidekov G. Future of prostate imaging: Artificial intelligence in assessing prostatic magnetic resonance imaging. World J Radiol 2023; 15(5): 136-145
- URL: https://www.wjgnet.com/1949-8470/full/v15/i5/136.htm
- DOI: https://dx.doi.org/10.4329/wjr.v15.i5.136
Prostate cancer (Pca; an adenocarcinoma) is one of the leading causes of death from oncological diseases, and it ranks second among adult males. Despite the high frequency of the disease, screening still largely relies on digital rectal examination, with low sensitivity and low specificity, and prostate-specific antigen (PSA) testing, with high sensitivity but low specificity. If the tests support a positive suspicion, a transrectal ultrasound (TRUS) biopsy is performed[1]. A Pca diagnosis is classified as either clinically significant, with the adenocarcinoma lesion requiring surgical treatment to curb the risk of metastasis, or non-significant, with follow-up recommended[2-4].
Multiparametric magnetic resonance imaging (mpMRI) is gaining ground as a primary method for Pca diagnosis. However, the diagnostic process requires a radiologist who has deep experiential knowledge with both the disease and the MRI technology[1-3,5]. The Prostate Imaging-Reporting & Data System (PI-RADS; introduced in 2012) and the 2.1 update (2019, with improved sensitivity and specificity) has begun to standardize the process by providing a classification system for findings detectable in Pca[6-8].
The mpMRI technology itself has opened up new opportunities for more accurate and earlier Pca detection (and diagnosis). It is specifically recommended for patients with elevated PSA levels but negative biopsy results and for biopsy-naïve patients who are being monitored for Pca due to risk factors (e.g., age, family history, race). In addition, mpMRI is considered a safer alternative to the TRUS biopsy, as it avoids the complication risks related to the invasive biopsy procedure (e.g., bleeding, infection, urinary hesitancy)[4].
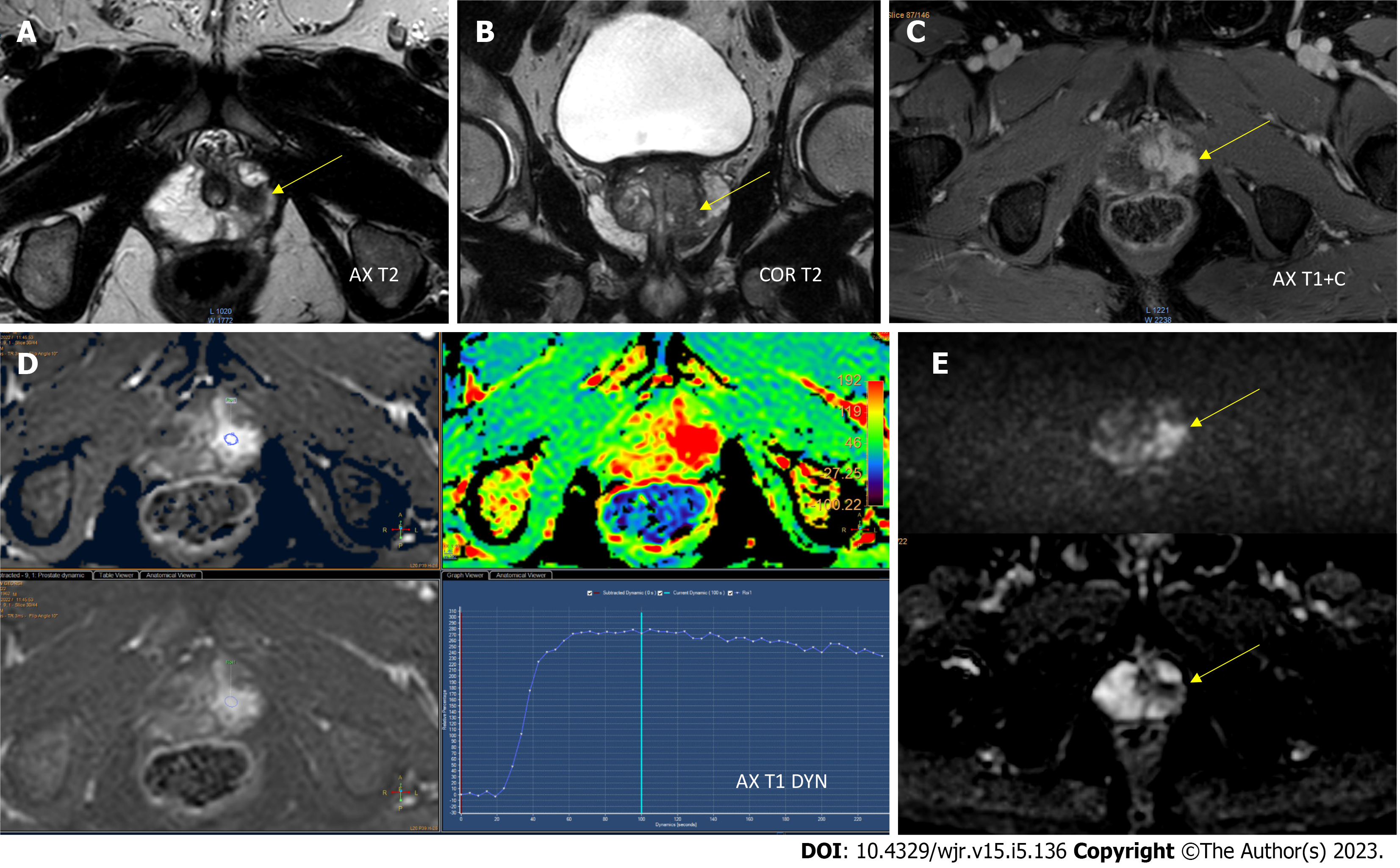
Three-dimensional images of the prostate gland, including high-resolution T2-weighted image (WI), diffusion-weighted image (DWI) and dynamic contrast-enhanced (DCE) image, are obtained using mpMRI (Figure 1). The imaging findings are combined with the overall clinical profile to determine the level of risk for a clinically significant cancer, following the PI-RADS classification[4].
American and European guidelines differ from each other in their recommendations for the appropriate time of biopsy[9]. Gleason staging has proven to be an accurate approach, but it (as well as the PI-RADS) has significant limitations in diagnosis and quantification; for example, the PI-RADS system is known to risk provision of an underestimation of tumor size, especially in patients with a low PI-RADS score, while higher PI-RADS score is associated with Gleason score upgrade[10]. In addition, the inherent heterogeneity of Pca, known limitations of mpMRI, and possible biopsy inaccuracies can lead to inconsistencies in the overall assessment of the patient's condition.
Currently, the detection of a prostate carcinoma lesion depends to a large extent on the experience of the radiologist, and in some cases even experienced radiologists find it difficult to detect the lesion or to classify the detected lesion by PI-RADS. In addition, in many cases, hypertrophy of the prostate with age makes it impossible to accurately localize the lesion and consequently hinders the surgeon’s ability to perform an accurate biopsy. It is also necessary to unify the description of a given lesion in relation to generally accepted templates. Fortunately, all these limitations can be overcome by the modern software technologies based on artificial intelligence (AI)[11].
The Pca detection process has its weaknesses at present. Indeed, prostate carcinoma lesions are often confused with prostatitis, benign nodules, or hemorrhagic nodules, especially in the transitional zone. This often results in unnecessary biopsies[12]. Another pitfall involves the histological assessment of the biopsied lesion, with inaccuracies resulting in dangerous false-negative findings or incorrect staging[13].
AI has been applied to various diseases in the fields of imaging diagnostics and pathological profiling, most often increasing the efficiency in evaluating results. Especially as with mpMRI, different AI-based solutions have been found to allow for accurate segmentation of the prostate as well as an accurate characterization of the tumors[14]. In the field of pathology, an improvement in diagnostics has also been observed. As with any disease that is managed clinically, a radiological-pathological correlation is required, and this presents an existing lacuna that AI can fill, and certainly biomarker data will play a role as well. Increased knowledge of the pathological mechanism, as can be supported by application of AI, is a crucial component to multidisciplinary clinical care (i.e. collaborative care teams of radiologists, pathologists, and urologists for Pca patients). Overall, this process of incorporating AI into any disease diagnosis will also aid in the discovery of hitherto hidden relationships between different pathology-related biomarkers[15,16].
AI is a computer system that performs actions similar to human intelligence. In radiology, AI has developed rapidly in recent years due to the ability of the cutting-edge technology to automatically extract information. Machine learning a subfield of AI is an algorithm that is trained for specific tasks without human intervention, which means that computers can be trained from certain examinations that have been previously described by a radiologist according to their didactic knowledge and practical experience. As more research data, including that involving AI, accumulates, the effectiveness of software increases. Human validation is still required, after which calibration is performed, resulting in better sensitivity and specificity of the novel/improved software. A subtype of machine learning is convolutional neural networks, where different systems interact with one another[17]. Of note, this type of system is the most frequently used in the development of AI[18].
AI has already shown great benefit in improving the detection, characterization, staging and participation in adequately treating Pca. Accurate prostate segmentation is particularly important when performing mpMRI, which without AI is relatively conditional on the perceptions of individual specialists. AI can be involved in the primary detection and staging of prostate carcinoma lesions relative to the PI-RADS system. A study by Cuocolo et al[14] published in 2021 investigated the characterization of human vs AI findings and demonstrated the benefit of the latter. In addition, AI can optimize the exact site for biopsy, as well as create a three-dimensional model to accurately represent the location of the tumor and its relationship to neighboring organs, improving preoperative preparation. Still other publications from recent years have shown regularity between the findings in T2, the changes in DWI, and the density of tissue composition, allowing for the creation of radiopathological maps[19-21].
AI has already proven its utility in other fields of medicine. For example, machine learning has been used in patients with appendicitis, emerging as a tool to predict whether the disease is acute or subacute; specifically, AI showed accurately predicted result in 83.75% of the cases, precision of 84.11%, sensitivity of 81.08%, and specificity of 81.01%[22]. In general, the ever-increasing role of precision medicine, the anticipated future improvements of machine learning and deep learning, and the ongoing expansion of robotics and radiomics are likely to facilitate the robust development of reproducible MRI-based prostatic diagnostics[23].
The greatest challenge to establishing AI in medical practice, at the moment, is the need for large volumes of data to be integrated into the AI systems. From a practical standpoint, this necessitates a large volume of time and effort from already-taxed radiologists with expertise in prostate imaging. Another challenge is that the collected data originate from different MRI devices made by various manufacturers with varying field strengths, and from studies performed using varying protocols. Ultimately, this means that studies should be grouped according to these varying features. Considering this issue, a study by Gaur et al[24] has shown the AI can not only reduce the time of interpretation of MRI findings from various machines but also improve the sensitivity (from 78% to 83.8% specifically), especially when radiologists with less experience in the field were using the technologies.
The diagnosis of Pca involves initial detection and accurate classification of the lesion(s) finding, and it is to these processes that software companies have directed their focus. AI systems are "trained" to detect cancer by inputting voluminous data from leading experts. Several groups are reporting various AI models for prostate segmentation, intraprostatic lesion detection and classification tasks with auspicious results[25].
Improvements are being sought in the detection of prostate carcinoma lesions that are invisible to human perception, thereby increasing early diagnosis[26-29]. In Table 1, the current AI products in the prostate field are summarized[30].
| Vendor | Product name | FDA approval class | CE approval class | Main features in prostate imaging |
| Siemens Healthineers | AI-Rad Companion Prostate MR | II | IIb - MDR | Segmentation, volume assessment, lesion annotation, PSA density |
| Quantib | Quantib® Prostate | II | IIb - MDR | Volume assessment, PSA density, segmentation, PI-RADS scoring, report structure |
| Quibim | QP-Prostate | II | IIb - MDR | ADC, Ktrans, parametric maps obtainment, volume assessment, segmentation, report structure |
| Quibim | Perfusion pharmacokinetics modeling | N/A | IIa - MDD | Ktrans map, volume assessment, contrast enhancement assistance |
| Quibim | Texture analysis | N/A | IIa - MDD | Quantification, radiomics, imaging biomarker discovery |
| Quibim | T2 mapping (relaxometry) | N/A | IIa - MDD | T2 values, T2 histogram |
| Siemens Healthineers | Prostate MR on syngo.via | N/A | IIa - MDD | Segmentation, volume assessment, lesion assessment, PI-RADS scoring |
| JLK Inc. | JPC-01K | N/A | I - MDD | Lesion detection |
| Lucida Medical | Prostate Intelligence™ | N/A | I - MDD | Segmentation, lesion characterization, PI-RADS scoring, report structure |
| Quibim | DWI - ADC | N/A | IIa - MDD | Volume assessment, ADC support, histogram |
| Quibim | DWI - IVIM | N/A | IIa - MDD | ADC support, multiparametric maps, perfusion assessment |
"AI-Rad companion prostate MR" by Siemens Medical Solutions (Malvern, PA, United States) aids the fusion between MRI and ultrasound. Performing an ultrasound-guided biopsy alone carries risks such as hemorrhage, infection, and abscessation. Furthermore, the procedure may not provide an answer to the presence of carcinoma in a given patient if performed solely, without previous physical examination and application of other imaging modalities. At the same time, performing an mpMRI scan cannot provide a histological diagnosis. The modern model of Pca diagnosis includes an ultrasound exa
Another Siemens product is the “Prostate MR” tool (Siemens Healthineers, Cary, NC, United States), which is available on the syngo.via workstation and is an AI that supports the evaluation of images obtained during a mpMRI scan. Analysis time needed for the AI is extremely short – between 3 sec and 10 sec. Prostate MR supports the primary detection and classification of findings, and offers description according to pre-entered standardized report templates. The use of this type of software is extremely valuable for training radiologists without experience in prostate diagnostics. Indeed, it has been reported that the software application leads to a reduction of false-positive results[32].
With the advent of mpMRI, the total number of examinations performed has increased significantly worldwide[33]. Radiologists today have to interpret multiple MRI scans of the prostate, but this requires great expertise in this challenging field. New guidelines from the European Association of Urology and the American Association of Radiology suggest that an MRI be performed before any biopsy is undertaken, and currently the number of prostate biopsies in the United States and Europe alone is over 3 million[33]. Eventual involvement of AI in the interpretation algorithm may improve the detection rate, accurate localization and risk stratification of patients with suspected Pca. “Quantib® Prostate” software (Quantib, Rotterdam, Netherlands) offers fast and automated segmentation of the prostate and detection of findings on the most used mpMRI sequences [T2WI, apparent diffusion coefficient (ADC), DWI, DCE]. The software also provides assistance in the PI-RADS classification of a discovery. Finally, with the help of the software, a standardized report can be written based on pre-created templates, thereby saving time and improving the quality of the report.
DCE perfusion imaging identifies tumors according to their vessel characteristics. The Pharmacokinetic Model used in Quantib® Prostate helps detect neoplasms and quantifies tumor neoan
"JPC-01K" (JLK Inc., Seoul, Korea) is a neural network-based software used to characterize tumors on mpMRI. This software aims to reduce the time needed to evaluate the prostate examination findings and assist in the description of such by providing quantitative analysis. It also aims to overcome the difficulties in image analysis, which are largely dependent on the radiologist and his/her qualifications and experience. The system uses mpMR images, T2WI, DWI, and DCE as input and visualizes the location of prostate carcinoma lesions and related probabilities. According to a study carried out in one center, the accuracy of the method was 99.65%, with a time required for analysis of only 2 min. The AI at this manufacturer undergoes constant improvement through the addition of new data from leading experts.
“Prostate Intelligence™” (Lucida Medical, Cambridge, United Kingdom) is AI-based software that allows prostate tumor detection on MR images. It is intended to augment a radiologist's interpretation of prostate MRI by providing a risk score and prostate segmentation, and aiding in lesion identification and segmentation. The processing time for this software is between 1 sec and 10 sec. The DWI algorithm by Quibim (Valencia, Spain) calculates the ADC. The suite provides information on the cellular and microstructural organization of tissues and highlights the relationship between pathological changes and the diffusion of water molecules. In addition, this suite aims to characterize tumoral processes to support early detection, diagnosis, treatment response evaluation and follow-up of patients.
The DWI algorithm by Quibim is also used to analyze the microstructure changes according to intra-voxel incoherent motion. The tool allows for the differentiation of pure diffusion changes due to variations in the vascular component and offers additional information complementary to conventional ADC results. This suite aims to characterize tumoral processes to support early detection, diagnosis, treatment response evaluation and follow-up of patients[31].
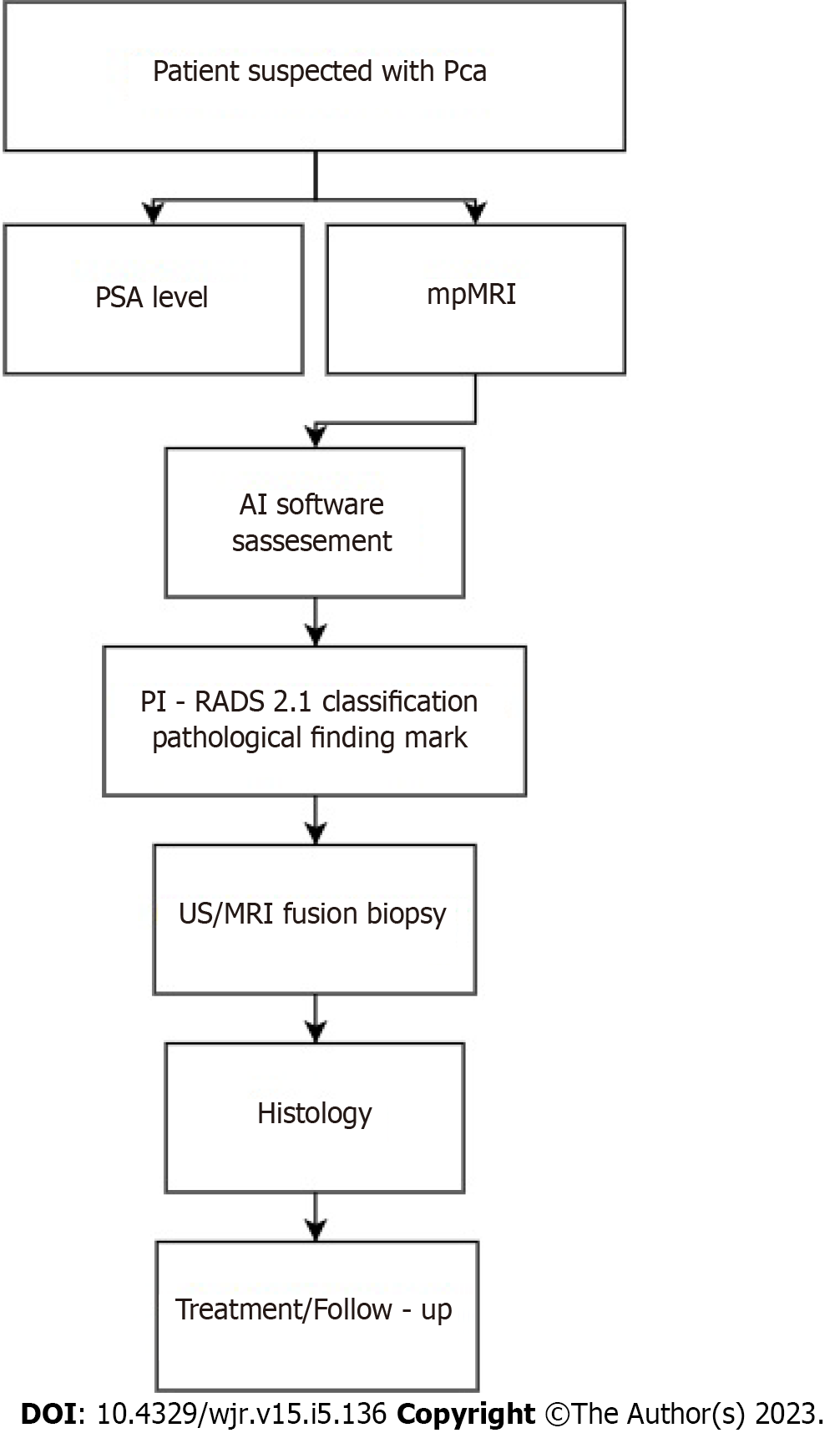
For timely detection, accurate diagnosis and proper treatment of the patient, we offer the algorithm presented in Figure 2.
Creating teams of radiologists and pathologists to jointly decide on the most accurate diagnosis and most effective and efficient treatment methods of patients with Pca would create a more efficient approach to clinical management of the disease to achieve the most successful outcome. With the help of AI, specialists from both fields can join forces, especially when making decisions about suspicious lesions classified as PI-RADS 3. It is possible to bring together in one system all critical components disease history, PSA levels, findings from imaging studies, genetic tests, laboratory tests, physical and histological exams, and treatment(s) performed. AI can facilitate the ability to analyze all these components and compare them to databases for risk stratification and better predictability[34,35].
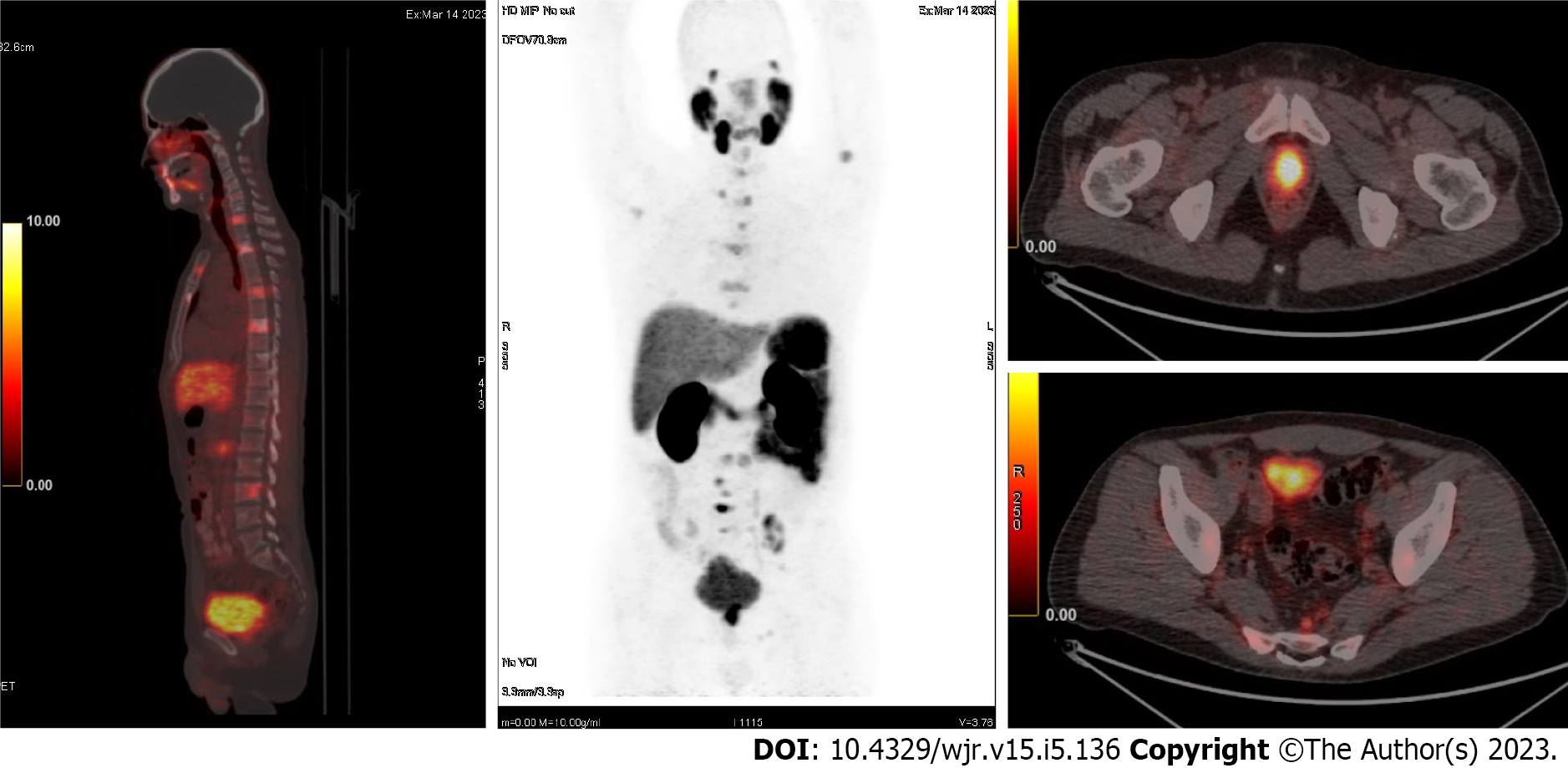
Unlike most other carcinomas, the application of 18F-fludeoxyglucose (FDG) in positron emission tomography/computed tomography (PET/CT) is limited for Pca, due to the low or missing glucose consumption that is typically presented by prostate carcinoma lesions. Thus, the use of specific targeting is required. Until recently, choline was considered a promising marker (since choline uptake/concentration is high in prostatic carcinoma lesion cells). While this radioactive indicator was originally used for staging of high-risk patients as well as re-staging after biochemical relapse, its low sensitivity led to its largely being abandoned. Other markers such as 11C-acetate, 18F-oorocyclobutan-1-carboxylic acid and 18F-uciclovire have been tested but have failed to meet expectations, presenting the same characteristics as choline and low sensitivity.
The prostate-specific membrane antigen (PSMA) currently dominates all other markers in PET scans for Pca. PSMA, also known as glutamate carboxypeptidase II, is a transmembrane glycoprotein, highly expressed in prostatic carcinoma lesion cells. PSMA expression tends to increase as Gleason score increases. So far, several 68gallium (68GA)-labeled ligands have been designed to target PSMA; these include PSMA-11 (known as Hbed-Cc or Hbed-PSMA), PSMA-I & T, and PSMA-617. Therefore, a
Multiple studies have shown that PET/CT with PSMA has a moderate sensitivity but a very high specificity for detecting metastases in lymph nodes and other organs. If the primary Pca shows PSMA expression, then a PSMA+ and PSMA- finding will be characterized as a secondary lesion or will be treated accordingly as a minor/benign lesion in the fragment imaging, although with the caveat of having high negative prognostic value. Due to the high monetary cost of PSMA studies, careful selection of patients suitable for examination is required. The mpMRI is superior for local assessment of the disease, and PSMA PET/MRI has an advantage in whole-body scanning. However, several restrictions are noted for patients suffering from Pca. For one, PET cameras are not always available and are missing in some of the nuclear medicine departments, especially in remote regions, for various logistical reasons. Another limitation is based in the fact that PSMA is not currently included in international guidelines. Lastly, although the utility of PSMA PET/CT in diagnosis of Pca is indisputable (outperforming diagnostics based solely on PSA, CT, and TRUS biopsy[36-40]) its role in monitoring of the disease remains unresolved.
Currently, only the “Pylarify AI™” software (Lantheus, Billerica, MA, United States) is legalized for support in PSMA PET/CT examinations, according to its demonstrated quantitative and accurate reporting. The AI software allows automated analysis of the CT examination’s findings and allowing for targeting of the hotspots[41,42].
The increased incidence of Pca in recent years and the improvement of MRI technologies have led to an increase in the number of the examinations performed on patients for diagnosis of the disease. The larger volume of data that has resulted, combined with the insufficient number and/or insufficiently trained personnel, has unfortunately complicated the clinical process and management of these patients. AI is a powerful modern tool that offers benefits of time reduction and improved quality and accuracy of interpretation of prostatic carcinoma lesion findings according to the unified PI-RADS system. AI application to the field of radiological imaging may revolutionize the approach to Pca patients. However, there is still a long way to go until we are able to fully calibrate the individual components of the new AI-based software solutions and carry out accurate and thorough studies in this arena to gain a comprehensive understanding of the pathology of the disease and clinical care benefits of this powerful tool.
The authors are grateful for the support provided by NextGenerationEU.
| 1. | Ferlay J, Colombet M, Soerjomataram I, Mathers C, Parkin DM, Piñeros M, Znaor A, Bray F. Estimating the global cancer incidence and mortality in 2018: GLOBOCAN sources and methods. Int J Cancer. 2019;144:1941-1953. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3585] [Cited by in RCA: 5056] [Article Influence: 632.0] [Reference Citation Analysis (2)] |
| 2. | Fenton JJ, Weyrich MS, Durbin S, Liu Y, Bang H, Melnikow J. Prostate-Specific Antigen-Based Screening for Prostate Cancer: Evidence Report and Systematic Review for the US Preventive Services Task Force. JAMA. 2018;319:1914-1931. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 259] [Cited by in RCA: 396] [Article Influence: 49.5] [Reference Citation Analysis (0)] |
| 3. | Hayes JH, Barry MJ. Screening for prostate cancer with the prostate-specific antigen test: a review of current evidence. JAMA. 2014;311:1143-1149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 290] [Cited by in RCA: 254] [Article Influence: 21.2] [Reference Citation Analysis (0)] |
| 4. | Doykov M, Chervenkov, L. , Tsvetkova-Trichkova, S., Doykova, K., Georgiev, A. Assessment of the Utility of Multiparametric Magnetic Resonance Imaging for Initial Detection of Prostate Cancer. Macedonian Journal of Medical Sciences. 2022;10:1840-1845. [RCA] [DOI] [Full Text] [Reference Citation Analysis (1)] |
| 5. | Barbieri CE, Bangma CH, Bjartell A, Catto JW, Culig Z, Grönberg H, Luo J, Visakorpi T, Rubin MA. The mutational landscape of prostate cancer. Eur Urol. 2013;64:567-576. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 138] [Cited by in RCA: 170] [Article Influence: 13.1] [Reference Citation Analysis (0)] |
| 6. | Rosenkrantz AB, Ayoola A, Hoffman D, Khasgiwala A, Prabhu V, Smereka P, Somberg M, Taneja SS. The Learning Curve in Prostate MRI Interpretation: Self-Directed Learning Versus Continual Reader Feedback. AJR Am J Roentgenol. 2017;208:W92-W100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 77] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 7. | Turkbey B, Rosenkrantz AB, Haider MA, Padhani AR, Villeirs G, Macura KJ, Tempany CM, Choyke PL, Cornud F, Margolis DJ, Thoeny HC, Verma S, Barentsz J, Weinreb JC. Prostate Imaging Reporting and Data System Version 2.1: 2019 Update of Prostate Imaging Reporting and Data System Version 2. Eur Urol. 2019;76:340-351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 711] [Cited by in RCA: 1750] [Article Influence: 250.0] [Reference Citation Analysis (0)] |
| 8. | Georgiev A, Chervenkov L, Doykov M, Doykova K, Uchikov P, Tsvetkova S. Surveillance Value of Apparent Diffusion Coefficient Maps: Multiparametric MRI in Active Surveillance of Prostate Cancer. Cancers (Basel). 2023;15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Reference Citation Analysis (0)] |
| 9. | Schoots IG, Padhani AR. Delivering Clinical impacts of the MRI diagnostic pathway in prostate cancer diagnosis. Abdom Radiol (NY). 2020;45:4012-4022. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 21] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 10. | Pooli A, Johnson DC, Shirk J, Markovic D, Sadun TY, Sisk AE Jr, Mohammadian Bajgiran A, Afshari Mirak S, Felker ER, Hughes AK, Raman SS, Reiter RE. Predicting Pathological Tumor Size in Prostate Cancer Based on Multiparametric Prostate Magnetic Resonance Imaging and Preoperative Findings. J Urol. 2021;205:444-451. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 49] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 11. | Aggarwal K. Machine Learning, and Deep Learning. Iraqi Journal for Computer Science and Mathematics. 2022;3:115-123. [DOI] [Full Text] |
| 12. | Loeb S, Vellekoop A, Ahmed HU, Catto J, Emberton M, Nam R, Rosario DJ, Scattoni V, Lotan Y. Systematic review of complications of prostate biopsy. Eur Urol. 2013;64:876-892. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 594] [Cited by in RCA: 767] [Article Influence: 59.0] [Reference Citation Analysis (0)] |
| 13. | Etzioni R, Penson DF, Legler JM, di Tommaso D, Boer R, Gann PH, Feuer EJ. Overdiagnosis due to prostate-specific antigen screening: lessons from U.S. prostate cancer incidence trends. J Natl Cancer Inst. 2002;94:981-990. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 670] [Cited by in RCA: 662] [Article Influence: 27.6] [Reference Citation Analysis (0)] |
| 14. | Cuocolo R, Cipullo MB, Stanzione A, Romeo V, Green R, Cantoni V, Ponsiglione A, Ugga L, Imbriaco M. Machine learning for the identification of clinically significant prostate cancer on MRI: a meta-analysis. Eur Radiol. 2020;30:6877-6887. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 76] [Article Influence: 12.7] [Reference Citation Analysis (0)] |
| 15. | Goldenberg SL, Nir G, Salcudean SE. A new era: artificial intelligence and machine learning in prostate cancer. Nat Rev Urol. 2019;16:391-403. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 153] [Cited by in RCA: 272] [Article Influence: 45.3] [Reference Citation Analysis (0)] |
| 16. | Raciti P, Sue J, Ceballos R, Godrich R, Kunz JD, Kapur S, Reuter V, Grady L, Kanan C, Klimstra DS, Fuchs TJ. Novel artificial intelligence system increases the detection of prostate cancer in whole slide images of core needle biopsies. Mod Pathol. 2020;33:2058-2066. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 122] [Article Influence: 20.3] [Reference Citation Analysis (0)] |
| 17. | Park SH, Han K. Methodologic Guide for Evaluating Clinical Performance and Effect of Artificial Intelligence Technology for Medical Diagnosis and Prediction. Radiology. 2018;286:800-809. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 467] [Cited by in RCA: 533] [Article Influence: 66.6] [Reference Citation Analysis (0)] |
| 18. | Yilmaz EC, Belue MJ, Turkbey B, Reinhold C, Choyke PL. A Brief Review of Artificial Intelligence in Genitourinary Oncological Imaging. Can Assoc Radiol J. 2022;8465371221135782. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 19. | McGarry SD, Hurrell SL, Iczkowski KA, Hall W, Kaczmarowski AL, Banerjee A, Keuter T, Jacobsohn K, Bukowy JD, Nevalainen MT, Hohenwalter MD, See WA, LaViolette PS. Radio-pathomic Maps of Epithelium and Lumen Density Predict the Location of High-Grade Prostate Cancer. Int J Radiat Oncol Biol Phys. 2018;101:1179-1187. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44] [Cited by in RCA: 46] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 20. | Chatterjee A, Bourne RM, Wang S, Devaraj A, Gallan AJ, Antic T, Karczmar GS, Oto A. Diagnosis of Prostate Cancer with Noninvasive Estimation of Prostate Tissue Composition by Using Hybrid Multidimensional MR Imaging: A Feasibility Study. Radiology. 2018;287:864-873. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 92] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 21. | Chatterjee A, Watson G, Myint E, Sved P, McEntee M, Bourne R. Changes in Epithelium, Stroma, and Lumen Space Correlate More Strongly with Gleason Pattern and Are Stronger Predictors of Prostate ADC Changes than Cellularity Metrics. Radiology. 2015;277:751-762. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 110] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 22. | Mijwil MM, Aggarwal K. A diagnostic testing for people with appendicitis using machine learning techniques. Multimed Tools Appl. 2022;81:7011-7023. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 29] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 23. | Hamm CA, Beetz NL, Savic LJ, Penzkofer T. [Artificial intelligence and radiomics in MRI-based prostate diagnostics]. Radiologe. 2020;60:48-55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 24. | Gaur S, Lay N, Harmon SA, Doddakashi S, Mehralivand S, Argun B, Barrett T, Bednarova S, Girometti R, Karaarslan E, Kural AR, Oto A, Purysko AS, Antic T, Magi-Galluzzi C, Saglican Y, Sioletic S, Warren AY, Bittencourt L, Fütterer JJ, Gupta RT, Kabakus I, Law YM, Margolis DJ, Shebel H, Westphalen AC, Wood BJ, Pinto PA, Shih JH, Choyke PL, Summers RM, Turkbey B. Can computer-aided diagnosis assist in the identification of prostate cancer on prostate MRI? a multi-center, multi-reader investigation. Oncotarget. 2018;9:33804-33817. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 76] [Cited by in RCA: 68] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 25. | Belue MJ, Turkbey B. Tasks for artificial intelligence in prostate MRI. Eur Radiol Exp. 2022;6:33. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 22] [Reference Citation Analysis (0)] |
| 26. | Winkel DJ, Wetterauer C, Matthias MO, Lou B, Shi B, Kamen A, Comaniciu D, Seifert HH, Rentsch CA, Boll DT. Autonomous Detection and Classification of PI-RADS Lesions in an MRI Screening Population Incorporating Multicenter-Labeled Deep Learning and Biparametric Imaging: Proof of Concept. Diagnostics (Basel). 2020;10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 37] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 27. | Aldoj N, Lukas S, Dewey M, Penzkofer T. Semi-automatic classification of prostate cancer on multi-parametric MR imaging using a multi-channel 3D convolutional neural network. Eur Radiol. 2020;30:1243-1253. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 85] [Article Influence: 12.1] [Reference Citation Analysis (0)] |
| 28. | Mehralivand S, Yang D, Harmon SA, Xu D, Xu Z, Roth H, Masoudi S, Sanford TH, Kesani D, Lay NS, Merino MJ, Wood BJ, Pinto PA, Choyke PL, Turkbey B. A Cascaded Deep Learning-Based Artificial Intelligence Algorithm for Automated Lesion Detection and Classification on Biparametric Prostate Magnetic Resonance Imaging. Acad Radiol. 2022;29:1159-1168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 53] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 29. | Winkel DJ, Tong A, Lou B, Kamen A, Comaniciu D, Disselhorst JA, Rodríguez-Ruiz A, Huisman H, Szolar D, Shabunin I, Choi MH, Xing P, Penzkofer T, Grimm R, von Busch H, Boll DT. A Novel Deep Learning Based Computer-Aided Diagnosis System Improves the Accuracy and Efficiency of Radiologists in Reading Biparametric Magnetic Resonance Images of the Prostate: Results of a Multireader, Multicase Study. Invest Radiol. 2021;56:605-613. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 83] [Article Influence: 16.6] [Reference Citation Analysis (0)] |
| 30. | Greer MD, Shih JH, Lay N, Barrett T, Bittencourt L, Borofsky S, Kabakus I, Law YM, Marko J, Shebel H, Merino MJ, Wood BJ, Pinto PA, Summers RM, Choyke PL, Turkbey B. Interreader Variability of Prostate Imaging Reporting and Data System Version 2 in Detecting and Assessing Prostate Cancer Lesions at Prostate MRI. AJR Am J Roentgenol. 2019;212:1197-1205. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 90] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 31. | Strohm L, Hehakaya C, Ranschaert ER, Boon WPC, Moors EHM. Implementation of artificial intelligence (AI) applications in radiology: hindering and facilitating factors. Eur Radiol. 2020;30:5525-5532. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 155] [Article Influence: 25.8] [Reference Citation Analysis (0)] |
| 32. | Yu X. False Positive Reduction Using Multiscale Contextual Features for Prostate Cancer Detection in Multi-Parametric MRI Scans. IEEE 17th International Symposium on Biomedical Imaging (ISBI). 2020;1355-1359. [DOI] [Full Text] |
| 33. | Mottet N, van den Bergh RCN, Briers E, Van den Broeck T, Cumberbatch MG, De Santis M, Fanti S, Fossati N, Gandaglia G, Gillessen S, Grivas N, Grummet J, Henry AM, van der Kwast TH, Lam TB, Lardas M, Liew M, Mason MD, Moris L, Oprea-Lager DE, van der Poel HG, Rouvière O, Schoots IG, Tilki D, Wiegel T, Willemse PM, Cornford P. EAU-EANM-ESTRO-ESUR-SIOG Guidelines on Prostate Cancer-2020 Update. Part 1: Screening, Diagnosis, and Local Treatment with Curative Intent. Eur Urol. 2021;79:243-262. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 606] [Cited by in RCA: 2006] [Article Influence: 334.3] [Reference Citation Analysis (0)] |
| 34. | van Wijk Y, Halilaj I, van Limbergen E, Walsh S, Lutgens L, Lambin P, Vanneste BGL. Decision Support Systems in Prostate Cancer Treatment: An Overview. Biomed Res Int. 2019;2019:4961768. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 14] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 35. | Lee G, Singanamalli A, Wang H, Feldman MD, Master SR, Shih NN, Spangler E, Rebbeck T, Tomaszewski JE, Madabhushi A. Supervised multi-view canonical correlation analysis (sMVCCA): integrating histologic and proteomic features for predicting recurrent prostate cancer. IEEE Trans Med Imaging. 2015;34:284-297. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 48] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 36. | Hahn P, Smith IC, Leboldus L, Littman C, Somorjai RL, Bezabeh T. The classification of benign and malignant human prostate tissue by multivariate analysis of 1H magnetic resonance spectra. Cancer Res. 1997;57:3398-3401. [PubMed] |
| 37. | Tsechelidis I, Vrachimis A. PSMA PET in Imaging Prostate Cancer. Front Oncol. 2022;12:831429. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 47] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 38. | Siva S, Udovicich C, Tran B, Zargar H, Murphy DG, Hofman MS. Expanding the role of small-molecule PSMA ligands beyond PET staging of prostate cancer. Nat Rev Urol. 2020;17:107-118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 45] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 39. | Zamboglou C, Carles M, Fechter T, Kiefer S, Reichel K, Fassbender TF, Bronsert P, Koeber G, Schilling O, Ruf J, Werner M, Jilg CA, Baltas D, Mix M, Grosu AL. Radiomic features from PSMA PET for non-invasive intraprostatic tumor discrimination and characterization in patients with intermediate- and high-risk prostate cancer - a comparison study with histology reference. Theranostics. 2019;9:2595-2605. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 63] [Cited by in RCA: 106] [Article Influence: 15.1] [Reference Citation Analysis (0)] |
| 40. | Nishino M, Hayakawa K, Minami M, Yamamoto A, Ueda H, Takasu K. Primary retroperitoneal neoplasms: CT and MR imaging findings with anatomic and pathologic diagnostic clues. Radiographics. 2003;23:45-57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 211] [Cited by in RCA: 165] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 41. | Nickols N, Anand A, Johnsson K, Brynolfsson J, Borreli P, Parikh N, Juarez J, Jafari L, Eiber M, Rettig M. aPROMISE: A Novel Automated PROMISE Platform to Standardize Evaluation of Tumor Burden in (18)F-DCFPyL Images of Veterans with Prostate Cancer. J Nucl Med. 2022;63:233-239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 46] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 42. | Johnsson K, Brynolfsson J, Sahlstedt H, Nickols NG, Rettig M, Probst S, Morris MJ, Bjartell A, Eiber M, Anand A. Analytical performance of aPROMISE: automated anatomic contextualization, detection, and quantification of [(18)F]DCFPyL (PSMA) imaging for standardized reporting. Eur J Nucl Med Mol Imaging. 2022;49:1041-1051. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 44] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: European Society of Radiology (ESR); Bulgarian Association of Radiology (BAR); European Society of Uroradiology (ESUR); European Society of Gastroabdominal Radiology (ESGAR).
Specialty type: Radiology, nuclear medicine and medical imaging
Country/Territory of origin: Bulgaria
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Konovalov AB, Russia; Lei Y, China; Mijwil MM, Iraq S-Editor: Liu XF L-Editor: Filipodia P-Editor: Zhao S