INTRODUCTION
Since December 2019, the world has witnessed the emergence and unrelenting spread of coronavirus disease 2019 (COVID-19) with its devastating impact on global public health. As of February 3, 2021, there have been 103 million confirmed cases worldwide and over 2.2 million deaths[1]. Although in the majority of cases, the disease manifests with respiratory symptoms such as fever, cough, and dyspnea, its extra-pulmonary manifestations due to multi-system involvement are being increasingly recognized[2]. Particularly, the incidence of gastrointestinal (GI) manifestations such as abdominal pain, nausea, vomiting, and diarrhea has varied from 12% to as much as 61% in patients with COVID-19[3-5]. GI tract involvement in COVID-19 is believed to be a direct consequence of tissue damage mediated by the virus and additionally due to inflammation-mediated cytotoxicity[6,7]. About 10% of patients with COVID-19 could manifest only with GI symptoms without co-existing respiratory symptoms, which could result in delayed diagnosis. Moreover, COVID-19 patients presenting with GI symptoms tend to progress to a severe form of disease with poor outcomes. This subset of patients requires greater attention for early identification of complications[5].
The pulmonary imaging features of COVID-19 have been extensively described in the literature, an understanding of which has provided a greater insight into the pathophysiology of the disease. In comparison, there is a paucity of literature with respect to the various GI imaging manifestations of COVID-19. Considering the high likelihood of GI tract involvement in COVID-19, it is becoming increasingly important for radiologists to be aware of the variety of abdominal imaging findings in patients with COVID-19. Early recognition of these features can facilitate timely management of COVID-19 associated complications as well as alert the treating physician to consider a diagnosis of COVID-19 in patients presenting with atypical symptoms. Moreover, knowledge of these imaging findings may enhance our understanding of the pathophysiology of GI phenomena in the novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection.
The aim of this article is to share our experience with the spectrum of GI manifestations that can be encountered in patients with COVID-19.
METHODOLOGY OF LITERATURE SEARCH
We performed a systematic review of the literature, in order to identify all published articles on patients with abdominal manifestations due to COVID-19. We conducted literature searches in PubMed/MEDLINE, EMBASE, and Google Scholar bibliographic databases, spanning the years 2019 to 2021. The keywords “abdominal”, “COVID-19”, “imaging”, and “radiology” were used in all possible combinations. We also performed specific searches pertaining to involvement of particular organs/systems, using keywords such as “colonic“, “small bowel”, “pancreas”, “gall bladder”, and “renal” in combination with “COVID-19” and “imaging”. Additionally, since thrombotic events are recognized as a major complication of the infection, we also searched for the literature pertaining to these, in the context of GI involvement, using the keywords “thrombosis”, “abdomen”, “imaging”, “infarction”, “gangrene”, and “COVID-19” in various combinations. Moreover, the reference lists of all relevant publications were reviewed for additional articles.
All publications pertinent to our research subject such as scientific studies, review articles, case series, and case reports were included in our literature search. These were carefully evaluated by two of the authors, to identify the relevant radiologic findings in these cases for inclusion in our literature review. Articles without full-text availability and those without details of radiologic evaluation were excluded.
With regards to our experience, considering this was an in-between pandemic, single-centre, imaging review of the GI manifestations of COVID-19 infection, we had a small cohort of patients under investigation. As compared to the large sample of COVID-19 RT-PCR positive patients presenting with respiratory complaints, fewer COVID-19 cases presented with GI symptoms. This small cohort was investigated by means of imaging and biochemical tests and appropriate treatment was instituted. The data pertaining to this particular cohort was retrieved from the patient database and was studied retrospectively. The imaging studies for each of these cases were reviewed. The relevant radiologic findings and clinical details were compiled for the purpose of this review. This review article is thus, based on our experience in a COVID centre as well as that of other researchers, elucidated by means of scientific studies and case reports. Based on all of these observations, we recommend a large-scale multicentre study based on a bigger sample size, to ascertain the statistical significance of our findings and to understand whether GI affection constitutes a statistically significant percentage in patients with COVID-19.
We will review the GI imaging manifestations of COVID-19 under the following sub-headings: Small and large bowel abnormalities; vascular occlusion and solid organ infarction; hepato-biliary involvement; pancreatic involvement; and bleeding complications.
SMALL AND LARGE BOWEL ABNORMALITIES
Large bowel thickening/colitis
The occurrence of GI symptoms in a COVID-19 patient, such as diarrhoea, hematochezia, or abdominal pain, may warrant a computed tomography (CT) evaluation for GI tract assessment. Various mechanisms have been implicated in GI tract involvement by the SARS-CoV-2[8]. Direct infection of the GI tract epithelial cells by binding to the angiotensin-converting enzyme-2 (ACE-2) surface receptors followed by viral replication and cell destruction and alternatively, cell injury resulting from an inflammatory response to the virus-infected cells could account for the GI manifestations of COVID-19[9,10]. A few cases of large bowel infection with SARS-CoV-2 have been reported, which on imaging, manifest with diffuse, circumferential, homogeneously enhancing bowel wall thickening in a variable distribution[11,12]. The wall thickening may involve one or more segments of the colon. In our experience and as described by other researchers, the bowel wall thickening is not associated with pericolic lymphadenopathy, pneumatosis, or ileus. In our institute, we encountered a patient with bloody diarrhea in whom contrast-enhanced CT (CECT) revealed homogeneously enhancing wall thickening involving the sigmoid colon (Figure 1). Owing to the rarity of isolated viral colitis, it is important to exclude signs of ischemia such as decreased/ absent wall enhancement, poor opacification of the mesenteric vascular arcade, and filling defects suggestive of thrombi in the abdominal arteries, so as to enable early identification of ischemic colitis. The absence of classical imaging features of inflammatory bowel disease like the “comb” sign, mural stratification, fibrofatty proliferation could prompt the consideration of infection as a probable cause of colitis[13]. The detection of SARS-CoV-2 RNA in the stool may conclusively establish the diagnosis. Colonoscopy is generally not indicated in uncomplicated infectious colitis, unless the patient presents with unusual manifestations such as severe GI bleeding[14].
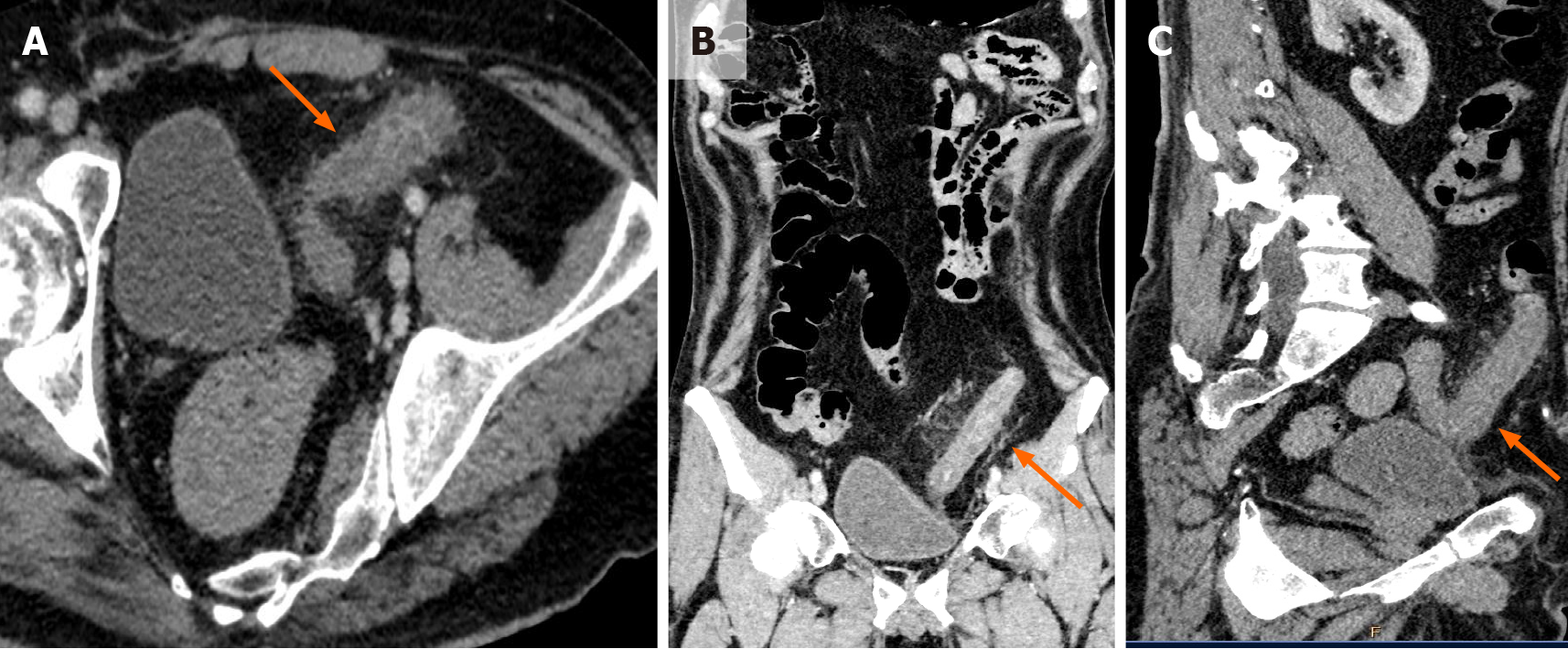
Figure 1 Contrast enhanced computed tomography imaging in a patient with coronavirus disease 2019 presenting with bloody diarrhea.
A: Axial; B: Coronal; C: Sagittal. Contrast enhanced computed tomography images of the abdomen and pelvis show diffuse edematous wall thickening involving the sigmoid colon (orange arrows in A, B, and C). Associated pericolic fat stranding is seen. In the absence of other causes of bowel wall thickening, a diagnosis of viral colitis was considered.
Acute mesenteric ischemia and enteric perforation
Patients with COVID-19 presenting with severe GI symptoms associated with abdominal distention, decreased bowel sounds, or worsening systemic status should alert the treating physician to the possibility of acute mesenteric ischemia, a potentially fatal complication of the disease[15]. Ischemia may occur as a result of hypercoagulability as a consequence of systemic inflammation, elevation of von Willebrand Factor levels secondary to endothelial damage induced by viral binding to ACE-2 surface receptors, or direct insult to enterocytes by the coronavirus itself[16,17]. An increase in D-dimer and lactate levels in the blood could indicate an ischemic complication, but these lack specificity[18]. Radiologic evaluation has a crucial role in the timely detection of acute mesenteric ischemia (AMI) and is the cornerstone of diagnosis. Abdominal radiography has a limited role in the evaluation of bowel ischemia, owing to its low sensitivity and specificity[19]. Ultrasonography (US), despite its ready availability and absence of radiation exposure, is also relatively non-specific for the diagnosis. Screening US may reveal decreased peristalsis, inter-bowel fluid, and/or excessive intra-luminal contents indicating stasis. However, its utility is limited if the patient is obese or has pneumoperitoneum or an excessive amount of bowel gas[20]. Moreover, these findings lack sensitivity and specificity for the diagnosis.
Computed tomography angiography remains the mainstay for definitive diagnosis of AMI[21]. Thrombi or emboli manifest as filling defects within the lumen of the abdominal aorta and its branches, namely, the celiac axis, superior mesenteric artery (SMA), and inferior mesenteric artery. Poor contrast opacification of the mesenteric vascular arcade on angiography images is indicative of hypoperfusion[22]. In our experience, this finding is well seen on maximum intensity projection (MIP) coronal images (Figure 2). Accordingly, the segment of the injured small bowel reveals wall thickening secondary to mural edema; this is the most frequently observed CT finding in AMI[23]. A very specific finding for AMI is absent or decreased contrast enhancement of the bowel wall. A target appearance of the bowel wall, representing mucosal hyperemia with surrounding mural edema, can be seen in ischemic colitis and after reperfusion following arterial occlusion. Disruption of normal bowel peristalsis leads to dilatation of the bowel lumen (> 3 cm); the dilated bowel may contain fluid, air, or both. In the late phase, thinning of the bowel wall is evident; the wall may not be discernible in some segments, thus appearing “paper thin” and featureless due to loss of normal tone. Eventually, transmural infarction leads to pneumatosis intestinalis/air in the bowel wall, followed by porto-mesenteric venous gas, pneumoperitoneum, and free fluid in the peritoneal cavity, due to extravasation of intra-luminal fluid and as a result of the peritoneal reaction to the bowel ischemia[24].
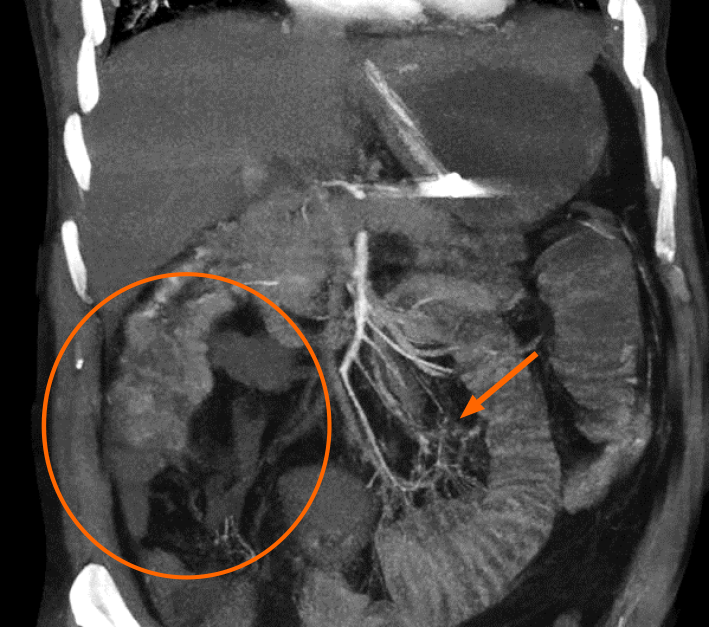
Figure 2 Acute mesenteric ischemia diagnosed on computed tomography mesenteric angiography performed in a critical patient with coronavirus disease 2019 presenting with severe abdominal pain.
The coronal maximum intensity projection image reveals a lack of opacification of the right sided branches of the superior mesenteric artery (SMA), namely, the ileo-colic and right colic branches (orange circle). The distal branches of the SMA also appear hypoperfused (orange arrow). Imaging features are consistent with SMA thrombosis.
Various investigators have reported AMI in critically ill patients with COVID-19, and the vast majority of patients were diagnosed in the late phase of AMI manifesting with frank perforation and pneumoperitoneum[25-29].
We encountered two cases of AMI as a complication of COVID-19 in our practice. Both patients were being treated for severe viral pneumonia in the intensive care unit. During the course of their treatment, they presented with abdominal distension, vomiting, and intractable abdominal pain. Clinical examination revealed diffuse abdominal tenderness, hypotension, and tachycardia, prompting the need for urgent imaging. On CT imaging, our first patient presented with frank jejunal perforation with pneumoperitoneum (Figure 3), thus requiring emergent laparotomy. In the second case, CT angiography revealed absent mural enhancement of distal ileal loops with barely discernible walls, suggestive of bowel gangrene (Figure 4). The proximal small bowel loops appeared dilated with air-fluid levels within. Thrombotic macro-vascular arterial occlusion was detected in the form of non-opacification of the ileo-colic branches of the SMA (Figure 2). Consequently, superior mesenteric artery thrombectomy with resection of the gangrenous bowel was performed. Both patients required prolonged supportive care but survived. Based on this experience, we believe that a high index of suspicion for AMI accompanied by prompt imaging play a key role in decreasing morbidity and mortality. Owing to the high mortality rate in the event of this devastating complication, a thorough understanding of the pathophysiology and clinical presentation of AMI as well as familiarity with the imaging features is of utmost importance to make a timely diagnosis so as to decrease morbidity and mortality.
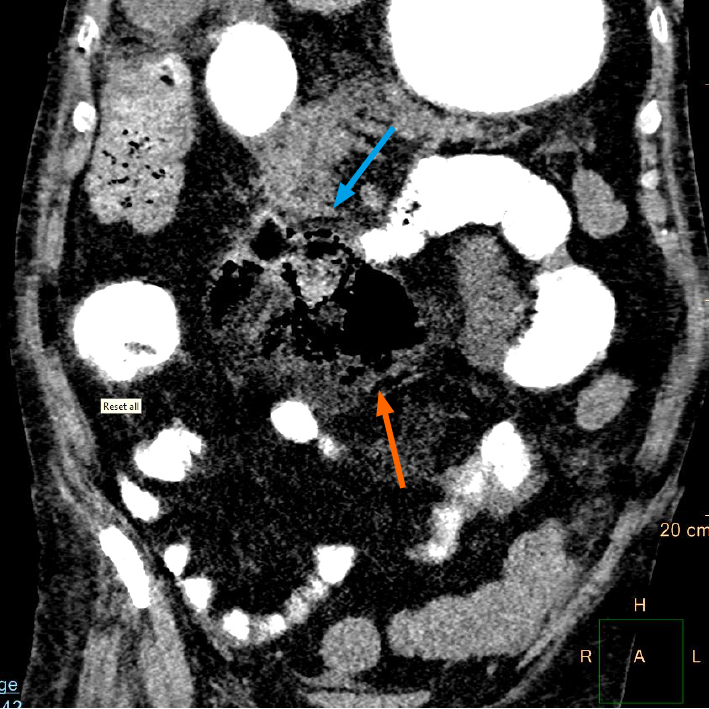
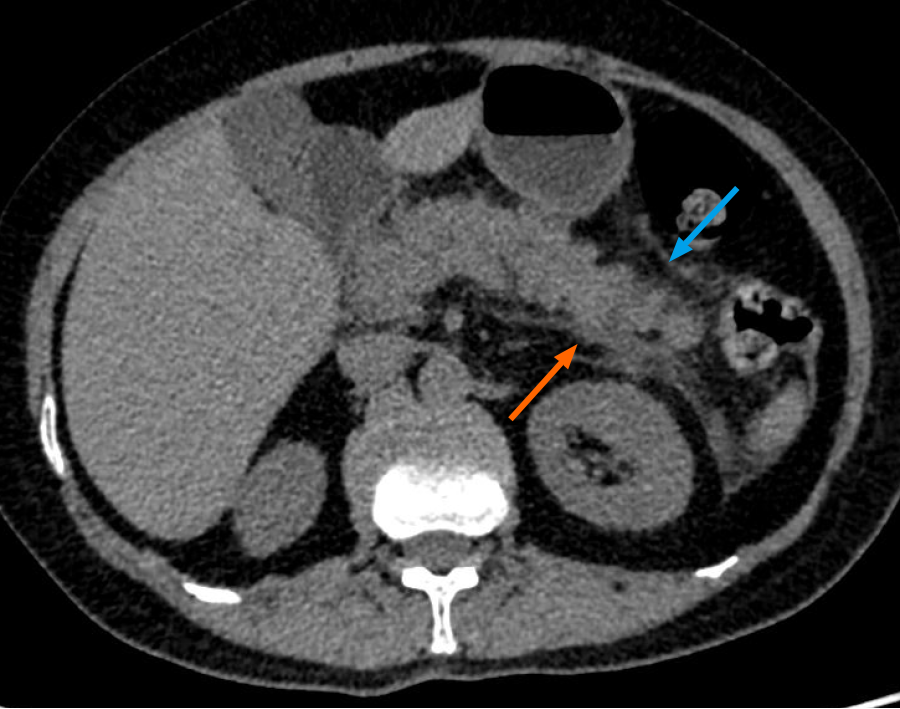
Figure 3 Bowel perforation detected on a computed tomography scan of the abdomen and pelvis performed for evaluation of severe abdominal pain and abdominal distension in a critical patient with coronavirus disease 2019.
Positive oral contrast is seen to opacify small and large bowel loops. There is evidence of jejunal perforation with a localized air collection in the mesentery (orange arrow) at the site and adjacent inflammation (blue arrow). The proximal jejunal loops appear dilated. The patient underwent emergency laparotomy with resection and anastomosis.
Figure 4 Small bowel ischemia detected on computed tomography mesenteric angiography study performed in a coronavirus disease 2019 patient presenting with severe abdominal pain and abdominal distension.
A and B: Axial contrast enhanced computed tomography (CT) images of the abdomen and pelvis; C: Sagittal contrast enhanced CT images of the abdomen and pelvis, showing dilated distal ileal loops in the right iliac fossa with non-enhancing, barely discernible walls suggestive of bowel gangrene (blue arrows in A, B, and C). The proximal small bowel loops appear dilated with air-fluid levels within, suggestive of stasis (orange arrow in B).
THROMBO-EMBOLIC PHENOMENA AND SOLID ORGAN INFARCTION
Over the past couple of months, an increasing number of reports have emerged highlighting the high incidence of thrombotic events in patients with coronavirus disease[30,31]. The state of hypercoagulability occurring in COVID-19 patients is believed to be mediated by a combination of inflammation, endothelial damage, and/or vascular injury[6]. Considering the likelihood of pro-thrombotic complications, it is justifiable to perform a contrast enhanced CT scan of the thorax and the abdomen, including the arterial and venous phases, in case of suspected pulmonary embolism or patients presenting with unexplained abdominal pain[32]. Many venous thromboembolic events have been documented in association with COVID-19 (Figure 5), whereas arterial thrombosis has been described in relatively fewer cases and could possibly be underestimated[33]. COVID-19 associated arterial thrombosis has been frequently observed in non-atherosclerotic vessels on CT imaging[34], suggesting that patients with a severe inflammatory reaction as indicated by elevation of D-dimer, fibrin degradation products, and platelet count coupled with decreased antithrombin values are at greater risk for thrombo-embolic phenomena[35].
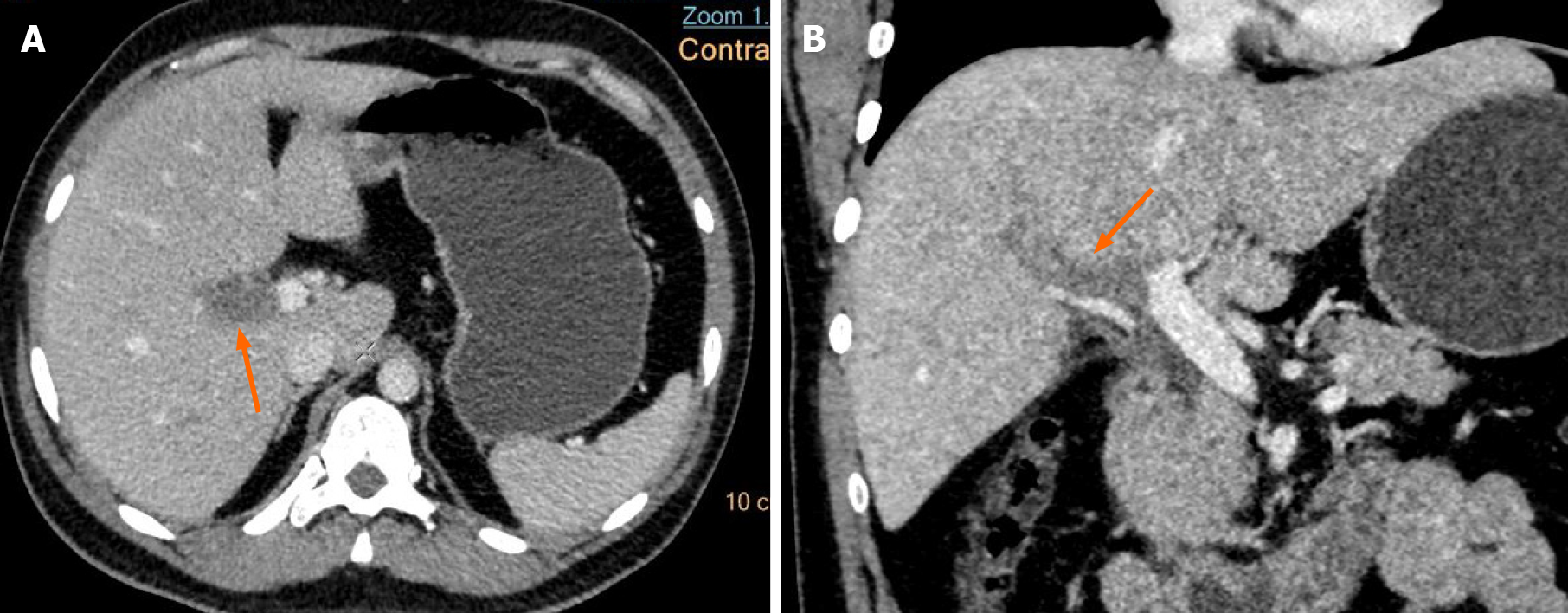
Figure 5 Venous thrombosis diagnosed in a coronavirus disease 2019 patient presenting with abdominal pain.
A: Axial; B: Coronal. Contrast enhanced computed tomography (CT) images of the abdomen show a hypodense filling defect in the main portal vein at the hilum extending into the right branch (orange arrows in A and B), suggestive of portal vein thrombosis. There were no features of mesenteric ischemia seen on the CT.
Solid organ infarction in COVID-19 could either be incidentally detected on CT imaging or could manifest with abdominal pain or features of organ dysfunction. Few reports of COVID-19 associated renal infarction have emerged; some of these manifesting with acute kidney injury. CECT that includes the arterial and venous phases is the study of choice for the recognition of kidney infarction. Ultrasound of the kidneys has a limited role in the detection of infarction due to its lower sensitivity and specificity[36].
Renal infarcts are well demonstrated preferably in the arterial phase; they manifest as solitary or multiple, discrete, wedge-shaped parenchymal defects involving both the cortex and medulla, with the apex pointing toward the medulla and base parallel to the subcapsular region[37,38] (Figure 6). A subcapsular enhancing cortical rim may be visualized a few days later, reflecting perfusion of capsular collaterals. In case of total renal infarction, CT demonstrates a non-enhancing kidney with non-opacification of the collecting system in the excretory phase. CT angiography may demonstrate filling defects in the aorta or the renal arterial vasculature suggestive of thrombi; however, these may not always be evident due to the occurrence of microthrombi, which may remain occult on imaging[39,40]. The presence of microthrombi in this setting has been previously documented on histopathologic evaluation of the glomerular capillaries of the infarcted parenchyma[41].
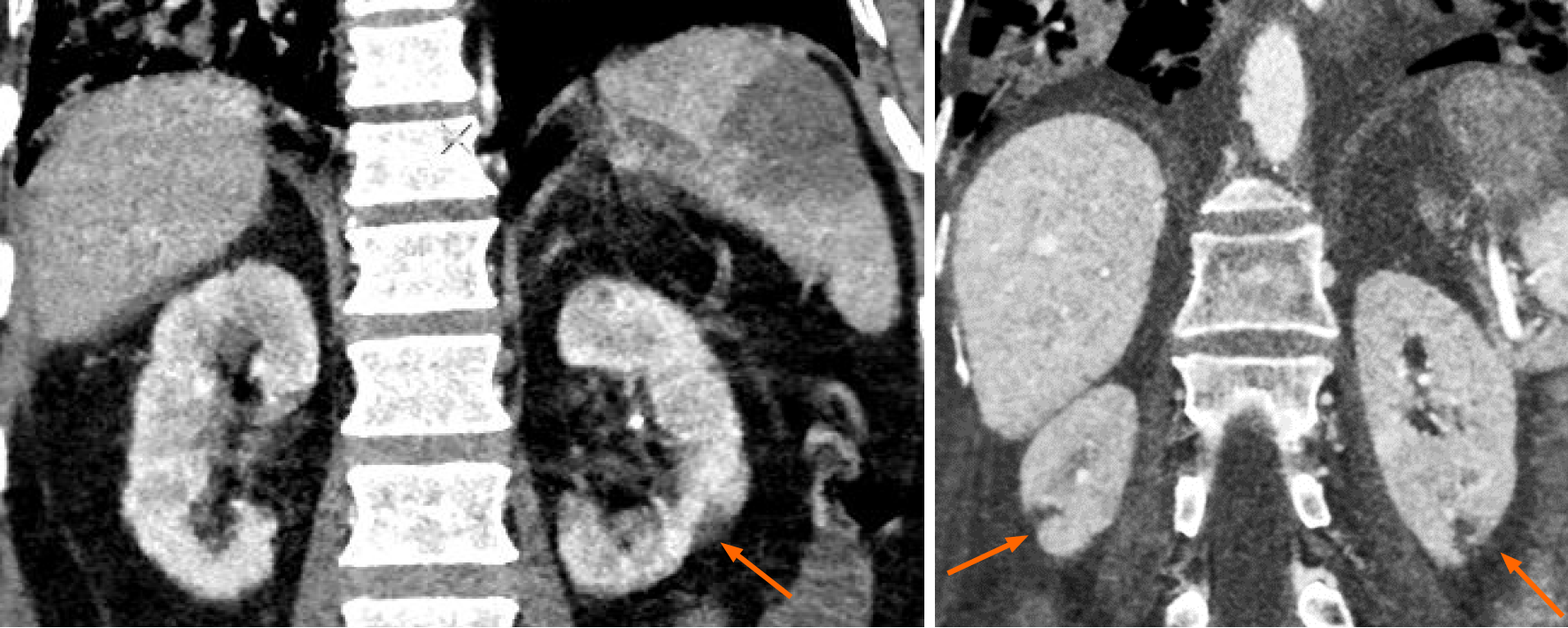
Figure 6 Solid organ infarction in a patient with coronavirus disease 2019.
Coronal contrast enhanced computed tomography (CT) images of the abdomen show discrete, wedge-shaped non-enhancing renal parenchymal defects, with their apex pointing towards the medulla and base parallel to the subcapsular region (orange arrows), suggestive of renal infarcts. These were incidentally detected during CT pulmonary angiography.
Reports of splenic infarction in COVID-19 are scarce in the published literature, since these are usually detected incidentally on chest CECT scans that extend to the upper abdomen[42]. These are usually silent but may occasionally manifest with left upper quadrant pain and abdominal guarding. CT imaging reveals sharply marginated, wedge shaped, hypodense areas with absent post contrast enhancement; these are well depicted in the porto-venous phase. Global splenic infarction appears as hypo/ non enhancement of the entire parenchyma[43] (Figure 7). CT angiography may demonstrate filling defects in the splenic artery or its hilar branches, representing thrombi.
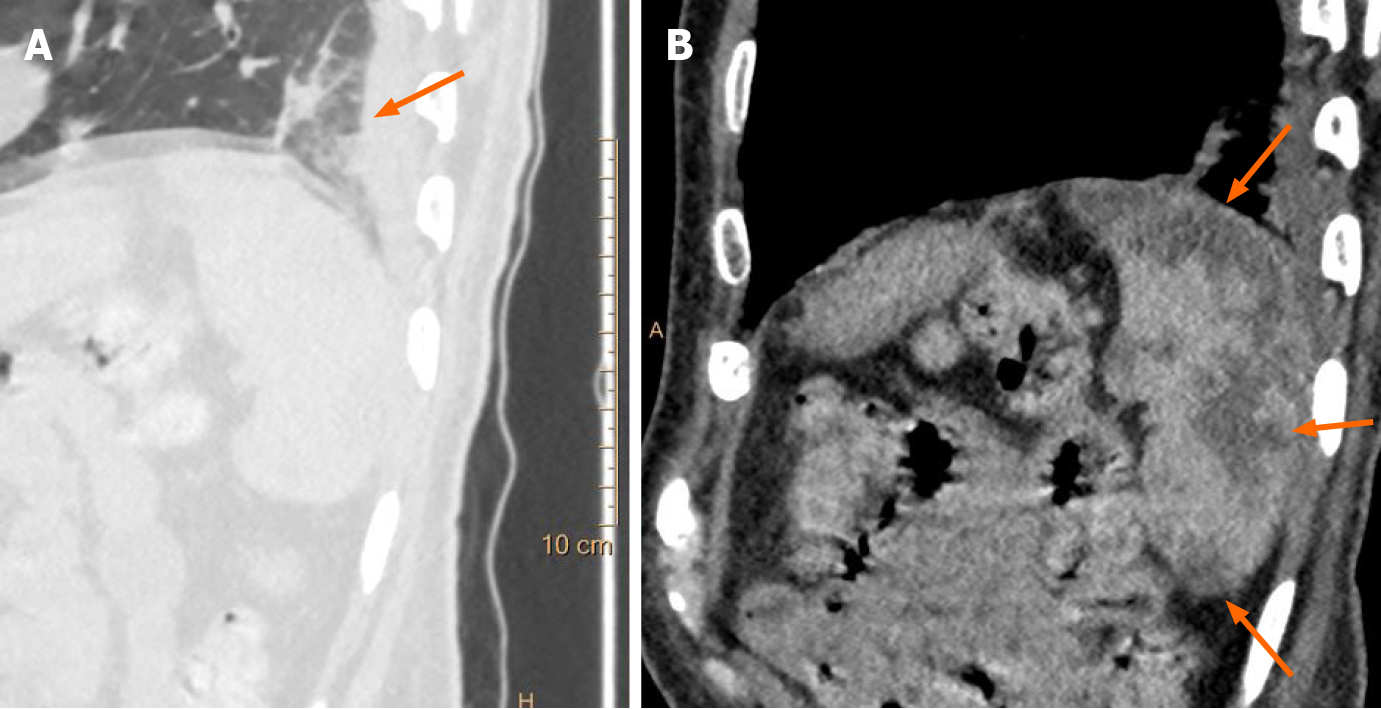
Figure 7 Incidentally detected splenic infarction in a patient with coronavirus disease 2019.
A: Sagittal chest computed tomography (CT) image shows subpleural ground glass opacities in the lung fields in a case of coronavirus disease 2019 (orange arrow); B: Sagittal contrast enhanced CT image of the abdomen in the same patient show incidentally detected, sharply marginated, wedge shaped, hypodense areas in the spleen, suggestive of splenic infarcts (orange arrows).
In our experience, solid organ infarction was always incidentally detected during imaging performed for suspected pulmonary thromboembolism, particularly in association with raised D-dimer levels. Thus, a combination of relevant serum biomarkers and judicious use of imaging, particularly contrast enhanced CT scans, plays a crucial role in the detection of COVID-19-related coagulopathy, thereby facilitating timely management to reduce morbidity and mortality.
HEPATO-BILIARY INVOLVEMENT
The association of hepato-biliary dysfunction with COVID-19 is being increasingly recognized[44]. As many as 40% of COVID-positive patients are found to have abnormal liver function tests (LFTs) on admission, suggesting hepatocyte injury either due to a severe inflammatory response or possibly as a result of ACE-2-mediated viral infection of hepatocytes[45].
Very few studies have investigated the role of abdominal imaging in the evaluation of COVID-19 related hepato-biliary dysfunction. The predominant abnormalities seen in these studies on CT/US imaging were distension of the gallbladder and gallbladder sludge (Figure 8), which are indicative of cholestasis[46-48]. Additional imaging features such as gallbladder wall thickening/mural edema were detected in fewer cases. Since these findings are commonly seen in acute hepatitis, they may serve as a useful clue to indicate hepatocellular dysfunction; however, further research is essential to establish the true significance of these observations.
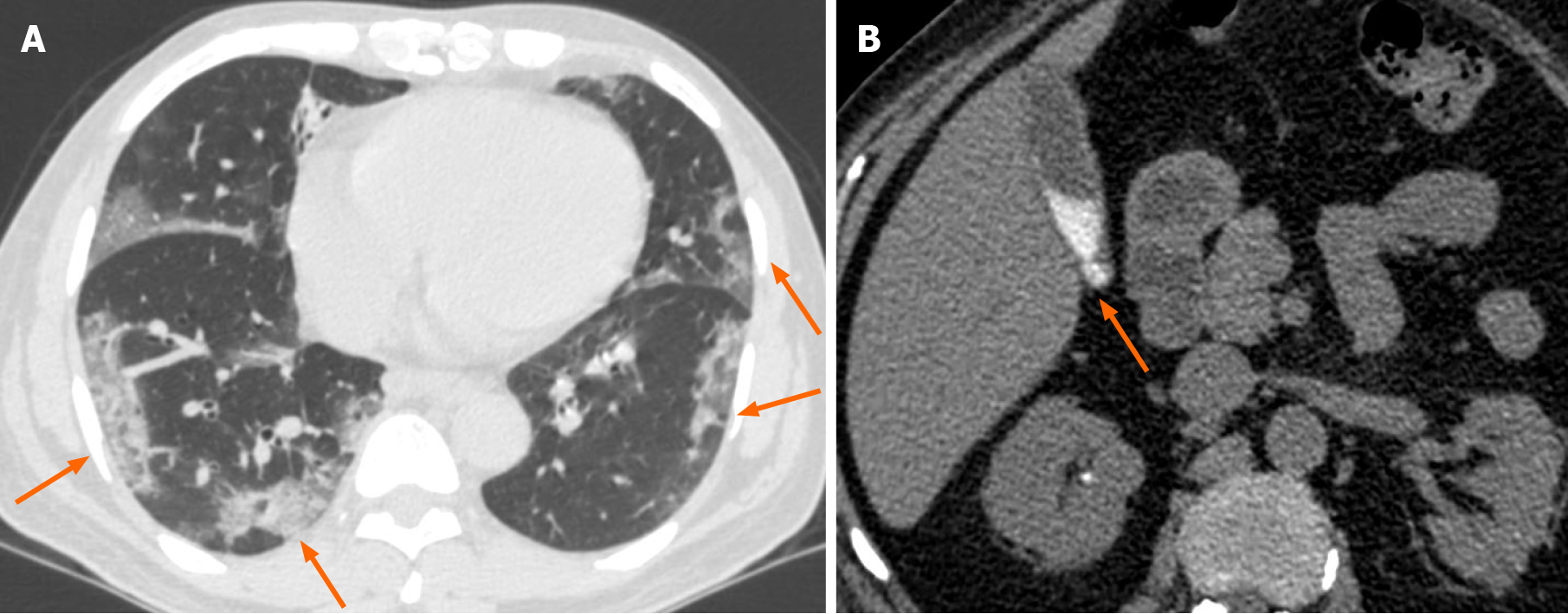
Figure 8 Evidence of cholestasis in a critically ill coronavirus disease 2019 patient.
A: Axial chest computed tomography (CT) image shows multiple peripheral ground glass opacities associated with interstitial thickening in both lung fields (orange arrows in A); B: Axial non-contrast CT image of the abdomen shows incidentally detected hyperdense sludge within the gall bladder lumen (orange arrow in B), suggesting cholestasis.
Hepatomegaly with increased parenchymal echogenicity is reported to be the most commonly encountered liver abnormality on abdominal US, possibly indicative of a diffuse parenchymal disease[46-48]. These findings may also be seen in COVID-19 patients with obesity and non-alcoholic fatty liver disease, which serve as potential risk factors for the increase in COVID-19 disease severity[49].
We did not encounter cases of isolated hepato-biliary involvement in COVID-19. However, we did observe increased severity of infection in patients with pre-existing chronic liver parenchymal disease, detected on imaging. The majority of patients presenting with deranged LFTs had no significant abnormality on screening abdominal US, while a small proportion of patients were found to have diffusely increased hepatic echogenicity. This subgroup of patients had associated co-morbidities such as obesity and type 2 diabetes mellitus, thus the US findings were highly suggestive of hepatic steatosis in the given setting. The definite imaging features on US indicating hepatic involvement in COVID-19 have not been ascertained so far.
PANCREATIC INVOLVEMENT
Viral pancreatitis is a well-known clinical entity. Although an accurate understanding of the spectrum of pancreatic injury is not established at present, recent reports have emerged highlighting acute pancreatitis (AP) as a possible manifestation of COVID-19[50-52]. COVID-19 induced pancreatic injury is believed to be a consequence of SARS-CoV-2 cytotoxicity mediated by viral binding to ACE-2 receptors expressed on pancreatic islet cells or possibly due to the severe immune response triggered by viral infection[53].
The initial diagnosis for AP is usually based on clinical parameters that include signs and symptoms of acute abdomen associated with an elevation of serum pancreatic enzymes, such as amylase and lipase; however, imaging plays a valuable role in aiding the diagnosis whenever the clinical presentation is unclear. Moreover, imaging is essential for diagnosing the etiology, staging disease severity, and evaluating complications[54,55]. Various researchers have elucidated the imaging features of COVID-induced AP based on isolated cases encountered by them in practice. Radiologically, it appears to be a mild form of disease, also termed as interstitial/edematous pancreatitis, with CT imaging features ranging from a normal-appearing pancreas and peripancreatic soft tissues to diffuse enlargement coupled with heterogeneous enhancement of the parenchyma with ill-defined or fuzzy borders. Peripancreatic inflammation appears as hazy stranding of the surrounding fat and streak of fluid along the anterior conal fascia and in the retro-mesenteric plane (Figure 9). To the best of our knowledge, no case of necrotizing pancreatitis in the setting of COVID-19 has been reported so far. Considering the possible occurrence of mild pancreatic injury in patients with COVID-19 pneumonia, it may be prudent to evaluate pancreatic enzymes in patients presenting with GI symptoms[56]. CT imaging could be used in conjunction with the clinical parameters in order to establish a correct diagnosis or provide an alternative diagnosis when in doubt. In the absence of other etiologies like gallstones, trauma, alcohol, or drug intake, viral infection can be considered as the causative factor for pancreatitis in patients with COVID-19.
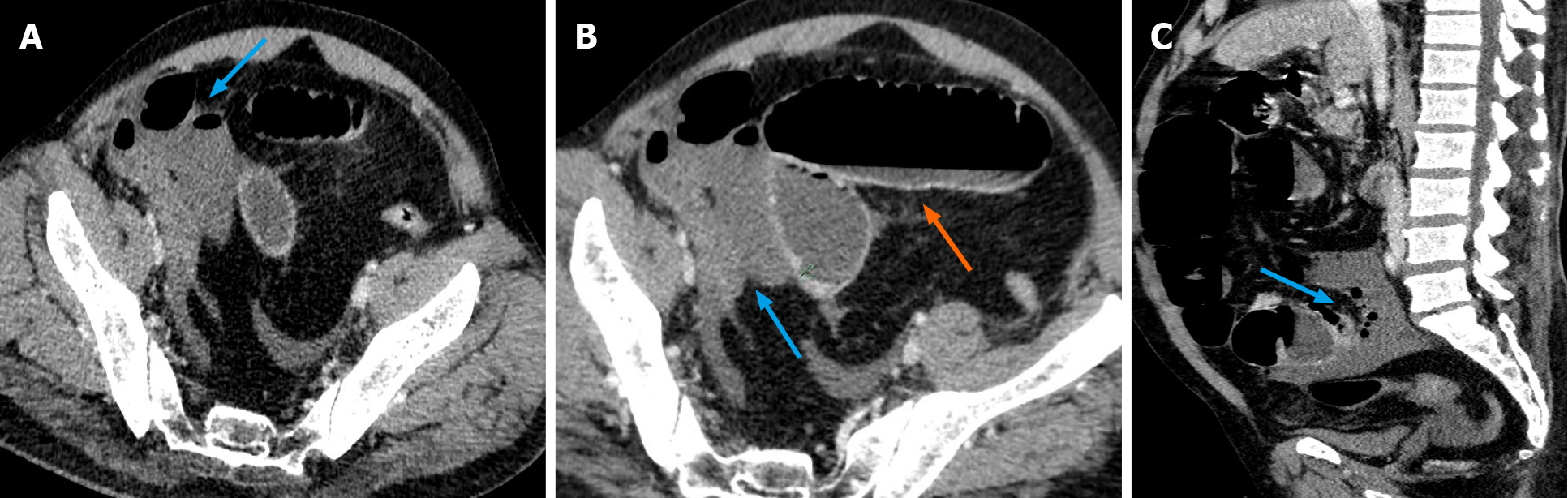
Figure 9 Acute viral pancreatitis in a coronavirus disease 2019 patient presenting with abdominal pain.
Non-contrast axial computed tomography image of the abdomen in a case of suspected viral pancreatitis (intravenous contrast could not be administered due to a history of renal parenchymal disease with elevated creatinine) is shown. The distal body and tail of pancreas reveal fuzzy margins with peri-pancreatic fat stranding (blue arrow). Thickening of the left anterior conal fascia is noted with a streak of fluid in the left retro-mesenteric plane (orange arrow). Elevated serum amylase and lipase levels, in conjunction with these imaging findings, were highly suggestive of a diagnosis of acute viral pancreatitis in a patient with coronavirus disease 2019 presenting with abdominal pain.
BLEEDING MANIFESTATIONS
Clinicians involved in the treatment of COVID-19 are familiar with the high tendency to develop a hypercoagulable state in patients with a severe form of the illness. The acute thrombotic complications in critically ill patients affecting different organ systems are being increasingly recognized by imaging[18]. However, there is a paucity of literature with respect to the occurrence of bleeding events in COVID-19, either as a result of coagulopathy or secondary to anti-coagulation therapies[57]. The increased risk of bleeding in COVID-19 patients is believed to result from an imbalance between production and destruction of platelets secondary to infection[58]. More importantly, the possibility of bleeding complications is increased by the use of therapeutic/prophylactic anticoagulation to combat the COVID-19 associated hypercoagulable state, as evidenced by elevated D-dimer levels[59]. A sudden drop in the hemoglobin level coupled with features of hypovolemia such as hypotension and tachycardia serves as clinical indicators for the development of major bleeding and warrants CT imaging to identify the site of bleed[60]. The majority of researchers, including us, have encountered abdominal hematomas as the most bleeding manifestation in critically ill COVID-19 patients, of these the ilio-psoas compartment appears to be the most frequent site of bleeding[61-64]. Non-contrast CT scans in these cases reveal diffuse enlargement of the ilio-psoas compartment with a hyperdense intra-muscular collection (Figure 10); sometimes a blood-fluid level may be noted within it, indicative of active bleeding. CT angiography may provide confirmatory evidence of active bleeding, presenting as a blush or extravasation of intravenously administered contrast seen in the arterial phase; this finding would necessitate immediate treatment[65]. Digital subtraction angiography may then be performed to identify the bleeding vessels followed by selective transarterial embolization. In the absence of radiologic evidence of active bleeding or hemodynamic instability, conservative treatment may be instituted[66]. In our experience, minimally invasive intervention in the form of pigtail catheter insertion is useful for drainage of large hematomas; this offers symptomatic relief by decompression of adjacent structures.
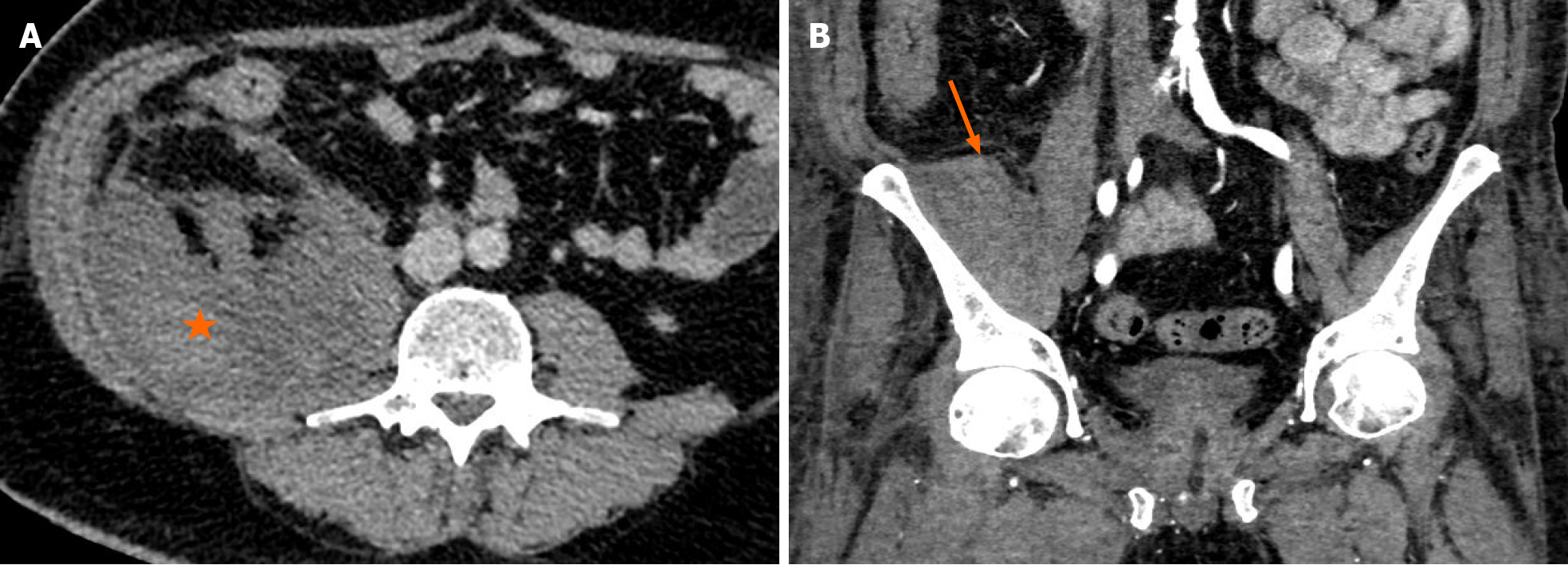
Figure 10 Bleeding manifestations encountered in treated cases of coronavirus disease 2019.
A: Contrast enhanced axial computed tomography (CT) image of the abdomen shows a hyperdense collection in the right ilio-psoas compartment (orange asterisk in A), suggestive of a hematoma; B: Contrast enhanced coronal CT image of the abdomen shows a hyperdense collection in the right iliacus muscle (orange arrow in B) in another patient. Both patients were being treated with anticoagulants for coronavirus disease 2019 associated hypercoagulable state evidenced by elevated D-dimer levels. CT imaging was performed to evaluate the cause of a sudden fall in hemoglobin.
Abdominal manifestations of COVID-19: Roadmap for future research
A limitation that we encountered while working on this review was that our work was based primarily on observations and experiences in a single tertiary care institute. Moreover, obtaining the relevant literature pertaining to imaging of abdominal complications of COVID-19 was an uphill task owing to the paucity of studies with large sample sizes with particular focus on imaging. Thus, with regards to future research, we believe that a multi-centre collaboration can result in higher rates of patient enrolment than single-centre studies, thereby generating a larger data pool and bigger sample sizes, in a shorter duration, in order to investigate the research question of interest. In this manner, it is possible to obtain statistically significant results which can be representative of the whole population, thereby leading to more accurate insights into the pathophysiology and imaging findings of GI tract involvement in COVID-19, and enable researchers to draw evidence-based conclusions.
Another advantage of multi-centre studies is that owing to the heterogeneity of available data, it may be possible to understand the chronology or temporal evolution of the abdominal imaging manifestations of COVID-19, as findings may vary depending on the timing of imaging during the course of infection. These results could aid our understanding of the timelines for the various abdominal complications in COVID-19, based on which standardized protocols can be developed to guide clinicians regarding the clinical red flags and worrisome biochemical parameters that require close attention in a COVID-19 patient presenting with GI symptoms, the indications and timing of abdominal imaging in COVID-19, the choice of imaging modality, particular imaging findings that need evaluation, and appropriate interventions for each complication. The formulation of standardized protocols for diagnosis and treatment could play a major role in the timely identification and management of devastating GI complications associated with COVID-19.
Artificial intelligence: Future directions and potential role in the COVID-19 era
Artificial intelligence (AI) based on radiologic evaluation appears to have a promising role in the diagnosis, severity assessment, and prognosis of COVID-19 pneumonia. Several researchers have demonstrated the utility of AI algorithms, particularly deep learning techniques, in the diagnosis of COVID-19 pneumonia based on chest CT images, differentiation of COVID-19 pneumonia from other non-COVID pneumonias, and quantification of the extent of lung parenchymal involvement using segmentation masks[67-69].
With increasing awareness and recognition of the extra-pulmonary manifestations of COVID-19, particularly the thrombotic complications, the corresponding imaging findings could also serve as appropriate targets for AI systems[67]. A subtype of the deep learning technology, namely, convolutional neural networks, has generated great interest amongst the radiology community owing to their varied applications[70] and could have a potential role in the detection of extra-pulmonary thrombotic complications of COVID-19 such as multi-organ infarction and arterial and venous thrombi on CT imaging. This technique of machine learning, however, would require the availability of large amounts of input data for adequate ‘training’. Typical data sets required for training could range from hundreds to thousands of patient’s scans. The data also needs accurate labels/annotations, which could be binary, meaning whether a study is positive or negative for COVID-19, or using segmentation labels to identify the extent of the abnormality. Training data sets may also be augmented further with the addition of clinical data, vital parameters, and blood test values. Moreover, it is advisable to include external test data sets of patients from a different demographic from the one used for training, so as to ascertain if the AI algorithm can be applied to various patient populations. Thus, multi-institutional collaboration and global data sharing are a must to generate data sets satisfactory for machine learning[70,71]. The availability of high-quality data sets of thrombotic complications in COVID-19 patients, detected on CT angiography images, could be used to develop innovative machine learning models for detection and quantification of extra-pulmonary disease severity. Thus, AI could certainly serve as a valuable tool to triage COVID-19 patients presenting to the emergency department, reduce radiologist workload, improve diagnostic accuracy, and facilitate prognostication and management decisions[72].
CONCLUSION
To conclude, GI manifestations of COVID-19 can present at the time of diagnosis or can occur anytime during the course of disease; this may necessitate imaging especially in critically ill patients. Hypercoagulability is one of the hallmarks of COVID-19, with multi-systemic implications. Our experience suggests that a high index of suspicion for abdominal visceral infarction and bowel ischemia should be maintained in COVID-19 patients presenting with severe GI symptoms. Timely imaging with CT angiography in these patients with clinical and biochemical markers of ischemia could play a major role in decreasing mortality. In patients with abdominal pain, CT imaging can also aid the diagnosis of viral-mediated inflammation of abdominal viscera, such as colitis and pancreatitis, thereby guiding appropriate management. With regards to treatment-related complications, prompt radiological investigations, such as non-contrast CT scans, are crucial for the diagnosis of occult bleeding associated with anticoagulant therapy in COVID-19 patients presenting with hypovolemia. Thus, in this COVID-19 era, radiologists could play a pivotal role in the detection of various GI tract abnormalities associated with the infection and in the timely recognition of thrombotic and treatment-related complications. An awareness of the COVID-19 associated abdominal imaging manifestations can enable radiologists to guide treating physicians for optimal disease management.
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/Licenses/by-nc/4.0/
Manuscript source: Invited manuscript
Specialty type: Radiology, nuclear medicine and medical imaging
Country/Territory of origin: India
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Jiang Y, Zhang L S-Editor: Liu M L-Editor: Wang TQ P-Editor: Yuan YY