©2014 Baishideng Publishing Group Inc.
World J Radiol. Oct 28, 2014; 6(10): 779-793
Published online Oct 28, 2014. doi: 10.4329/wjr.v6.i10.779
Published online Oct 28, 2014. doi: 10.4329/wjr.v6.i10.779
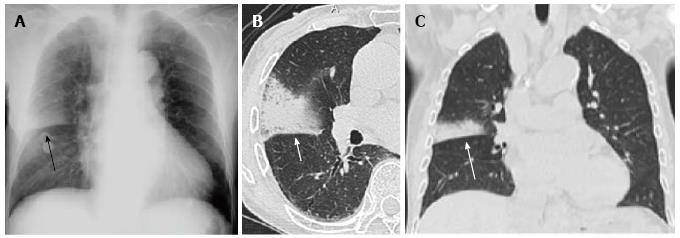
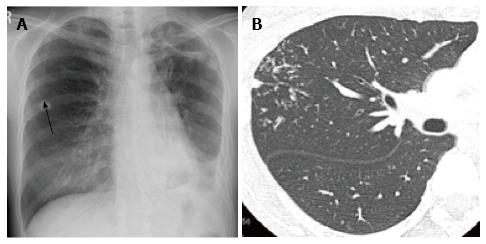
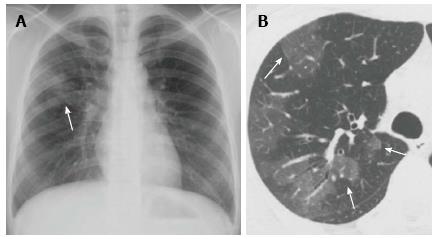
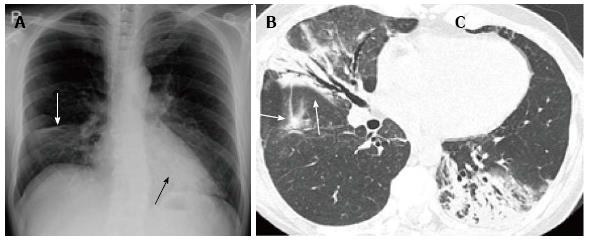
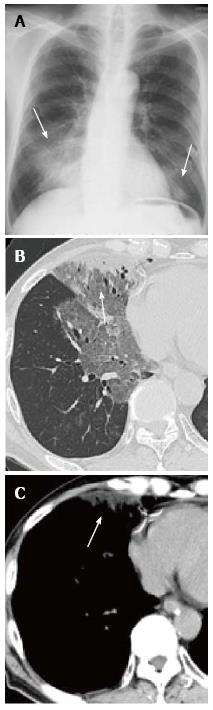
Figure 1 Streptococcus pneumoniae pneumonia showing alveolar pneumonia in a man in his 80s.
A: Chest radiograph shows a nonsegmental consolidation in the right middle lung field, which is demarcated by the minor fissure suggestive of upper lobe pneumonia (arrow); B, C: Thin-section computed tomography (B) and a coronal reformatted image (C) demonstrate a nonsegmental consolidation with air bronchograms suggestive of alveolar pneumonia (arrows).
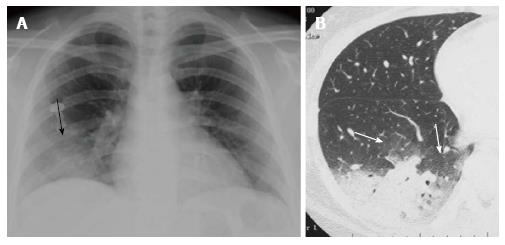
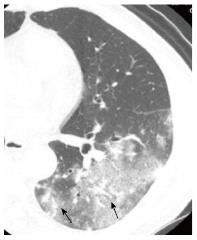
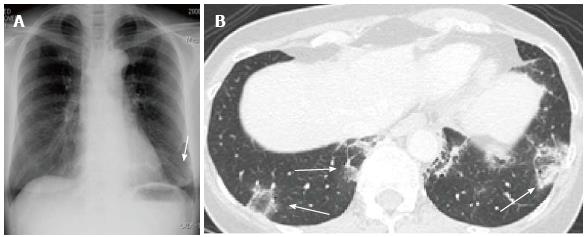
Figure 2 Mycoplasma pneumoniae pneumonia showing alveolar pneumonia in a woman in her 30s.
A: Chest radiograph demonstrates ill-defined consolidation in the right lower lung field (arrow); B: Thin-section CT reveals a non-segmental consolidation with air bronchograms at the dorsal aspect of the right lower lobe. Areas of ground-glass opacity are also noted around the consolidation (arrows). CT: Computed tomography.
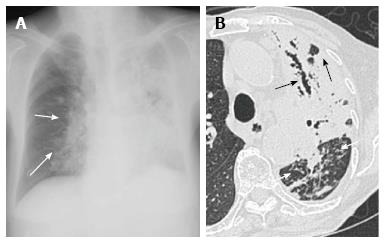
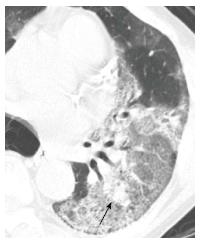
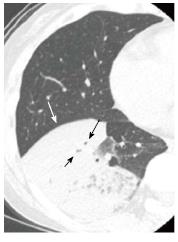
Figure 3 Chlamydophila pneumoniae pneumonia showing alveolar pneumonia in a man in his 60s.
A: Chest radiograph shows an ill-defined consolidation at the right lower lung field (arrow); B: On thin-section CT, a subpleural focal consolidation is seen at the right S8 of the right lower lobe, partially extending into the middle lobe (black arrow). The interlobular fissure is mildly thickened (arrow heads). Mild bronchial wall thickening is also noted (white arrow). CT: Computed tomography.
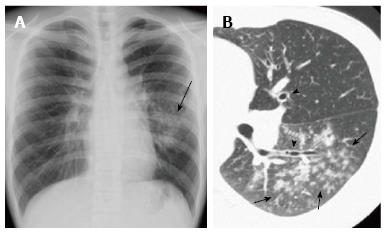
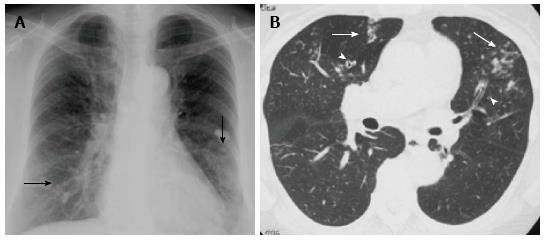
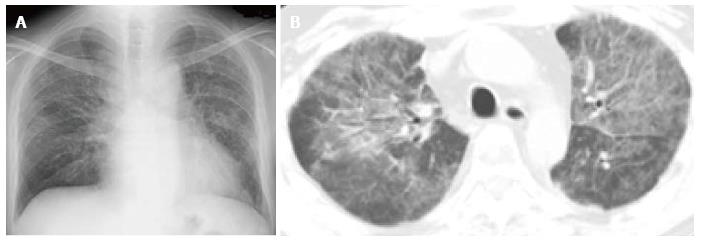
Figure 4 Tuberculous pneumonia in a woman in her 80s.
A: Chest radiograph shows extensive consolidations with poor aeration of the left lung and peribronchovascular consolidations of the right lung (arrows); B: Thin-section computed tomography reveals extensive consolidation with air bronchograms and cavities in the left upper lobe (black arrows). Note that the bronchi in the consolidation are dilated. Dense centrilobular nodules are seen in the left lower lobe (white arrows).
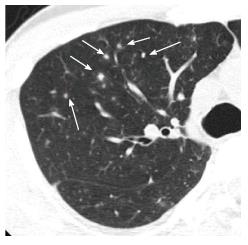
Figure 5 Mycoplasma pneumoniae pneumonia showing bronchopneumonia in a man in his 10s.
A: Chest radiograph shows reticulonodular opacities and focal consolidation in the left middle to lower lung field (arrow). The left pulmonary hilum appears enlarged; B: Thin-section computed tomography demonstrates fluffy centrilobular nodules with surrounding ground-glass opacity in the left lower lobe (arrows). Note that central bronchial wall is thickened (arrow heads).
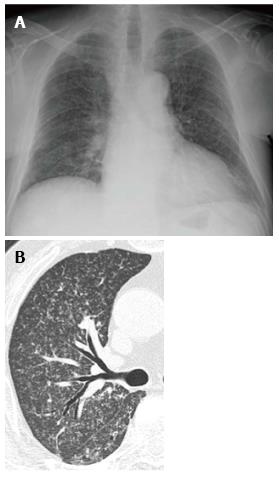
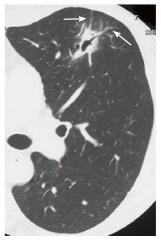
Figure 6 Postprimary tuberculosis in a woman in her 40s.
A: Chest radiograph shows faint nodular opacities in the right middle lung field (arrow). There is also volume loss of the left lung with patchy consolidations and thickening of the pleura and possible left pleural effusion, indicative of old tuberculosis; B: Thin-section computed tomography demonstrates centrilobular branching opacities (tree-in-bud appearance) in the right upper lobe (arrows). The branching opacities are denser, more distributed and more peripherally located than those of ordinary bronchopneumonia (compare with Figure 3).
Figure 7 Chlamydophila pneumoniae pneumonia showing infectious bronchiolitis in a woman in her 60s.
A: Chest radiograph shows faint reticulonodular opacities in both lower lung fields (arrows); B: Thin-section computed tomography reveals centrilobular nodules (arrows) with bronchiectasis (arrow heads) in the middle lobe and lingula.
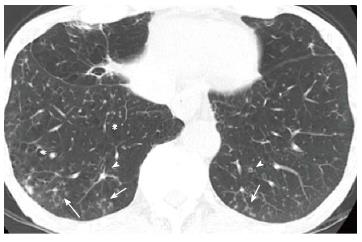
Figure 8 Chronic transbronchial infection (diffuse aspiration bronchiolitis) in a man in his 70s.
This patient had a history of esophageal carcinoma and associated repeated aspiration. Thin-section computed tomography at the level of lung base shows centrilobular nodules (arrows) with bronchiectasis (arrow heads). Low attenuation areas suggestive of pulmonary emphysema are also present (*).
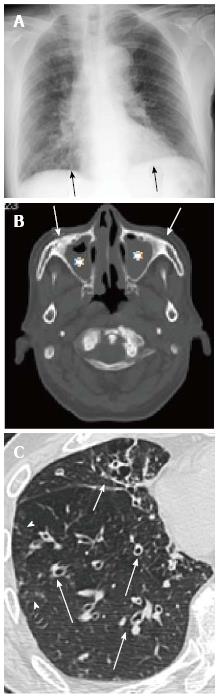
Figure 9 Sinobronchial syndrome in a man in his 70s.
A: Chest radiograph shows bilateral reticulonodular opacities in both lower lung fields (arrows); B: computed tomography (CT) at the level of maxillary sinus demonstrates opacification of the maxillary sinuses (*) and bone sclerosis of the sinus walls (arrows), suggestive of chronic paranasal sinusitis; C: Thin-section CT reveals bronchial wall thickening with bronchiectasis (arrows) and minimal centrilobular opacities (arrow heads).
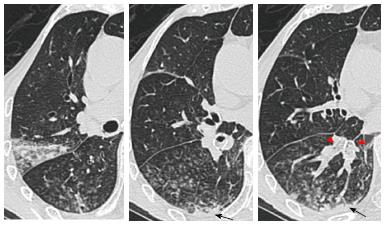
Figure 10 Mycoplasma pneumoniae pneumonia showing ground-glass opacity predominant pneumonia in a woman in her 30s.
A: Chest radiograph shows patchy ground-glass opacity (GGO) with peribronchial nodules in the right middle lung field (arrow); B: Thin-section computed tomography reveals areas of GGO in the right upper lobe. Note that the GGO are partly demarcated by interlobular septa (arrows).
Figure 11 Chlamydophila pneumoniae pneumonia showing ground-glass opacity predominant pneumonia in a man in her 60s.
Thin-section computed tomography shows patchy ground-glass opacity in the left lower lobe, in which thickened bronchovascular bundles are present (arrows).
Figure 12 Legionella pneumophila pneumonia in a man in his 50s.
Thin-section computed tomography shows extensive ground-glass opacity (GGO) in the left lower lobe intermingled with focal consolidations that are sharply demarcated from the surrounding GGO (arrow).
Figure 13 H1N1 influenza pneumonia in a man in his 40s.
Thin-section computed tomography shows patchy ground-glass opacity that are sharply demarcated from the surrounding lung parenchyma by interlobular septa (geographic distribution) in both lungs. Faint centrilobular nodules are also seen (arrow).
Figure 14 Pneumocystis jirovecii pneumonia in a man in his 20s.
A: Chest radiograph shows bilateral reticulonodular opacities; B: Chest computed tomography with a 5 mm slice thickness demonstrates bilateral ground-glass opacity with reticulations.
Figure 15 Random nodules predominant pneumonia (varicella-zoster pneumonia) in a man in his 30s.
Thin-section computed tomography demonstrates scattered small solid or ground-glass opacity nodules which are unrelated to centrilobular structures (arrows).
Figure 16 Miliary tuberculosis in a man in his 60s.
A: Chest radiograph diffuse reticulonodular opacities in both lungs; B: Thin-section computed tomography demonstrates diffuse military nodules with a random distribution.
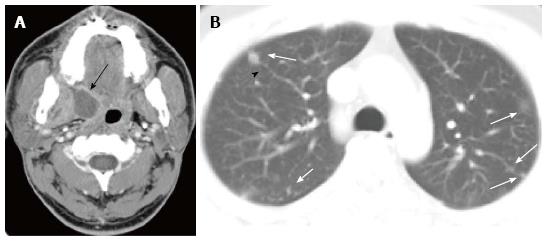
Figure 17 Pulmonary septic emboli from paratonsillar abscess in a man in his 20s.
A: Enhanced computed tomography (CT) at the level of oropharynx shows an abscess at the right paratonsillar region (arrow); B: Chest CT with a 5 mm slice thickness reveals small nodules in both lungs (arrows), some of which are in contact with the periphery of pulmonary vessels (arrow head).
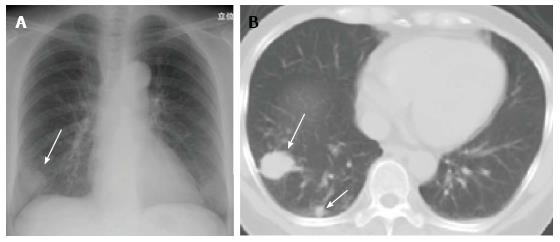
Figure 18 Cryptococcus neoformans pneumonia in a woman in her 50s.
A: Chest radiograph shows a mass in the right lung base (arrow); B: Chest computed tomography with a 5 mm slice thickness shows a mass and nodule in the right lower lobe (arrows). Multiple nodules/masses in the same pulmonary lobe are considered characteristic findings of Cryptococcus pneumonia.
Figure 19 Aspiration pneumonia in a woman in her 70s (causative pathogen unknown).
Thin-section computed tomography images show centrilobular nodules with surrounding ground-glass opacities and subpleural non-segmental consolidations (arrows) at the dorsal portions of the right lung. Note that the lumens of segmental bronchi are filled with aspirated materials (arrow heads).
Figure 20 Pneumonia caused by aspiration of gastric fluid in a man in his 50s.
A: Initial thin-section computed tomography (CT) shows patchy ground-glass opacity in the left lung with reticulations; B: Thin-section CT 2 d later demonstrates partly increased attenuation with concaved margin of the opacities as well as a general resolution of pneumonia.
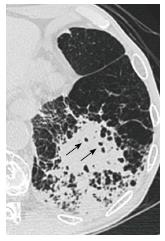
Figure 21 Pneumonia on a background of pulmonary emphysema in a man in his 70s (causative pathogen unknown).
Thin-section computed tomography shows patchy consolidations with small air-containing spaces consistent with preexistent low attenuation areas in the left lower lobe.
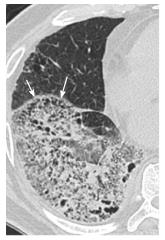
Figure 22 Pneumonia on a background of pulmonary emphysema mimicking honeycombing in a man in his 60s (causative pathogen unknown).
Thin-section computed tomography shows an extensive area of ground-glass opacity intermingled with consolidation in the right lower lobe. Pseudohoneycombing is seen along the interlobar fissure (arrows).
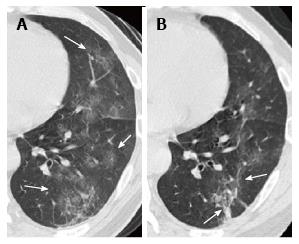
Figure 23 Cryptogenic organizing pneumonia in a woman in her 50s.
A: Chest radiograph shows a consolidation in the right lower lung field with depression of the right minor fissure suggestive of volume loss of the middle lobe (white arrow). Retrocardiac consolidation is marginally seen (black arrow); B, C: Thin-section computed tomography of the right lung (B) and left lung (C) demonstrate consolidations with air bronchograms in both lungs. Note that the bronchi within the consolidations are mildly dilated and that the consolidations have concaved margins (arrows), suggesting organization of the disease.
Figure 24 Cryptogenic organizing pneumonia with reversed halo sign in a woman in her 50s: courtesy of Dr.
Takahiro Haruyama and Dr. Asako Yamamoto, attending radiologists at the department of Radiology, Teikyo University School of Medicine. A: Chest radiograph shows an ill-defined consolidation in the left lower lung field (arrow); B: Thin-section computed tomography reveals bibasilar ground-glass opacity with a ring of consolidation (reversed halo sign (arrows).
Figure 25 Chronic eosinophilic pneumonia in a woman in her 30s.
Chest radiograph shows bilateral subpleural consolidations with upper to middle lung field predominance, consistent with the appearance, “the photographic negative of pulmonary edema”.
Figure 26 Invasive mucinous adenocarcinoma (formerly mucinous bronchioloalveolar carcinoma) in a woman in her 60s.
Thin-section computed tomography shows a nonsegmental consolidation with a bulging fissure (white arrow) and narrowed air bronchograms (black arrows).
Figure 27 Pulmonary malignant lymphoma (mucosa associated lymphoid tissue lymphoma) in a woman in her 30s.
Thin-section computed tomography shows a focal consolidation with dilated air bronchograms in the lingula of the left upper lobe. Note mild thickening of the vessels penetrating the consolidation (arrows), suggestive of infiltrative growth of malignant lymphoma along the vessels.
Figure 28 Exogenous lipoid pneumonia in a woman in her 30s: Courtesy of Dr.
Kazuhiro Suzuki, an attending radiologist, at the department of Radiology, Juntendo University School of Medicine. This patient had been taking petrolatum (paraffin) for intractable constipation. The presence of lipid was confirmed by transbronchial lung biopsy. A: Chest radiograph shows bilateral consolidations in the lower lung fields (arrows); B: Thin-section CT demonstrates an area of clearly demarcated ground-glass opacity with a subpleural consolidation (arrow); C: Chest computed tomography (CT) with a mediastinal window setting reveals the subpleural consolidation to be of fat attenuation (arrow, mean CT value -45HU).
- Citation: Nambu A, Ozawa K, Kobayashi N, Tago M. Imaging of community-acquired pneumonia: Roles of imaging examinations, imaging diagnosis of specific pathogens and discrimination from noninfectious diseases. World J Radiol 2014; 6(10): 779-793
- URL: https://www.wjgnet.com/1949-8470/full/v6/i10/779.htm
- DOI: https://dx.doi.org/10.4329/wjr.v6.i10.779