©2014 Baishideng Publishing Group Inc.
World J Radiol. Oct 28, 2014; 6(10): 741-755
Published online Oct 28, 2014. doi: 10.4329/wjr.v6.i10.741
Published online Oct 28, 2014. doi: 10.4329/wjr.v6.i10.741
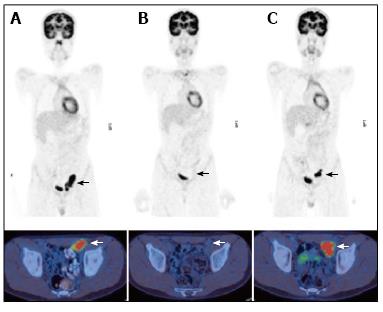
Figure 1 A 13 year-old male with nodular sclerosing Hodgkin’s disease.
PET/CT at staging (A) demonstrated disease in the left external iliac region. After completion of chemotherapy 4 mo later (B) there was a complete metabolic response with no activity in the residual lymph node mass. PET/CT performed 6 mo later (C) for surveillance demonstrated a recurrence at the same site. PET/CT: Positron emission tomography/computed tomography.
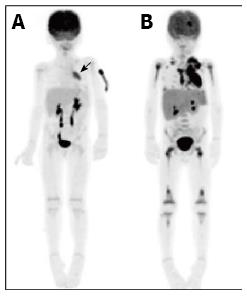
Figure 2 A 5-year-old male patient with relapsed T-cell lymphoblastic lymphoma.
Restaging PET at the time of relapse 1 year after initial therapy demonstrated an FDG-avid mediastinal mass (A, arrow). Repeat PET performed following 1 cycle of FLAG-Ida chemotherapy demonstrated no response to treatment and progression of disease to stage IV with extensive bone marrow involvement (B). PET: Positron emission tomography; FDG: 2-deoxy-2-(18F)fluoro-D-glucose.
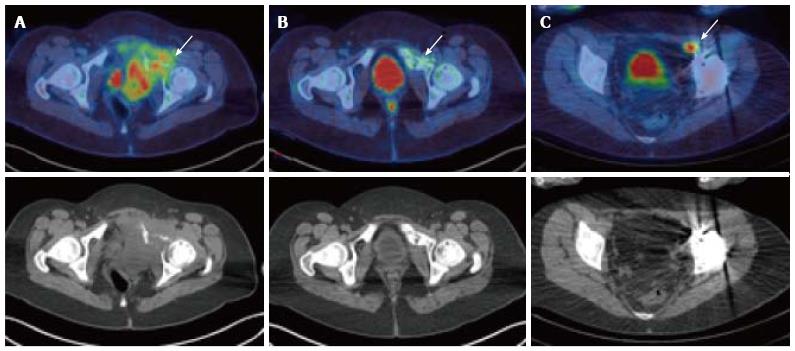
Figure 3 A 17-year-old female with Ewing’s sarcoma involving the left superior pubic ramus.
Staging PET/CT showed extensive disease (A, arrow) with bone destruction and a large FDG-avid pelvic mass. Following chemotherapy, at 5 mo after diagnosis, there was an excellent metabolic response with minimal residual FDG uptake (B, arrow). Patient underwent surgical resection and extracorporeal radiotherapy to the bone. Sixteen months after completion of treatment, surveillance PET/CT demonstrated recurrence in a left external iliac lymph node (C) which was not detectable on the CT or MRI due to marked metal artefact. PET/CT: Positron emission tomography/computed tomography; FDG: 2-deoxy-2-(18F)fluoro-D-glucose; MRI: Magnetic resonance imaging.
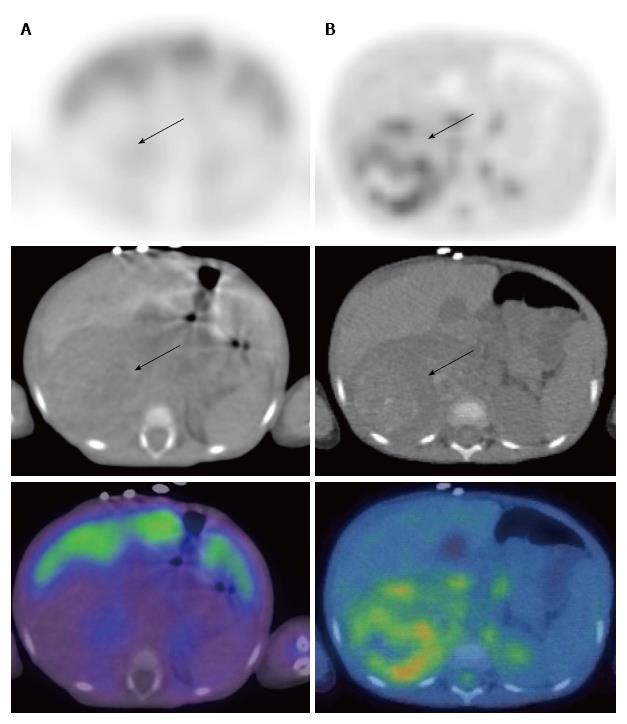
Figure 4 Neuroblastoma in a 2-year-old female.
123I-metaiodobenzylguanidine (MIBG) single positron emission tomography/computed tomography (SPECT/CT) images (A) demonstrated a large right suprarenal mass displacing the organs which was not MIBG-avid (arrows). FDG PET/CT (B) showed moderate heterogenous metabolic activity within the mass. PET/CT: Positron emission tomography/computed tomography; FDG: 2-deoxy-2-(18F)fluoro-D-glucose.
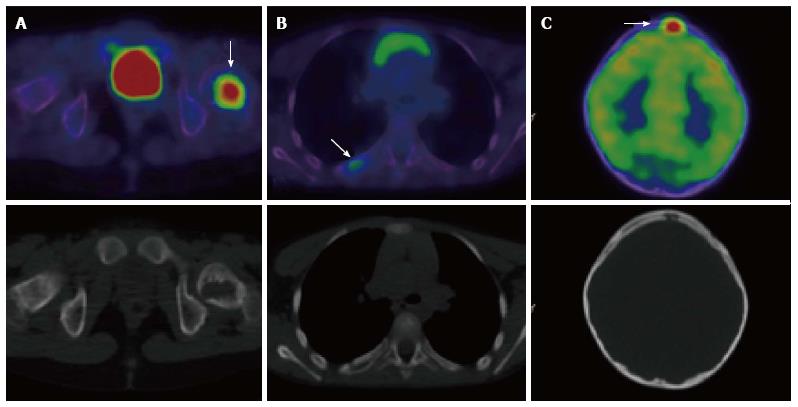
Figure 5 A 7-year-old male with Langerhans cell histiocytosis.
Skeletal survey demonstrated an isolated left femoral lesion, confirmed on PET/CT (A, arrow). Additional lesions (arrows) in the right 6th rib posteriorly (B) and in the skull (C) were also identified on the PET/CT scan. Top panel: fused PET/CT images, bottom panel: low dose CT component of the scan. PET/CT: Positron emission tomography/computed tomography.
Figure 6 An extreme case of widespread brown fat activity in a 16-year-old female with treated Hodgkin’s disease.
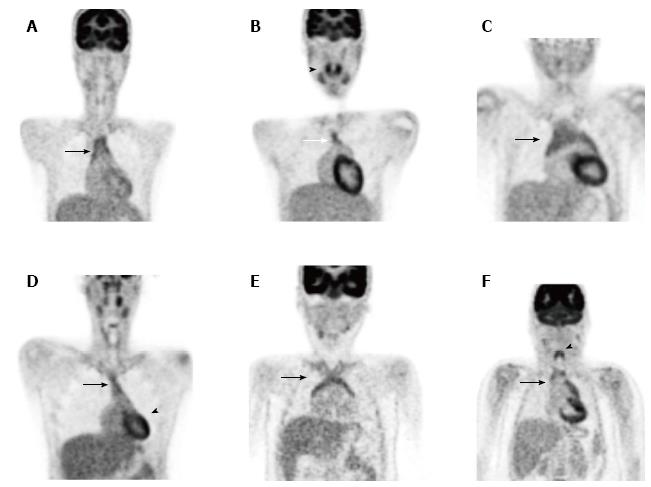
Figure 7 Normal physiological variants: various patterns of thymic uptake (A-F, arrow), tonsillar uptake (B, arrowhead), cardiac uptake (D, arrowhead) and laryngeal uptake (F, arrowhead).
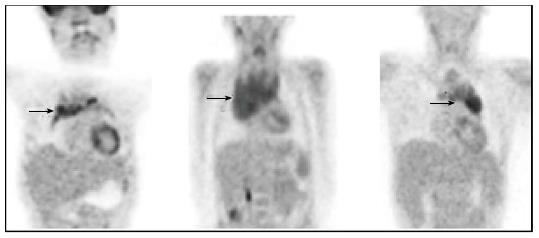
Figure 8 Examples of abnormal thymic uptake due to malignant disease (arrows).
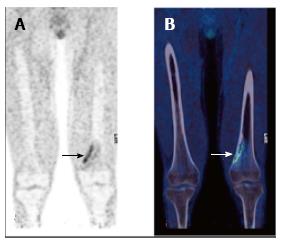
Figure 9 Normal 2-deoxy-2-(18F)fluoro-D-glucose positron emission tomography scan of an 8-year-old female showing physiological growth plate uptake (arrow).
Figure 10 Non–ossifying fibroma (arrow) in the left distal femur of a 17-year-old male patient with Langerhans cell histiocytosis.
FDG PET (A) showing avid uptake, CT (B) showing typical benign radiological features. PET: Positron emission tomography; CT: Computed tomography; FDG: 2-deoxy-2-(18F)fluoro-D-glucose.
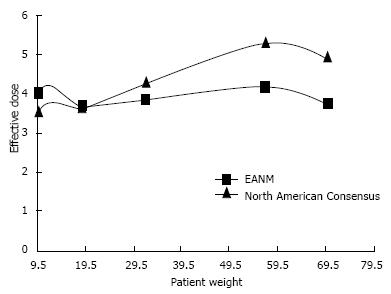
Figure 11 Effective dose vs patient weight for 2-deoxy-2-(18F)fluoro-D-glucose (European Association of Nuclear Medicine and North American Consensus Guidelines).
Image courtesy of Bruce McBride, Chief Physicist, Department of Nuclear Medicine and PET, The Prince of Wales and Sydney Children’s Hospitals. PET: Positron emission tomography; EANM: European Association of Nuclear Medicine.
- Citation: Freebody J, Wegner EA, Rossleigh MA. 2-deoxy-2-(18F)fluoro-D-glucose positron emission tomography/computed tomography imaging in paediatric oncology. World J Radiol 2014; 6(10): 741-755
- URL: https://www.wjgnet.com/1949-8470/full/v6/i10/741.htm
- DOI: https://dx.doi.org/10.4329/wjr.v6.i10.741