©The Author(s) 2025.
World J Radiol. Jul 28, 2025; 17(7): 106556
Published online Jul 28, 2025. doi: 10.4329/wjr.v17.i7.106556
Published online Jul 28, 2025. doi: 10.4329/wjr.v17.i7.106556
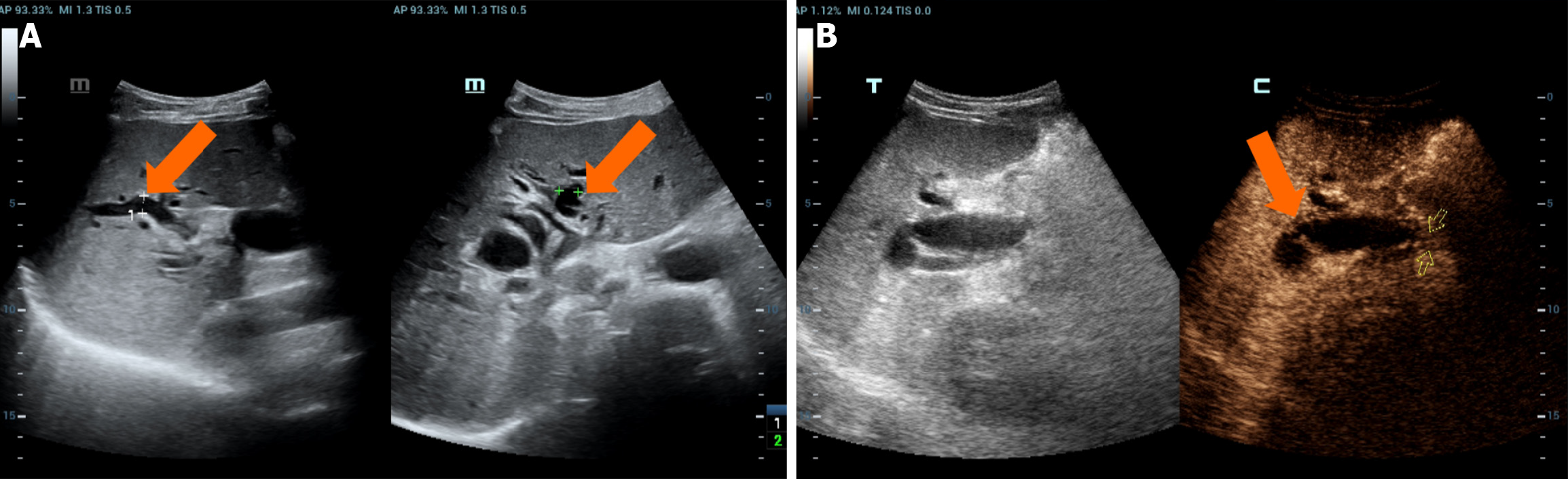
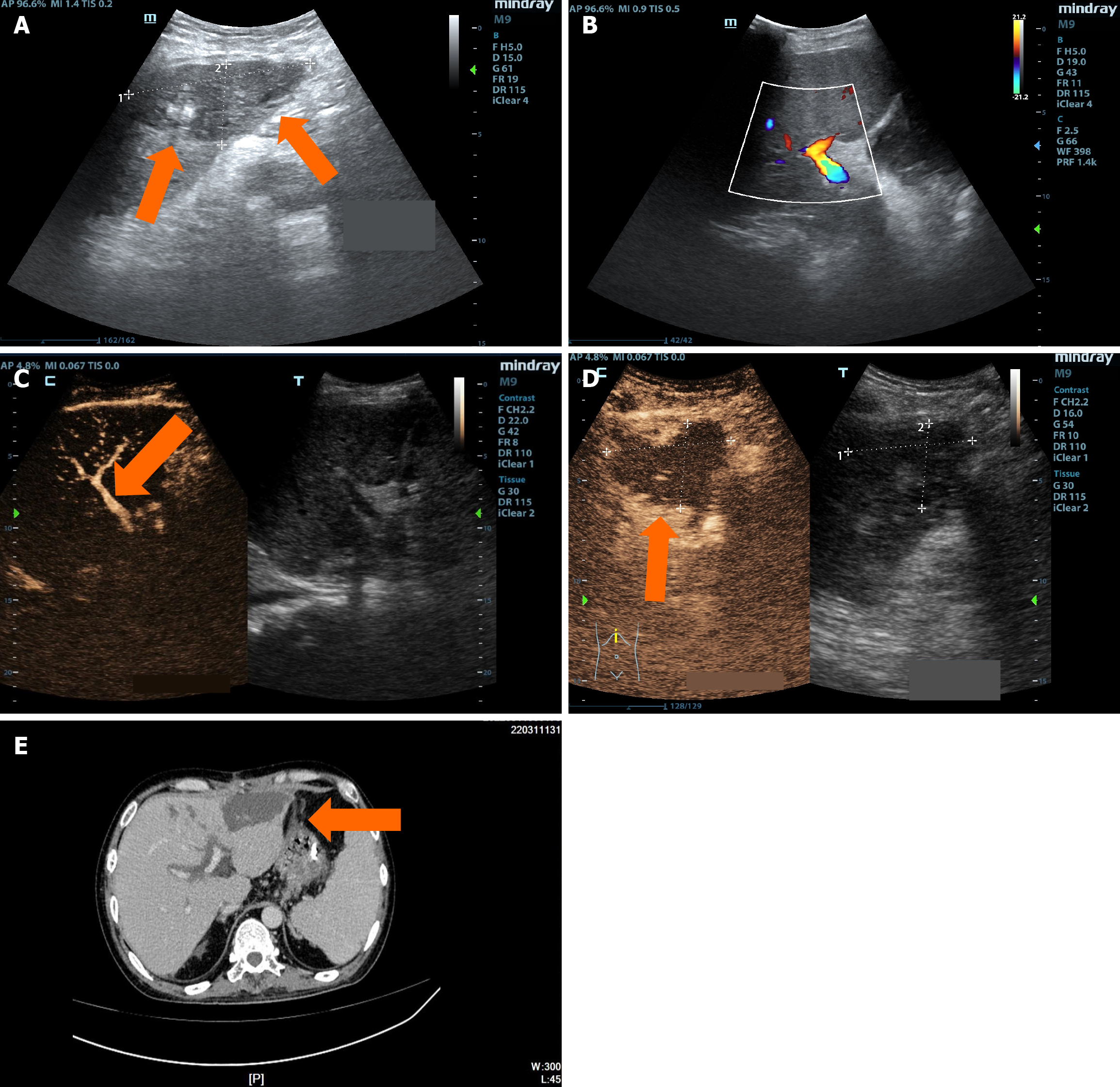
Figure 1 A 68-year-old male patient who had undergone piggyback liver transplantation for primary hepatocellular carcinoma was examined more than four months postoperatively.
A: Two-dimensional ultrasound showed that the morphology and parenchymal echoes of the transplanted liver appeared normal, with no significant abnormalities. However, the intrahepatic and extrahepatic bile ducts were diffusely dilated, with the inner diameter of the widest part of the intrahepatic bile duct measuring 8.1 mm (indicated by the arrow); B: Intravenous contrast-enhanced ultrasound revealed Wedge-shaped stenosis at the common bile duct anastomosis and diffuse intrahepatic and extrahepatic bile duct dilation. Magnetic resonance cholangiopancreatography later confirmed the diagnosis of anastomotic biliary strictures. Frequency of ultrasonic probe: 3.5 MHz; Contrast agent: SonoVue® (Bracco).
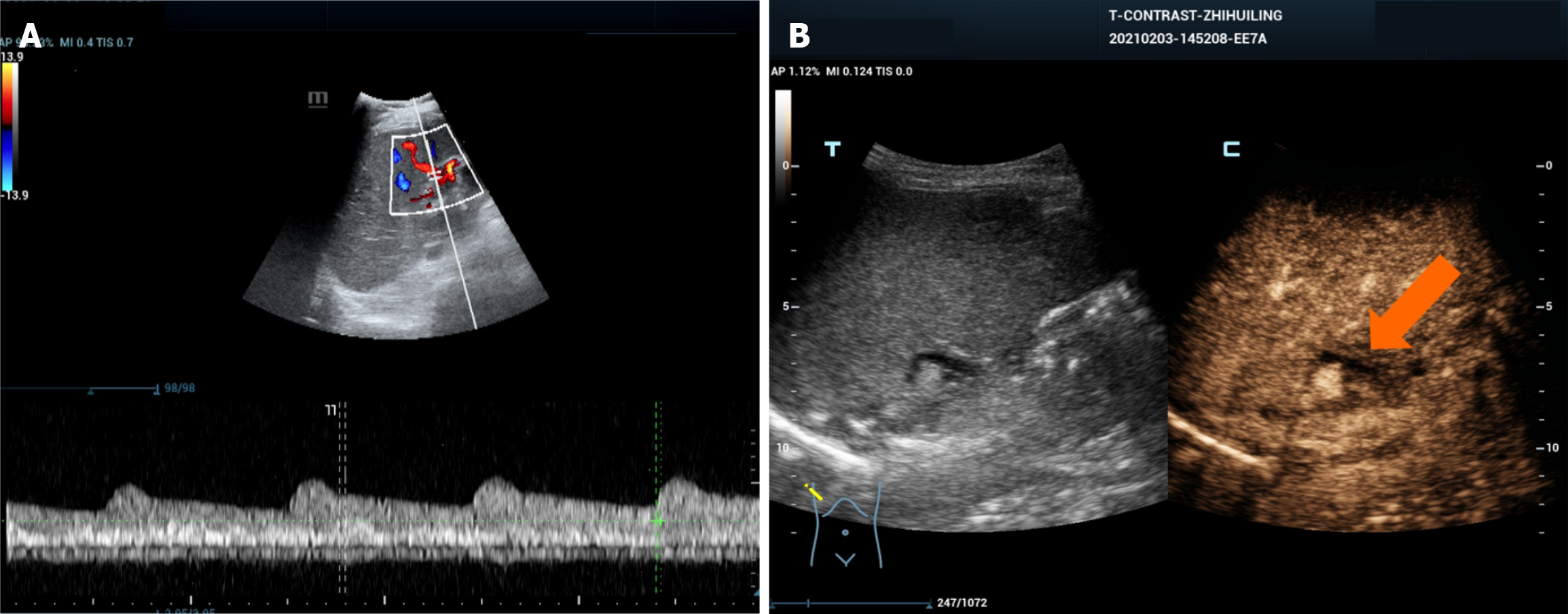
Figure 2 A 46-year-old female patient who underwent liver transplantation due to liver failure.
Three months postoperatively, an ultrasound examination revealed ischemia of the bile duct wall near the porta hepatis region. A: Color Doppler ultrasound indicated a reduced hepatic artery resistance index in the right hepatic artery; B: Intravenous contrast-enhanced ultrasound showed mild stenosis of the upper segment of the common bile duct, mild dilation of the intrahepatic bile ducts, and low perfusion of the bile duct wall arteries near the porta hepatis region during the arterial phase (indicated by the arrow).
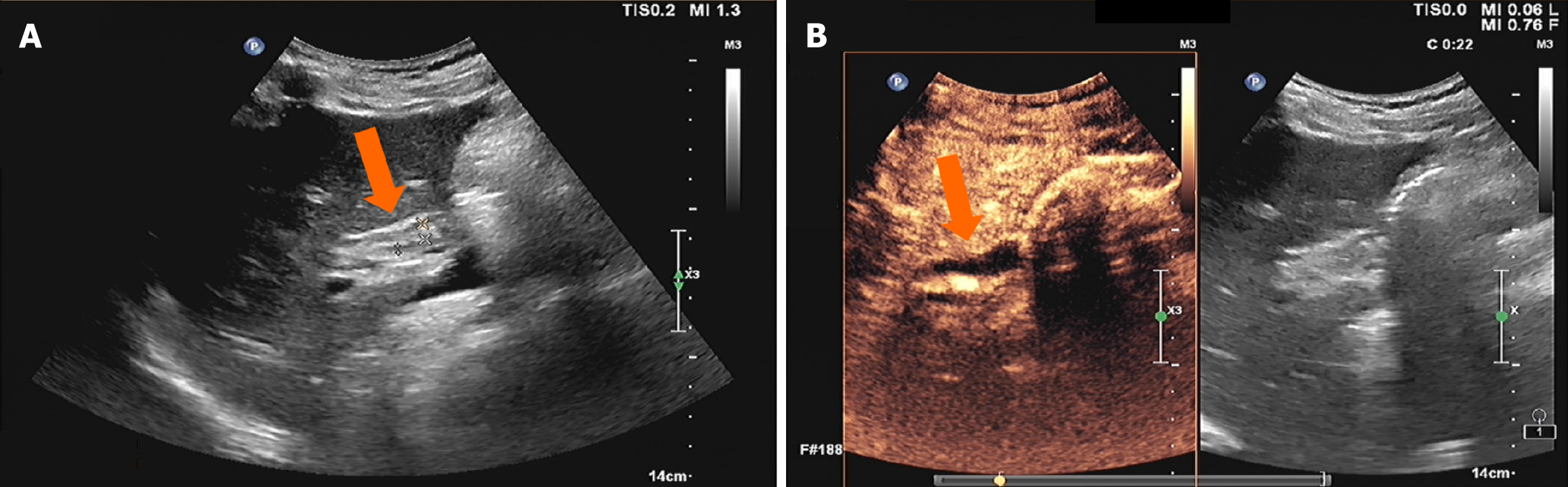
Figure 3 A 57-year-old male patient who underwent liver transplantation due to liver failure.
More than two months postoperatively, an ultrasound examination revealed necrosis of the bile duct wall near the porta hepatis region. A: Two-dimensional ultrasound revealed that morphology and parenchymal echoes of the transplanted liver showed no significant abnormalities. The common bile duct wall was edematous and thickened, measuring approximately 5.3 mm in thickness, with a narrowed lumen of about 2.3 mm (indicated by the arrow); B: Contrast-enhanced ultrasound revealed complete non-perfusion of the bile duct wall near the common bile duct anastomosis (indicated by the arrow).
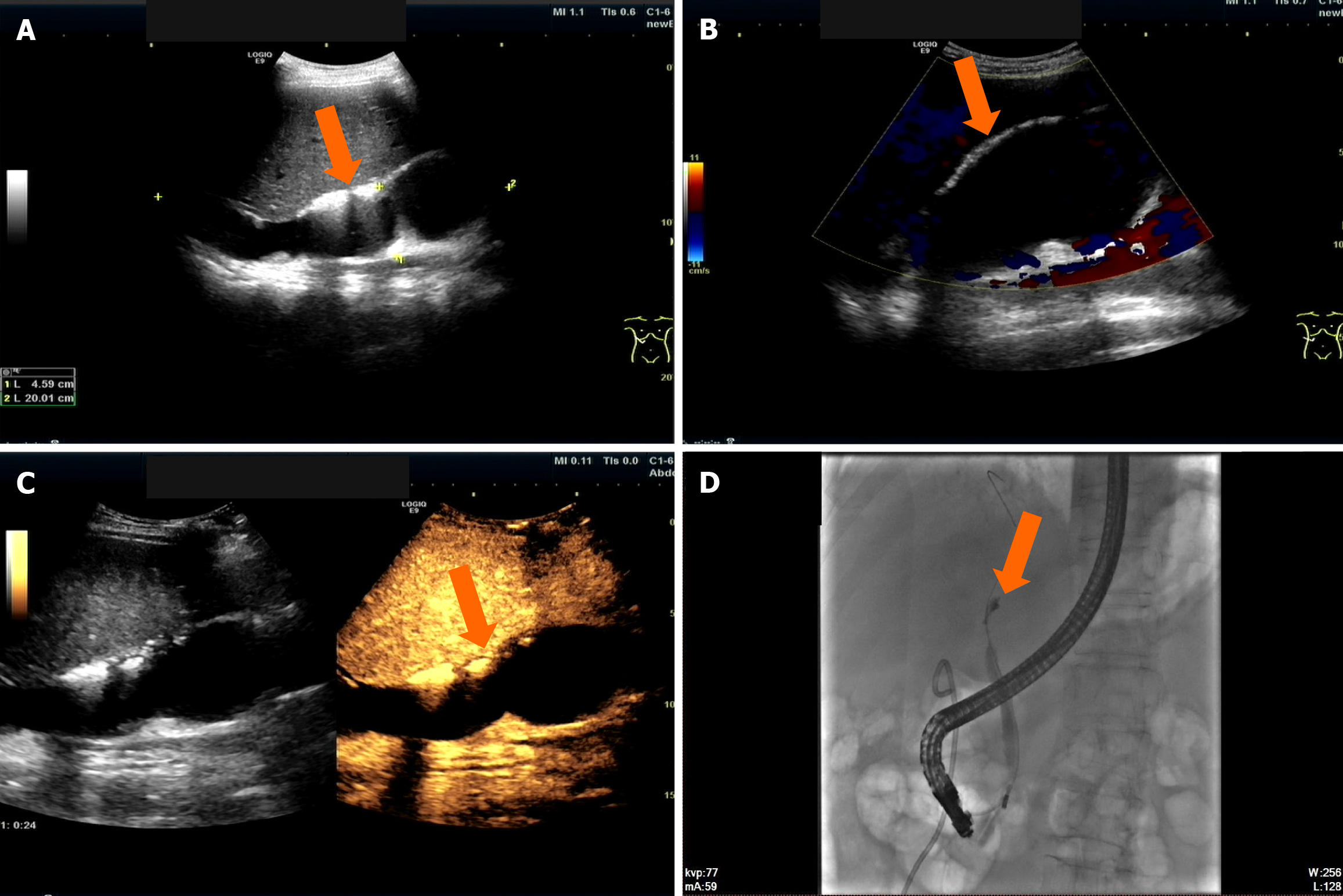
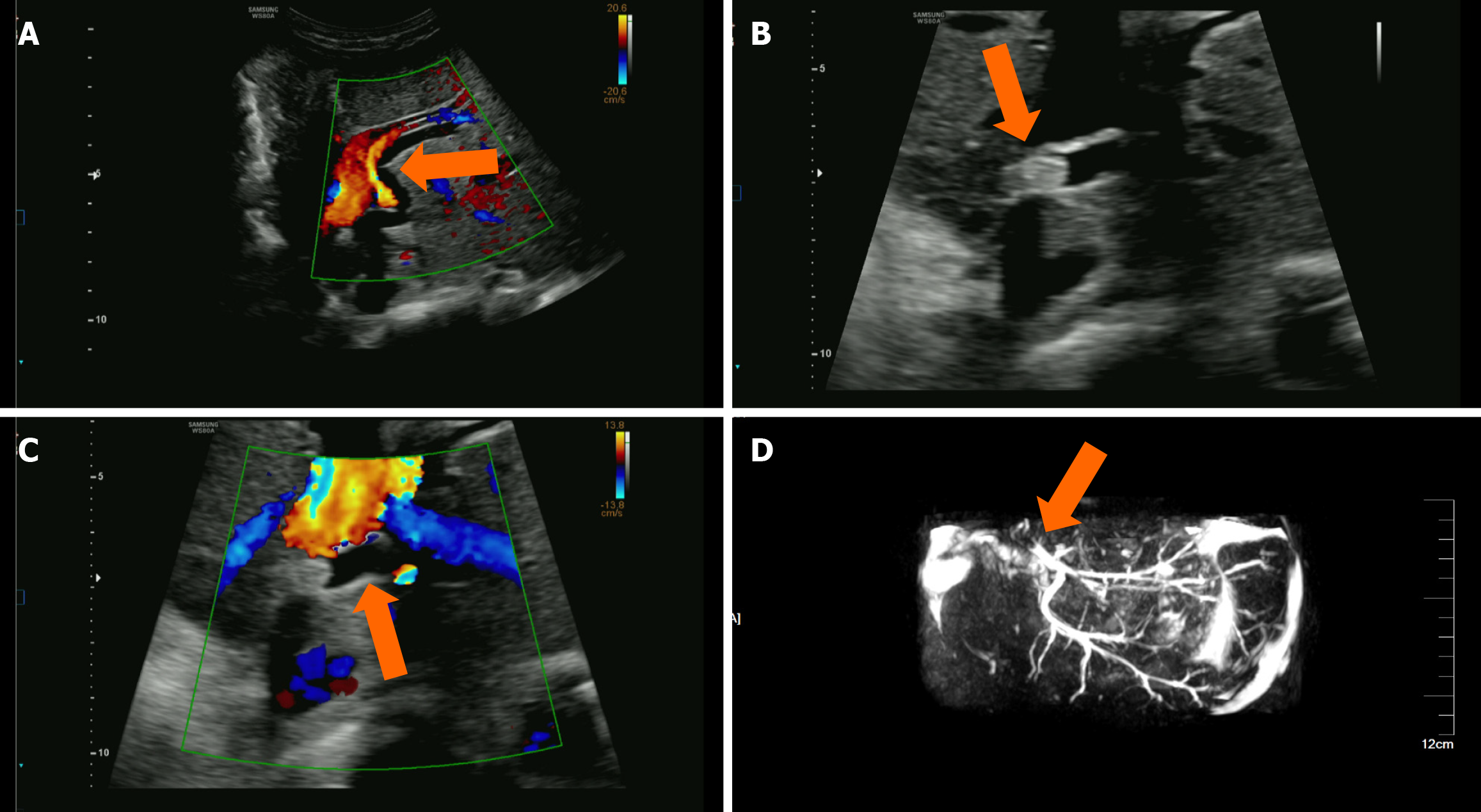
Figure 4 A 60-year-old male patient who underwent liver transplantation for primary biliary cirrhosis.
Twelve days postoperatively, an ultrasound examination revealed a biliary duct fistula. A and B: Two-dimensional ultrasound and color Doppler ultrasound showed that a large anechoic area with an irregular shape and good acoustic transmission was visible in the hepatic hilum, measuring approximately 200 mm × 46 mm, with no significant blood flow signals observed internally; C: Intravenous contrast-enhanced ultrasound showed no internal enhancement, with clear margins (indicated by the arrow); D: Endoscopic retrograde cholangiopancreatography showed that a catheter was successfully inserted, and a small amount of 10% Ultravist (Shering, Berlin, Germany) was injected. A narrow segment, approximately 8 mm long, was visible at the biliary duct anastomosis, and a fistula was observed in the intrahepatic biliary duct on the left side of the liver. The contrast agent infiltrated into the extrahepatic liver through the fistula (indicated by the arrow).
Figure 5 A 30-year-old male patient, more than 4 months post-liver transplantation, presented with a one-week history of fever and diarrhea, followed by vomiting and impaired consciousness for two hours.
A: Two-dimensional ultrasound showed multiple hypoechoic areas within the transplanted liver, suggestive of infarct foci; B: Color Doppler ultrasound showed that no arterial blood flow signals were observed in the hepatic artery course area, indicating hepatic artery occlusion; C: Intravenous contrast-enhanced ultrasound (CEUS) showed no visualization of the entire hepatic artery, consistent with hepatic artery occlusion; D: Intravenous CEUS indicated no enhancement in multiple hypoechoic areas within the liver, consistent with infarct foci; E: Magnetic resonance imaging revealed multiple hypoattenuating lesions within the liver, with an increase in number and size compared to previous scans, suggesting biloma and intrahepatic biliary duct dilation.
Figure 6 Follow-up ultrasound examination of an 8-year-old girl who underwent split hepatic transplantation due to congenital biliary atresia.
A: Ultrasound showed intrahepatic biliary duct dilation with a smooth biliary duct wall; B and C: Two-dimensional ultrasound showed that a high-echo mass approximately 12 mm × 6 mm in size was visible within the dilated intrahepatic biliary duct, with clear margins from the biliary duct wall and no posterior acoustic shadowing. Color Doppler ultrasound showed no significant color flow signals inside or around the high-echo mass; D: Magnetic resonance cholangiopancreatography showed intrahepatic biliary stones with biliary duct dilation.
- Citation: Zhang Y, Hao J, Luo Z, Li YJ, Liu Z, Zhao NB. Detecting biliary complications following liver transplantation with contrast-enhanced ultrasound. World J Radiol 2025; 17(7): 106556
- URL: https://www.wjgnet.com/1949-8470/full/v17/i7/106556.htm
- DOI: https://dx.doi.org/10.4329/wjr.v17.i7.106556