©The Author(s) 2024.
World J Radiol. Oct 28, 2024; 16(10): 552-560
Published online Oct 28, 2024. doi: 10.4329/wjr.v16.i10.552
Published online Oct 28, 2024. doi: 10.4329/wjr.v16.i10.552
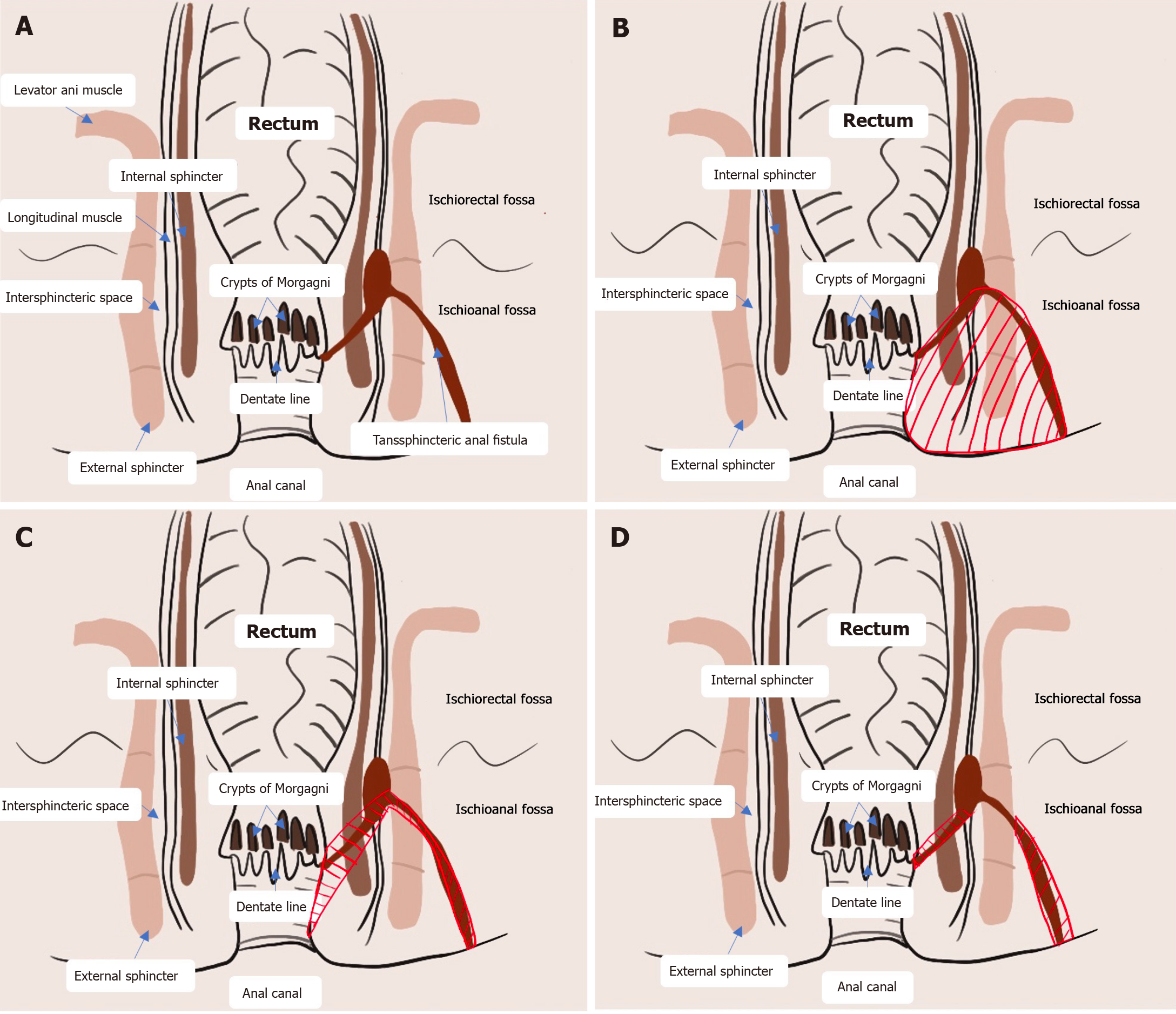
Figure 1 Representative images showing the surgical procedure for anal fistulas; the red shaded area indicates the surgical wound, and the green arrow denotes the surgical approach and operating path.
A: Drainage from the intersphincteric infection contaminates the anal glands and perianal space through the glandular branches, creating an anal fistula and intersphincteric abscess; B: Fistulectomy involves the surgical removal of fistula tissues and surrounding muscles, fat and connective tissues, resulting in a large wound area; C: Transanal opening of the intersphincteric space (TROPIS) involves the identification of the internal opening by injecting methylene blue or using a probe, followed by opening the fistula tract in the intersphincteric plane through the transanal route, resecting the lower part of the internal sphincter and scraping out the remaining branching fistulas; D: Modified TROPIS involves the widening of the intersphincteric plane through the transanal route and the identification of the internal opening easily and precisely, followed by drainage of the fistulas passing through the intersphincteric plane and tunnel-like fistulectomy of fistulas located lateral to the external sphincter. Branching fistulas with larger curvatures located lateral to the external sphincter are scraped out.
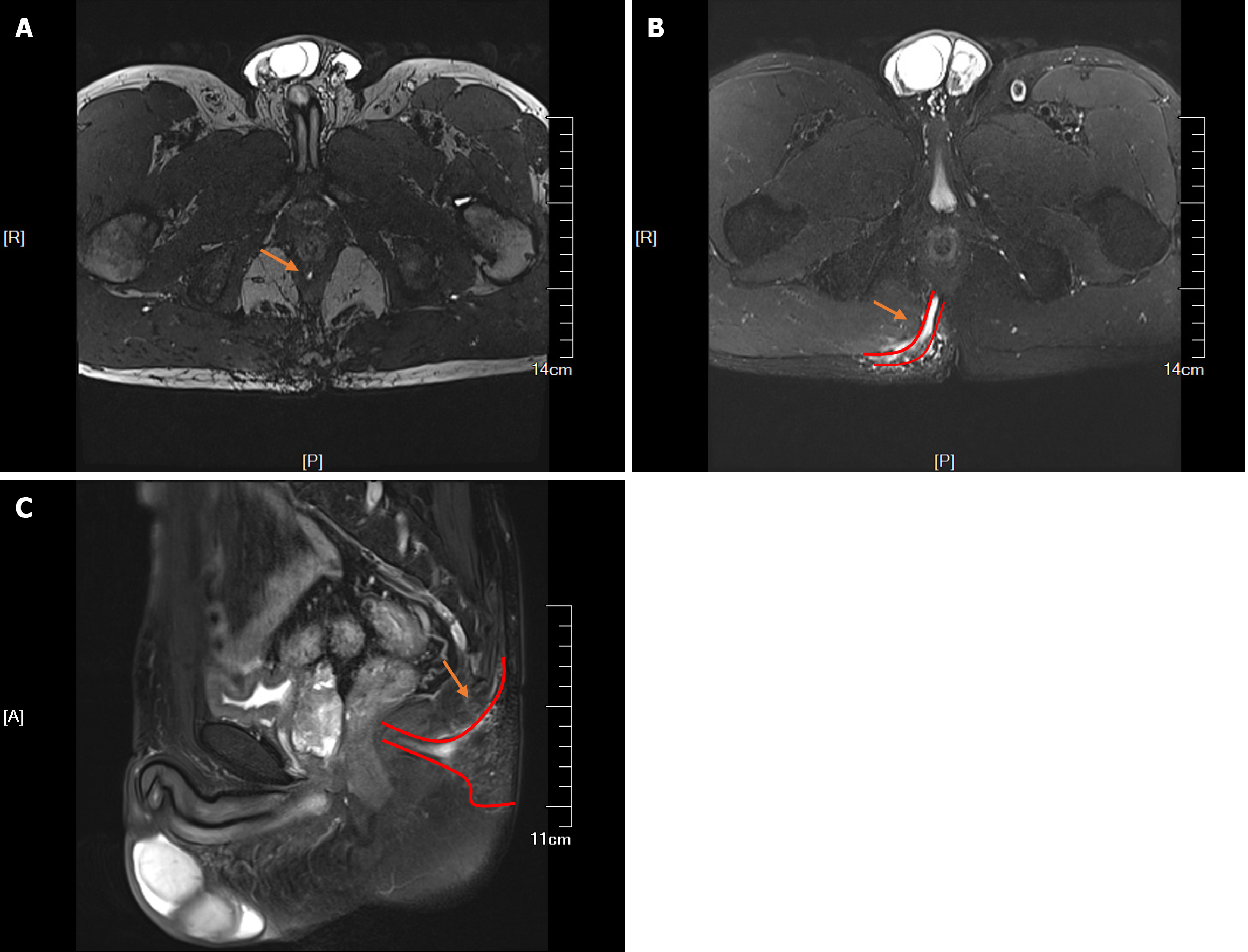
Figure 2 Magnetic resonance imaging of a patient with a high complex anal fistula.
A: Identification of the internal opening; B: Visualization of the main fistula with a broad range of perianal infection; C: Upwards spread of the infection responsible for the fistula.
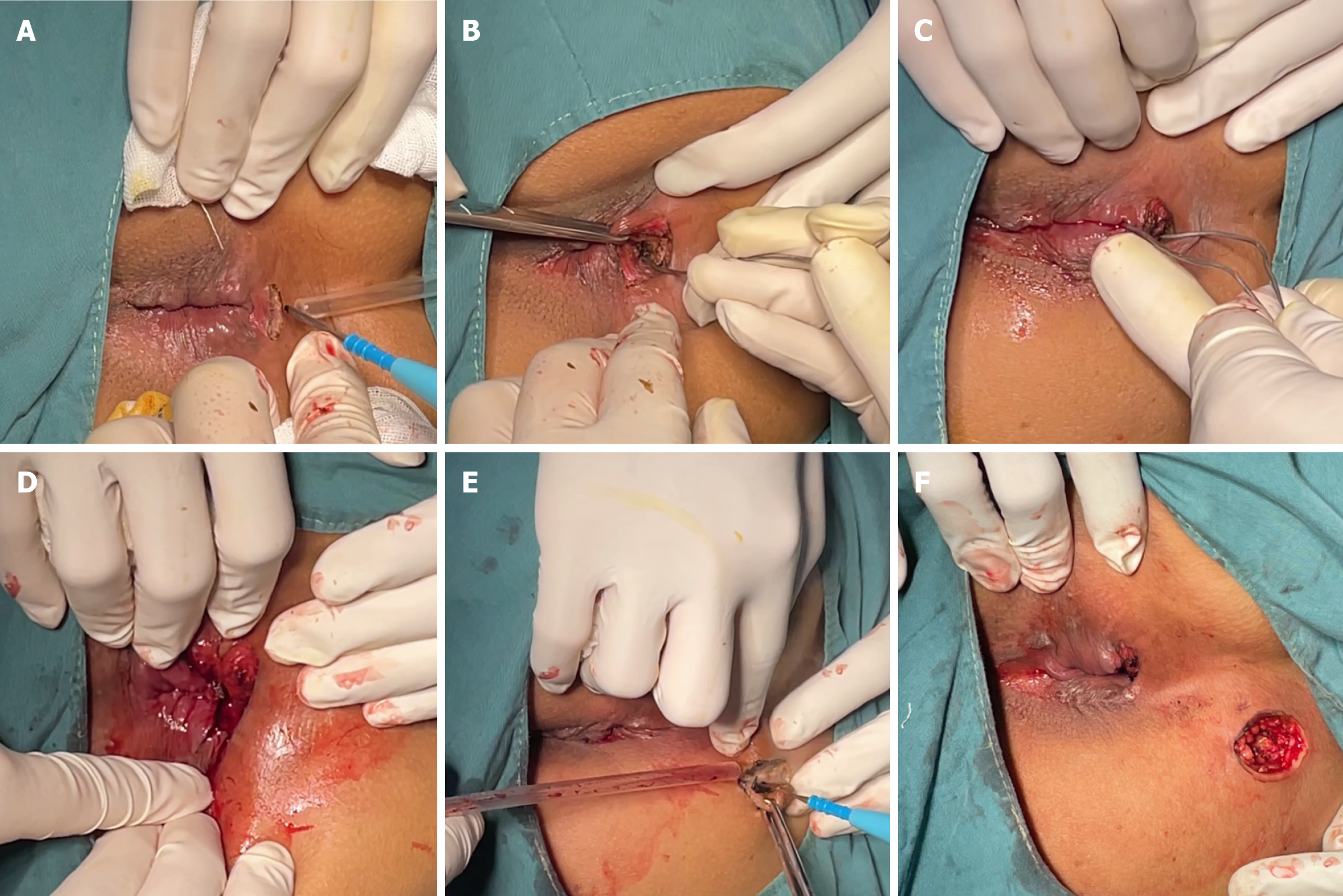
Figure 3 Procedure of the modified transanal opening of the intersphincteric space.
A: An arc-shaped incision was made at the posterior median intersphincter groove of the perianal area, and the sphincter space was opened; B: The probe was inserted into the sphincter space to identify the internal opening; C: The probe was passed through the internal opening; D: A small part of the internal sphincter and connective tissues inferior to the internal opening were incised, and the edges of the incision were ligated and trimmed; E: A circular incision was made at the external incision, and then tunnel-like fistulectomy of the fistulas at the lateral side of the external sphincter was performed; F: Intact skin on and beneath the external sphincter was preserved.
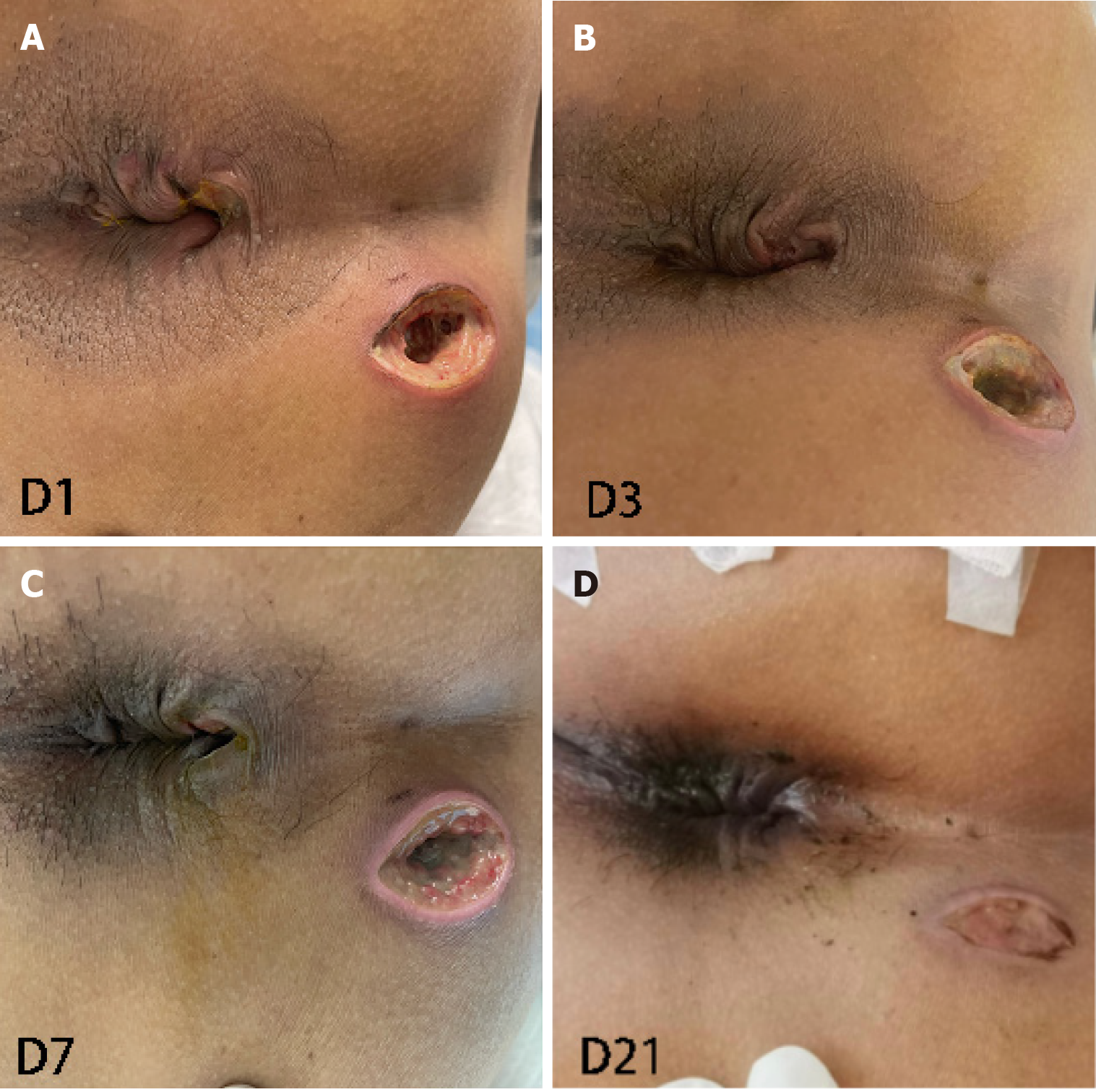
Figure 4 Wound healing at 1, 3, 7 and 21 days after surgery.
A: Day 1; B: Day 3; C: Day 7; D: Day 21.
Figure 5
Complete healing of the wound was observed at the 2-month follow-up.
- Citation: Wang YQ, Wang Y, Jia XF, Yan QJ, Zheng XP. High complex anal fistula managed by the modified transanal opening of the intersphincteric space via the inter-sphincteric approach: A case report. World J Radiol 2024; 16(10): 552-560
- URL: https://www.wjgnet.com/1949-8470/full/v16/i10/552.htm
- DOI: https://dx.doi.org/10.4329/wjr.v16.i10.552