©The Author(s) 2021.
World J Radiol. Jun 28, 2021; 13(6): 192-222
Published online Jun 28, 2021. doi: 10.4329/wjr.v13.i6.192
Published online Jun 28, 2021. doi: 10.4329/wjr.v13.i6.192
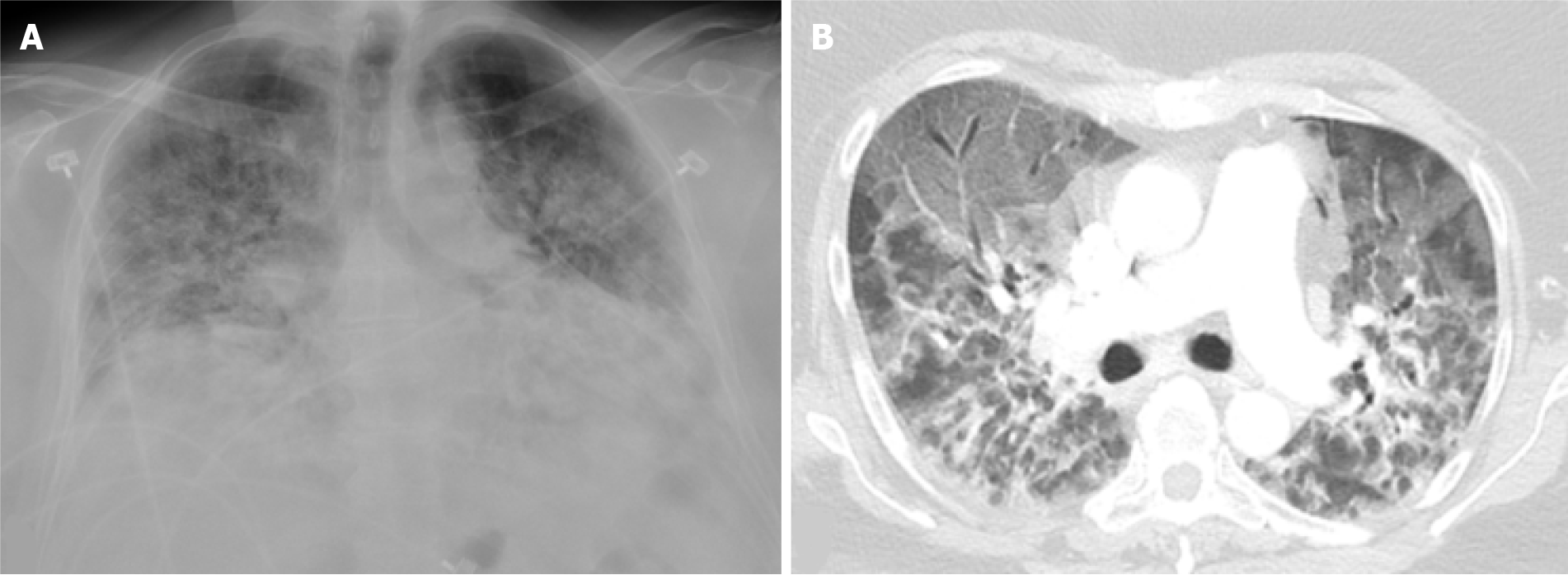
Figure 1 Severe coronavirus disease 2019 pneumonia.
Portable chest X-ray and axial image from a computed tomography of the chest in a 52-yr-old female with a history of morbid obesity who was admitted for acute hypoxic respiratory failure secondary to severe acute respiratory syndrome coronavirus 2. A: Chest X-ray shows low lung volumes with diffuse bilateral alveolar and interstitial opacities; B: Chest computed tomography shows diffuse ground glass opacities anteriorly, typical of acute lung injury. The peribronchial and perilobular opacities posteriorly are typical of acute lung injury that has entered a healing phase. The patient subsequently expired.
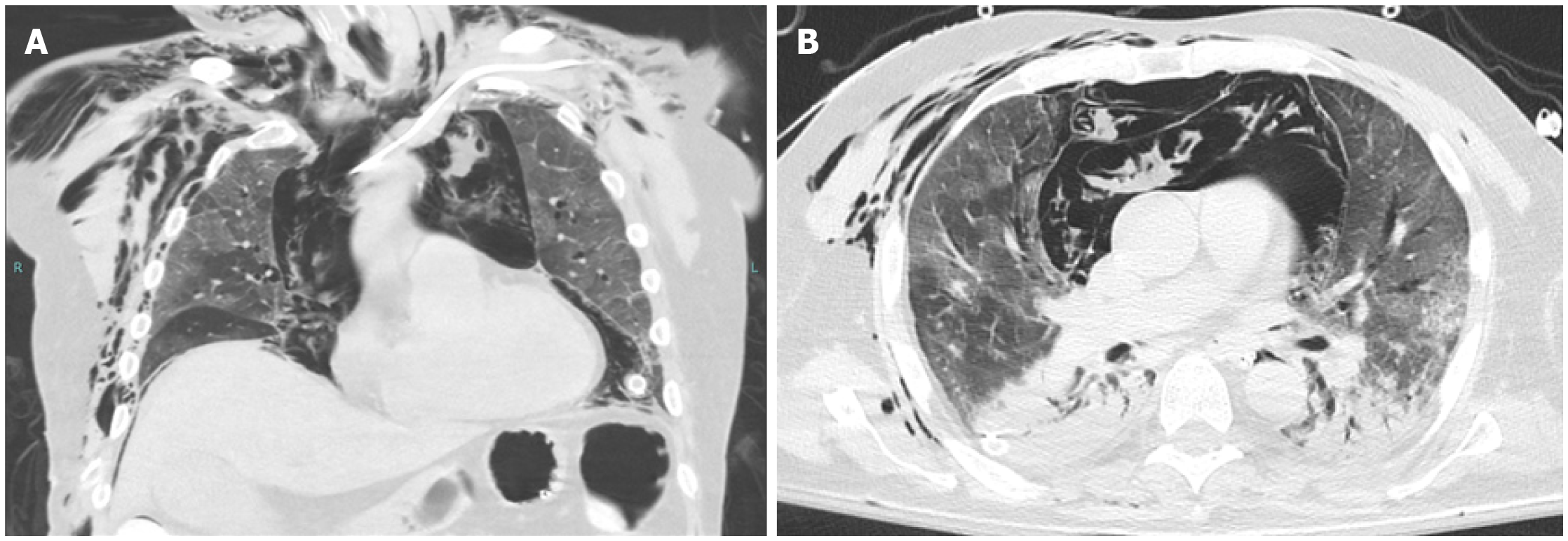
Figure 2 Barotrauma.
A and B: Coronal (A) and axial (B) images from an unenhanced computed tomography of the chest of a 75-yr-old male with no significant past medical history, who was intubated for acute hypoxic respiratory failure secondary to coronavirus disease 2019 pneumonia. There are ground glass opacities anteriorly, as well as consolidations with air bronchograms posteriorly, a pattern typical for acute respiratory distress syndrome. There is a massive amount of air within the mediastinum resulting from alveolar rupture (Macklin effect). The arrow on image (A) points to interstitial emphysema, surrounding a pulmonary vein. The arrow on image (B) points to nonanatomic air within a pulmonary lobule, which may represent the initial barotrauma event. There is extensive soft tissue emphysema in the lower neck and lateral chest wall, as well as in the extraperitoneal space of the abdominal cavity. Bilateral thoracostomy tubes and a peripherally-inserted central catheter are in place. The patient could not be weaned from ventilation and subsequently expired.
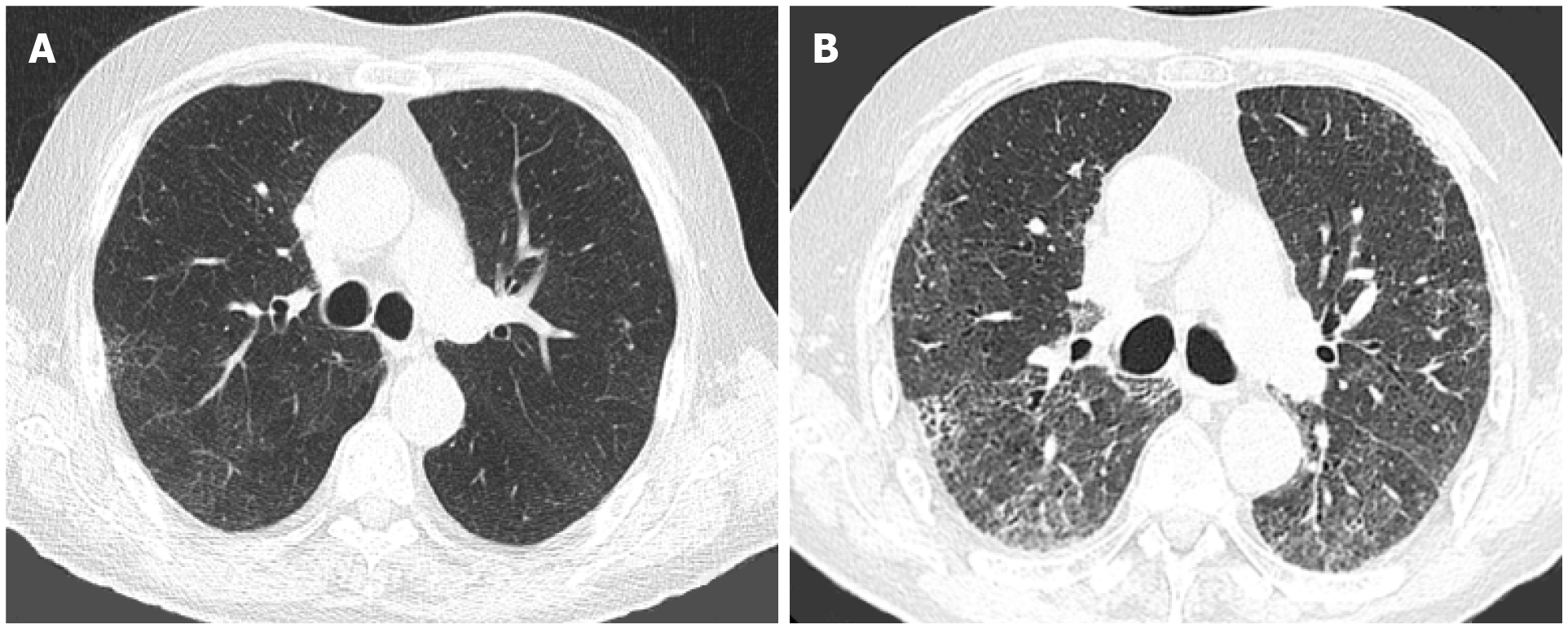
Figure 3 Pulmonary fibrosis.
Axial images from computed tomographies of the chest performed 2 yr apart in an 83-yr-old male with a history of silicosis. A: In June 2018, there was mild lung hyperaeration with mild reticulation; B: In August 2020, 4 mo after recovering from coronavirus disease 2019 pneumonia, there is extensive fibrosis, with areas of honeycombing, traction bronchiectasis/bronchiolectasis and architectural distortion.
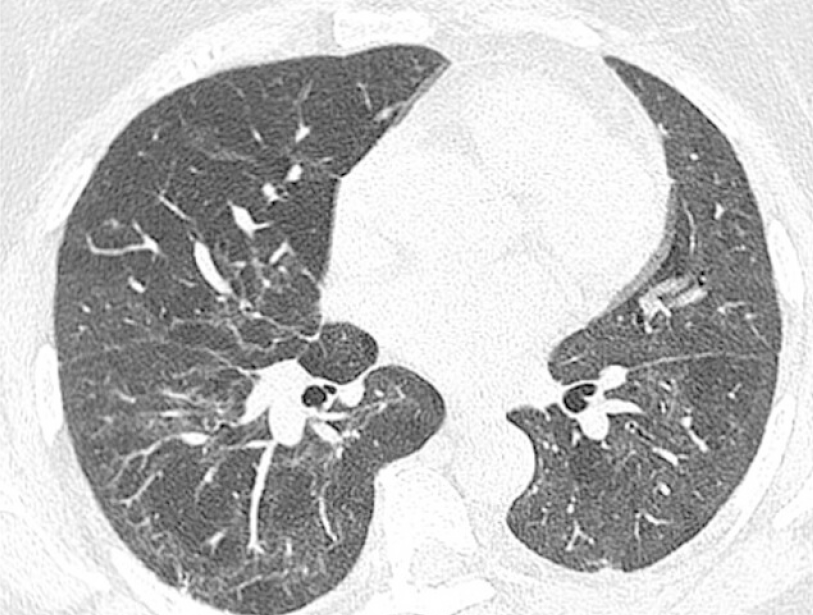
Figure 4 Non-specific interstitial pneumonia.
Axial image from a computed tomography of the chest in a 59-yr-old female 6 mo after recovering from acute hypoxic respiratory failure secondary to coronavirus disease 2019. Mild fibrosis in a peribronchial distribution and subpleural sparing in the right lower lobe is in keeping with mild fibrotic non-specific interstitial pneumonia. There is also a mosaic pattern caused by obstructive small airways disease (confirmed on expiration views, not shown), with altered perfusion in the lungs.
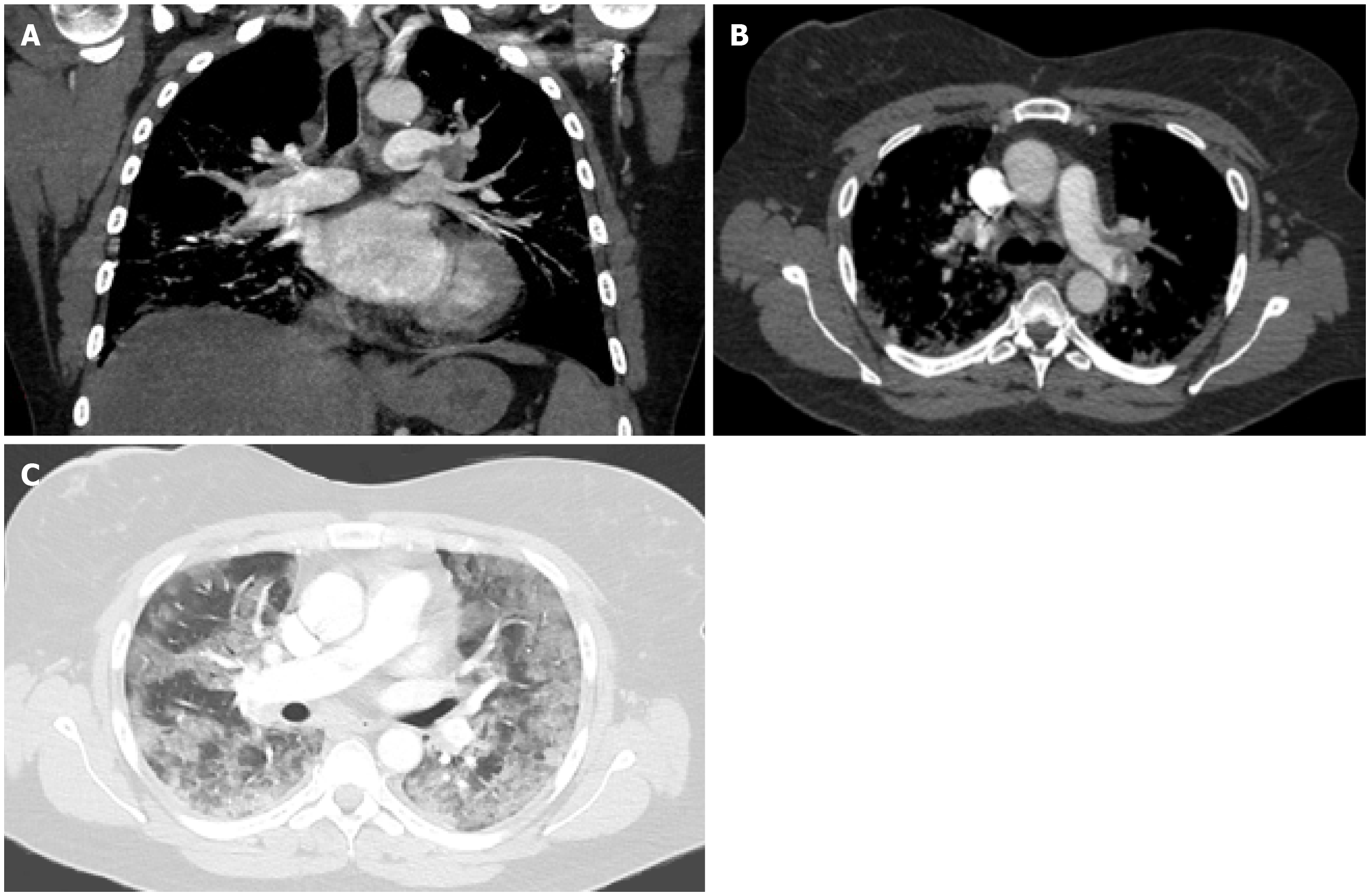
Figure 5 Pulmonary embolism.
A-C: Coronal (A) and axial (B and C) images from a computed tomography angiography of the chest in a 53-year-old female with a history of chronic lymphocytic leukemia and asthma who was admitted for acute hypoxic respiratory failure secondary to coronavirus disease 2019 pneumonia, complicated by pulmonary emboli. A large filling defect is seen in the left pulmonary artery extending into lobar and segmental branches (A and B). Diffuse ground glass opacities are noted on the lungs bilaterally (C).
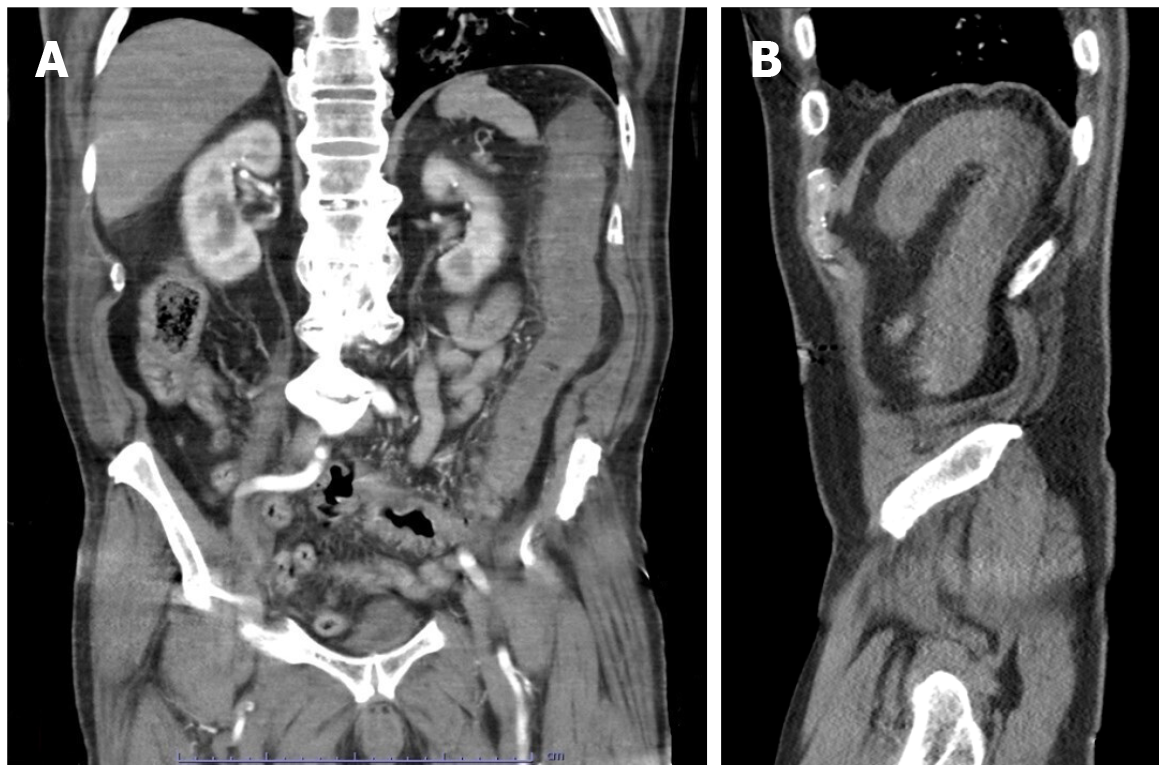
Figure 6 Acute ischemic colitis.
A and B: Coronal (A) and sagittal (B) reconstructed images from a computed tomography angiogram of the abdomen and pelvis in an 80-yr-old male admitted for sepsis and lactic acidosis. There is bowel wall thickening and hypoenhancement involving the descending colon, with surrounding inflammatory changes. There is no evidence of pneumatosis coli, pneumoperitoneum or proximal vessel occlusion. Bilateral ground-glass opacities were visualized at the lung bases (not shown). The patient was positive for severe acute respiratory syndrome coronavirus 2.
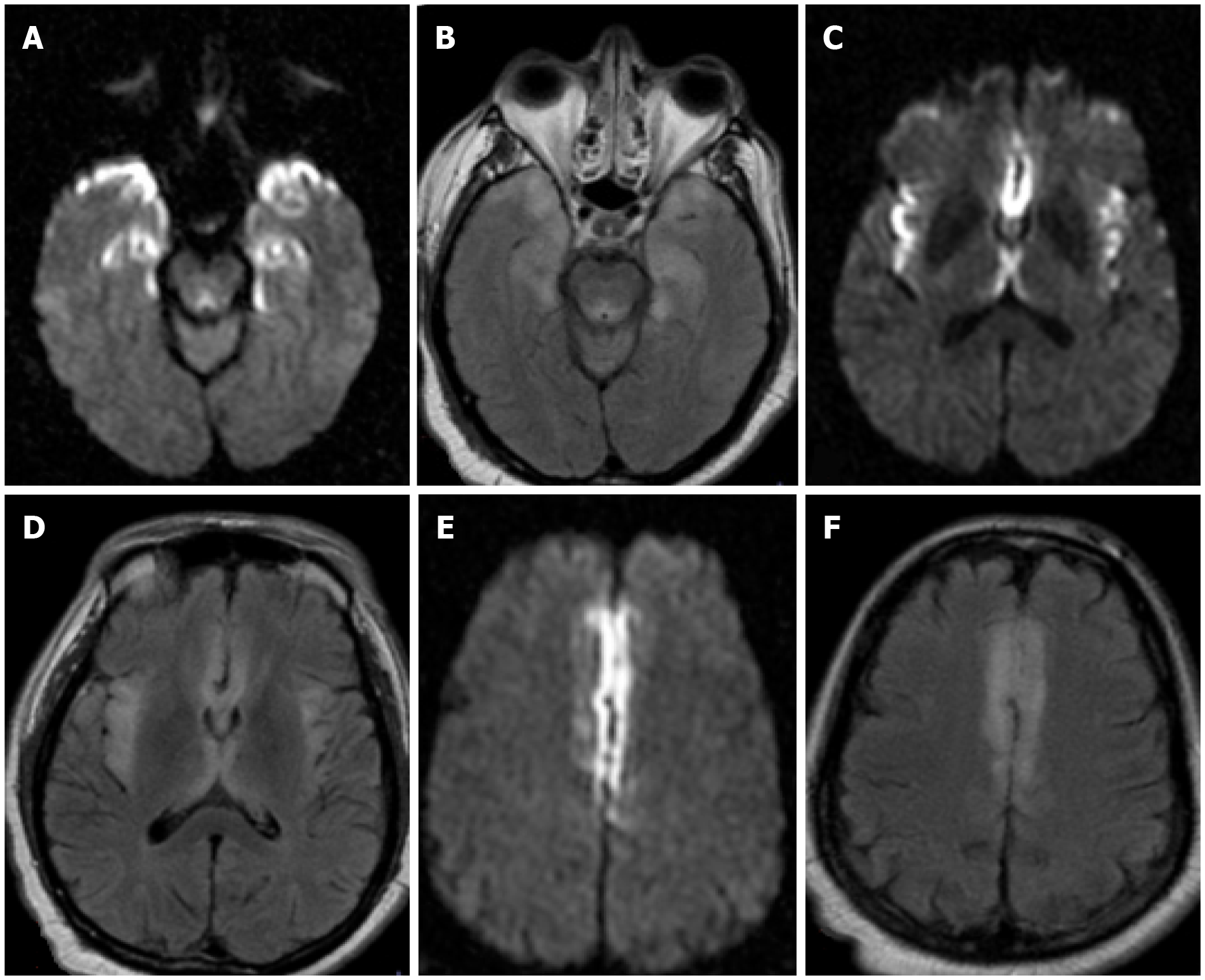
Figure 7 Encephalopathy.
A-F: Axial DWI (A, C and E) and FLAIR (B, D and F) sequences from a brain MRI in a 49-year-old - male who was admitted for acute hypoxic respiratory failure secondary to severe acute respiratory syndrome coronavirus 2. A brain MRI was ordered 3d after presentation for progressive lethargy. There were multifocal symmetric areas of restricted diffusion and T2/FLAIR prolongation in bilateral mesial temporal lobes (A and B), insular cortex (C and D), and cingulate cortex (E and F). Cerebrospinal fluid analysis was negative. The patient’s mental status gradually returned to baseline after medical management. Findings were attributed to COVID-19 – related encephalopathy.
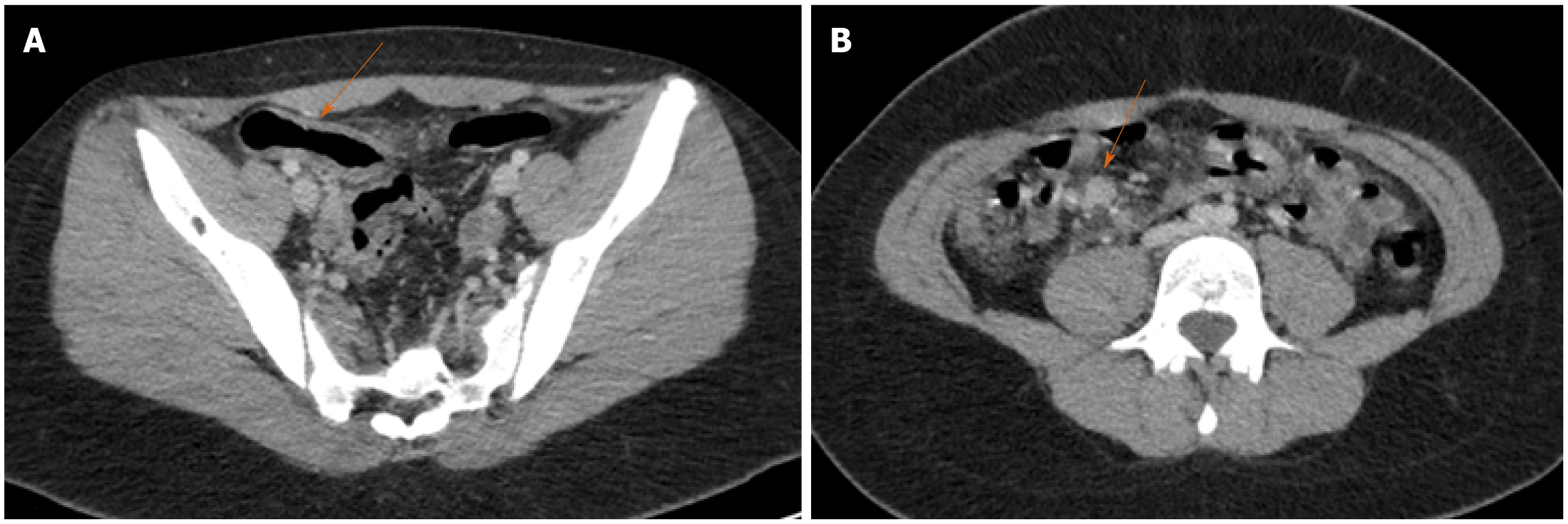
Figure 8 Terminal ileitis in the setting of multisystem inflammatory syndrome in a child.
Axial images of a contrast-enhanced computed tomography of the abdomen and pelvis in a 13-yr-old female who presented with a 4d history of abdominal pain. A: There is wall thickening in the terminal ileum with adjacent fat stranding; B: Multiple reactive lymph nodes are seen in the right lower quadrant. Clinical and laboratory findings met criteria for multisystem inflammatory syndrome in children. Of note, the patient had tested positive for severe acute respiratory syndrome coronavirus-2 4 wk prior to presentation. The patient recovered after medical treatment including intravenous immunoglobulin, prednisone and dopamine.
- Citation: Sideris GA, Nikolakea M, Karanikola AE, Konstantinopoulou S, Giannis D, Modahl L. Imaging in the COVID-19 era: Lessons learned during a pandemic. World J Radiol 2021; 13(6): 192-222
- URL: https://www.wjgnet.com/1949-8470/full/v13/i6/192.htm
- DOI: https://dx.doi.org/10.4329/wjr.v13.i6.192