Published online Sep 26, 2025. doi: 10.4330/wjc.v17.i9.111044
Revised: July 5, 2025
Accepted: August 15, 2025
Published online: September 26, 2025
Processing time: 87 Days and 23.3 Hours
Coronary artery bypass grafting (CABG) and percutaneous coronary intervention (PCI) are well-established treatments for multivessel coronary artery disease (CAD), a condition where multiple heart arteries are narrowed. A newer approach, fractional flow reserve (FFR)-guided PCI, uses a specialized measurement to select which artery blockages to treat, aiming to enhance patient outcomes. Despite its adoption, the comparative effectiveness of FFR-guided PCI vs CABG remains unclear, particularly regarding key health outcomes such as survival, heart-related complications, and the need for further procedures.
To evaluate the safety and effectiveness of FFR -guided PCI compared to CABG in patients with multivessel CAD.
This meta-analysis followed standard reporting guidelines and included randomized controlled trials (RCTs) comparing FFR-guided PCI with CABG in patients with multivessel CAD. We searched medical databases, including PubMed, EMBASE, ScienceDirect, and ClinicalTrials.gov, from their start to May 2025. We calculated combined risk ratios (RRs) with 95% confidence intervals (95%CIs) to analyze the data.
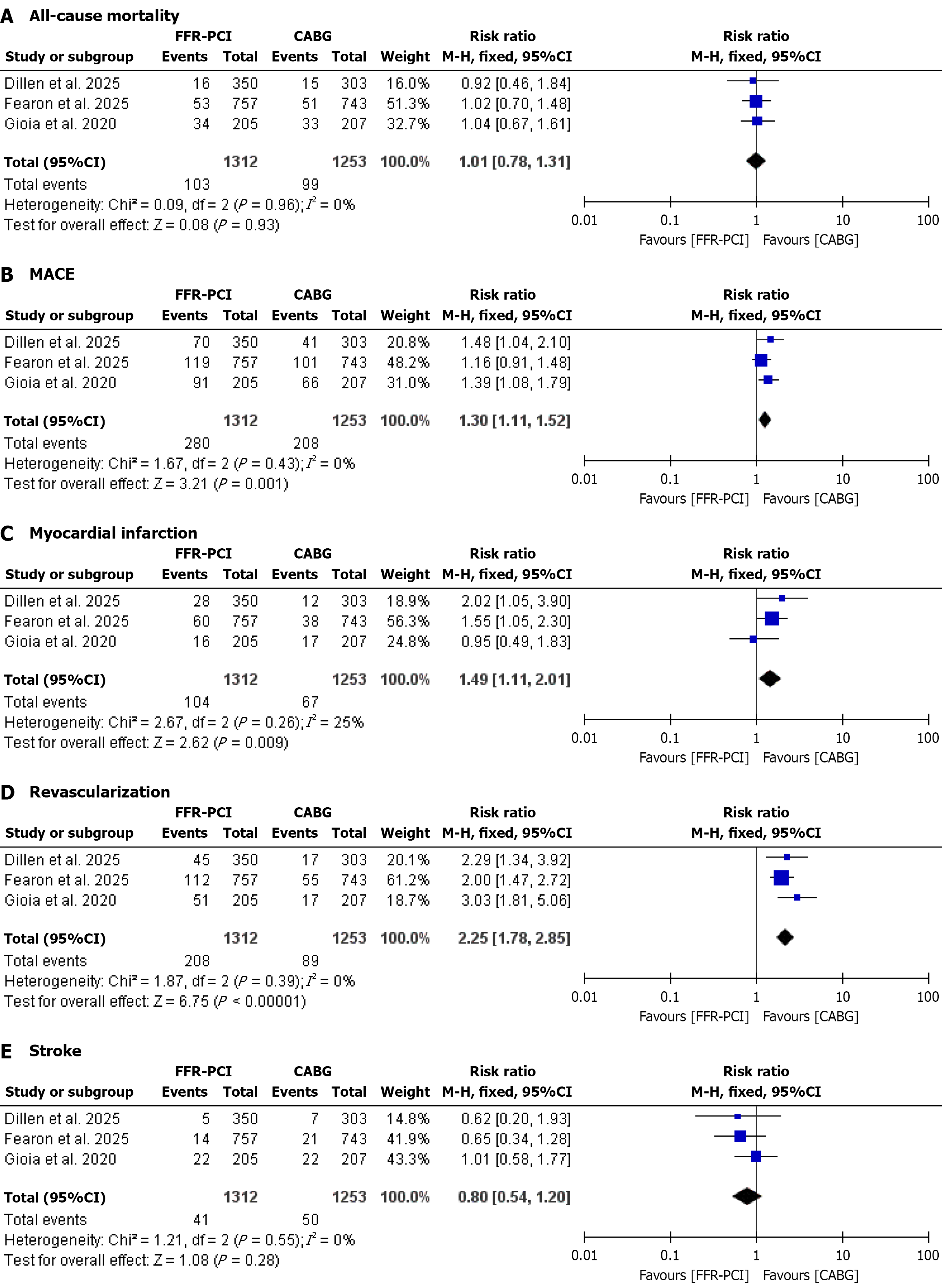
Three RCTs were analyzed. There was no notable difference in all-cause mortality between FFR-guided PCI and CABG (RR = 1.01, 95%CI: 0.78-1.31, P = 0.93). However, FFR-guided PCI showed higher rates of major adverse cardiac events (MACEs; RR = 1.30, 95%CI: 1.11-1.52, P = 0.001), myocardial infarction (RR = 1.49, 95%CI: 1.11-2.01, P = 0.009), and repeat revascularization (RR = 2.25, 95%CI: 1.78-2.85, P < 0.00001). Stroke rates were comparable between the two treatments (RR = 0.80, 95%CI: 0.54-1.20, P = 0.28).
FFR-guided PCI and CABG have similar rates of all-cause mortality and stroke in patients with multivessel CAD. However, CABG results in fewer MACEs, myocardial infarctions, and repeat procedures.
Core Tip: This meta-analysis compares fractional flow reserve (FFR)-guided percutaneous coronary intervention (PCI) with coronary artery bypass grafting (CABG) for multivessel coronary artery disease. While both treatments show similar all-cause mortality and stroke rates, CABG significantly reduces major adverse cardiac events, myocardial infarction, and repeat revascularization. These findings highlight CABG’s superior efficacy in managing complex coronary disease, challenging the broader adoption of FFR-guided PCI. The results underscore the need for tailored treatment strategies and further trials to optimize outcomes in diverse patient populations.
- Citation: Kataveni S, Ellahi E, Zafar F, Veettil INK, Iqbal A, Dhir B, Sabarish S, Erambalur S, Yathindra MR, Kvn M, Nawaz S, Dudekula SK, Haq UU, Hussain A, Khawar MM. Fractional flow reserve guided percutaneous coronary intervention vs coronary artery bypass grafting for multivessel coronary artery disease: A meta-analysis. World J Cardiol 2025; 17(9): 111044
- URL: https://www.wjgnet.com/1949-8462/full/v17/i9/111044.htm
- DOI: https://dx.doi.org/10.4330/wjc.v17.i9.111044
Multivessel coronary artery disease (CAD), defined as significant stenosis (> 70%) in two or more major coronary arteries with a diameter of 2.5 mm or greater, is a prevalent condition encountered in patients undergoing coronary angiography[1]. It poses a significant clinical challenge due to its association with extensive myocardial ischemia, impaired ventricular function, and an increased risk of adverse cardiac events, including myocardial infarction, heart failure, and mortality[1]. The management of multivessel CAD primarily involves two revascularization strategies: Percutaneous coronary inter
The introduction of fractional flow reserve (FFR) has transformed PCI by providing a physiological assessment of coronary stenoses. FFR measures the ratio of distal coronary pressure to aortic pressure during maximal hyperemia, with a value ≤ 0.80 indicating ischemia that warrants intervention[5]. By identifying functionally significant lesions, FFR-guided PCI reduces unnecessary stent placements and has been shown to lower the composite endpoint of death, non
Despite these advancements, the optimal revascularization strategy for multivessel CAD remains a subject of ongoing debate[8]. CABG, which bypasses both flow-limiting and angiographically mild lesions using arterial or venous grafts, has been associated with better long-term survival and lower rates of repeat revascularization, particularly in patients with higher SYNTAX scores or complex disease[9,10]. In contrast, FFR-guided PCI offers comparable outcomes in terms of mortality and major adverse cardiac events (MACEs) in certain populations, as demonstrated by the FFR vs angiogra
The conflicting results from individual randomized controlled trials (RCTs) and observational studies highlight significant clinical uncertainty[12]. Limitations such as small sample sizes, lack of randomization in subgroup analyses, and variability in patient populations (e.g., exclusion of left main disease or differences in SYNTAX scores) underscore the need for a comprehensive synthesis of evidence[13]. Moreover, advancements in medical technology, including newer-generation drug-eluting stents and improved surgical techniques, have altered the treatment landscape, necessitating updated comparisons[14]. A meta-analysis is, therefore, timely and essential to pool data from multiple studies, en
A meta-analysis is, therefore, timely and essential to pool data from multiple studies, enhancing statistical power and providing robust estimates of treatment effects across diverse patient populations. This meta-analysis aims to systematically compare the efficacy and safety of FFR-guided PCI vs CABG in patients with multivessel CAD, focusing on key clinical outcomes such as all-cause mortality, myocardial infarction, stroke, and the need for repeat revascularization. By addressing heterogeneity across studies and incorporating contemporary data, this study seeks to clarify the optimal revascularization strategy, inform clinical guidelines, and support patient-centered decision-making for this high-risk population.
This systematic review and meta-analysis were conducted per the PRISMA 2020 guidelines[15,16]. The protocol is registered on PROSPERO CRD420251077550.
Inclusion criteria: The inclusion criteria for this systematic review and meta-analysis included studies involving adult patients aged 18 years or older who were diagnosed with multivessel CAD, defined as at least a 50% diameter stenosis in two or more major epicardial vessels, with or without diabetes mellitus. Eligible studies compared FFR-guided PCI using contemporary drug-eluting stents with CABG, including both on-pump and off-pump techniques. Studies were required to report at least one of the following outcomes with a minimum follow-up of 3 years, prioritizing 5-year data when available: All-cause mortality (primary outcome), MACEs, myocardial infarction, repeat revascularization, or stroke, as defined by individual studies. Only RCTs and observational cohort studies published in English with full-text availability were included, with no restrictions on publication year.
Exclusion criteria: The exclusion criteria encompassed studies involving patients with single-vessel disease or isolated left main disease, those including patients presenting with acute coronary syndromes other than stable or unstable angina (e.g., ST-elevation myocardial infarction), and studies that did not employ FFR guidance for PCI. Additionally, non-comparative studies, case reports, editorials, expert opinions, and duplicates were excluded.
The search strategy for this meta-analysis was designed to retrieve studies from PubMed, EMBASE, ScienceDirect, and ClinicalTrials.gov, using MeSH and free-text keywords aligned with the PICOS framework. The search strategy for PubMed combined medical subject headings (MeSHs) terms is as follows ((((Fractional Flow Reserve, Myocardial[Mesh]) OR (Myocardial Fractional Flow Reserve)) AND ((((((((((((Percutaneous Coronary Intervention[Mesh]) OR (Coronary Intervention, Percutaneous)) OR (Coronary Interventions, Percutaneous)) OR (Intervention, Percutaneous Coronary)) OR (Interventions, Percutaneous Coronary)) OR (Percutaneous Coronary Interventions)) OR (Percutaneous Coronary Revascularization)) OR (Coronary Revascularization, Percutaneous)) OR (Coronary Revascularizations, Percutaneous)) OR (Percutaneous Coronary Revascularizations)) OR (Revascularization, Percutaneous Coronary)) OR (Revascularizations, Percutaneous Coronary))) AND (((((((((((((Coronary Artery Bypass[Mesh]) OR (Artery Bypass, Coronary)) OR (Artery Bypasses, Coronary)) OR (Bypasses, Coronary Artery)) OR (Coronary Artery Bypasses)) OR (Coronary Artery Bypass Grafting)) OR (Coronary Artery Bypass Surgery)) OR (Aortocoronary Bypass)) OR (Aortocoronary Bypasses)) OR (Bypass, Aortocoronary)) OR (Bypasses, Aortocoronary)) OR (Bypass Surgery, Coronary Artery)) OR (Bypass, Coronary Artery))) AND ((((((((((Coronary Stenosis[Mesh]) OR (Stenoses, Coronary)) OR (Stenosis, Coronary)) OR (Coronary Stenoses)) OR (Coronary Artery Stenosis)) OR (Artery Stenoses, Coronary)) OR (Artery Stenosis, Coronary)) OR (Coronary Artery Stenoses)) OR (Stenoses, Coronary Artery)) OR (Stenosis, Coronary Artery)) with free-text keywords, including “Fractional Flow Reserve, Myocardial,” “Percutaneous Coronary Intervention,” “Coronary Artery Bypass,” and “Coronary Stenosis”. Boolean operators (AND, OR) were used to combine terms. "Fractional Flow Reserve, Myocardial" OR "Myocardial Fractional Flow Reserve" was paired with "Percutaneous Coronary Intervention" OR synonyms (e.g., "Coronary Revascularization, Percutaneous") using AND, then combined with "Coronary Artery Bypass" OR synonyms (e.g., "Coronary Artery Bypass Grafting") using AND, and finally with "Coronary Stenosis" OR synonyms (e.g., "Coronary Artery Stenosis") using AND. The NOT operator was not used. These terms were tailored to each database to identify studies based on predefined population, intervention, comparison, and outcome criteria. Manual searches of bibliographies and grey literature, including conference proceedings, abstracts, and preprints, were performed to ensure comprehensive data collection.
All identified citations were imported into Zotero reference management software for duplicate removal. Two indepen
Data were extracted independently by two reviewers (Sabarish S and Kvn M) using a standardized, pre-piloted Google Sheets form. Extracted data included study characteristics (author, year, country, study design), participant demogra
The risk of bias for RCTs was assessed using the Cochrane Risk of Bias 2 (RoB 2) tool, which evaluates domains such as randomization process, deviations from intended interventions, missing outcome data, measurement of the outcome, and selection of reported results[17].
Although eligibility criteria allowed for observational cohort studies, none were included; however, had they been included, the Newcastle-Ottawa Scale (NOS) would have been used to assess bias, evaluating three domains: Selection of study groups (e.g., representativeness, selection of controls), comparability of groups (e.g., adjustment for confounders), and ascertainment of outcomes (e.g., adequacy of follow-up), with a maximum score of 9 stars indicating high quality. The RoB 2 tool is designed explicitly for RCTs, focusing on randomization-related biases, whereas NOS is suited for observational studies, addressing confounding and selection biases.
For each outcome, the number of events and the total number of patients in the FFR-guided PCI and CABG groups were extracted. These data were pooled using risk ratios (RRs) with 95% confidence intervals (95%CIs) calculated via the Mantel-Haenszel method. Heterogeneity was assessed using I2. For each outcome, a forest plot was constructed to visually analyze the data, and funnel plots were generated to check the publication bias. All statistical analyses were performed using Review Manager (RevMan) version 5.4. Following the statistical analysis, the quality of evidence for each outcome was evaluated using the GRADE approach, assessing domains such as risk of bias, inconsistency, impre
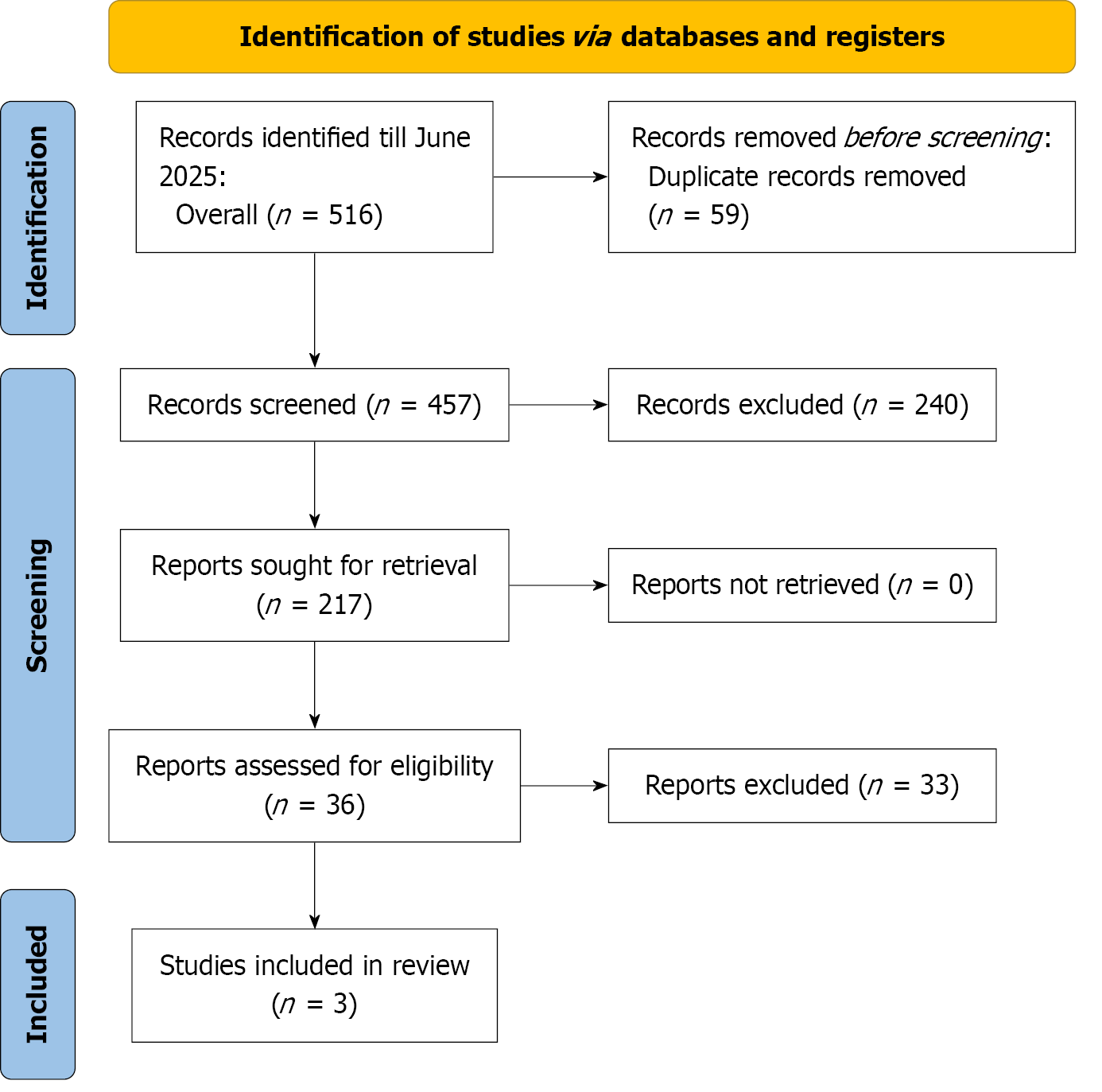
The PRISMA statement flowchart outlines the literature screening process and study selection. The initial search across multiple databases yielded 532 articles: PubMed (n = 118), EMBASE (n = 23), ScienceDirect (n = 389), and ClinicalTrials.gov (n = 2). After removing duplicates, 412 unique records were screened. From these, 36 full-text articles were retrieved for detailed assessment. Ultimately, 3 studies[8,18,19] met the eligibility criteria and were included in both the qualitative and quantitative meta-analyses. All included studies were RCTs (n = 3); no observational cohort studies met the inclusion criteria (Figure 1).
The meta-analysis included three RCTs comparing FFR-guided PCI vs CABG in patients with multivessel CAD, with baseline characteristics summarized across 3412 participants (1719 PCI, 1693 CABG). Sample sizes ranged from 205 to 757 for PCI and 207 to 743 for CABG. Mean ages were comparable, ranging from 65.33 to 67.43 years, with a slight male predominance (75.2%-83% male). Body mass index was reported in two studies, averaging 28.1-29.35 kg/m², indicating similar obesity profiles. Diabetes prevalence was approximately 28%-29% in one study, while hypertension was consistently high (70.1%-75%). Family history of CAD varied (21.6%-33%), and previous myocardial infarction was reported in 10.7%-34% of patients. The proportion of patients with left ventricular ejection fraction ≤ 50% was notably higher in Gioia et al[13] (2020; 66.2%-66.5%) compared to Fearon et al[8] (2025; 18%). Dillen et al[14] (2025) did not report most baseline characteristics, limiting comparisons. Overall, baseline characteristics were broadly similar across groups, supporting the comparability of PCI and CABG cohorts, though incomplete data in one study constrained comprehensive assessment (Table 1).
| Ref. | Study design | Sample size | Age (years) | Sex (male/female) | BMI (kg/m²) | Diabetes | Hypertension | Family history of CAD | Previous (MI) | LVEF ≤ 50% (%) | |||||||||
| PCI | CABG | PCI | CABG | PCI | CABG | PCI | CABG | PCI | CABG | PCI | CABG | PCI | CABG | PCI | CABG | PCI | CABG | ||
| Dillen et al[14], 2025 | RCT | 757 | 743 | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | |
| Fearon et al[8] 2025 | RCT | 757 | 743 | 65.67 ± 9.66 | 65.33 ± 8.91 | 81/19 | 83/17 | 28.3 | 28.1 | 28 | 29 | 71 | 75 | 33 | 29 | 33 | 34 | 18 | 18 |
| Gioia et al[13], 2020 | RCT | 205 | 207 | 67.35 ± 9.96 | 67.43 ± 8.35 | 75.9/24.1 | 75.2/24.8 | 29.35 | 29.09 | NA | NA | 70.5 | 70.1 | 21.6 | 22.6 | 11.5 | 10.7 | 66.5 | 66.2 |
Using the ROB 2.0 tool, we assessed the risk of bias across five domains (D1: Randomization, D2: Intervention deviations, D3: Missing outcome data, D4: Outcome measurement, D5: Result selection) for three studies. Dillen et al[14] (2025) exhibited some concerns in D1 and D2, resulting in an overall rating of some concerns, despite low risk in D3, D4, and D5. Fearon et al[8] (2025) showed some concerns in D2 but achieved an overall low risk rating, with all other domains rated low. Similarly, Gioia et al[13] (2020) had some concerns in D5 but was rated low risk overall, with low risk in D1, D2, D3, and D4. In summary, Fearon et al[8] and Gioia et al[13] demonstrated robust methodological quality with low overall bias, while Dillen et al[14] raised moderate concerns due to issues in randomization and intervention adherence (Supplemen
Forest plots for all clinical outcomes are presented in Figure 2. Three studies, with baseline characteristics summarized in Table 1, reported all-cause mortality, showing no significant difference between FFR-guided percutaneous coronary intervention and CABG (pooled relative risk1.01, 95%CI: 0.78-1.31, P = 0.93), with no heterogeneity (I² = 0%). Three studies reported MACEs, indicating a significantly higher rate with FFR-guided percutaneous coronary intervention compared to CABG (pooled relative risk 1.30, 95%CI: 1.11-1.52, P = 0.001), with no heterogeneity (I² = 0%). Three studies reported myocardial infarction, demonstrating a significantly higher rate with FFR-guided PCI compared to CABG (pooled relative risk 1.49, 95%CI: 1.11-2.01, P = 0.009), with low heterogeneity (I² = 25%). Three studies reported repeat revascularization, revealing a significantly higher rate with FFR-guided PCI compared to CABG (pooled relative risk 2.25, 95%CI: 1.78-2.85, P < 0.00001), with no heterogeneity (I² = 0%). Three studies reported stroke, showing no significant difference between FFR-guided PCI and CABG (pooled relative risk 0.80, 95%CI: 0.54-1.20, P = 0.28), with no heterogeneity (I² = 0%).
Publication bias was evaluated using funnel plots for all clinical outcomes, including target lesion revascularization, major adverse cardiovascular events, stent thrombosis, all-cause mortality, cardiac mortality, and myocardial infarction. The plots displayed symmetrical distributions of effect sizes around the pooled estimates, with no notable asymmetry observed across the included studies. This symmetry suggests the absence of significant publication bias, indicating that the meta-analysis results are unlikely to be skewed by selective reporting or non-publication of smaller studies with non-significant findings (Supplementary Figure 3).
The GRADE assessment evaluated the certainty of evidence for five clinical outcomes from three RCTs comparing FFR-guided PCI with CABG. All-cause mortality and stroke showed low certainty due to serious risks of bias (one study with some concerns in randomization and intervention adherence) and imprecision (wide confidence intervals: RR = 1.01, 95%CI: 0.78-1.31 for mortality; RR = 0.80, 95%CI: 0.54-1.20 for stroke). MACE, myocardial infarction, and repeat revascularization achieved moderate certainty, downgraded only for serious risk of bias (RR = 1.30, 95%CI: 1.11-1.52; RR = 1.49, 95%CI: 1.11-2.01; RR = 2.25, 95%CI: 1.78-2.85, respectively). No heterogeneity (I² = 0%-25%) or publication bias was detected across outcomes, and indirectness was not a concern (Supplementary Table 1).
This meta-analysis of three RCTs, involving 1918 patients with multivessel CAD, compared FFR-guided PCI with CABG reveals key insights into their relative safety and efficacy. No significant differences were observed in all-cause mortality or stroke between the two strategies, indicating comparable outcomes for these critical endpoints. The primary findings indicate that both strategies yield comparable outcomes in terms of long-term survival and stroke risk, suggesting that FFR-PCI can be a viable alternative to CABG for certain patients, particularly those with less complex disease. However, CABG demonstrates a clear advantage in reducing the incidence of myocardial infarction, major adverse cardiac and cerebrovascular events (MACCE), and the need for repeat revascularization. These results underscore CABG’s superior durability in managing complex coronary disease, aligning with its ability to provide more complete revascularization compared to the targeted approach of FFR-PCI[8,9].
When examining individual outcomes, the lack of difference in all-cause mortality and stroke between FFR-PCI and CABG highlights the safety of both procedures in appropriately selected patients. This equivalence may reflect advance
Comparing these findings to prior studies, the results are consistent with landmark trials that have established CABG as the preferred strategy for complex multivessel CAD. For instance, earlier trials demonstrated higher revascularization rates with PCI compared to CABG, a trend that persists even with FFR guidance, which optimizes lesion selection[23,24]. However, unlike older studies that relied on angiography-guided PCI, this meta-analysis reflects contemporary practice by focusing on physiologically guided interventions, offering a more relevant comparison. The findings also align with studies in high-risk populations, such as diabetic patients, where CABG has consistently shown better long-term out
Several factors may explain the observed differences between FFR-PCI and CABG. FFR-guided PCI targets only ischemia-causing lesions, potentially leaving non-flow-limiting but vulnerable plaques untreated, which can progress and cause future events[27]. In contrast, CABG bypasses entire diseased segments, providing a more comprehensive solution that mitigates the risk of ischemia from both culprit and non-culprit lesions[28]. Additionally, lesion complexity, such as calcified or bifurcated plaques, poses challenges for PCI, whereas CABG overcomes these by grafting beyond the lesion[29]. Advances in surgical techniques, including the use of arterial grafts and improved perioperative care, further en
To prevent future myocardial infarction, MACCEs, and repeat revascularization, several strategies are recommended. Hybrid revascularization, combining FFR-guided PCI for non-complex lesions with CABG for complex disease, could optimize outcomes[31]. Advanced stent technologies, such as newer-generation drug-eluting stents or bioresorbable scaffolds, may reduce stent-related complications[32,33]. Optimized medical therapy, including dual antiplatelet therapy, statins, and risk factor modification (e.g., diabetes control, smoking cessation), can prevent disease progression in untreated vessels[34].
This meta-analysis has several strengths, including its exclusive use of RCTs, rigorous bias assessment using the Cochrane Risk of Bias 2 tool, and low heterogeneity across outcomes (I² = 0%-25%), which enhances the reliability of the findings. The focus on contemporary FFR-guided PCI and CABG practices ensures relevance to current clinical decision-making. However, limitations include the small number of included studies (three RCTs), which may limit the generali
In conclusion, this meta-analysis demonstrates that FFR-guided PCI and CABG yield comparable all-cause mortality and stroke rates in patients with multivessel CAD. However, CABG is superior in reducing myocardial infarction, MACCEs, and repeat revascularization, supporting its preference for complex disease, particularly in high-risk patients like those with diabetes or high SYNTAX scores. Recommended strategies to prevent future adverse events include hybrid revascularization, advanced stent technologies, optimized medical therapy, patient selection with risk stratification tools, and structured long-term follow-up. Future research should focus on large-scale trials exploring these strategies, novel stent designs, and subgroup-specific outcomes to optimize patient-centered care and inform clinical guidelines.
| 1. | Gul F, Parekh A. Multivessel Disease. 2023 Feb 8. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing, 2025. [PubMed] |
| 2. | Van den Eynde J, Bomhals K, Noé D, Jacquemyn X, McCutcheon K, Bennett J, Puskas JD, Oosterlinck W. Revascularization strategies in patients with multivessel coronary artery disease: a Bayesian network meta-analysis. Interact Cardiovasc Thorac Surg. 2022;34:947-957. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 3. | Sipahi I, Akay MH, Dagdelen S, Blitz A, Alhan C. Coronary artery bypass grafting vs percutaneous coronary intervention and long-term mortality and morbidity in multivessel disease: meta-analysis of randomized clinical trials of the arterial grafting and stenting era. JAMA Intern Med. 2014;174:223-230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 157] [Cited by in RCA: 172] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 4. | Serruys PW, Morice MC, Kappetein AP, Colombo A, Holmes DR, Mack MJ, Ståhle E, Feldman TE, van den Brand M, Bass EJ, Van Dyck N, Leadley K, Dawkins KD, Mohr FW; SYNTAX Investigators. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N Engl J Med. 2009;360:961-972. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2982] [Cited by in RCA: 3059] [Article Influence: 179.9] [Reference Citation Analysis (0)] |
| 5. | Pijls NH, De Bruyne B, Peels K, Van Der Voort PH, Bonnier HJ, Bartunek J Koolen JJ, Koolen JJ. Measurement of fractional flow reserve to assess the functional severity of coronary-artery stenoses. N Engl J Med. 1996;334:1703-1708. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1629] [Cited by in RCA: 1652] [Article Influence: 55.1] [Reference Citation Analysis (0)] |
| 6. | Tonino PA, De Bruyne B, Pijls NH, Siebert U, Ikeno F, van' t Veer M, Klauss V, Manoharan G, Engstrøm T, Oldroyd KG, Ver Lee PN, MacCarthy PA, Fearon WF; FAME Study Investigators. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention. N Engl J Med. 2009;360:213-224. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2974] [Cited by in RCA: 3160] [Article Influence: 185.9] [Reference Citation Analysis (0)] |
| 7. | De Bruyne B, Pijls NH, Kalesan B, Barbato E, Tonino PA, Piroth Z, Jagic N, Möbius-Winkler S, Rioufol G, Witt N, Kala P, MacCarthy P, Engström T, Oldroyd KG, Mavromatis K, Manoharan G, Verlee P, Frobert O, Curzen N, Johnson JB, Jüni P, Fearon WF; FAME 2 Trial Investigators. Fractional flow reserve-guided PCI versus medical therapy in stable coronary disease. N Engl J Med. 2012;367:991-1001. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1837] [Cited by in RCA: 2069] [Article Influence: 147.8] [Reference Citation Analysis (0)] |
| 8. | Fearon WF, Zimmermann FM, Ding VY, Takahashi K, Piroth Z, van Straten AHM, Szekely L, Davidavičius G, Kalinauskas G, Mansour S, Kharbanda R, Östlund-Papadogeorgos N, Aminian A, Oldroyd KG, Al-Attar N, Jagic N, Dambrink JE, Kala P, Angerås O, MacCarthy P, Wendler O, Casselman F, Witt N, Mavromatis K, Miner SES, Sarma J, Engstrøm T, Christiansen EH, Tonino PAL, Reardon MJ, Otsuki H, Kobayashi Y, Hlatky MA, Mahaffey KW, Desai M, Woo YJ, Yeung AC, Pijls NHJ, De Bruyne B. Outcomes after fractional flow reserve-guided percutaneous coronary intervention versus coronary artery bypass grafting (FAME 3): 5-year follow-up of a multicentre, open-label, randomised trial. Lancet. 2025;405:1481-1490. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 19] [Article Influence: 19.0] [Reference Citation Analysis (0)] |
| 9. | Mohr FW, Morice MC, Kappetein AP, Feldman TE, Ståhle E, Colombo A, Mack MJ, Holmes DR Jr, Morel MA, Van Dyck N, Houle VM, Dawkins KD, Serruys PW. Coronary artery bypass graft surgery versus percutaneous coronary intervention in patients with three-vessel disease and left main coronary disease: 5-year follow-up of the randomised, clinical SYNTAX trial. Lancet. 2013;381:629-638. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1214] [Cited by in RCA: 1264] [Article Influence: 97.2] [Reference Citation Analysis (0)] |
| 10. | Head SJ, Davierwala PM, Serruys PW, Redwood SR, Colombo A, Mack MJ, Morice MC, Holmes DR Jr, Feldman TE, Ståhle E, Underwood P, Dawkins KD, Kappetein AP, Mohr FW. Coronary artery bypass grafting vs. percutaneous coronary intervention for patients with three-vessel disease: final five-year follow-up of the SYNTAX trial. Eur Heart J. 2014;35:2821-2830. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 235] [Cited by in RCA: 246] [Article Influence: 20.5] [Reference Citation Analysis (0)] |
| 11. | Takahashi K, Otsuki H, Zimmermann FM, Ding VY, Engstrøm T, Hørsted Thyregod HG, Beleslin B, Putnik S, Tapp L, Barker T, Redwood S, Young C, Bech GJ, Hoohenkerk GJF, De Bruyne B, Pijls NHJ, Fearon WF; FAME 3 Trial Investigators. FFR-Guided Percutaneous Coronary Intervention vs Coronary Artery Bypass Grafting in Patients With Diabetes. JAMA Cardiol. 2025;10:603-608. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 12. | Fearon WF, Zimmermann FM, De Bruyne B, Piroth Z, van Straten AHM, Szekely L, Davidavičius G, Kalinauskas G, Mansour S, Kharbanda R, Östlund-Papadogeorgos N, Aminian A, Oldroyd KG, Al-Attar N, Jagic N, Dambrink JE, Kala P, Angerås O, MacCarthy P, Wendler O, Casselman F, Witt N, Mavromatis K, Miner SES, Sarma J, Engstrøm T, Christiansen EH, Tonino PAL, Reardon MJ, Lu D, Ding VY, Kobayashi Y, Hlatky MA, Mahaffey KW, Desai M, Woo YJ, Yeung AC, Pijls NHJ; FAME 3 Investigators. Fractional Flow Reserve-Guided PCI as Compared with Coronary Bypass Surgery. N Engl J Med. 2022;386:128-137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 253] [Article Influence: 63.3] [Reference Citation Analysis (0)] |
| 13. | Di Gioia G, Soto Flores N, Franco D, Colaiori I, Sonck J, Gigante C, Kodeboina M, Bartunek J, Vanderheyden M, Van Praet F, Casselman F, Degriek I, Stockman B, Barbato E, Collet C, De Bruyne B. Coronary Artery Bypass Grafting or Fractional Flow Reserve-Guided Percutaneous Coronary Intervention in Diabetic Patients With Multivessel Disease. Circ Cardiovasc Interv. 2020;13:e009157. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 14. | Dillen DMM, Otsuki H, Takahashi K, Kobayashi Y, Piroth Z, Noiseux N, Nakadi BE, Kalinauskas G, Szekely L, Davidavičius G, Teeuwen K, Tonino PAL, Pijls NHJ, De Bruyne B, Fearon WF, Zimmermann FM. Impact of Bifurcation Lesions on Outcomes After FFR-Guided PCI or CABG. Circ Cardiovasc Interv. 2025;18:e014610. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 15. | Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8:336-341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9207] [Cited by in RCA: 8355] [Article Influence: 522.2] [Reference Citation Analysis (2)] |
| 16. | Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44932] [Cited by in RCA: 51475] [Article Influence: 10295.0] [Reference Citation Analysis (2)] |
| 17. | Cochrane Methods Bias. RoB 2: A revised Cochrane risk-of-bias tool for randomized trials. [cited 10 June 2025]. Available from: https://methods.cochrane.org/bias/resources/rob-2-revised-cochrane-risk-bias-tool-randomized-trials. |
| 18. | Farkouh ME, Domanski M, Sleeper LA, Siami FS, Dangas G, Mack M, Yang M, Cohen DJ, Rosenberg Y, Solomon SD, Desai AS, Gersh BJ, Magnuson EA, Lansky A, Boineau R, Weinberger J, Ramanathan K, Sousa JE, Rankin J, Bhargava B, Buse J, Hueb W, Smith CR, Muratov V, Bansilal S, King S 3rd, Bertrand M, Fuster V; FREEDOM Trial Investigators. Strategies for multivessel revascularization in patients with diabetes. N Engl J Med. 2012;367:2375-2384. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1325] [Cited by in RCA: 1387] [Article Influence: 99.1] [Reference Citation Analysis (0)] |
| 19. | Serruys PW, Kogame N, Katagiri Y, Modolo R, Buszman PE, Íñiguez-Romo A, Goicolea J, Hildick-Smith D, Ochala A, Dudek D, Piek JJ, Wykrzykowska JJ, Escaned J, Banning AP, Farooq V, Onuma Y. Clinical outcomes of state-of-the-art percutaneous coronary revascularisation in patients with three-vessel disease: two-year follow-up of the SYNTAX II study. EuroIntervention. 2019;15:e244-e252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 48] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 20. | Gaudino MFL, An KR, Calhoon J. Mechanisms for the Superiority of Coronary Artery Bypass Grafting in Complex Coronary Artery Disease. Ann Thorac Surg. 2023;115:1333-1336. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 21. | Ren J, Siderakis C, Royse C, Hwang B, Royse A. Is total arterial coronary artery bypass grafting the next step forward? Vessel Plus. 2024;8:40. [DOI] [Full Text] |
| 22. | Koo BK, Hu X, Kang J, Zhang J, Jiang J, Hahn JY, Nam CW, Doh JH, Lee BK, Kim W, Huang J, Jiang F, Zhou H, Chen P, Tang L, Jiang W, Chen X, He W, Ahn SG, Yoon MH, Kim U, Lee JM, Hwang D, Ki YJ, Shin ES, Kim HS, Tahk SJ, Wang J; FLAVOUR Investigators. Fractional Flow Reserve or Intravascular Ultrasonography to Guide PCI. N Engl J Med. 2022;387:779-789. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 105] [Article Influence: 26.3] [Reference Citation Analysis (0)] |
| 23. | Sakata K, Nakahashi T, Kawashiri MA. Prognostic superiority of coronary artery bypass grafting to percutaneous coronary intervention in non-diabetic patients with anatomically complex multivessel coronary artery disease. Cardiovasc Diagn Ther. 2017;7:S77-S81. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 24. | Park SJ, Ahn JM, Kim YH, Park DW, Yun SC, Lee JY, Kang SJ, Lee SW, Lee CW, Park SW, Choo SJ, Chung CH, Lee JW, Cohen DJ, Yeung AC, Hur SH, Seung KB, Ahn TH, Kwon HM, Lim DS, Rha SW, Jeong MH, Lee BK, Tresukosol D, Fu GS, Ong TK; BEST Trial Investigators. Trial of everolimus-eluting stents or bypass surgery for coronary disease. N Engl J Med. 2015;372:1204-1212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 320] [Cited by in RCA: 392] [Article Influence: 35.6] [Reference Citation Analysis (0)] |
| 25. | Xie Q, Huang J, Zhu K, Chen Q. Percutaneous coronary intervention versus coronary artery bypass grafting in patients with coronary heart disease and type 2 diabetes mellitus: Cumulative meta-analysis. Clin Cardiol. 2021;44:899-906. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 22] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 26. | Khan A, Ishfaq L, Wolbert P, Darapaneni H, Khetarpal V, Sahu S, Farooq W. C-70 | Comparative Outcomes of Left Main PCI vs. CABG: A Meta-Analysis of Mortality, Revascularization, and Quality of Life. J Soc Cardiovasc Angiogr Interv. 2025;4:103060. [DOI] [Full Text] |
| 27. | Shah T, Geleris JD, Zhong M, Swaminathan RV, Kim LK, Feldman DN. Fractional flow reserve to guide surgical coronary revascularization. J Thorac Dis. 2017;9:S317-S326. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 28. | Bhat S, Yatsynovich Y, Sharma UC. Coronary revascularization in patients with stable coronary disease and diabetes mellitus. Diab Vasc Dis Res. 2021;18:14791641211002469. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 29. | Kang SJ, Lee CW, Song H, Ahn JM, Kim WJ, Lee JY, Park DW, Lee SW, Kim YH, Mintz GS, Park SW, Park SJ. OCT analysis in patients with very late stent thrombosis. JACC Cardiovasc Imaging. 2013;6:695-703. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 74] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 30. | Stefanini GG, Holmes DR Jr. Drug-eluting coronary-artery stents. N Engl J Med. 2013;368:254-265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 512] [Cited by in RCA: 561] [Article Influence: 43.2] [Reference Citation Analysis (0)] |
| 31. | Xaplanteris P, Fournier S, Pijls NHJ, Fearon WF, Barbato E, Tonino PAL, Engstrøm T, Kääb S, Dambrink JH, Rioufol G, Toth GG, Piroth Z, Witt N, Fröbert O, Kala P, Linke A, Jagic N, Mates M, Mavromatis K, Samady H, Irimpen A, Oldroyd K, Campo G, Rothenbühler M, Jüni P, De Bruyne B; FAME 2 Investigators. Five-Year Outcomes with PCI Guided by Fractional Flow Reserve. N Engl J Med. 2018;379:250-259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 492] [Cited by in RCA: 689] [Article Influence: 86.1] [Reference Citation Analysis (0)] |
| 32. | Alfonso F, Byrne RA, Rivero F, Kastrati A. Current treatment of in-stent restenosis. J Am Coll Cardiol. 2014;63:2659-2673. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 343] [Cited by in RCA: 437] [Article Influence: 36.4] [Reference Citation Analysis (0)] |
| 33. | Farooq V, Serruys PW, Bourantas CV, Zhang Y, Muramatsu T, Feldman T, Holmes DR, Mack M, Morice MC, Ståhle E, Colombo A, de Vries T, Morel MA, Dawkins KD, Kappetein AP, Mohr FW. Quantification of incomplete revascularization and its association with five-year mortality in the synergy between percutaneous coronary intervention with taxus and cardiac surgery (SYNTAX) trial validation of the residual SYNTAX score. Circulation. 2013;128:141-151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 324] [Cited by in RCA: 316] [Article Influence: 24.3] [Reference Citation Analysis (0)] |
| 34. | Gunn J, Taggart DP. Revascularisation for acute coronary syndromes: PCI or CABG? Heart. 2003;89:967-970. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/