Published online Jan 26, 2025. doi: 10.4330/wjc.v17.i1.97406
Revised: September 20, 2024
Accepted: November 27, 2024
Published online: January 26, 2025
Processing time: 236 Days and 18 Hours
Listening to music has been shown to reduce pain and anxiety before, during, and after invasive coronary procedures.
To perform a systematic review and meta-analysis to explore the effect of thera
An exhaustive literature search of 3 electronic databases (MEDLINE, Scopus, Cochrane CENTRAL) was conducted from inception until 10th December 2023. The results of our analyses are presented as standard mean difference (SMD) or weighted mean difference, with 95%CI and pooled using a random effects model. A P value < 0.05 was considered significant in all cases.
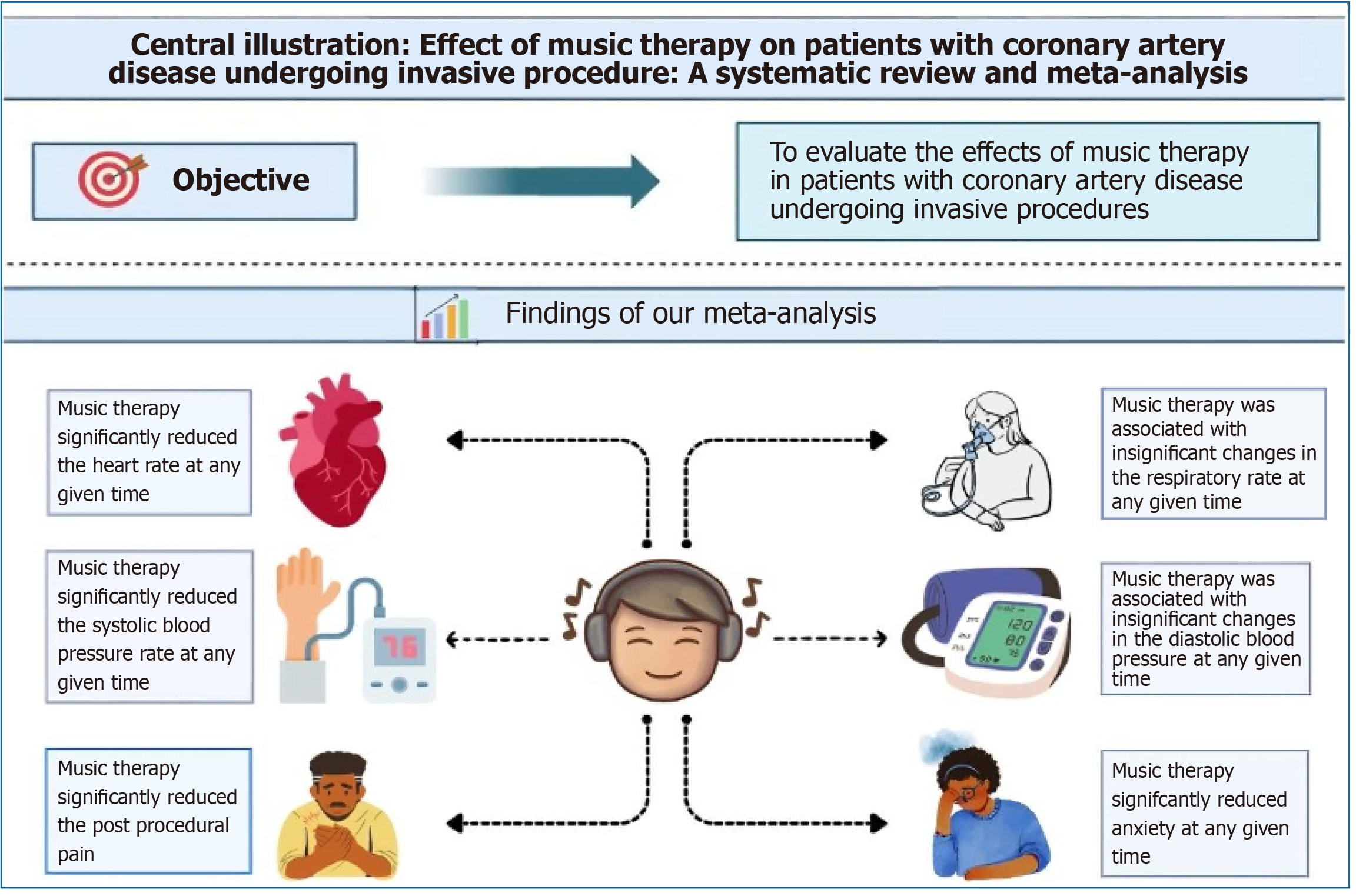
From 21 studies, 2141 participants were included in our analysis. The pooled analysis demonstrated that music listening significantly improves post-procedural pain (SMD = -0.78, 95%CI: -1.34 to -0.23; P = 0.006), anxiety (SMD = -0.86, 95%CI: -1.43 to -0.29; P = 0.003), heart rate [mean difference (MD) = -3.38, 95%CI: -5.51 to -1.25; P = 0.002], and systolic blood pressure (MD = -5.89, 95%CI: -9.75 to -2.02; P = 0.003). There was no significant improvement in diastolic blood pressure (MD = -3.22, 95%CI: -6.58 to 0.14; P = 0.06) or respiratory rate (MD = -0.97, 95%CI: -1.98 to 0.03; P = 0.06).
Music listening can be used in healthcare settings for patients undergoing invasive coronary procedures to reduce anxiety levels and improve their physiological parameters.
Core Tip: This meta-analysis evaluated the therapeutic effects of music listening on patients undergoing invasive coronary procedures such as percutaneous coronary intervention and coronary artery bypass grafting. The study demonstrated that music therapy significantly reduces post-procedural anxiety, heart rate, systolic blood pressure and pain levels. These findings highlight the potential use of music as a non-pharmacological intervention to improve patient outcomes and well-being in healthcare settings, making it a valuable complementary treatment for managing the psychological and physiological stress associated with invasive cardiac procedures.
- Citation: Siddiqi AK, Shafiq A, Ahmed M, Anwer A, Maniya MT, Ahmed A, Chachar MA, Hasibuzzaman MA. Therapeutic use of music listening in patients undergoing invasive coronary procedures: A meta-analysis. World J Cardiol 2025; 17(1): 97406
- URL: https://www.wjgnet.com/1949-8462/full/v17/i1/97406.htm
- DOI: https://dx.doi.org/10.4330/wjc.v17.i1.97406
The leading cause of mortality is coronary heart disease (CHD), accounting for approximately 9.5 million deaths globally[1]. Coronary procedures are an effective treatment for CHD as they facilitate the removal of blood clots, which increases myocardial blood flow[2]. However, invasive procedures such as angiography and percutaneous coronary intervention (PCI) result in serious anxiety, panic, and mental stress[3,4]. The physiological response of the body to stress is anxiety, which is characterized by elevated levels of serum adrenaline, heart rate (HR), respiratory rate (RR), blood pressure (BP), and decreased pain threshold[5]. Elevated HR and BP during invasive cardiovascular procedures enhance the cardiac strain and treatment risk[6,7]. In order to mitigate anxiety and pain both before and after such invasive procedures, several strategies have been devised. Among these is a non-pharmacological technique such as music listening[3,8].
For thousands of years, people have recognized the therapeutic effects of music[9]. However, how music impacts the human body is not entirely understood. The majority of theories postulate that music affects the autonomic and central nervous systems at subcortical levels in addition to being perceived consciously and that the limbic system is essential for processing musical aspects[10]. In addition to assessing the levels of stress and anxiety during cardiac procedures, several studies have examined the impact of music listening on cardiovascular outcomes such as BP and HR. Although these outcomes were previously investigated in a previous meta-analysis[11], it included only 10 studies and concluded its search in 2019. Given the recent expansion of literature in this area, an update to these results was long overdue. There
This systematic review and meta-analysis followed the recommended reporting format specified in the Preferred Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines[12]. Permission from the Institutional Review Board was not required as data used in this study were publicly available.
An electronic search of the MEDLINE, Scopus, and Cochrane CENTRAL databases was carried out from inception until 10th December 2023. The search string used consisted of the following keywords and related Medical Subject Headings terms: ((((((music therapy) AND (coronary procedures)) OR (percutaneous coronary intervention)) OR (PCI)) OR (coronary artery bypass grafting)) OR (CABG)) OR (cardiac catheterization). The retrieved studies that met the eligibility criteria were included in this meta-analysis. No language limitations were imposed while searching the literature. Further studies were found by manually searching references in past meta-analyses, reviews, and published articles. Two researchers (Shafiq A and Ahmed M) carried out the literature search, study selection, and data extraction independently. In the event of any disagreements, a third reviewer (Shafiq A) was consulted. It is important to note that the studies included in this review utilize music listening, which involves the provision of pre-recorded music for patients. This is distinct from music therapy, a structured intervention led by credentialed music therapists, which involves individualized, therapeutic use of music tailored to the patient's needs. The studies included in this review focus on music listening, facilitated by healthcare providers or self-administered by patients.
The eligibility requirements were as follows: (1) Published clinical trials, both randomized and non-randomized; (2) Participants who were at least eighteen years old with an indication for PCI, coronary angiography, coronary artery bypass grafting (CABG) or vascular angiography; (3) Details of the music intervention that was used; and (4) Outcomes measured included anxiety, pain, HR, systolic BP (SBP), diastolic BP (DBP) and RR. Literature reviews, case reports, case series, animal studies, interventional trials without music listening, and studies with fewer than five patients were exclu
Articles yielded through a search of the databases were exported to EndNote where they were checked for duplicates. Following the elimination of duplicates, papers were individually evaluated and screened based on title and abstract. Using the previously mentioned eligibility criteria, the remaining studies were further shortlisted. The quality of the non-randomized studies used in this meta-analysis was assessed using the Cochrane Risk of Bias in Non-randomized Studies-of Interventions (ROBINS-I) tool[13]. The ROBINS-I tool uses seven domains to determine overall bias in each non-randomized clinical trial. Studies were classified as having low, moderate, serious, or critical risk of bias. Trials that had information missing in one or more domains were classified as no information. All randomized controlled trials were assessed for risk of bias using the Cochrane Risk of Bias 2 tool. Five domains were used to evaluate the studies: (1) Randomization; (2) Deviation from intended interventions; (3) Missing outcome data; (4) Outcome measurement; and (5) Selection of reported results. Based on the Risk of Bias tool, each randomized controlled trial (RCT) was classified as having a high risk of bias, some concerns, or a low risk of bias.
All statistical analyses were conducted using RevMan (version 5.4.1; Copenhagen: The Nordic Cochrane Collaboration, 2014). The random effects model was used to pool the data for the following outcomes: (1) Anxiety; (2) Pain; (3) RR; (4) SBP; (5) DBP; and (6) HR. Except for pain and anxiety, which are reported as standard mean difference (SMD), all outcomes are presented as weighted mean difference with 95%CI. In each case, results were deemed statistically significant if the P value was less than or equal to 0.05. The Higgins I2 test was used to investigate heterogeneity. It was determined that an I2 value of 25%–50% was mild, 50%–75% was moderate, and > 75% was severe. Analysis was conducted based on outcome measurements reported in each study at any time, before the procedure, during the procedure, and after the procedure across the control and intervention groups.
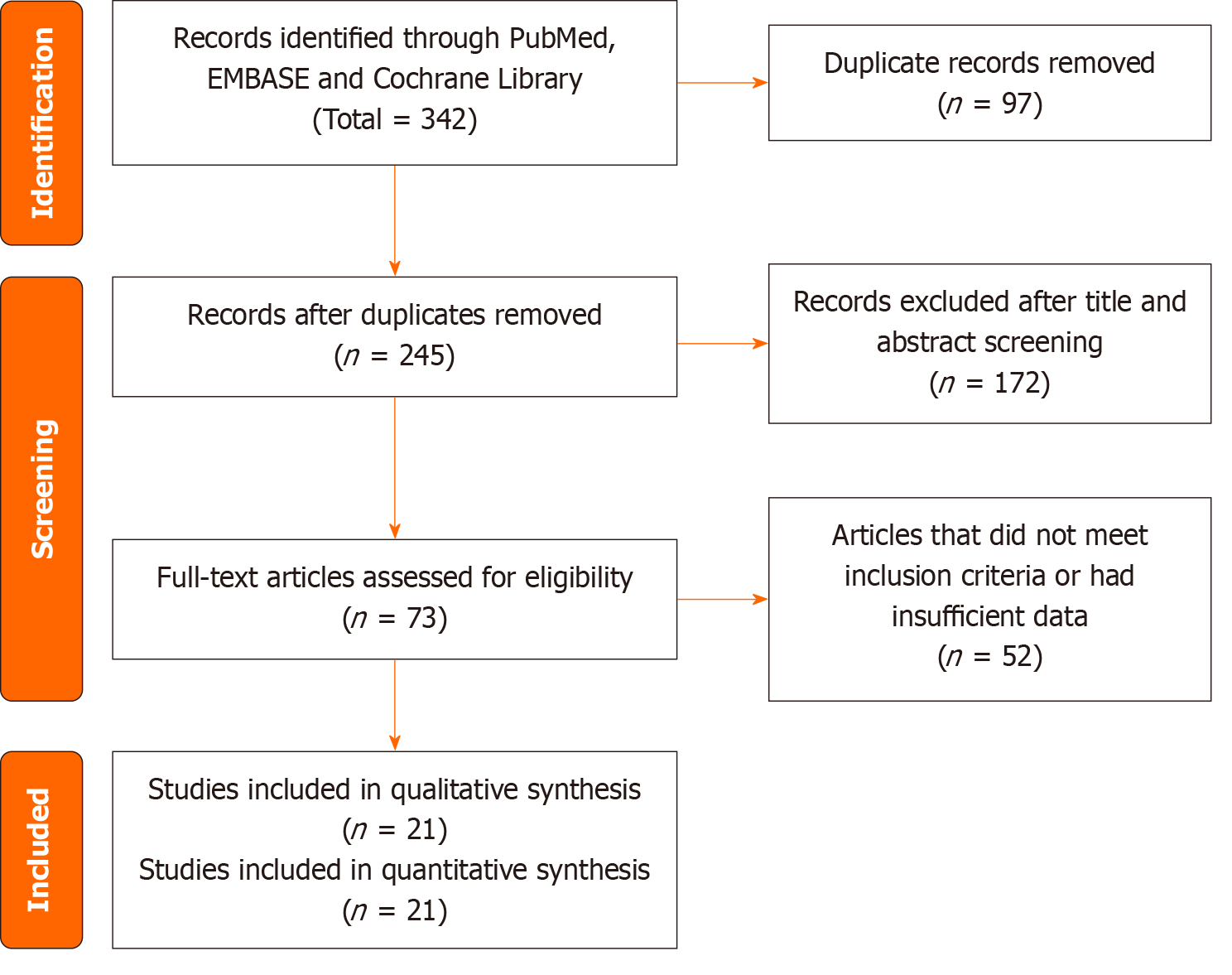
We performed a comprehensive literature search using PubMed/MEDLINE, EMBASE, and the Cochrane Library. The initial search yielded 342 records. The duplicate studies were removed, and articles were screened based on the study title and abstract. The full text of 73 studies was reviewed and a total of 21 studies were considered eligible for inclusion in our meta-analysis. The details of the literature search and study selection process are shown in the PRISMA flowchart of Figure 1.
A total of 21 studies[3,8,14-32] were included in our pooled analysis. The included studies were published from 1995 to 2023. There was variability in the study design of pooled articles that included 11 RCTs and 10 non-randomized studies. A total of 2141 patients were included in our pooled analysis. The mean age of patients ranged from 18 years to 74 years. Seven studies were conducted in the United States[18-21,27,28,32], 5 in Iran[3,8,14,26,31], 2 in Turkey[16,17], 2 in China[15,30], 2 in Sweden[24,25], 2 in Hong Kong[22,29] and 1 in Germany[23]. The detailed baseline characteristics of the included studies are provided in Table 1[3,8,14-32].
| Ref. | Country | Year | N | Sex (male/female) | Age (intervention/control) | Type of study | Type of music | Tempo (beats/minute) | Lyrics | Duration (minute) | Time of intervention | Mode of delivery | Outcome |
| Moradipanah et al[14] | Iran | 2009 | 74 | 37/37 | Mean = 50.6 | RCT | Slow and steady rhythms | 60-80 | No | 20 | Before angiography | Earphones plugged to a cassette | Anxiety (DASS-21 score) |
| Dong et al[15] | China | 2023 | 86 | 50/36 | Mean = 57.6/54.8 | RCT | Low-key music | 60-80 | - | 15 | 2 hours after extubation | Binaural headphones | Pain (VAS), anxiety (STAI), HR, SBP, DBP, RR |
| Oyur Çelik et al[16] | Turkey | 2022 | 62 | 31/31 | Mean = 58.58/56.81 | RCT | Instrumentaland Nihavend mode | - | No | 45 | Before coronary angiography | Music CD | Pain (VAS), anxiety (STAI), HR, SBP, DBP, RR |
| Doğan and Şenturan[17] | Turkey | 2012 | 200 | 140/60 | Range = 18-66 | Pretest/posttest control group | Calming and relaxing and Huseyni mode | - | No | - | During coronary angiography | CD player | Anxiety (STAI score) |
| Forooghy et al[8] | Iran | 2015 | 64 | 41/23 | Range = 45-82 | RCT | Light instrumental by Bach | - | No | 20-40 | Before coronary angioplasty | MP3 player and headphones | Anxiety (STAI), SBP, DBP, RR, HR |
| Zimmerman et al[18] | United States | 1996 | 96 | 64/30 | Mean = 67 | Repeated measures experiment | Participant's choice | - | No | 30 | Post CABG | Headphones | Pain (VRS, McGill pain questionnaire score) |
| Bally et al[19] | United States | 2003 | 107 | 64/49 | Mean = 59/58 | Pretest-posttest control group | Self-selected by patient | - | - | - | Before, during or after coronary angiography | Headphones and cassette recorder | Anxiety (STAI), pain (VAS), HR, SBP, DBP |
| Rejeh et al[3] | Iran | 2016 | 130 | 64/66 | Mean = 61.68 | Quasi-randomized controlled trial | Pleasant natural sounds | - | - | - | 30 minutes before coronary angiography | MP3 player and foam-lined headphones | Anxiety (STAI), SBP, DBP, RR, HR |
| Hamel et al[20] | United States | 2001 | 101 | 63/38 | Range = 43-74 | Quasi-experimental | ÄòTrance‚ ÄìZendance‚Äô by Halpern | 70-80 | No | 20 | Prior to cardiac catheterization | Portable CD player | Anxiety (STAI), HR, BP |
| Cadiganv et al[21] | United States | 2001 | 140 | 100/40 | Mean = 62.2 | RCT | Mixture of symphonic music and nature sounds | - | No | 30 | Post PCI or on bedrest | CD player and headphones | Pain (VAS), SBP, DBP, HR, RR |
| Taylor-Piliae et al[22] | Hong Kong (China) | 2002 | 45 | 23/7 | Mean = 58.2 | Experimental three-group | New age and Chinese instrumental or classical | - | No | -5 | 1 hour prior to catheterization | Cassette recorder and headphones | Anxiety (SAI), HR, RR |
| Argstatter et al[23] | Germany | 2006 | 90 | 31/24 | Mean = 66.5 | Pretest-posttest, three-armed | ÄúRelaxation‚ Äù by Martin Rumme | - | - | - | During cardiac catheterization | Earphones | Anxiety (STAI), HR, SBP, DBP |
| Nilsson[25] | Sweden | 2012 | 68 | 0/68 | Mean = 67/65 | RCT | Soft and relaxing musicure | 60-80 | No | - | During coronary angiography and/or PCI | Maysound music player | Anxiety (NRS) |
| Nilsson[24] | Sweden | 2009 | 238 | 119/119 | Mean = 67/64 | RCT | Soft and relaxing musicure | 60-80 | No | - | During coronary angiography and/or PCI | Maysound music player | Anxiety (STAI, NRS), pain (VAS) |
| Amiri et al[26] | Iran | 2017 | 90 | 56/34 | Mean = 58.61 | RCT | ÄúSounds of Nature and Äù by Stein A | - | No | 30 | Before CABG | Sony MP3 player | Anxiety (STAI) |
| Barnason et al[27] | United States | 1995 | 96 | 65/31 | Mean = 67 | Repeated measures and quasi-experimental | Participant's choice | - | No | 30 | Post-operative day 2 and 3 after CABG | Headphones | Anxiety (NRS, STAI), SBP, DBP, HR |
| Buffum et al[28] | United States | 2006 | 170 | 166/4 | Mean = 67.01/66.65 | Quasi-experimental | Classical, jazz, rock, country western, and easy listening | - | - | 15 | Before vascular angiography | Boombox style CD player without headphones | Anxiety (STAI), SBP, DBP, RR, HR |
| Chan[29] | Hong Kong (China) | 2006 | 43 | 31/12 | Range = 35-75 | RCT | Soft and slow music | - | No | 45 | During C-clamp procedure | MP3 player with headphones | Pain (University of California Los Angeles), SBP, DBP, HR, RR |
| Dai et al[30] | China | 2020 | 99 | 37/29 | Mean = 53.4/53.1 | Retrospective study | Light and relaxing | - | - | 30 | After coronary bypass | Binaural headphones | Pain (NRS), anxiety (SAS) |
| Heidari et al[31] | Iran | 2015 | 60 | 33/27 | Mean = 56.33/60.91 | RCT | Sounds of nature | - | - | 30 | Before CABG | Digital MP3 player with headphones | Anxiety (VAS-A), HR, SBP, DBP |
| Twiss et al[32] | United States | 2006 | 86 | 28/58 | Mean = 72.6/75.1 | RCT | Choice between six relaxing CDs | - | - | - | Throughout CABG procedure and post-op | Headphones | Anxiety (STAI) |
The quality assessment of included RCTs was performed using the Cochrane risk of bias tool and ROBINS-I was used for non-randomized studies. The details of bias assessment for each included study are provided in Supplementary Table 1[8,14-16,21,24-26,29,31,32] and Supplementary Table 2[3,15,18-20,22,23,27,28,30].
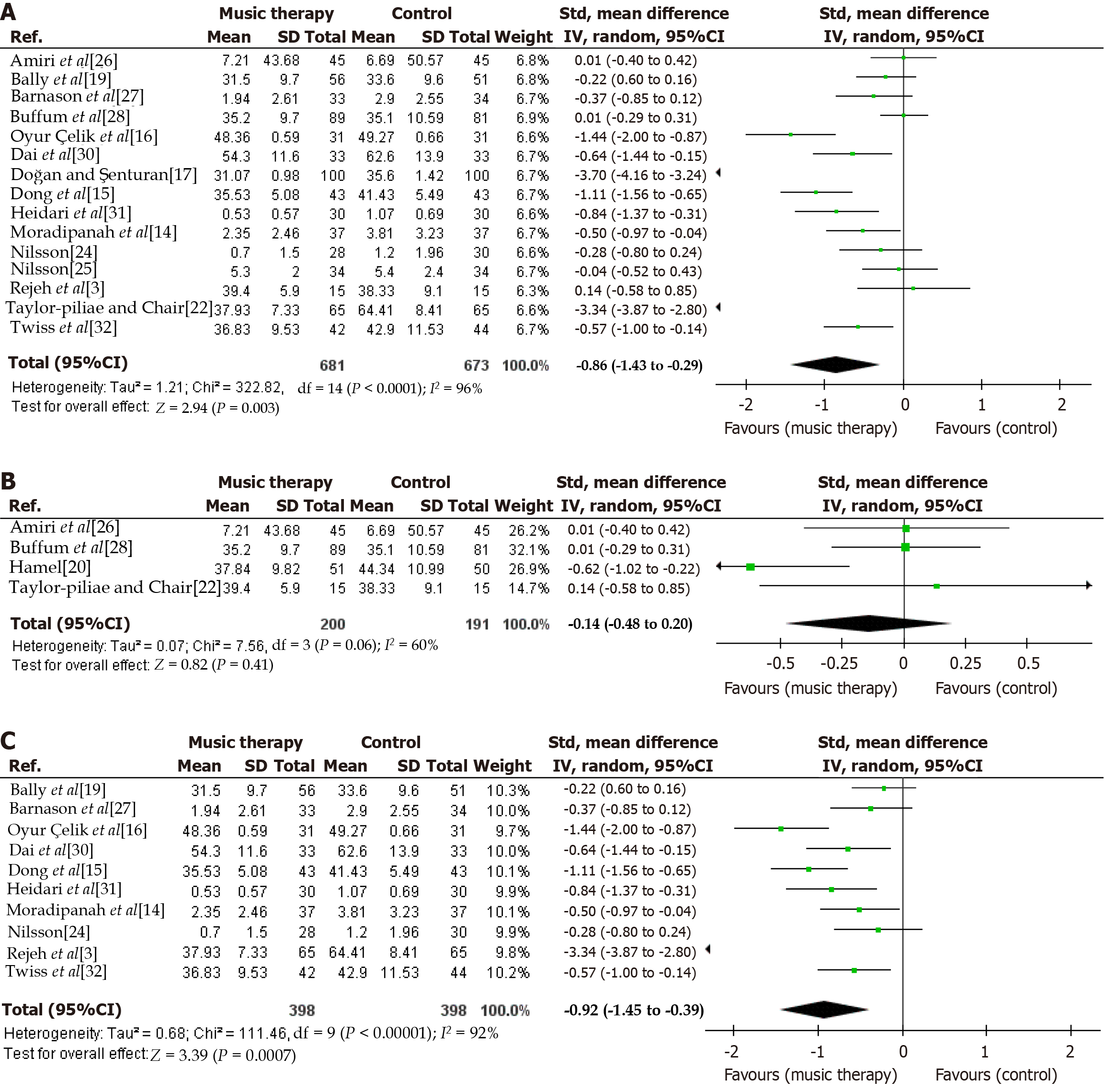
Anxiety: Data for anxiety at any time was reported by 15 studies. Our pooled analysis showed that anxiety at any time was significantly reduced in the music listening group (SMD = -0.86, 95%CI: -1.43 to -0.29; P = 0.003) (Figure 2A). High heterogeneity was observed (I2 = 96%). No significant difference was observed between the music listening and the control group for pre-procedural anxiety (SMD = -0.14, 95%CI: -0.48 to 0.20; P = 0.41, I2 = 60%) (Figure 2B). Music listening was associated with significantly reduced post-procedural anxiety (SMD = -0.92, 95%CI: -1.45 to -0.39; P = 0.0007, I2 = 92%) (Figure 2C)[3,14-17,19,20,22,24-28,30-32].
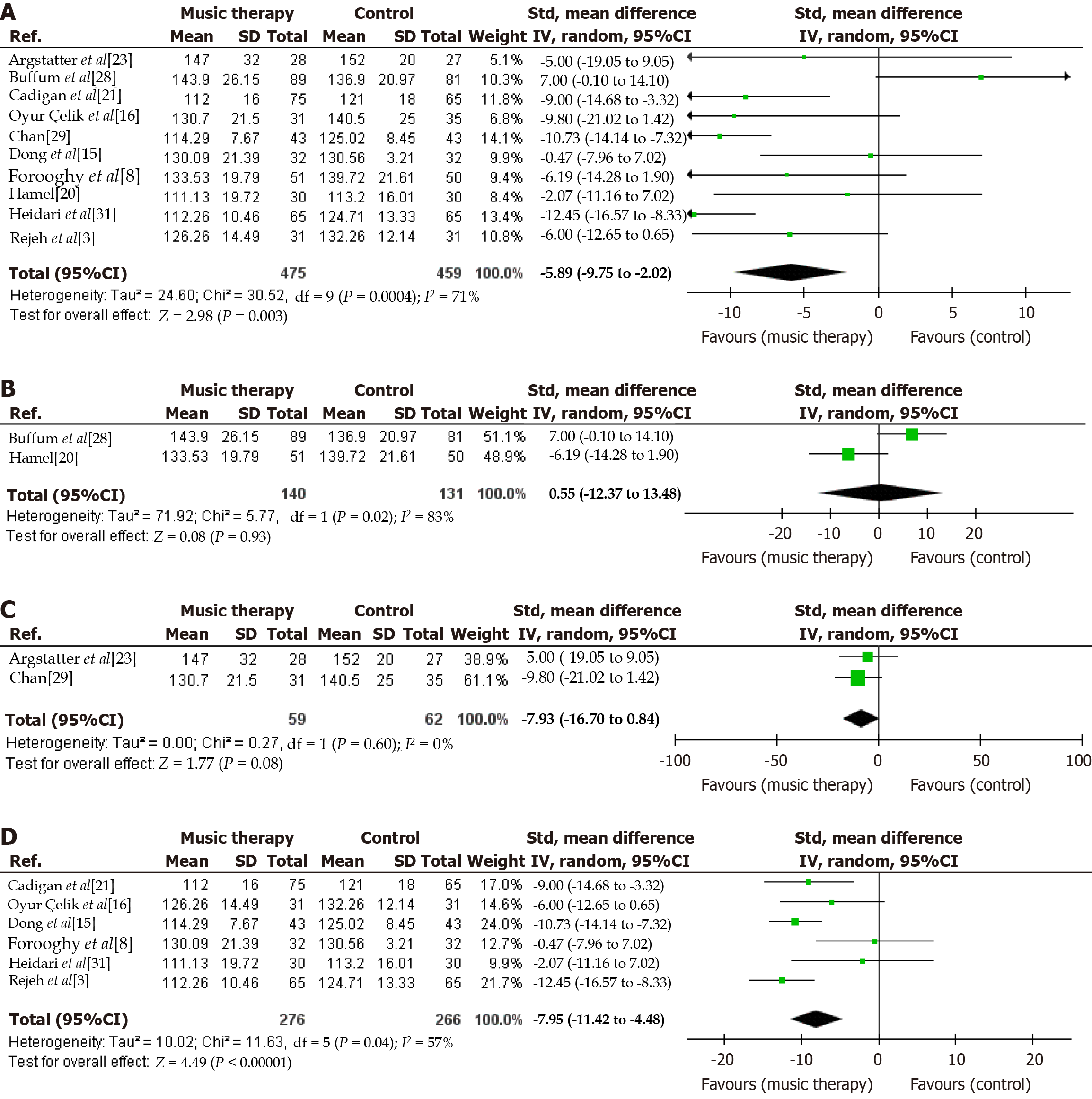
SBP: Ten studies provided data for SBP at any time. Our pooled analysis demonstrated that SBP at any time was signi
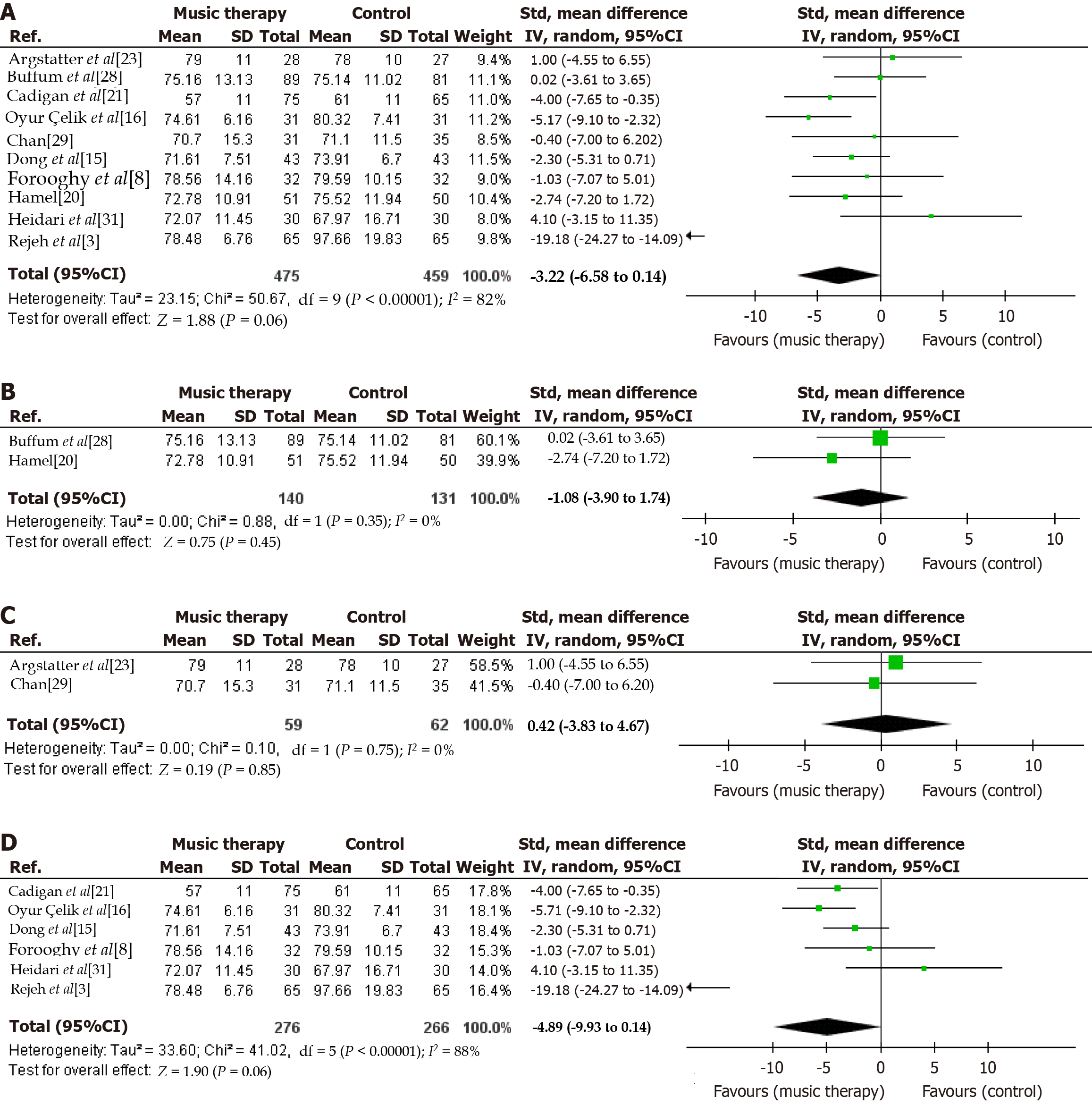
DBP: Data for DBP at any time was reported by 10 studies. There was no significant difference between the music listening and the control group for DBP at any time (MD = -3.22, 95%CI: -6.58 to 0.14; P = 0.06) (Figure 4A). High heterogeneity was observed (I2 = 82%). No significant difference was observed for pre-procedural DBP (MD = -1.08, 95%CI:
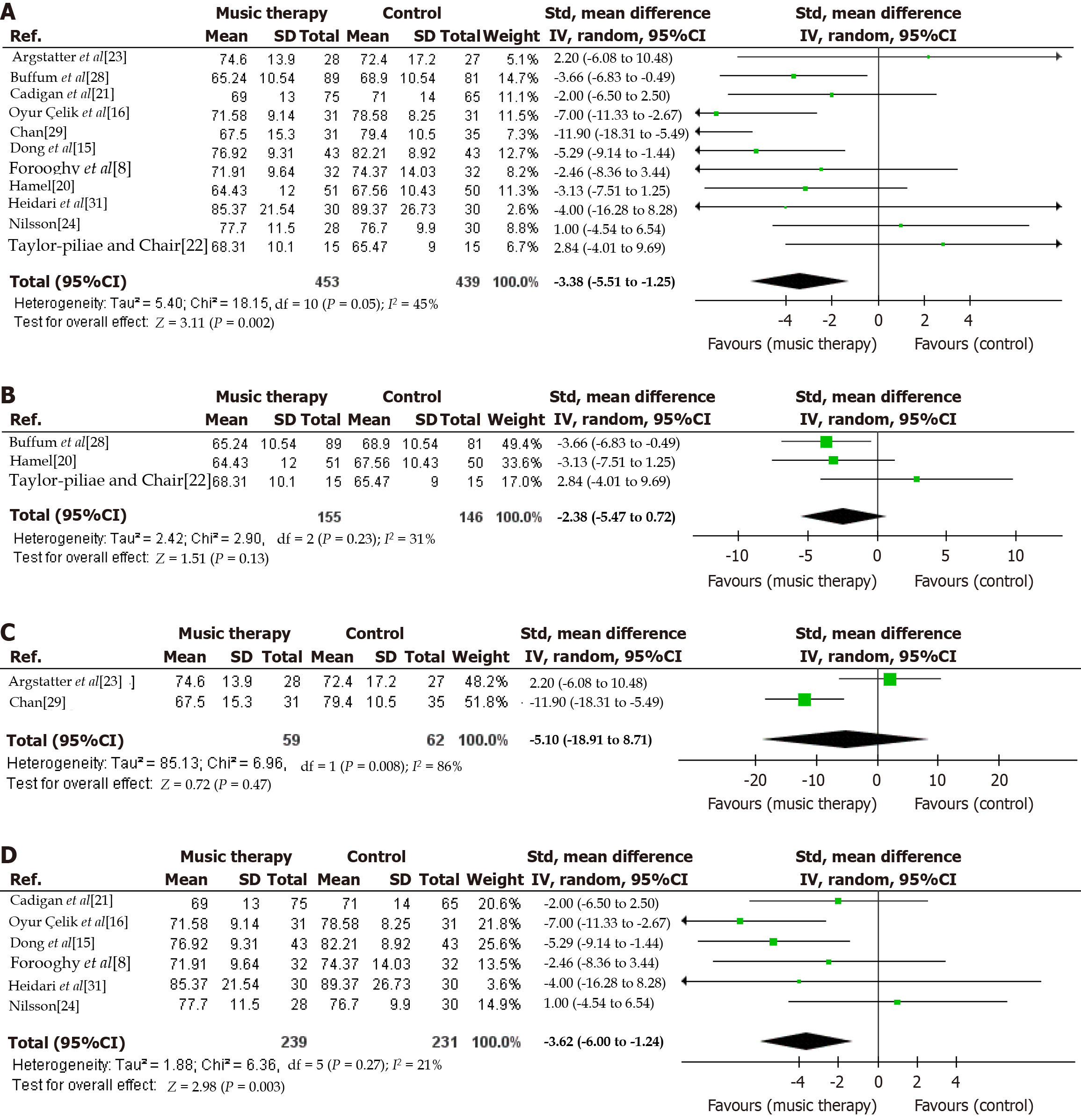
HR: Data for HR at any time was reported by 11 studies. HR at any time was significantly reduced in the music listening group (MD = -3.38, 95%CI: -5.51 to -1.25; P = 0.002) (Figure 5A). Moderate heterogeneity was observed (I2 = 45%). The pooled analysis showed no significant difference for pre-procedural HR (MD = -2.38, 95%CI: -5.47 to 0.72; P = 0.13, I2 = 31%) (Figure 5B) and procedural HR (MD = -5.10, 95%CI: -18.91 to 8.71; P = 0.47, I2 = 86%) (Figure 5C). Post-procedural HR was significantly reduced in patients who were in the music listening group (MD = -3.62, 95%CI: -6.00 to -1.24; P = 0.003, I2 = 21%) (Figure 5D)[8,15,16,20-24,28,29,31].
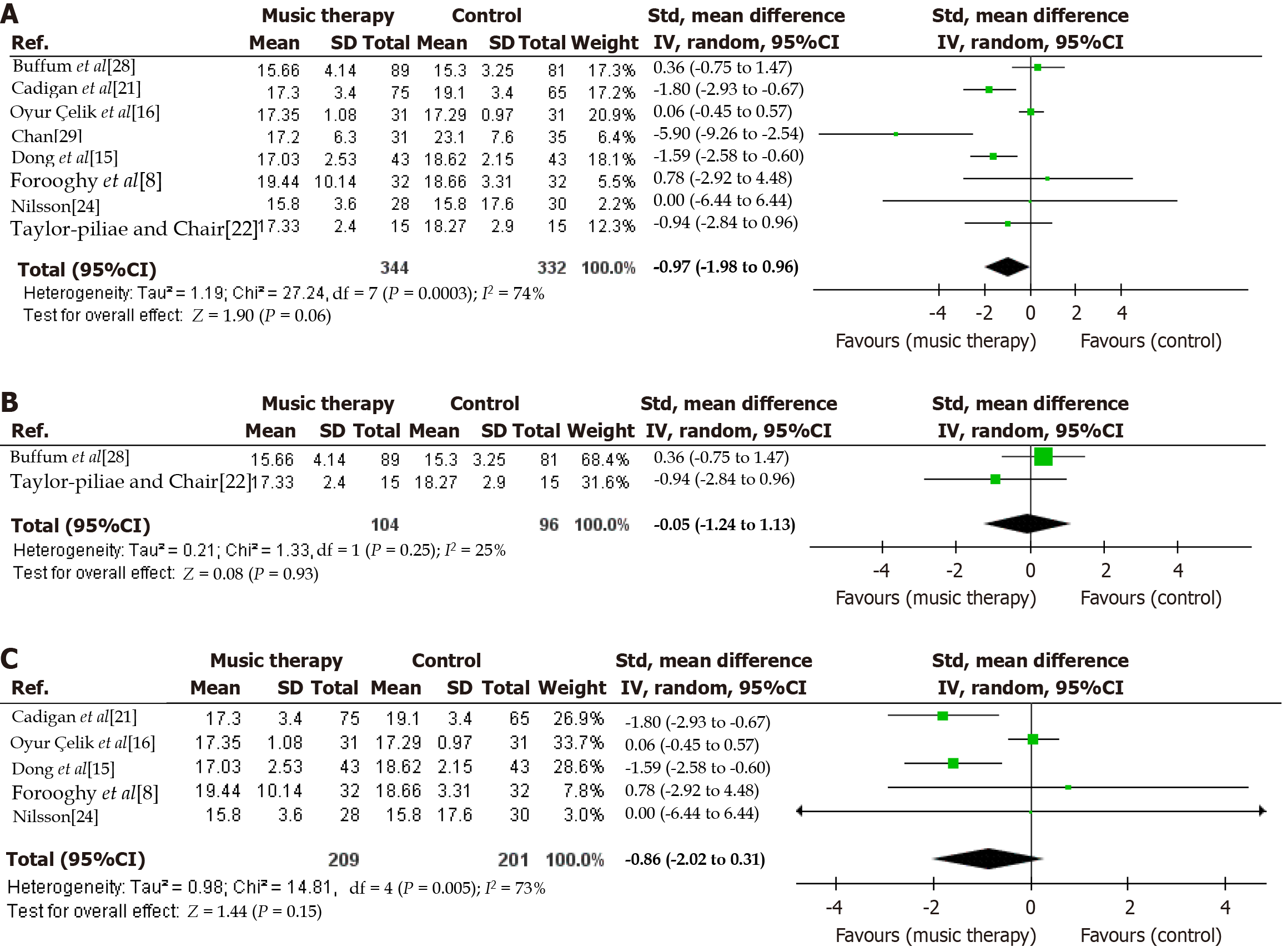
RR: Data for RR at any time was provided by 8 studies. Our pooled analysis showed that there was no significant difference between the two groups for RR at any time (MD = -0.97, 95%CI: -1.98 to 0.03; P = 0.06) (Figure 6A). Moderate heterogeneity was observed (I2 = 74%). No significant changes were observed for pre-procedural RR (MD = -0.05, 95%CI:
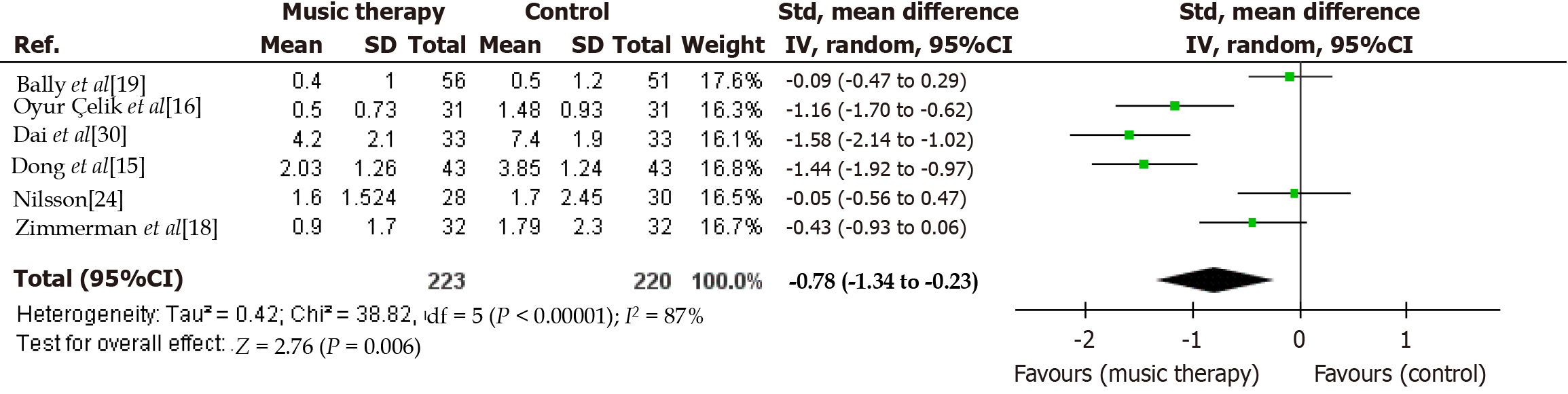
Pain: Six studies reported data for post-procedural pain. Our pooled analysis showed that music listening significantly reduced post-procedural pain (SMD = -0.78, 95%CI: -1.34 to -0.23; P = 0.006) (Figure 7)[15,16,18,19,24,30]. High heterogeneity was observed (I2 = 87%).
Our systematic review and meta-analysis of 21 studies evaluated the therapeutic effect of music on patients undergoing invasive cardiac surgeries. Our pooled analysis of results from 2141 participants demonstrated significant improvements in post-procedural pain, anxiety, HR, and SBP. However, we discovered no significant difference in DBP and RR. A central illustration summarizing the findings of our study is provided in Figure 8.
Our study focused on music therapy, defined as the clinical and evidence-based use of music interventions to accomplish individualized therapeutic goals. This includes managing symptoms such as anxiety, pain, and stress, which are prevalent in patients undergoing invasive cardiac procedures. Music therapy can be self-administered by patients through pre-selected playlists or conducted with the support of a music therapist, who tailors the intervention to patient’s specific emotional and physiological needs. This approach is grounded in both physiological theories and neurological evidence, which suggests that music interacts with the brain’s limbic and autonomic systems to modulate stress and emotional responses.
Our findings differed substantially from the previous meta-analysis[11]. In contrast to our results, the previous meta-analysis demonstrated the non-significance of music listening in improving post-procedural pain, HR, SBP, and DBP. The significant improvement observed in anxiety in previous studies was comparable to the findings of our meta-analysis. These discrepancies were noted because our analysis included many high-powered, previously missed published studies that had not been included in any of the prior analyses. Our study also considered some additional outcomes, such as RR, which have not been explored in the previous meta-analysis[11]. Hence, considering it is the most comprehensive and up-to-date analysis, this gives our study more statistical ability to produce the most precise and accurate assessments of impact sizes within the scope of the present literature.
Our results are consistent with other studies by Shum et al[33] and Lai and Good[34] that discovered that listening to music can regulate bodily rhythms by slowing them down. Consequently, this results in a decline in the body's noradre
The current research can be utilized to direct clinical procedures and raise the standard of care provided to patients having coronary angiography or PCI. For music intervention supplied during the treatment, appropriate intervention settings (kind, pace, volume, duration, and listening equipment) and music providers can be created. Inquiring about the patient's preferred music for relaxation during pre-operative care may allow nurses to play similar music in the catheterization room before invasive cardiac procedures. If patients' choices, rather than the preferences of researchers or surgeons, are taken into consideration when selecting music, we anticipate that the effects of music intervention may be more noticeable. To encourage research endeavors and a more individualized approach to choosing music that suits patients' preferences, the hospital may include a licensed music therapist in the surgery team. To ensure that patients receive tailored music interventions that align with their therapeutic needs, a licensed music therapist can collaborate with the healthcare team to create personalized playlists. This approach respects the expertise of music therapists and allows nurses to focus on their core responsibilities while supporting non-pharmacological interventions. Nevertheless, further research is needed to ascertain if and how using a music therapist influences the effectiveness of music intervention.
To the best of our knowledge, this meta-analysis represents the most comprehensive and current examination of the role of the therapeutic use of music in patients undergoing invasive cardiac procedures. This enables us to derive reliable conclusions from our pooled investigation as well as the most precise and dependable assessments of the impact sizes. Previous research in this area was constrained by a smaller data set and a more constrained range of results. Additionally, in contrast to the previous meta-analysis, we observed significant results for most of our outcomes.
While our study had certain strengths, there were some limitations that we encountered when performing the meta-analysis. Firstly, different studies reported the observed outcomes at different times, pre-procedural, post-procedural, and at any given time. This discrepancy was resolved by generating a subgroup analysis of all three instances. Secondly, significant heterogeneity was observed in all our outcomes. This could be attributed to the different types of music, mode of delivery, differences in patient population and their baseline characteristics, and time of intervention used. Additionally, this meta-analysis included 21 studies from seven different countries: (1) United States; (2) China; (3) Iran; (4) Turkey; (5) Sweden; (6) Germany; and (7) Hong Kong (China). Coronary procedures such as PCI and CABG are common treatments for coronary artery disease, but the characteristics of patients undergoing these procedures can differ significantly across regions due to differences in healthcare systems, socioeconomic status, and lifestyle choices. For example, in the United States and Western European countries such as Germany and Sweden, advanced coronary care is widely available, and patients frequently obtain prompt procedures. These nations have aging populations and a greater prevalence of coronary artery disease risk factors including hypertension and diabetes, which may impact procedure results as well as patient responsiveness to non-pharmacological therapies like music listening. In contrast, patient populations in Iran, Turkey, and China may have greater disparity in healthcare availability, particularly in rural regions. Cultural variables influence how nontraditional treatments, such as music listening, are perceived and integrated into care. For example, the music utilized in research from Iran and Turkey may have cultural meaning, perhaps influencing anxiety and pain results differently than in Western countries. Considering these differences, the generalizability of our findings may vary based on the population and healthcare context. While the therapeutic use of music has demonstrated consistent effects on anxiety and pain across diverse settings, the extent to which these results can be broadly applied may depend on the specific demographics and cultural backgrounds of the patients.
Last but not the least, our study focused exclusively on anxiety and does not include other psychological outcomes such as depression. We chose to examine anxiety as the primary psychological outcome for several reasons. First, anxiety is a well-documented response to invasive cardiac procedures and is frequently associated with worsened physiological parameters such as elevated HR and BP. This makes anxiety a key factor that can directly affect the success and outcomes of cardiac interventions. Anxiety also has a significant impact on patient’s perception of pain, thus exacerbating discomfort during and after procedures. By focusing on anxiety, our study aims to target a modifiable psychological factor that can lead to broader improvements in both, emotional well-being and physical health outcomes in patients undergoing invasive cardiac procedures. While depression and other psychosocial parameters are also relevant, anxiety is typically the most immediate and acute response to the stress of surgery, which made it the most logical focus of our analysis.
We acknowledge that research shows differences in outcomes between researcher-selected and patient-selected music in music listening interventions. While the studies included in our analysis did not consistently specify the method of music selection, this distinction could influence outcomes, as patient-preferred music may enhance relaxation and emotional engagement more effectively than researcher-selected music. Further research in this area would be beneficial to clarify the role of music selection in optimizing therapeutic outcomes.
Patients having cardiac surgery who already struggle with one or more psychological issues need special consideration. We discovered sufficient evidence in our study to validate the effectiveness of music listening interventions in improving anxiety, post-procedural pain, HR, and SBP, but not for improving RR and DBP. Therefore, therapeutic use of music can be used in healthcare settings to lower patients' anxiety levels and improve their physiological parameters.
| 1. | Benjamin EJ, Muntner P, Alonso A, Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, Chang AR, Cheng S, Das SR, Delling FN, Djousse L, Elkind MSV, Ferguson JF, Fornage M, Jordan LC, Khan SS, Kissela BM, Knutson KL, Kwan TW, Lackland DT, Lewis TT, Lichtman JH, Longenecker CT, Loop MS, Lutsey PL, Martin SS, Matsushita K, Moran AE, Mussolino ME, O'Flaherty M, Pandey A, Perak AM, Rosamond WD, Roth GA, Sampson UKA, Satou GM, Schroeder EB, Shah SH, Spartano NL, Stokes A, Tirschwell DL, Tsao CW, Turakhia MP, VanWagner LB, Wilkins JT, Wong SS, Virani SS; American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. Heart Disease and Stroke Statistics-2019 Update: A Report From the American Heart Association. Circulation. 2019;139:e56-e528. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4294] [Cited by in RCA: 6162] [Article Influence: 880.3] [Reference Citation Analysis (5)] |
| 2. | Su SF, Chang MY, Wu MS, Liao YC. Safety and efficacy of using vascular closure devices for hemostasis on sheath removal after a transfemoral artery percutaneous coronary intervention. Jpn J Nurs Sci. 2019;16:172-183. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (1)] |
| 3. | Rejeh N, Heravi-Karimooi M, Tadrisi SD, Jahani A, Vaismoradi M, Jordan S. The impact of listening to pleasant natural sounds on anxiety and physiologic parameters in patients undergoing coronary angiography: A pragmatic quasi-randomized-controlled trial. Complement Ther Clin Pract. 2016;25:42-51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 25] [Article Influence: 2.5] [Reference Citation Analysis (2)] |
| 4. | Angioli R, De Cicco Nardone C, Plotti F, Cafà EV, Dugo N, Damiani P, Ricciardi R, Linciano F, Terranova C. Use of music to reduce anxiety during office hysteroscopy: prospective randomized trial. J Minim Invasive Gynecol. 2014;21:454-459. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 84] [Article Influence: 7.0] [Reference Citation Analysis (1)] |
| 5. | Gaspersz R, Nawijn L, Lamers F, Penninx BWJH. Patients with anxious depression: overview of prevalence, pathophysiology and impact on course and treatment outcome. Curr Opin Psychiatry. 2018;31:17-25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 103] [Article Influence: 12.9] [Reference Citation Analysis (1)] |
| 6. | Soltani E, Nomali M, Ghiyasvandian S, Kazemnejad A, Zakerimoghadam M. Effect of Listening to Preferred Music on General Comfort Level among Patients Underwent Coronary Artery Bypass Graft Surgery: A Randomized Controlled Trial. J Med Res. 2018;4:233-239. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 7. | Kühlmann AYR, de Rooij A, Kroese LF, van Dijk M, Hunink MGM, Jeekel J. Meta-analysis evaluating music interventions for anxiety and pain in surgery. Br J Surg. 2018;105:773-783. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 107] [Cited by in RCA: 245] [Article Influence: 30.6] [Reference Citation Analysis (1)] |
| 8. | Forooghy M, Mottahedian Tabrizi E, Hajizadeh E, Pishgoo B. Effect of Music Therapy on Patients' Anxiety and Hemodynamic Parameters During Coronary Angioplasty: A Randomized Controlled Trial. Nurs Midwifery Stud. 2015;4:e25800. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 26] [Article Influence: 2.4] [Reference Citation Analysis (2)] |
| 9. | Gasenzer ER, Neugebauer EA. [The relations between music and medicine in history and present]. Dtsch Med Wochenschr. 2011;136:2644-2651. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 10. | Juslin PN, Västfjäll D. Emotional responses to music: the need to consider underlying mechanisms. Behav Brain Sci. 2008;31:559-575; discussion 575. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 736] [Cited by in RCA: 523] [Article Influence: 29.1] [Reference Citation Analysis (1)] |
| 11. | Su SF, Yeh WT. Music Interventions in Percutaneous Coronary Procedures: A Meta-Analysis. Clin Nurs Res. 2021;30:135-145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (2)] |
| 12. | Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 52948] [Cited by in RCA: 48584] [Article Influence: 2857.9] [Reference Citation Analysis (3)] |
| 13. | Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, Henry D, Altman DG, Ansari MT, Boutron I, Carpenter JR, Chan AW, Churchill R, Deeks JJ, Hróbjartsson A, Kirkham J, Jüni P, Loke YK, Pigott TD, Ramsay CR, Regidor D, Rothstein HR, Sandhu L, Santaguida PL, Schünemann HJ, Shea B, Shrier I, Tugwell P, Turner L, Valentine JC, Waddington H, Waters E, Wells GA, Whiting PF, Higgins JP. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7683] [Cited by in RCA: 12494] [Article Influence: 1249.4] [Reference Citation Analysis (2)] |
| 14. | Moradipanah F, Mohammadi E, Mohammadil A. Effect of music on anxiety, stress, and depression levels in patients undergoing coronary angiography. East Mediterr Health J. 2009;15:639-647. [PubMed] |
| 15. | Dong Y, Zhang L, Chen LW, Luo ZR. Music therapy for pain and anxiety in patients after cardiac valve replacement: a randomized controlled clinical trial. BMC Cardiovasc Disord. 2023;23:32. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 21] [Reference Citation Analysis (1)] |
| 16. | Oyur Çelik G, Güzelçiçek A, Çelik S. The Effects of Music Therapy on Patients With Coronary Artery Disease Before the Invasive Procedure: A Randomized Controlled Study. J Perianesth Nurs. 2022;37:194-198. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 17] [Article Influence: 3.4] [Reference Citation Analysis (2)] |
| 17. | Doğan MV, Şenturan L. The effect of music therapy on the level of anxiety in the patients undergoing coronary angiography. OJN. 2012;02:165-169. [RCA] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 23] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 18. | Zimmerman L, Nieveen J, Barnason S, Schmaderer M. The effects of music interventions on postoperative pain and sleep in coronary artery bypass graft (CABG) patients. Sch Inq Nurs Pract. 1996;10:153-170; discussion 171. [PubMed] |
| 19. | Bally K, Campbell D, Chesnick K, Tranmer JE. Effects of Patient-Controlled Music Therapy During Coronary Angiography on Procedural Pain and Anxiety Distress Syndrome. Crit Care Nurse. 2003;23:50-58. [PubMed] |
| 20. | Hamel WJ. The effects of music intervention on anxiety in the patient waiting for cardiac catheterization. Intensive Crit Care Nurs. 2001;17:279-285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 84] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 21. | Cadigan ME, Caruso NA, Haldeman SM, McNamara ME, Noyes DA, Spadafora MA, Carroll DL. The effects of music on cardiac patients on bed rest. Prog Cardiovasc Nurs. 2001;16:5-13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 31] [Article Influence: 1.2] [Reference Citation Analysis (1)] |
| 22. | Taylor-Piliae RE, Chair SY. The effect of nursing interventions utilizing music therapy or sensory information on Chinese patients' anxiety prior to cardiac catheterization: a pilot study. Eur J Cardiovasc Nurs. 2002;1:203-211. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 55] [Article Influence: 5.5] [Reference Citation Analysis (1)] |
| 23. | Argstatter H, Haberbosch W, Bolay HV. Study of the effectiveness of musical stimulation during intracardiac catheterization. Clin Res Cardiol. 2006;95:514-522. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 42] [Article Influence: 2.1] [Reference Citation Analysis (1)] |
| 24. | Nilsson U. The effect of music intervention in stress response to cardiac surgery in a randomized clinical trial. Heart Lung. 2009;38:201-207. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 136] [Article Influence: 8.0] [Reference Citation Analysis (1)] |
| 25. | Nilsson U. Effectiveness of music interventions for women with high anxiety during coronary angiographic procedures: a randomized controlled. Eur J Cardiovasc Nurs. 2012;11:150-153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 1.6] [Reference Citation Analysis (1)] |
| 26. | Amiri MJ, Sadeghi T, Negahban Bonabi T. The effect of natural sounds on the anxiety of patients undergoing coronary artery bypass graft surgery. Perioper Med (Lond). 2017;6:17. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 19] [Article Influence: 2.1] [Reference Citation Analysis (1)] |
| 27. | Barnason S, Zimmerman L, Nieveen J. The effects of music interventions on anxiety in the patient after coronary artery bypass grafting. Heart Lung. 1995;24:124-132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 109] [Article Influence: 3.5] [Reference Citation Analysis (1)] |
| 28. | Buffum MD, Sasso C, Sands LP, Lanier E, Yellen M, Hayes A. A music intervention to reduce anxiety before vascular angiography procedures. J Vasc Nurs. 2006;24:68-73; quiz 74. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 67] [Article Influence: 3.4] [Reference Citation Analysis (1)] |
| 29. | Chan MF. Effects of music on patients undergoing a C-clamp procedure after percutaneous coronary interventions: a randomized controlled trial. Heart Lung. 2007;36:431-439. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 47] [Article Influence: 2.5] [Reference Citation Analysis (1)] |
| 30. | Dai WS, Huang ST, Xu N, Chen Q, Cao H. The effect of music therapy on pain, anxiety and depression in patients after coronary artery bypass grafting. J Cardiothorac Surg. 2020;15:81. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 36] [Article Influence: 6.0] [Reference Citation Analysis (1)] |
| 31. | Heidari S, Babaii A, Abbasinia M, Shamali M, Abbasi M, Rezaei M. The Effect of Music on Anxiety and Cardiovascular Indices in Patients Undergoing Coronary Artery Bypass Graft: A Randomized Controlled Trial. Nurs Midwifery Stud. 2015;4:e31157. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 29] [Article Influence: 2.6] [Reference Citation Analysis (1)] |
| 32. | Twiss E, Seaver J, McCaffrey R. The effect of music listening on older adults undergoing cardiovascular surgery. Nurs Crit Care. 2006;11:224-231. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 79] [Article Influence: 4.0] [Reference Citation Analysis (1)] |
| 33. | Shum A, Taylor BJ, Thayala J, Chan MF. The effects of sedative music on sleep quality of older community-dwelling adults in Singapore. Complement Ther Med. 2014;22:49-56. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 37] [Article Influence: 3.1] [Reference Citation Analysis (1)] |
| 34. | Lai HL, Good M. Music improves sleep quality in older adults. J Adv Nurs. 2005;49:234-244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 119] [Article Influence: 5.7] [Reference Citation Analysis (1)] |
| 35. | Wu L, Yao Y. Exploring the effect of music therapy as intervention to reduce anxiety pre- and post-operatively in CABG surgery: A quantitative systematic review. Nurs Open. 2023;10:7544-7565. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 1.7] [Reference Citation Analysis (1)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/