Published online Jun 26, 2024. doi: 10.4330/wjc.v16.i6.339
Revised: May 21, 2024
Accepted: May 24, 2024
Published online: June 26, 2024
Processing time: 123 Days and 14.4 Hours
Mesenchymal stem cells (MSCs) as living biopharmaceuticals with unique properties, i.e., stemness, viability, phenotypes, paracrine activity, etc., need to be administered such that they reach the target site, maintaining these properties unchanged and are retained at the injury site to participate in the repair process. Route of delivery (RoD) remains one of the critical determinants of safety and efficacy. This study elucidates the safety and effectiveness of different RoDs of MSC treatment in heart failure (HF) based on phase II randomized clinical trials (RCTs). We hypothesize that the RoD modulates the safety and efficacy of MSC-based therapy and determines the outcome of the intervention.
To investigate the effect of RoD of MSCs on safety and efficacy in HF patients.
RCTs were retrieved from six databases. Safety endpoints included mortality and serious adverse events (SAEs), while efficacy outcomes encompassed changes in left ventricular ejection fraction (LVEF), 6-minute walk distance (6MWD), and pro-B-type natriuretic peptide (pro-BNP). Subgroup analyses on RoD were performed for all study endpoints.
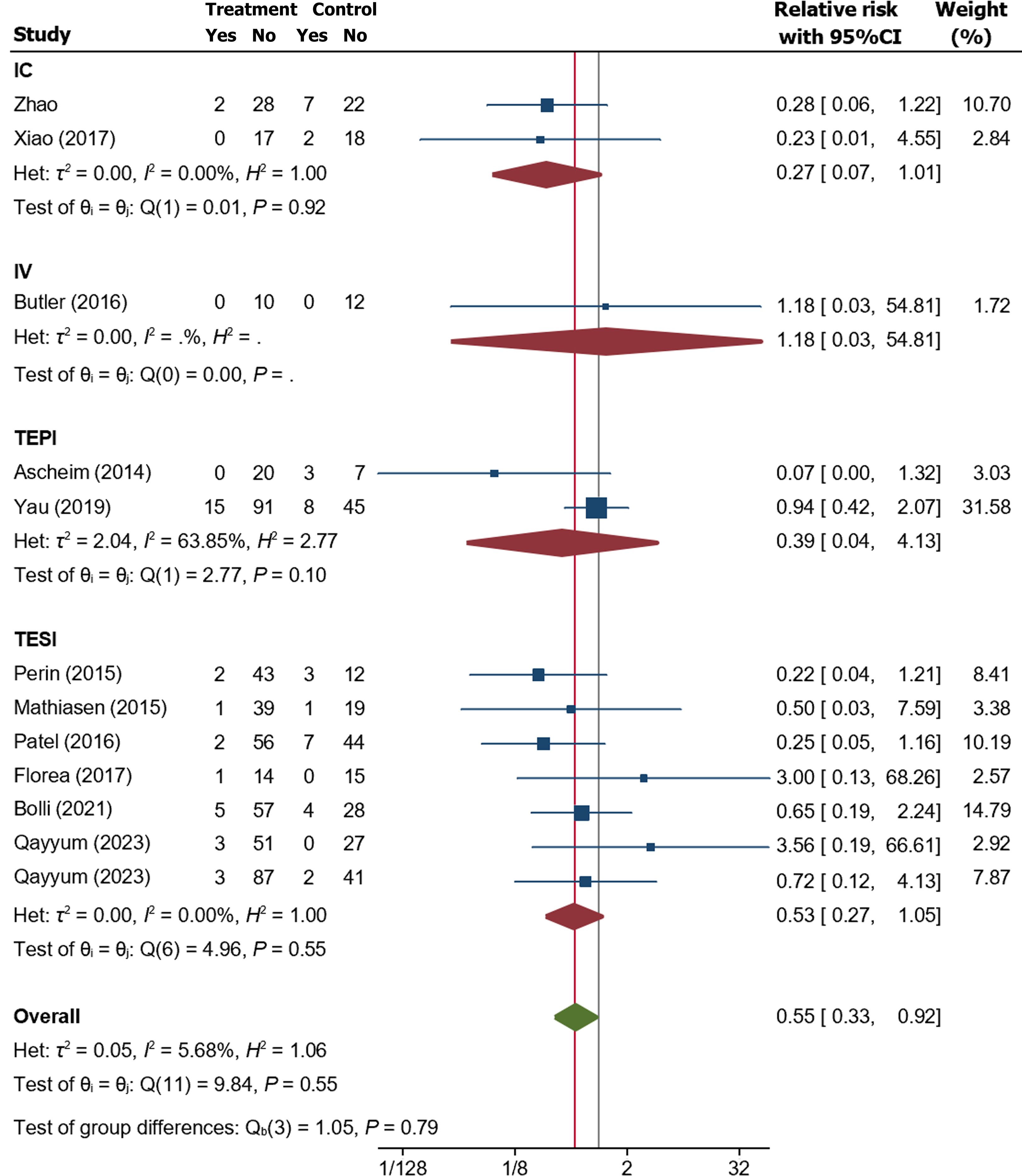
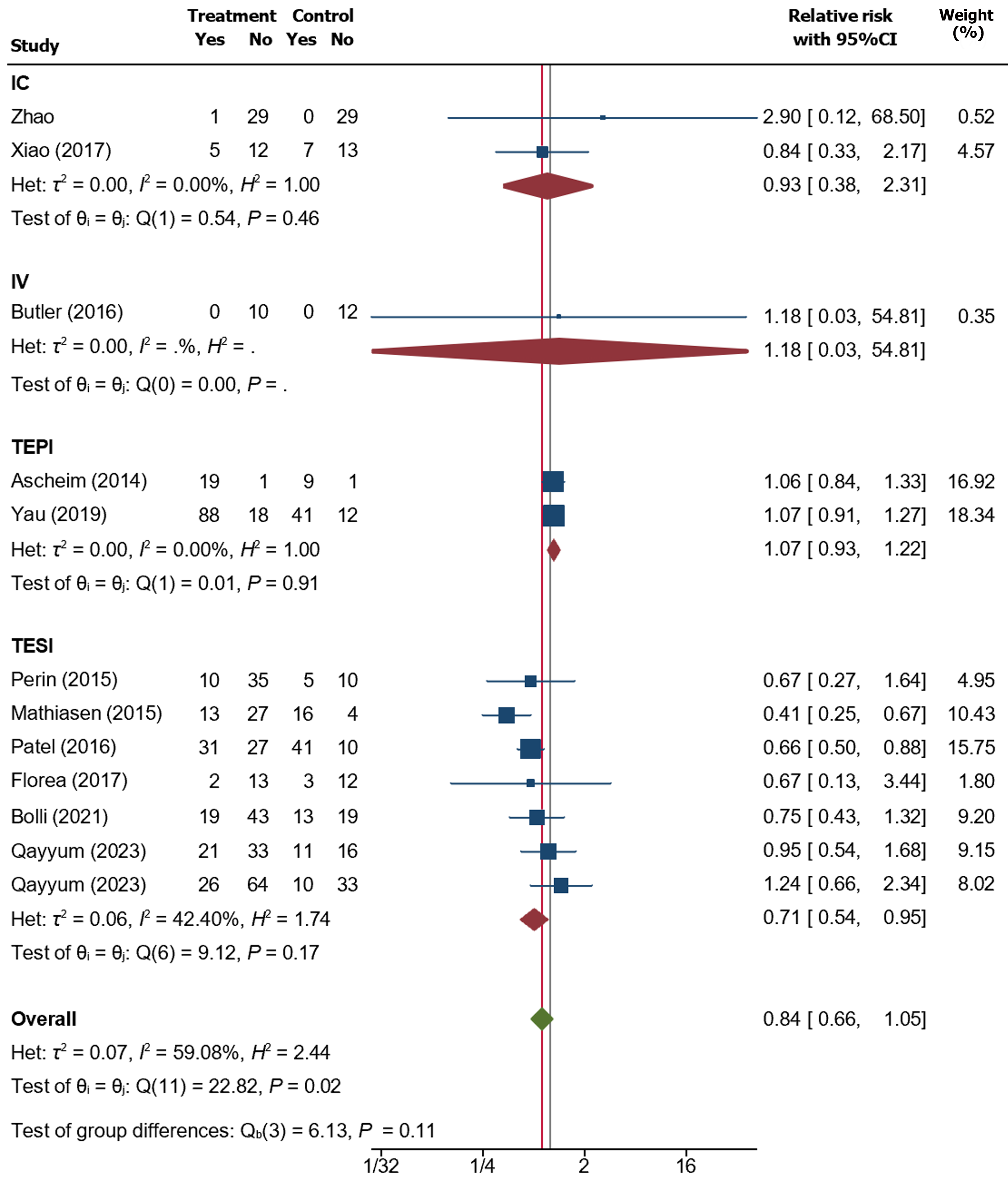
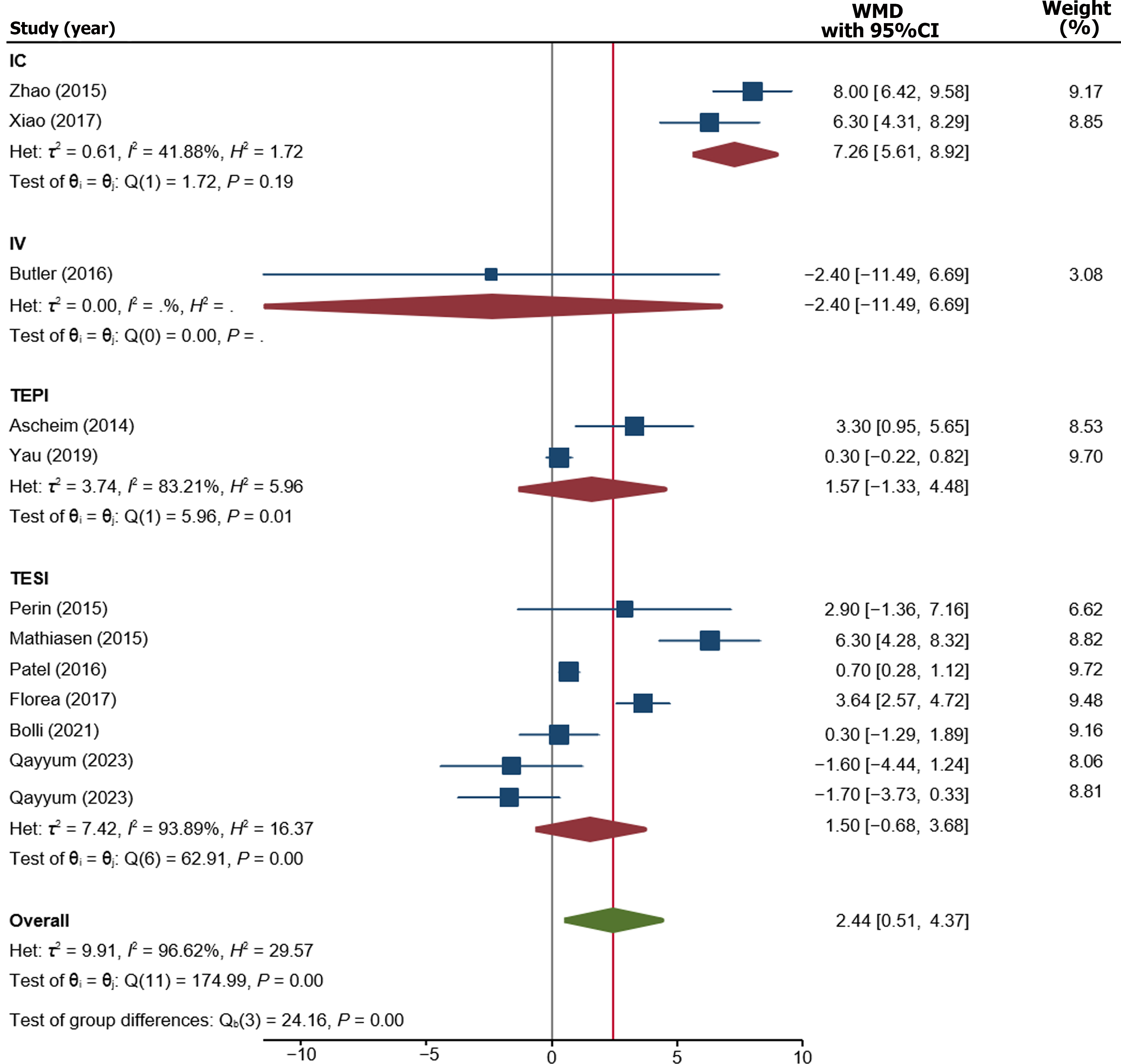
Twelve RCTs were included. Overall, MSC therapy demonstrated a significant decrease in mortality [relative risk (RR): 0.55, 95% confidence interval (95%CI): 0.33-0.92, P = 0.02] compared to control, while SAE outcomes showed no significant difference (RR: 0.84, 95%CI: 0.66-1.05, P = 0.11). RoD subgroup analysis revealed a significant difference in SAE among the transendocardial (TESI) injection subgroup (RR = 0.71, 95%CI: 0.54-0.95, P = 0.04). The pooled weighted mean difference (WMD) demonstrated an overall significant improvement of LVEF by 2.44% (WMD: 2.44%, 95%CI: 0.80-4.29, P value ≤ 0.001), with only intracoronary (IC) subgroup showing significant improvement (WMD: 7.26%, 95%CI: 5.61-8.92, P ≤ 0.001). Furthermore, the IC delivery route significantly improved 6MWD by 115 m (WMD = 114.99 m, 95%CI: 91.48-138.50), respectively. In biochemical efficacy outcomes, only the IC subgroup showed a significant reduction in pro-BNP by -860.64 pg/mL (WMD: -860.64 pg/Ml, 95%CI: -944.02 to -777.26, P = 0.001).
Our study concluded that all delivery methods of MSC-based therapy are safe. Despite the overall benefits in efficacy, the TESI and IC routes provided better outcomes than other methods. Larger-scale trials are warranted before implementing MSC-based therapy in routine clinical practice.
Core Tip: Route of delivery (RoD) remains a critical determinant of safety and efficacy in cardiac stem cell therapy, particularly in heart failure (HF) patients. HF occurs when the heart’s pumping ability is inadequate to meet the body’s metabolic needs. Mesenchymal stem cells (MSCs) are living biopharmaceuticals with unique properties that need to be administered such that they reach the target site and are retained there to participate in the repair process. This systematic review and meta-analysis of phase II randomized clinical trials determine the RoD effect on the safety and efficacy of MSCs during HF treatment.
- Citation: Jihwaprani MC, Sula I, Charbat MA, Haider KH. Establishing delivery route-dependent safety and efficacy of living biodrug mesenchymal stem cells in heart failure patients. World J Cardiol 2024; 16(6): 339-354
- URL: https://www.wjgnet.com/1949-8462/full/v16/i6/339.htm
- DOI: https://dx.doi.org/10.4330/wjc.v16.i6.339
According to the updates from the American Heart Association, the prevalence of heart failure (HF) is expected to increase by 46% from 2012 to 2030, affecting approximately eight million individuals aged 18 years and older, highlighting a substantial increase in healthcare financial burden globally[1]. The contemporary treatment modalities provide only symptomatic relief without addressing the underlying issues, primarily attributed to the loss of functioning cardiomyocytes (CMs) and accentuated by the limited intrinsic repair mechanism to replace the lost CMs. This remains a challenge for the contemporary treatment options to compensate for the massive loss of functioning CMs, which enter the heart into a vicious cycle of remodeling, the hallmark of both ischemic and non-ischemic HF[2]. Hence, there is an urgent need to develop novel therapeutic strategies to address this issue that can repopulate the ischemically damaged myocardium with morphofunctionally competent CMs[3,4].
Mesenchymal stem cells (MSCs) are emerging as a promising living bio-drug for treating HF patients[5,6]. Since the reporting of the first clinical study by Hamano et al[7] using autologous bone marrow-derived MSCs (BM-MSCs) as an adjunct to coronary artery bypass graft surgery in five patients, several clinical trials have established the safety of MSC-based therapy in cardiac and non-cardiac diseases[8]. Current clinical trials to evaluate the efficacy of MSCs in HF patients have increased exponentially, among which are the Congestive Heart Failure Cardiopoietic Regenerative Therapy (CHART-1)[9], Double-Blind Randomized Assessment of Clinical Events With Allogeneic Mesenchymal Precursor Cells in Heart Failure[10], Cardiopoietic stem Cell therapy in heart failure (C-CURE) study[11], and Prospective Randomized Study of MSC Therapy in Patients Undergoing Cardiac Surgery[12] besides several randomized clinical trials (RCTs) advancing to phase III as well[13,14]. Despite these advancements and some encouraging data, there is little consensus on the best cell route of delivery (RoD) for the heart, which has been shown to significantly modulate the survival and efficacy of the delivered MSCs[15].
To date, numerous studies have investigated the efficacy of MSCs using various RoD, with the most commonly employed methods being transendocardial (TESI), transepicardial injection (TEPI) under direct vision, IC infusion, and intravenous (IV) infusion[16]. Each RoD has its own set of advantages and limitations, encompassing factors such as delivery method convenience, invasiveness level, capability for site-directed cell delivery, the need for adjunct procedures, i.e., left ventricular (LV) assist device (LVAD), coronary artery bypass grafting, eligibility for multiple or repeated dose administrations, and potential side-effect profiles.
This systematic review and meta-analysis primarily focus on evaluating phase II RCT data to investigate the effect of RoD of MSCs for safety and efficacy in HF patients. We hypothesize that the route of cell delivery modulates the safety and efficacy of MSC-based therapy and determines the outcome of the intervention. To the best of our knowledge, this is the first systematic review and meta-analysis to evaluate the effect of the route of administering MSCs on HF patients derived from early phase-II RCTs.
This study used the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) protocol. Its design was comprehensively developed and prospectively registered in the PROSPERO International Prospective Register of Systematic Reviews, registration number CRD42023484749.
The identification of relevant studies was conducted from October 18 to November 19, 2023, using the following databases: PubMed/MEDLINE, Clinicaltrials.gov, ScienceDirect, Cochrane CENTRAL, EBSCOHost, and the European Union Drug Regulating Authorities Clinical Trials (EudraCT). The keyword ‘heart failure’ was adopted as a MeSH term. In contrast, the terms “Mesenchymal Stem Cells”, “Mesenchymal Precursor Cells”, “Mesenchymal Progenitor Cells”, and equivalent terms were used as a text field search. We incorporated all the predefined keywords with the Boolean operators “AND” and “OR”. Lastly, we thoroughly snowballed the references from retrieved articles for potentially relevant studies.
Using our predefined eligibility criteria, the review included all studies which were: (1) Phase II RCT; (2) recruited adult patients aged over 18 years old with HF; (3) had a control arm; (4) intervention arm received MSC therapy; and (5) written in the English language. Any studies that did not fulfill the aforementioned inclusion criteria were therefore excluded. Following the literature compilation, two reviewers (MJ and IS) independently screened the retrieved studies for duplicates and compliance with eligibility criteria. Any discrepancies were solved by discussion between the reviewers and, when appropriate, the involvement of the remaining two authors (MC and KH).
After the initial abstract and title screening, the studies were further screened for full-text review and data extraction. The data extraction was accomplished using the predefined Excel sheet that incorporated several primary variables, including the trial registry, name of primary author, year of publication, design of the RCT, blinding status, country, sample size, mean age, type of MSC and its source, type of control arm, the RoD, MSC dose, New York Heart Association (NYHA) status at baseline, imaging modalities used for LV assessment, and time to follow up for primary outcomes and LV ejection fraction (LVEF) assessment. Furthermore, the five outcome variables were recorded, including the number of serious adverse events (SAE), number of death, LVEF (percentage), 6-minute walk distance (6MWD) (meters), and Pro-B-type natriuretic peptide (pro-BNP) (in pg/mL). The outcome variables were recorded at baseline and upon follow-up when relevant.
We assessed the included RCTs using the Jadad scale to evaluate the risk of bias. In summary, the Jadad scale assesses three items: randomization (up to two points), double-blinding (up to two points), and correct reporting of withdrawals and dropouts (up to one point)[17]. Upon completion of the evaluation process, the scores ranging from zero to five were added to determine the quality score for each trial. A study with 0-2 was considered low quality, while the one scoring ≥ 3 was considered superior quality.
The endpoints of this study included safety and efficacy outcomes. Safety outcomes were defined as the number of deaths and SAEs on follow-up. Efficacy outcomes, on the other hand, encompassed functional, clinical, and biochemical outcomes, which were determined by changes in LVEF (percentage), 6MWD (meters), and pro-BNP (pg/mL) compared to their respective baseline values. Regenerative capacity, ideally evaluated by LV wall thickness, was not included in the efficacy outcome measure due to a lack of data almost uniformly across all the included trials. Safety outcomes were regarded as dichotomous variables and were reported in relative risk (RR). In contrast, the efficacy outcomes were regarded as continuous and reported in weighted mean difference (WMD). The random-effect model was used due to a variety of population origins. The RR was considered statistically significant if the 95% confidence interval (CI) did not contain the value of 1, i.e., the null hypothesis value. On the other hand, if the WMD’s 95%CI included the value of 0, the value was considered not statistically significant. Further, as our study focuses on the influence of different RoD on the outcomes, we run a subgroup analysis of the RoD in all outcome variables.
Heterogeneity analysis was evaluated with I2 statistics and τ2. The I2 values of < 25% represent a low heterogeneity, with 25%-75% as moderate probability, whereas > 75% is considered high probability. The funnel plot assessed publication bias visually, using Egger’s regression test for statistical assessments. Subgroup meta-analyses were implemented to identify the sources of heterogeneity. We also performed standard leave-one-out sensitivity analyses to safety and efficacy endpoints to identify studies that significantly influenced the pooled estimates. Results were considered to be statistically significant at P value ≤ 0.05. This statistical analysis used the IBM SPSS Statistics for Mac (Version 28.0. IBM Corp., Armonk, NY, United States) and Stata (Stata Statistical Software: Version 17, College Station, TX: Stata Corp LP).
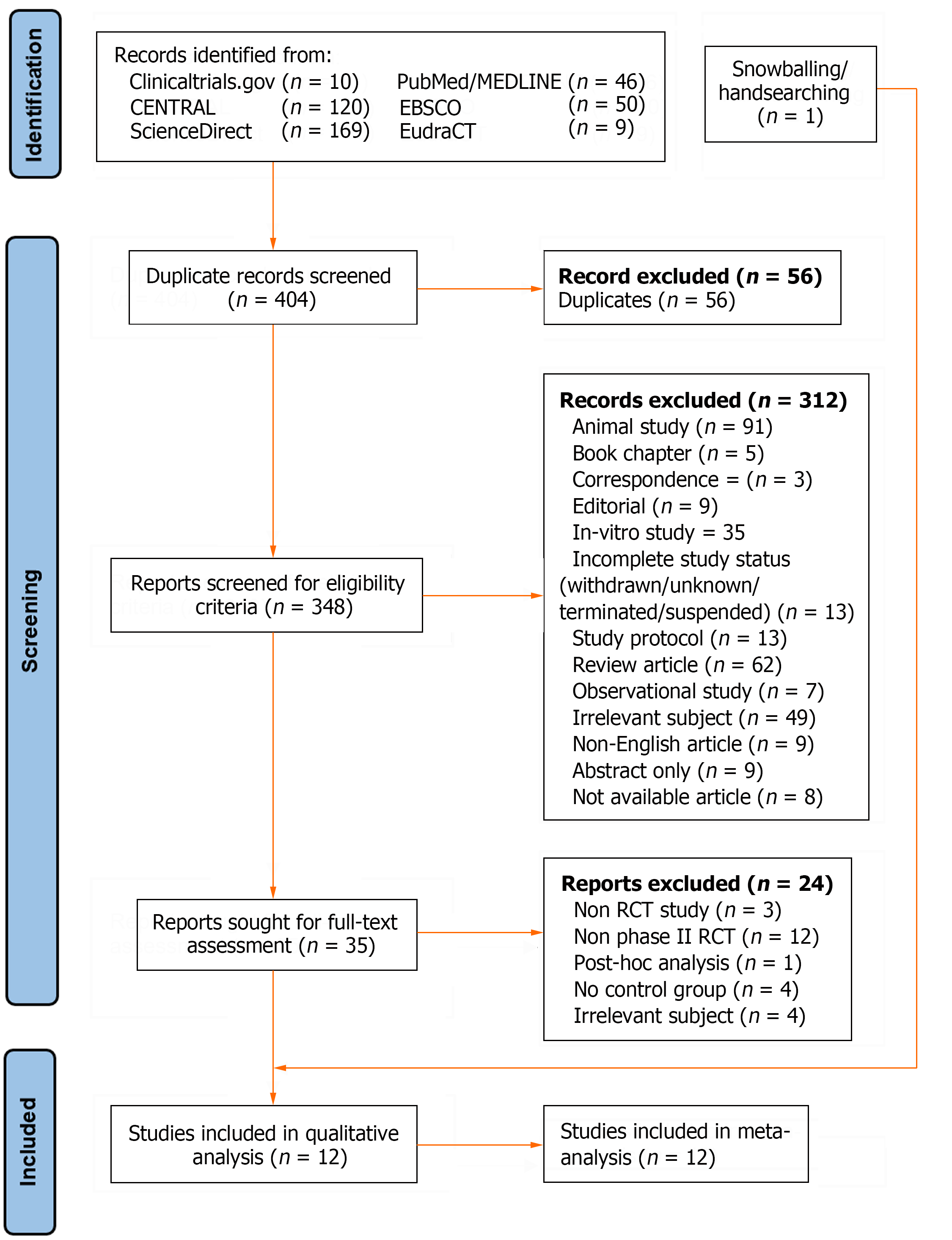
A total of 404 studies were identified from six databases, i.e., Clinicaltrials.gov (n = 10), CENTRAL (n = 120), ScienceDirect (n = 169), PubMed/MEDLINE (n = 46), EBSCOHost (n = 50), and EudraCT (n = 9). Initial screening identified duplicates (n = 56), with further abstract/title screening excluded studies for animal studies (n = 91), book chapter (n = 5), correspondence (n = 3), editorial (n = 9), in-vitro studies (n = 35), incomplete study status (n = 13), study protocol (n = 13), review article (n = 62), observational study (n = 7), irrelevant subject (n = 49), non-English articles (n = 9), abstract only (n = 9), and not available articles (n = 8). Upon full-text assessment of the remaining 35 studies, 24 studies were excluded from the review for non-RCT study (n = 3), non-phase II RCT (n = 12), posthoc analysis (n = 1), no available control arm (n = 4), and irrelevant subject (n = 4). In addition, handpicking from the references of retrieved papers yielded one study, leaving us with twelve studies for inclusion in systematic review and meta-analysis, as depicted in the PRISMA flow diagram of the study (Figure 1).
Table 1 shows the baseline characteristics of the 12 RCTs included in our study that were published between 2014 and 2023. Male participants represented most of the sample, with the mean age ranging from 40 to 70. Nine of the 12 RCTs were double-blinded. Nine studies used BM-MSC as an intervention, seven of which were allogeneic MSCs retrieved from healthy donors. On the other hand, only two and one RCTs used adipose-derived MSC (A-MSC) and umbilical cord-derived MSC, all of which were allogeneic. Ten RCTs used placebo-treated patients (e.g., isotonic saline) for comparison. In contrast, Florea et al[18] had BM-MSC at a lower dose, i.e., 20 million, as a control arm (compared to 100 million in the treatment arm). In contrast, Zhao et al[19] only used standard care as the control arm, i.e., drug only, instead of injecting a placebo-containing solution.
| Ref. | Trial registry | Study design, phase, blinding | Sample size (n) | Size at each arm (n) | Sex (n) | Age (yr) | Intervention | Source | Cell type | RoD | Dose (million) | NYHA | |||||
| M | F | I | II | III | IV | ||||||||||||
| Ascheim et al[21], 2014 | NCT01442129 | RCT, II, double-blind | 30 | Exp | 20 | 17 | 3 | 55.10 ± 15.40 | BM-MSC | NA | Allo | TEPI | 25 | 0 | 0 | 3 | 17 |
| Ctrl | 10 | 8 | 12 | 62.20 ± 7.80 | Placebo | 0 | 1 | 2 | 7 | ||||||||
| Perin et al[27], 2015 | NCT00721045 | RCT, II, double-blind | 60 | Exp | 45 | 44 | 1 | 62.20 ± 10.30 | BM-MSC | Iliac crest | Allo | TESI | 25, 75, 150 | 0 | 31 | 6 | 0 |
| Ctrl | 15 | 11 | 4 | 62.70 ± 11.20 | Placebo | 0 | 14 | 9 | 0 | ||||||||
| Mathiasen et al[25], 2015 | NCT00644410 | RCT, II, double-blind | 60 | Exp | 40 | 36 | 6 | 66.10 ± 7.70 | BM-MSC | NA | Auto | TESI | NA | 0 | 11 | 29 | 0 |
| Ctrl | 20 | 14 | 6 | 64.20 ± 10.60 | Placebo | 0 | 5 | 15 | 0 | ||||||||
| Zhao et al[19], 2015 | NA | RCT, NA, NA | 59 | Exp | 30 | 24 | 6 | 52.90 ± 16.32 | UC-MSC | Fetal UC | Allo | IC | NA | NA | NA | NA | NA |
| Ctrl | 29 | 19 | 10 | 53.21 ± 11.46 | Standard care | NA | NA | NA | NA | ||||||||
| Patel et al[23], 2016 | NCT01670981 | RCT, II, double-blind | 109 | Exp | 58 | 55 | 3 | 65.30 ± 8.49 | BM-MSC | Iliac crest | Auto | TESI | NA | 0 | 2 | 52 | 4 |
| Ctrl | 51 | 45 | 6 | 64.70 ± 9.94 | Placebo | 0 | 2 | 47 | 2 | ||||||||
| Butler et al[22], 2017 | NCT02467387 | RCT, II, single-blind | 22 | Exp | 10 | 13 | 9 | 47.30 ± 12.80 | BM-MSC | NA | Allo | IV | 1.5/kg | 0 | 21 | 1 | 0 |
| Ctrl | 12 | Placebo | |||||||||||||||
| Xiao et al[29], 2017 | NA | RCT, NA, double-blind | 37 | Exp | 17 | 12 | 5 | 51.60 ± 12.20 | BM-MSC | Iliac spine | Auto | IC | NA | NA | NA | NA | NA |
| Ctrl | 20 | 14 | 6 | 15.40 ± 11.60 | Placebo | NA | NA | NA | NA | ||||||||
| Florea et al[18], 2017 | NCT02013674 | RCT, II, double-blind | 30 | Exp | 15 | 15 | 0 | 65.60 ± 9.40 | BM-MSC | NA | Allo | TESI | 100 | 6 | 7 | 1 | 1 |
| Ctrl | 15 | 12 | 3 | 66.80 ± 12.20 | BM-MSC | NA | Allo | TESI | 20 | 4 | 8 | 3 | 0 | ||||
| Yau et al[20], 2019 | NCT02362646 | RCT, II, NA | 159 | Exp | 106 | 94 | 12 | 55.50 ± 12.30 | BM-MSC | NA | Allo | TEPI | 150 | 0 | 0 | 31 | 75 |
| Ctrl | 53 | 47 | 6 | 56.90 ± 11.70 | Placebo | 0 | 0 | 12 | 41 | ||||||||
| Bolli et al[26], 2021 | NCT02501811 | RCT, II, double-blind | 94 | Exp | 62 | 58 | 4 | 61.35 ± 8.90 | BM-MSC ± CPC | NA | Allo | TESI | 150 | 2 | 46 | 14 | 0 |
| Ctrl | 32 | 31 | 1 | 63.10 ± 8.80 | Placebo | 1 | 28 | 3 | 0 | ||||||||
| Qayyum et al[28], 2023 | NCT03092284 | RCT, II, double-blind | 81 | Exp | 54 | 44 | 10 | 67.00 ± 9.00 | A-MSC | Abd SC | Allo | TESI | 100 | NA | NA | NA | NA |
| Ctrl | 27 | 24 | 3 | 66.60 ± 8.10 | Placebo | NA | NA | NA | NA | ||||||||
| Qayyum et al[28], 2023 | NCT02673164 | RCT, II, double-blind | 133 | Exp | 90 | 84 | 6 | 66.40 ± 8.10 | A-MSC | Abd SC | Allo | TESI | 100 | 0 | 62 | 28 | 0 |
| Ctrl | 43 | 38 | 5 | 64.00 ± 8.80 | Placebo | 0 | 30 | 13 | 0 | ||||||||
Regarding RoD, seven studies employed the TESI RoD, whereas both TEPI and IC routes accounted for two studies each. Only one study used IV RoD for MSC delivery. Out of the total sample of 874 participants, the TESI route contributed to the largest sample size (total n = 567, intervention arm n = 364, control arm n = 203), followed by TEPI (total n = 189, intervention arm n = 126, control arm n = 63), IC (total n = 96, intervention arm n = 47, control arm n = 49), and IV infusion (total n = 22, intervention arm n = 10, control arm n = 12). Two studies, i.e., Yau et al[20] and Ascheim et al[21], included populations necessitating the placement of LVAD with the TEPI-administered MSCs or placebo during the placement of LVAD. There was a large variability in the injected dose of the MSCs, ranging from 25-150 million cells. The follow-up for primary outcomes and LVEF assessment was conducted beyond six months for all studies except Butler et al[22], which assessed the LVEF three months after the procedure. The measurements of LVEF, 6MWD, and pro-BNP on the baseline and during the follow-up have been summarized in Table 2.
| Ref. | Trial registry | Arm | FU | Imaging | SAE/death | LVEF (%) | 6MWD (meter) | Pro-BNP (pg/mL) | |||||||
| For 1° outcome | For LVEF | Echo | CCT | CMR | SPECT | Baseline | FU | Baseline | FU | Baseline | FU | ||||
| Ascheim et al[21], 2014 | NCT01442129 | Exp | 12 | 12 | Yes | No | No | No | 19/0 | 17.50 ± 3.90 | 24.00 ± 3.90 | NA | 883.00 ± 233.00 | NA | NA |
| Ctrl | 9/3 | 19.30 ± 5.10 | 22.50 ± 5.10 | NA | 1080.00 ± 359.50 | NA | NA | ||||||||
| Perin et al[27], 2015 | NCT00721045 | Exp | 36 | 12 | Yes | No | No | Yes | 10/2 | 31.30 ± 8.58 | 32.40 ± 8.70 | 401.60 ± 96.40 | 427.30 ± 115.10 | 436.80 ± 563.40 | 347.30 ± 335.69 |
| Ctrl | 5/3 | 34.60 ± 6.43 | 33.10 ± 9.30 | 319.30 ± 121.40 | 346.60 ± 121.80 | 217.70 ± 149.60 | 319.80 ± 193.02 | ||||||||
| Mathiasen et al[25], 2015 | NCT00644410 | Exp | 6 | 6 | Yes | Yes | Yes | No | 13/1 | 28.20 ± 9.30 | 33.20 ± 3.80 | 401.00 ± 70.00 | 421.40 ± 76.60 | 582.69 ± 970.01 | NA |
| Ctrl | 16/1 | 25.10 ± 8.50 | 23.80 ± 3.70 | 385.00 ± 81.00 | 414.72 ± 79.60 | 564.08 ± 981.86 | NA | ||||||||
| Zhao et al[19], 2015 | NA | Exp | 6 | 6 | No | No | No | No | 1/2 | 30.00 ± 4.50 | 49.00 ± 5.10 | 312.17 ± 89.19 | 466.36 ± 82.90 | 4376.27 ± 510.71 | 1648.96 ± 304.54 |
| Ctrl | 0/7 | 28.00 ± 4.90 | 39.00 ± 3.50 | 295.07 ± 46.87 | 334.27 ± 43.80 | 4701.76 ± 513.53 | 2835.09 ± 412.03 | ||||||||
| Patel et al[23], 2016 | NCT01670981 | Exp | 12 | 12 | Yes | No | No | No | 31/2 | 26.50 ± 5.10 | 28.10 ± 6.13 | 313.00 ± 100.00 | 370.62 ± 114.30 | 1755.00 ± 1842.00 | NA |
| Ctrl | 41/7 | 24.40 ± 6.00 | 25.30 ± 6.10 | 302.00 ± 105.00 | 353.43 ± 128.30 | 2132.00 ± 2021.00 | NA | ||||||||
| Butler et al[22], 2017 | NCT02467387 | Exp | 6 | 3 | No | No | Yes | No | 0/0 | 34.30 ± 7.91 | 34.10 ± 9.70 | NA | NA | 806.27 ± 1387.85 | 768.25 ± 2945.53 |
| Ctrl | 0/0 | 34.50 ± 7.49 | 36.70 ± 5.40 | NA | NA | NA | NA | ||||||||
| Xiao et al[29], 2017 | NA | Exp | 12 | 12 | Yes | No | No | Yes | 5/0 | 34.10 ± 3.600 | 41.00 ± 6.70 | 309.00 ± 84.70 | NA | 539.20 ± 213.60 | NA |
| Ctrl | 7/2 | 33.70 ± 4.00 | 34.30 ± 5.30 | 323.30 ± 89.40 | NA | 575.30 ± 207.60 | NA | ||||||||
| Florea et al[18], 2017 | NCT02013674 | Exp | 12 | 12 | Yes | Yes | No | No | 2/1 | 30.10 ± 8.80 | 33.10 ± 7.30 | 434.90 ± 120.00 | 463.00 ± 143.10 | 377.70 ± NA | NA |
| Ctrl | 3/0 | 37.60 ± 13.30 | 37.30 ± 13.00 | 398.70 ± 111.60 | 409.70 ± 130.20 | 532.30 ± NA | NA | ||||||||
| Yau et al[20], 2019 | NCT02362646 | Exp | 12 | 6 | Yes | No | No | No | 88/15 | 17.30 ± 5.80 | 19.00 ± 9.40 | NA | NA | NA | NA |
| Ctrl | 41/8 | 16.20 ± 6.00 | 17.60 ± 6.20 | NA | NA | NA | NA | ||||||||
| Bolli et al[26], 2021 | NCT02501811 | Exp | 12 | 12 | No | No | Yes | No | 19/5 | 29.23 ± 6.30 | 30.50 ± 6.90 | 367.72 ± 83.85 | 398.72 ± 93.10 | 1026.07 ± 2702.11 | 640.37 ± 1512.69 |
| Ctrl | 13/4 | 29.66 ± 6.18 | 29.40 ± 5.90 | 367.60 ± 85.60 | 384.88 ± 101.70 | 856.72 ± 1364.72 | 1072.32 ± 2161.64 | ||||||||
| Qayyum et al[28], 2023 | NCT03092284 | Exp | 12 | 6 | Yes | No | No | No | 21/3 | 34.20 ± 7.90 | 34.80 ± 5.80 | 388.00 ± 92.00 | 400.00 ± 86.10 | 1382.71 ± 1538.32 | 1850.22 ± 951.24 |
| Ctrl | 11/0 | 33.76 ± 2.70 | 33.80 ± 6.90 | 416.00 ± 121.00 | 447.87 ± 120.20 | 1283.77 ± 1206.81 | 1589.83 ± 543.70 | ||||||||
| Qayyum et al[28], 2023 | NCT02673164 | Exp | 12 | 6 | Yes | No | No | No | 26/3 | 31.60 ± 7.20 | 32.80 ± 7.50 | 419.00 ± 12.00 | 432.00 ± 13.00 | 1495.00 ± 2242.00 | 1607.00 ± 274.00 |
| Ctrl | 10/2 | 32.00 ± 8.90 | 34.70 ± 9.70 | 423.00 ± 18.00 | 451.00 ± 19 | 1828.00 ± 2376.00 | 1652.00 ± 595.00 | ||||||||
Table 3 summarizes the quality results of the twelve studies included in the meta-analysis. Using the Jadad scale risk of bias score ranging from 1-5 points, nine studies were of “high” quality (three studies scoring five points[23-25], two studies scoring four points[18,26], and four studies scoring three points each[20,21,27,28]. Three studies were considered “low” quality (one scoring two points[22], and two studies scoring one point each[19,29].
| Ref. | Trial registry | Jadad scale | Quality | |||
| R (0-2) | B (0-2) | D (0-1) | Total | |||
| Ascheim et al[21], 2014 | NCT01442129 | 1 | 1 | 1 | 3 | High |
| Perin et al[27], 2015 | NCT00721045 | 2 | 0 | 1 | 3 | High |
| Mathiasen et al[25], 2015 | NCT00644410 | 2 | 2 | 1 | 5 | High |
| Zhao et al[19], 2015 | NA | 1 | 0 | 0 | 1 | Low |
| Patel et al[23], 2016 | NCT01670981 | 2 | 2 | 1 | 5 | High |
| Butler et al[22], 2017 | NCT02467387 | 1 | 0 | 1 | 2 | Low |
| Xiao et al[29], 2017 | NA | 1 | 0 | 0 | 1 | Low |
| Florea et al[18], 2017 | NCT02013674 | 2 | 1 | 1 | 4 | High |
| Yau et al[20], 2019 | NCT02362646 | 2 | 0 | 1 | 3 | High |
| Bolli et al[26], 2021 | NCT02501811 | 1 | 2 | 1 | 4 | High |
| Qayyum et al[28], 2023 | NCT03092284 | 1 | 1 | 1 | 3 | High |
| Qayyum et al[28], 2023 | NCT02673164 | 2 | 2 | 1 | 5 | High |
The funnel plot (Supplementary Figure 1) depicts the visual assessment of publication bias, showing an apparent symmetric distribution across all study endpoints. Correspondingly, Egger’s test for small-study effects demonstrated no publication bias for death (P = 0.64), SAE (P = 0.99), LVEF (P = 0.33), 6MWD (P = 0.73), and pro-BNP (P = 0.31). Leave-one-out sensitivity analyses were performed for all endpoints, as shown in Supplementary Figure 2.
Death: Mortality was measured in all twelve RCTs included in the meta-analysis. As illustrated in Figure 2, a significant reduction in mortality rate was evident, and the result indicated a 45% reduction in mortality among patients treated with MSCs (RR: 0.55, 95%CI: 0.33-0.92, P = 0.02). However, subgroup analyses showed no significant mortality reduction across all the delivery routes. Leave-one-out sensitivity analysis showed a non-significant decrease in the risk of death when a study by either Perin et al[27], Zhao et al[19], or Patel et al[23] was omitted (Supplementary Figure 2). In addition, among the TESI subgroup, the risk of death was significantly reduced when a study by Florea et al[18] and Qayyum et al[28] was omitted (Supplementary Figure 3). The studies largely showed a low overall heterogeneity (I2 = 5.68%); within-subgroup heterogeneity between subgroups was low (I2 = 0.00%) apart from the TEPI route (I2 = 63.85%). The heterogeneity of the IV subgroup could not be analyzed across all study endpoints due to the availability of only one study in the subgroup.
SAEs: SAE analysis revealed no overall significant morbidity benefits (RR: 0.84, 95%CI: 0.66-1.05, P = 0.11) (Figure 3) with moderate heterogeneity (I2 = 59.08%). Subgroup analysis revealed a significant change in the incidence of SAEs among the TESI subgroup, favoring the intervention arm (RR: 0.71, 95%CI: 0.54-0.95, P = 0.04). Other delivery routes demonstrated no difference in the risk for SAEs. Within-subgroup heterogeneity was moderate in the TESI subgroup (I2 = 42.40%) and low in both TEPI and IC subgroups (I2 = 0.00% in both subgroups).
Functional outcomes (LVEF): All twelve RCTs have reported changes in LVEF compared to baseline. The imaging modalities used to measure the LV systolic performance included echocardiography (n = 9), cardiac computed tomography scan (n = 2), cardiac magnetic resonance (n = 3), and single-photon emission computed tomography (SPECT) (n = 2), as shown in Table 2. Four studies evaluated the LV functional outcome with multiple imaging modalities[20,27,29,30]. As illustrated in Figure 4, there was a significant increase in LVEF compared to baseline (WMD: 2.44%, 95%CI: 0.80-4.29, P ≤ 0.001) with significant overall heterogeneity (I2 = 96.62%). Further subgroup analysis revealed a significant increase only in the IC subgroup (WMD: 7.26%, 95%CI: 5.61-8.92, P ≤ 0.001). There was no significant improvement in different RoD subgroups, including TESI (WMD: 1.50%, 95%CI: -0.68-3.68), TEPI (WMD: 1.57%, 95%CI: -1.33-4.48), and IV routes (WMD: -2.40%, 95%CI: -11.49-6.69). There was a high within-subgroup heterogeneity in both TESI (I2 = 93.89%) and TEPI subgroups (I2 = 83.21%) and moderate heterogeneity in the IC subgroup (I2 = 41.88%).
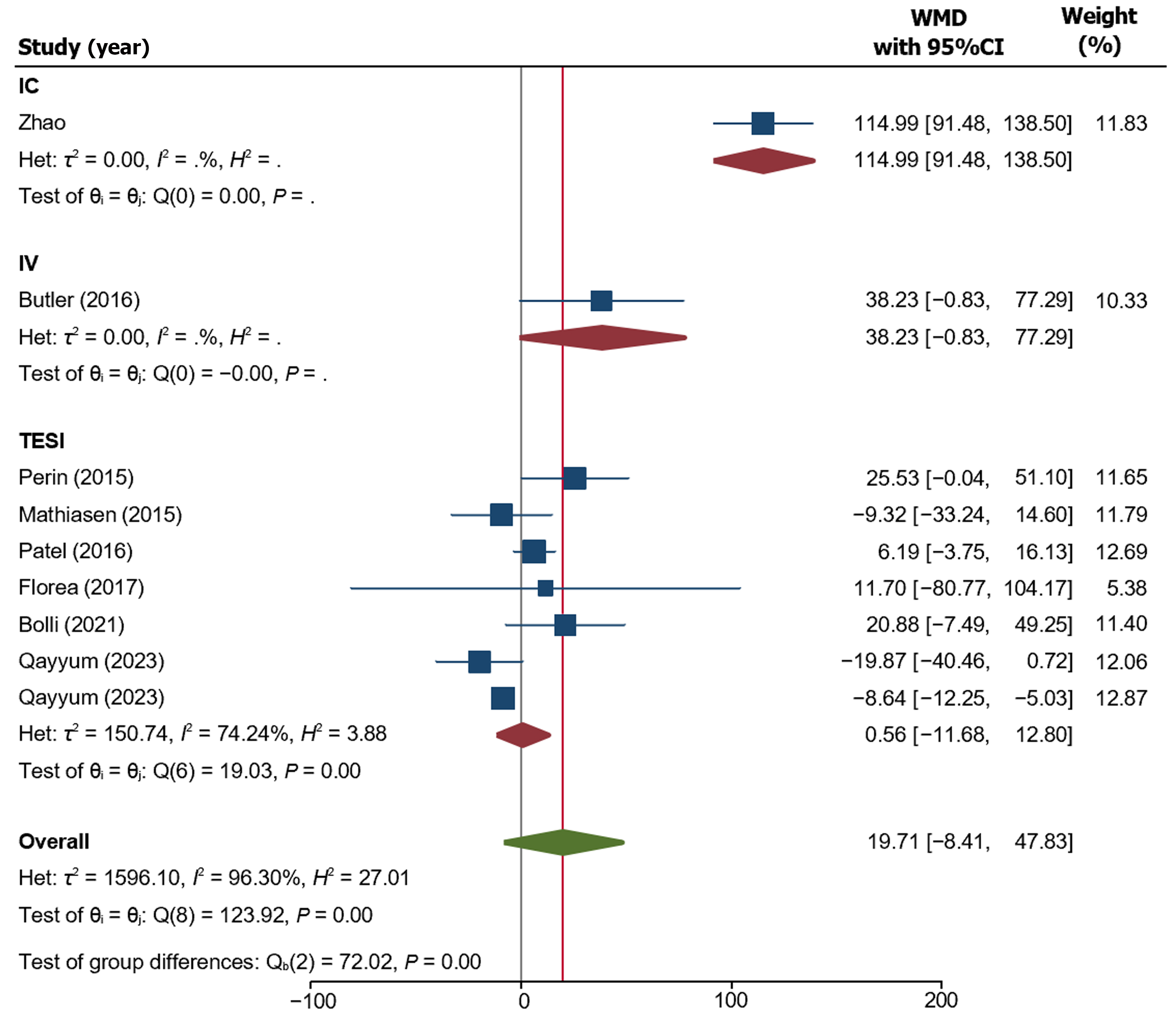
Clinical outcomes (6-minute walk distance): Only nine of the twelve studies assessed 6MWD as a clinical outcome parameter (Figure 5). Although Butler et al[22] did not report on baseline and follow-up 6MWD, they incorporated the changes in 6MWD in their study endpoints. Overall, there was no significant change in 6MWD (WMD: 19.71 m, 95%CI: -8.41-47.83, P = 0.17) with high heterogeneity across the studies (I2 = 96.30%). Among the subgroups, IC demonstrated a significant rise in 6MWD of 114.99 m (95%CI: 91.48-138.50, P ≤ 0.001). There was no significant increase among the IV (WMD: 38.23 m, 95%CI: -0.83-77.29, P = 0.05) and TESI subgroups (WMD: 0.56 m, 95%CI: -11.68-12.80, P ≥ 0.05). There were no studies within TEPI RoD reporting the 6MWD outcome. Within-subgroup heterogeneity revealed moderate heterogeneity among the TEPI subgroup (I2 = 74.24%), whereas both IC and IV subgroups were not assessed for heterogeneity because of single-study subgroups.
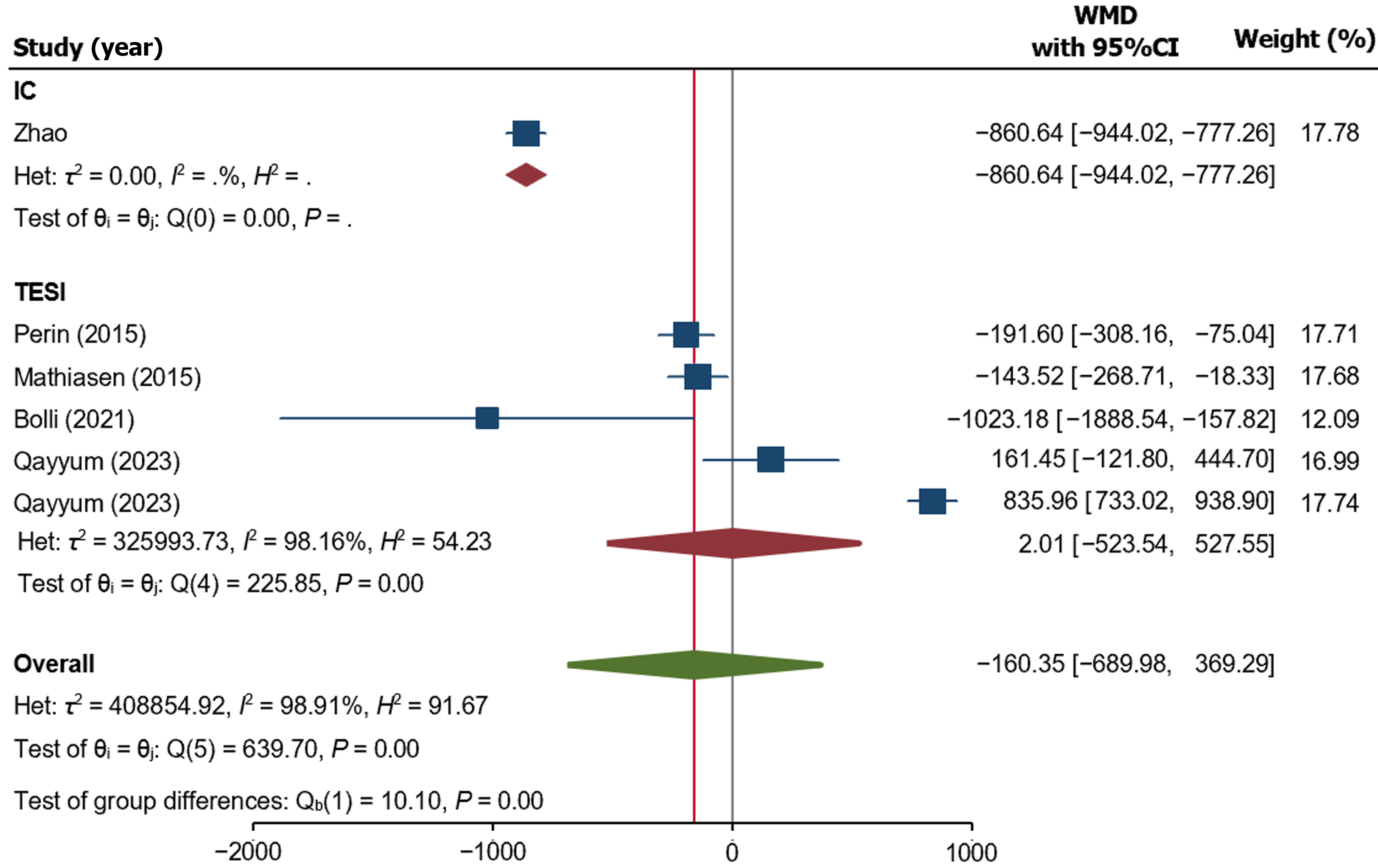
Biochemical outcome (pro-BNP Test): Only six studies assessed the biochemical outcome, i.e., pro-BNP, as displayed in Figure 6. There was no significant overall change in the pro-BNP level (WMD: -160.35 pg/mL, 95%CI: -689.98-369.29, P = 0.54) with high heterogeneity across the studies (I2 = 98.91%). Among subgroups, the IC delivery route significantly reduced the pro-BNP level (WMD = -860.64 pg/mL, 95%CI: -944.02 to -777.26, P value = 0.001). TESI significantly reduced the pro-BNP level among the subgroups (WMD: -860.64 pg/mL, 95%CI: -944.02 to -777.26, P value ≥ 0.05). Significant heterogeneity was found among the TESI subgroup (I2 = 98.91%).
The emergence of MSCs as living bio-drugs has given rise to unique challenges regarding RoD, as it remains a crucial determinant of their safety and efficacy in clinical settings. MSCs are distinct from routine pharmaceuticals in molecular weight, size, shape, and above all, being with a living status; they need to be administered such that they reach the target site, i.e., damaged myocardium, in large enough numbers with high viability, maintain their stemness and original phenotype and are retained at the injury site for long enough time to participate in the repair process with minimal off-target accumulation. Some commonly used RoD in the reported clinical studies encompass IM, IC, retrograde intracoronary (IC) sinus, IV, TESI, and scaffold-based delivery methods, each with advantages and limitations[16]. Our study provides a systematic review and meta-analysis of twelve published phase II RCTs to determine if different RoD affect the safety and efficacy of MSCs during HF treatment. The essential findings of the study are: (1) MSC-based treatment resulted in a significant reduction in all-cause mortality compared to the control; (2) there was no significant change in the incidence of SAEs depending upon the RoD; and (3) both TESI and IC injection yielded superior efficacy outcomes compared to other routes. We will discuss the effect of each RoD on MSC delivery in the following sections.
Though invasive, TEPI under direct vision as an adjunct to LVAD allows site-directed delivery of cells with a better retention rate. In our meta-analysis, however, two out of twelve studies used TEPI RoD without significantly reducing all-cause mortality and morbidity. Also, there was no significant improvement in LVEF, 6MWD, and pro-BNP levels compared to the baseline. These data contradict a meta-analysis by Soetisna et al[31], which reported an increase in the 6MWD in patients with ischemic heart disease treated. Nevertheless, apart from suggested efficacy limitations in our findings, one of the significant drawbacks to implementing the TEPI RoD is its invasive nature, which may also lead to perforation and arrhythmia. Therefore, this approach only offers superior advantages to other RoDs.
TESI RoD was our meta-analysis’s second most utilized RoD in seven of the twelve studies. TESI is one of the minimally invasive RoDs for site-directed implantation of cells using electromagnetic mapping. Our meta-analysis did not reveal a significant reduction in mortality but a significant overall morbidity reduction. The finding contradicted Gyöngyösi et al[30], who reported a significant reduction of all-cause mortality in their pooled analysis of eighteen studies. However, it was noteworthy that the heterogeneity of the TESI RoD subgroup was substantial across all study endpoints. As such, our study found a significant reduction in mortality when excluding a Danish phase II trial by Qayyum et al[28] among the TESI arm subgroup. In this study, the MSC-treated arm had 3 cases of death, whereas the control arm demonstrated no mortality. Nevertheless, the leave-one-out sensitivity analysis failed to demonstrate the efficacy benefits of the TESI route, including LVEF, pro-BNP, and 6MWD. Despite the early trials demonstrating a promising efficacy performance of the TESI route, the recent SCIENCE and Danish trials (2023) did not demonstrate improvement in any of the efficacy parameters[24,28]. As such, our findings contradicted an earlier meta-analysis by Fan et al[32], which found an improvement in LVEF among HF patients treated with MSC therapy using the TESI delivery route.
IC RoD is technically less invasive, safe, catheter-based, and easy to manipulate in cell delivery. Still, it may not be feasible for large-size cells like MSCs and high doses of cells, especially high-consistency cell preparations. IC route demonstrated insignificant pooled safety benefits, including all-cause mortality and SAEs. However, the IC route outperformed other RoD in all efficacy endpoints, including overall superiority in improving clinical, functional, and biochemical parameters. Our data supported the use of IC routes, consistent with data reported by Fan et al[32] that demonstrated the superiority of MSC-based therapy via IC RoD in improving exercise capacity in HF patients. Nevertheless, despite the seemingly encouraging findings, the pooled data in this study was considerably low (n = 96) compared to other RoDs, such as TESI and TEPI injections (n = 567 and n = 189, respectively). The low number of analyzed samples was also compounded by the low quality of RCTs (Jadad score of 1/5 in both studies).
The assessment of the IV RoD was limited due to the inclusion of only one RCT. This study had a relatively small sample size and scored low on the Jadad scale. The IV route showed no significant reduction in both mortality and morbidity. Unfortunately, the functional and biochemical outcomes were not reported, and the clinical outcomes of 6MWD were also insignificant. At the same time, other systematic reviews have noted an increase in clinical outcomes[32]. Studies did not find significant improvements in LVEF or mortality rate for cardiac patients[32,33]. The limited effectiveness of the IV route may be attributed to the low number of cells reaching the target site and the low cell retention rate associated with systemic delivery approaches[34]. Despite the simplicity and non-invasiveness of the IV route, the current evidence needs to be more comprehensive to support its use in HF patients.
Our meta-analysis implemented strenuous efforts in study design and data analysis to evaluate the optimal RoD for MSC-based therapy. We have also included MSCs from different tissue sources, in addition to biochemical parameters, i.e., pro-BNP, in efficacy outcome analysis. Most RCTs included scored high in the Jadad score (nine of the twelve studies), which reduced the risk of bias in each study and enhanced the quality of pooled evidence.
Despite our best endeavors, this study has limitations. Firstly, the analysis encompassed a small pool of RCTs, thus having a limited sample size. Also, specific relevant secondary outcomes were not analyzed, such as health-related quality of life, hospital readmission, performance status (NYHA classification), and various cardiac function indices (e.g., wall motion score, LV end-systolic and diastolic volume, etc.) primarily due to lack of data availability. Notwithstanding these constraints, we thoroughly compared MSC-based therapy RoD for HF using the accessible evidence. From a practical standpoint, using IC routes can be an attractive choice, given the efficacy, superiority, and feasibility of a minimally invasive approach compared to TEPI[35]. Animal studies have also demonstrated an excellent cardiac retention rate using IC compared to TESI and IV RoD[36]. However, there is a potential risk of emboli, microinfarction, and inaccessibility due to the diseased coronary arteries[37,38]. Hence, the findings in this study need cautious interpretation, and we suggest analyzing phase II/III and III RCTs in the future to provide more substantial evidence to support their clinical application.
In conclusion, this study establishes the safety of IM, IC, IV, and TESI for MSC-based therapy based on pooled available data in phase II RCTs. In addition, IC and TESI routes provided superior outcomes compared to other routes in improving clinical, functional, and biochemical outcomes. These data in the early phase RCTs provide evidence that warrants investigations in phase II/III and phase III clinical trials before their implementation in clinical practice.
| 1. | Tsao CW, Aday AW, Almarzooq ZI, Alonso A, Beaton AZ, Bittencourt MS, Boehme AK, Buxton AE, Carson AP, Commodore-Mensah Y, Elkind MSV, Evenson KR, Eze-Nliam C, Ferguson JF, Generoso G, Ho JE, Kalani R, Khan SS, Kissela BM, Knutson KL, Levine DA, Lewis TT, Liu J, Loop MS, Ma J, Mussolino ME, Navaneethan SD, Perak AM, Poudel R, Rezk-Hanna M, Roth GA, Schroeder EB, Shah SH, Thacker EL, VanWagner LB, Virani SS, Voecks JH, Wang NY, Yaffe K, Martin SS. Heart Disease and Stroke Statistics-2022 Update: A Report From the American Heart Association. Circulation. 2022;145:e153-e639. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2995] [Cited by in RCA: 3638] [Article Influence: 909.5] [Reference Citation Analysis (0)] |
| 2. | Marín-García J. Cell death in the pathogenesis and progression of heart failure. Heart Fail Rev. 2016;21:117-121. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 3. | Hooper K, Hmeljak J. Disease Models & Mechanisms helps move heart failure to heart success. Dis Model Mech. 2022;15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 4. | Becher PM, Jugdutt BI, Baugh J, Schmack B. Experimental Heart Failure Models and Their Pathophysiological Characterization. Biomed Res Int. 2016;2016:2538263. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 5. | Kalou Y, Al-Khani AM, Haider KH. Bone Marrow Mesenchymal Stem Cells for Heart Failure Treatment: A Systematic Review and Meta-Analysis. Heart Lung Circ. 2023;32:870-880. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 23] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 6. | Al-khani AM, Khalifa MA, Haider KH. Mesenchymal Stem Cells for Cardiac Repair. In: Haider KH, editors. Handbook of Stem Cell Therapy. Singapore: Springer, 2022: 1-53. [DOI] [Full Text] |
| 7. | Hamano K, Nishida M, Hirata K, Mikamo A, Li TS, Harada M, Miura T, Matsuzaki M, Esato K. Local implantation of autologous bone marrow cells for therapeutic angiogenesis in patients with ischemic heart disease: clinical trial and preliminary results. Jpn Circ J. 2001;65:845-847. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 245] [Cited by in RCA: 224] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 8. | Rodríguez-Fuentes DE, Fernández-Garza LE, Samia-Meza JA, Barrera-Barrera SA, Caplan AI, Barrera-Saldaña HA. Mesenchymal Stem Cells Current Clinical Applications: A Systematic Review. Arch Med Res. 2021;52:93-101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 247] [Article Influence: 41.2] [Reference Citation Analysis (0)] |
| 9. | Teerlink JR, Metra M, Filippatos GS, Davison BA, Bartunek J, Terzic A, Gersh BJ, Povsic TJ, Henry TD, Alexandre B, Homsy C, Edwards C, Seron A, Wijns W, Cotter G; CHART Investigators. Benefit of cardiopoietic mesenchymal stem cell therapy on left ventricular remodelling: results from the Congestive Heart Failure Cardiopoietic Regenerative Therapy (CHART-1) study. Eur J Heart Fail. 2017;19:1520-1529. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 83] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 10. | Perin EC, Borow KM, Henry TD, Mendelsohn FO, Miller LW, Swiggum E, Adler ED, Chang DH, Fish RD, Bouchard A, Jenkins M, Yaroshinsky A, Hayes J, Rutman O, James CW, Rose E, Itescu S, Greenberg B. Randomized Trial of Targeted Transendocardial Mesenchymal Precursor Cell Therapy in Patients With Heart Failure. J Am Coll Cardiol. 2023;81:849-863. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 65] [Article Influence: 21.7] [Reference Citation Analysis (0)] |
| 11. | Bartunek J, Terzic A, Davison BA, Behfar A, Sanz-Ruiz R, Wojakowski W, Sherman W, Heyndrickx GR, Metra M, Filippatos GS, Waldman SA, Teerlink JR, Henry TD, Gersh BJ, Hajjar R, Tendera M, Senger S, Cotter G, Povsic TJ, Wijns W; CHART Program. Cardiopoietic stem cell therapy in ischaemic heart failure: long-term clinical outcomes. ESC Heart Fail. 2020;7:3345-3354. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 26] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 12. | Karantalis V, DiFede DL, Gerstenblith G, Pham S, Symes J, Zambrano JP, Fishman J, Pattany P, McNiece I, Conte J, Schulman S, Wu K, Shah A, Breton E, Davis-Sproul J, Schwarz R, Feigenbaum G, Mushtaq M, Suncion VY, Lardo AC, Borrello I, Mendizabal A, Karas TZ, Byrnes J, Lowery M, Heldman AW, Hare JM. Autologous mesenchymal stem cells produce concordant improvements in regional function, tissue perfusion, and fibrotic burden when administered to patients undergoing coronary artery bypass grafting: The Prospective Randomized Study of Mesenchymal Stem Cell Therapy in Patients Undergoing Cardiac Surgery (PROMETHEUS) trial. Circ Res. 2014;114:1302-1310. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 249] [Cited by in RCA: 269] [Article Influence: 22.4] [Reference Citation Analysis (0)] |
| 13. | Attar A, Monabati A, Montaseri M, Vosough M, Hosseini SA, Kojouri J, Abdi-Ardekani A, Izadpanah P, Azarpira N, Pouladfar G, Ramzi M. Transplantation of mesenchymal stem cells for prevention of acute myocardial infarction induced heart failure: study protocol of a phase III randomized clinical trial (Prevent-TAHA8). Trials. 2022;23:632. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 14. | Borow KM, Yaroshinsky A, Greenberg B, Perin EC. Phase 3 DREAM-HF Trial of Mesenchymal Precursor Cells in Chronic Heart Failure. Circ Res. 2019;125:265-281. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 52] [Cited by in RCA: 60] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 15. | Kanelidis AJ, Premer C, Lopez J, Balkan W, Hare JM. Route of Delivery Modulates the Efficacy of Mesenchymal Stem Cell Therapy for Myocardial Infarction: A Meta-Analysis of Preclinical Studies and Clinical Trials. Circ Res. 2017;120:1139-1150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 139] [Article Influence: 13.9] [Reference Citation Analysis (0)] |
| 16. | Kalou YMN, Hashemi ASA, Joudeh RM, Aramini B, Haider KH. Mesenchymal Stem Cell-Based Heart Cell Therapy: The Effect of Route of Cell Delivery in the Clinical Perspective. In: Haider KH, editor. Stem cells: From Potential to Promise. Singapore: Springer, 2021: 151-190. [DOI] [Full Text] |
| 17. | Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, McQuay HJ. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17:1-12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12275] [Cited by in RCA: 13045] [Article Influence: 434.8] [Reference Citation Analysis (3)] |
| 18. | Florea V, Rieger AC, DiFede DL, El-Khorazaty J, Natsumeda M, Banerjee MN, Tompkins BA, Khan A, Schulman IH, Landin AM, Mushtaq M, Golpanian S, Lowery MH, Byrnes JJ, Hendel RC, Cohen MG, Valasaki K, Pujol MV, Ghersin E, Miki R, Delgado C, Abuzeid F, Vidro-Casiano M, Saltzman RG, DaFonseca D, Caceres LV, Ramdas KN, Mendizabal A, Heldman AW, Mitrani RD, Hare JM. Dose Comparison Study of Allogeneic Mesenchymal Stem Cells in Patients With Ischemic Cardiomyopathy (The TRIDENT Study). Circ Res. 2017;121:1279-1290. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 162] [Article Influence: 18.0] [Reference Citation Analysis (0)] |
| 19. | Zhao XF, Xu Y, Zhu ZY, Gao CY, Shi YN. Clinical observation of umbilical cord mesenchymal stem cell treatment of severe systolic heart failure. Genet Mol Res. 2015;14:3010-3017. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 47] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 20. | Yau TM, Pagani FD, Mancini DM, Chang HL, Lala A, Woo YJ, Acker MA, Selzman CH, Soltesz EG, Kern JA, Maltais S, Charbonneau E, Pan S, Marks ME, Moquete EG, O'Sullivan KL, Taddei-Peters WC, McGowan LK, Green C, Rose EA, Jeffries N, Parides MK, Weisel RD, Miller MA, Hung J, O'Gara PT, Moskowitz AJ, Gelijns AC, Bagiella E, Milano CA; Cardiothoracic Surgical Trials Network. Intramyocardial Injection of Mesenchymal Precursor Cells and Successful Temporary Weaning From Left Ventricular Assist Device Support in Patients With Advanced Heart Failure: A Randomized Clinical Trial. JAMA. 2019;321:1176-1186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 76] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 21. | Ascheim DD, Gelijns AC, Goldstein D, Moye LA, Smedira N, Lee S, Klodell CT, Szady A, Parides MK, Jeffries NO, Skerrett D, Taylor DA, Rame JE, Milano C, Rogers JG, Lynch J, Dewey T, Eichhorn E, Sun B, Feldman D, Simari R, O'Gara PT, Taddei-Peters WC, Miller MA, Naka Y, Bagiella E, Rose EA, Woo YJ. Mesenchymal precursor cells as adjunctive therapy in recipients of contemporary left ventricular assist devices. Circulation. 2014;129:2287-2296. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 122] [Cited by in RCA: 130] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 22. | Butler J, Epstein SE, Greene SJ, Quyyumi AA, Sikora S, Kim RJ, Anderson AS, Wilcox JE, Tankovich NI, Lipinski MJ, Ko YA, Margulies KB, Cole RT, Skopicki HA, Gheorghiade M. Intravenous Allogeneic Mesenchymal Stem Cells for Nonischemic Cardiomyopathy: Safety and Efficacy Results of a Phase II-A Randomized Trial. Circ Res. 2017;120:332-340. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 138] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 23. | Patel AN, Henry TD, Quyyumi AA, Schaer GL, Anderson RD, Toma C, East C, Remmers AE, Goodrich J, Desai AS, Recker D, DeMaria A; ixCELL-DCM Investigators. Ixmyelocel-T for patients with ischaemic heart failure: a prospective randomised double-blind trial. Lancet. 2016;387:2412-2421. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 134] [Article Influence: 13.4] [Reference Citation Analysis (0)] |
| 24. | Qayyum AA, van Klarenbosch B, Frljak S, Cerar A, Poglajen G, Traxler-Weidenauer D, Nadrowski P, Paitazoglou C, Vrtovec B, Bergmann MW, Chamuleau SAJ, Wojakowski W, Gyöngyösi M, Kraaijeveld A, Hansen KS, Vrangbaek K, Jørgensen E, Helqvist S, Joshi FR, Johansen EM, Follin B, Juhl M, Højgaard LD, Mathiasen AB, Ekblond A, Haack-Sørensen M, Kastrup J; SCIENCE Investigators. Effect of allogeneic adipose tissue-derived mesenchymal stromal cell treatment in chronic ischaemic heart failure with reduced ejection fraction - the SCIENCE trial. Eur J Heart Fail. 2023;25:576-587. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 38] [Reference Citation Analysis (0)] |
| 25. | Mathiasen AB, Qayyum AA, Jørgensen E, Helqvist S, Fischer-Nielsen A, Kofoed KF, Haack-Sørensen M, Ekblond A, Kastrup J. Bone marrow-derived mesenchymal stromal cell treatment in patients with severe ischaemic heart failure: a randomized placebo-controlled trial (MSC-HF trial). Eur Heart J. 2015;36:1744-1753. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 209] [Cited by in RCA: 249] [Article Influence: 22.6] [Reference Citation Analysis (0)] |
| 26. | Bolli R, Mitrani RD, Hare JM, Pepine CJ, Perin EC, Willerson JT, Traverse JH, Henry TD, Yang PC, Murphy MP, March KL, Schulman IH, Ikram S, Lee DP, O'Brien C, Lima JA, Ostovaneh MR, Ambale-Venkatesh B, Lewis G, Khan A, Bacallao K, Valasaki K, Longsomboon B, Gee AP, Richman S, Taylor DA, Lai D, Sayre SL, Bettencourt J, Vojvodic RW, Cohen ML, Simpson L, Aguilar D, Loghin C, Moyé L, Ebert RF, Davis BR, Simari RD; Cardiovascular Cell Therapy Research Network (CCTRN). A Phase II study of autologous mesenchymal stromal cells and c-kit positive cardiac cells, alone or in combination, in patients with ischaemic heart failure: the CCTRN CONCERT-HF trial. Eur J Heart Fail. 2021;23:661-674. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 117] [Article Influence: 23.4] [Reference Citation Analysis (0)] |
| 27. | Perin EC, Borow KM, Silva GV, DeMaria AN, Marroquin OC, Huang PP, Traverse JH, Krum H, Skerrett D, Zheng Y, Willerson JT, Itescu S, Henry TD. A Phase II Dose-Escalation Study of Allogeneic Mesenchymal Precursor Cells in Patients With Ischemic or Nonischemic Heart Failure. Circ Res. 2015;117:576-584. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 145] [Cited by in RCA: 155] [Article Influence: 14.1] [Reference Citation Analysis (0)] |
| 28. | Qayyum AA, Mouridsen M, Nilsson B, Gustafsson I, Schou M, Nielsen OW, Hove JD, Mathiasen AB, Jørgensen E, Helqvist S, Joshi FR, Johansen EM, Follin B, Juhl M, Højgaard LD, Haack-Sørensen M, Ekblond A, Kastrup J. Danish phase II trial using adipose tissue derived mesenchymal stromal cells for patients with ischaemic heart failure. ESC Heart Fail. 2023;10:1170-1183. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 34] [Reference Citation Analysis (0)] |
| 29. | Xiao W, Guo S, Gao C, Dai G, Gao Y, Li M, Wang X, Hu D. A Randomized Comparative Study on the Efficacy of Intracoronary Infusion of Autologous Bone Marrow Mononuclear Cells and Mesenchymal Stem Cells in Patients With Dilated Cardiomyopathy. Int Heart J. 2017;58:238-244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 34] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 30. | Gyöngyösi M, Pokushalov E, Romanov A, Perin E, Hare JM, Kastrup J, Fernández-Avilés F, Sanz-Ruiz R, Mathur A, Wojakowski W, Martin-Rendon E, Pavo N, Pavo IJ, Hemetsberger R, Traxler D, Spannbauer A, Haller PM. Meta-Analysis of Percutaneous Endomyocardial Cell Therapy in Patients with Ischemic Heart Failure by Combination of Individual Patient Data (IPD) of ACCRUE and Publication-Based Aggregate Data. J Clin Med. 2022;11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 31. | Soetisna TW, Thamrin AMH, Permadijana D, Ramadhani ANE, Sugisman, Santoso A, Mansyur M. Intramyocardial Stem Cell Transplantation during Coronary Artery Bypass Surgery Safely Improves Cardiac Function: Meta-Analysis of 20 Randomized Clinical Trials. J Clin Med. 2023;12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 32. | Fan M, Huang Y, Chen Z, Xia Y, Chen A, Lu D, Wu Y, Zhang N, Qian J. Efficacy of mesenchymal stem cell therapy in systolic heart failure: a systematic review and meta-analysis. Stem Cell Res Ther. 2019;10:150. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 42] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 33. | Lalu MM, Mazzarello S, Zlepnig J, Dong YYR, Montroy J, McIntyre L, Devereaux PJ, Stewart DJ, David Mazer C, Barron CC, McIsaac DI, Fergusson DA. Safety and Efficacy of Adult Stem Cell Therapy for Acute Myocardial Infarction and Ischemic Heart Failure (SafeCell Heart): A Systematic Review and Meta-Analysis. Stem Cells Transl Med. 2018;7:857-866. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 70] [Cited by in RCA: 107] [Article Influence: 13.4] [Reference Citation Analysis (0)] |
| 34. | Caplan H, Olson SD, Kumar A, George M, Prabhakara KS, Wenzel P, Bedi S, Toledano-Furman NE, Triolo F, Kamhieh-Milz J, Moll G, Cox CS Jr. Mesenchymal Stromal Cell Therapeutic Delivery: Translational Challenges to Clinical Application. Front Immunol. 2019;10:1645. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 183] [Cited by in RCA: 224] [Article Influence: 32.0] [Reference Citation Analysis (0)] |
| 35. | Ishikawa K. Intracoronary injection of large stem cells: size matters. Circ Cardiovasc Interv. 2015;8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 12] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 36. | Freyman T, Polin G, Osman H, Crary J, Lu M, Cheng L, Palasis M, Wilensky RL. A quantitative, randomized study evaluating three methods of mesenchymal stem cell delivery following myocardial infarction. Eur Heart J. 2006;27:1114-1122. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 462] [Cited by in RCA: 461] [Article Influence: 23.1] [Reference Citation Analysis (0)] |
| 37. | Vulliet PR, Greeley M, Halloran SM, MacDonald KA, Kittleson MD. Intra-coronary arterial injection of mesenchymal stromal cells and microinfarction in dogs. Lancet. 2004;363:783-784. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 352] [Cited by in RCA: 331] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 38. | Suzuki K, Brand NJ, Smolenski RT, Jayakumar J, Murtuza B, Yacoub MH. Development of a novel method for cell transplantation through the coronary artery. Circulation. 2000;102:III359-III364. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 28] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/