©The Author(s) 2025.
World J Cardiol. Oct 26, 2025; 17(10): 107750
Published online Oct 26, 2025. doi: 10.4330/wjc.v17.i10.107750
Published online Oct 26, 2025. doi: 10.4330/wjc.v17.i10.107750
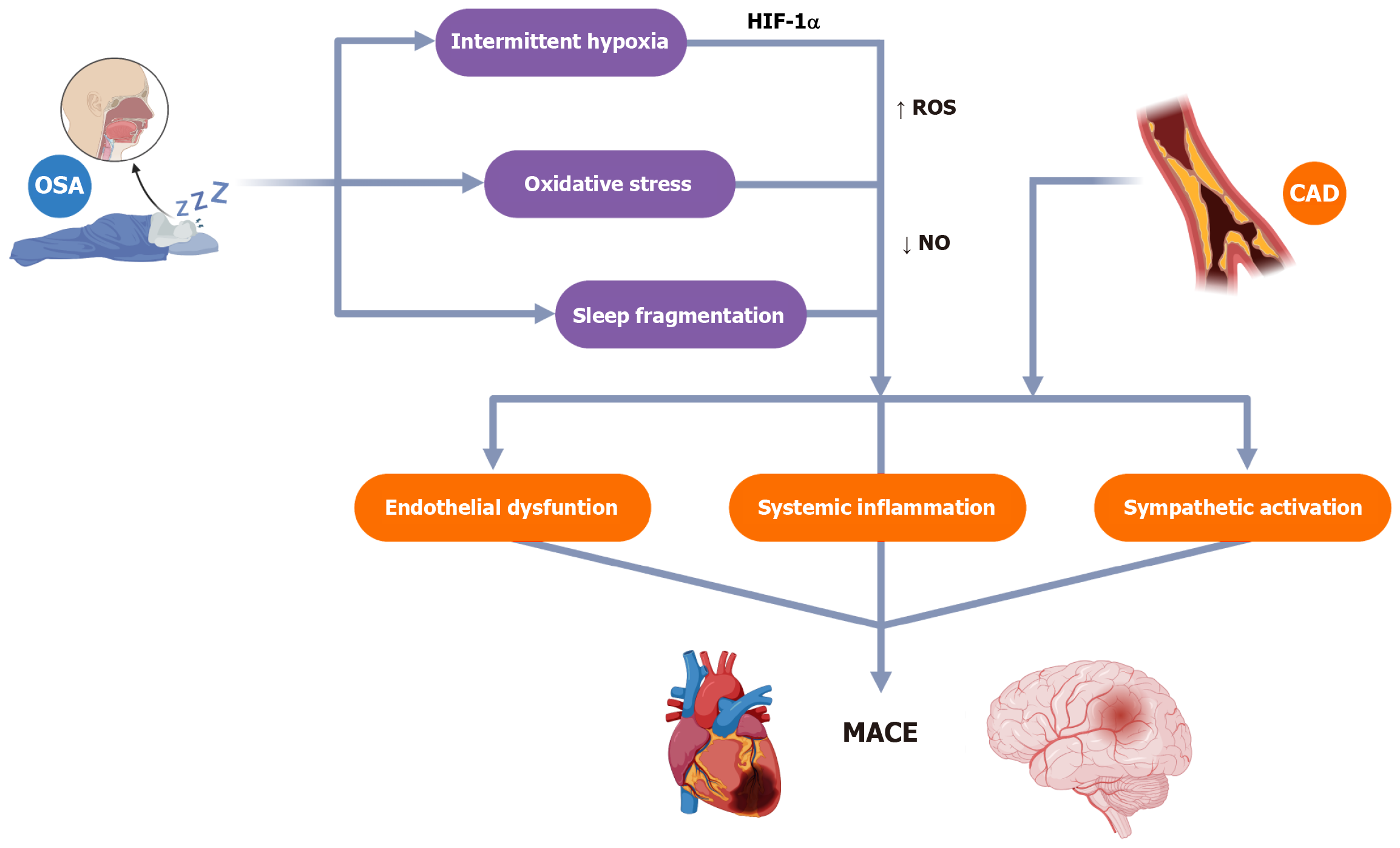
Figure 1 Cardiovascular consequences of obstructive sleep apnea.
CAD: Coronary artery disease; MACE: Major adverse cardiac events; NO: Nitric oxide; HIF-1α: Hypoxia-inducible factor 1-alpha; OSA: Obstructive sleep apnoea; ROS: Reactive oxygen species.
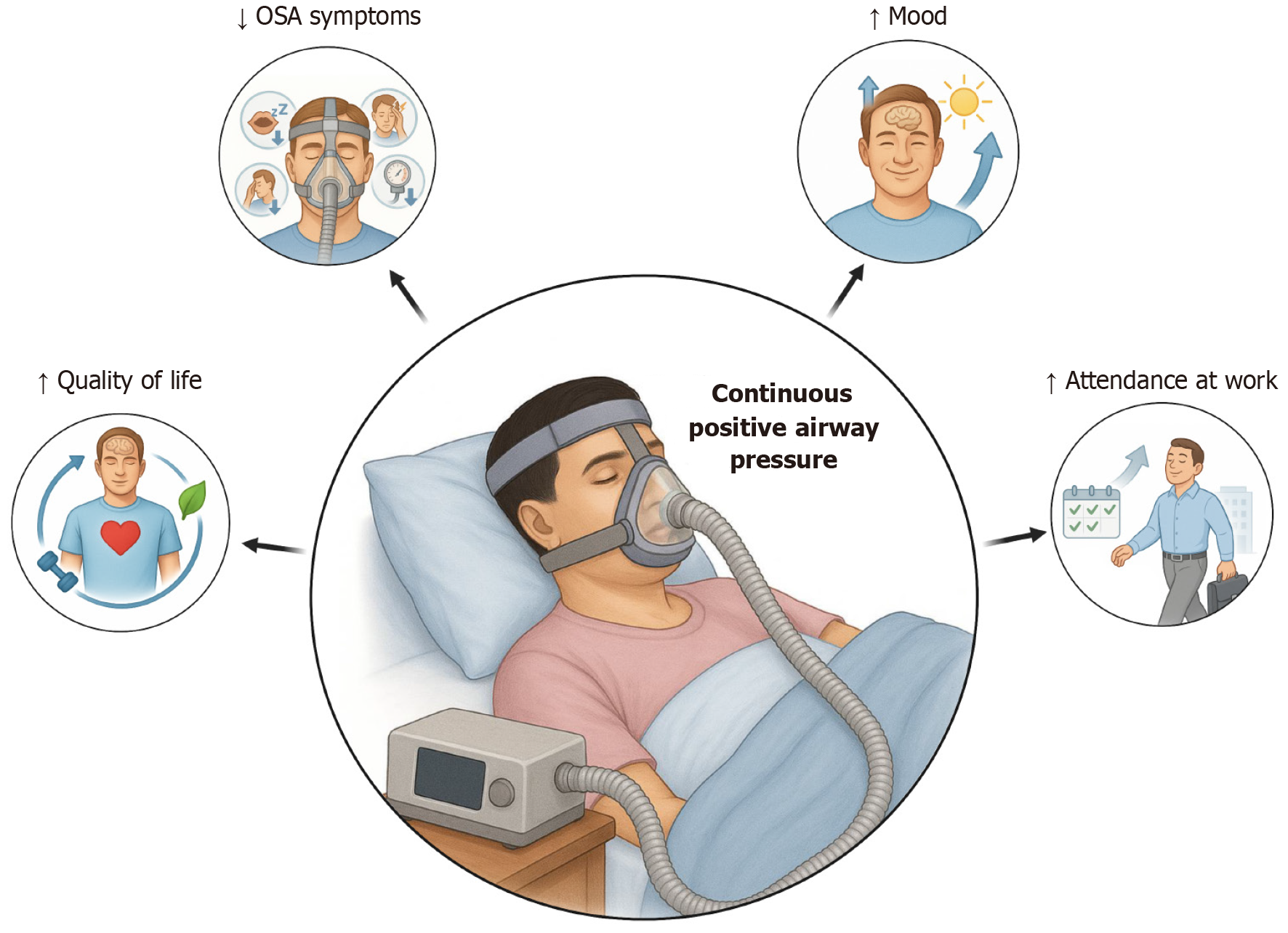
Figure 2 Clinical impact of continuous positive airway pressure therapy in patients with obstructive sleep apnea.
OSA: Obstructive sleep apnea.
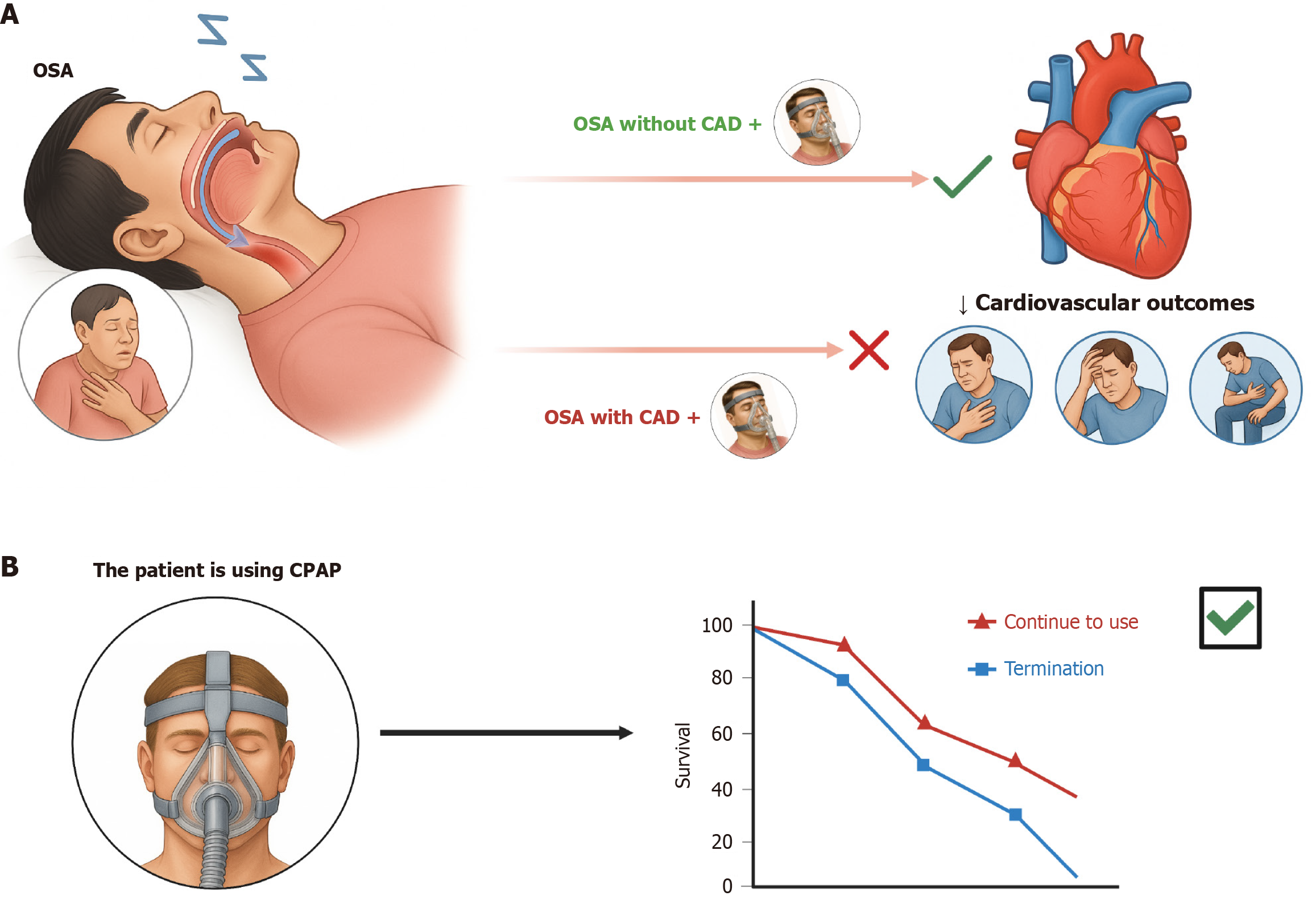
Figure 3 Impact of continuous positive airway pressure therapy on clinical outcomes in patients with obstructive sleep apnea.
A: In patients with obstructive sleep apnea without established coronary artery disease (CAD), continuous positive airway pressure (CPAP) therapy reduces the risk of future cardiovascular events. However, in those with preexisting CAD, the prognostic benefit of CPAP remains unproven despite the physiological rationale; B: Among patients already receiving CPAP therapy, continuation is associated with improved survival compared with treatment discontinuation, highlighting the importance of long-term adherence in optimizing patient outcomes. CPAP: Continuous positive airway pressure; CAD: Coronary artery disease; OSA: Obstructive sleep apnea.
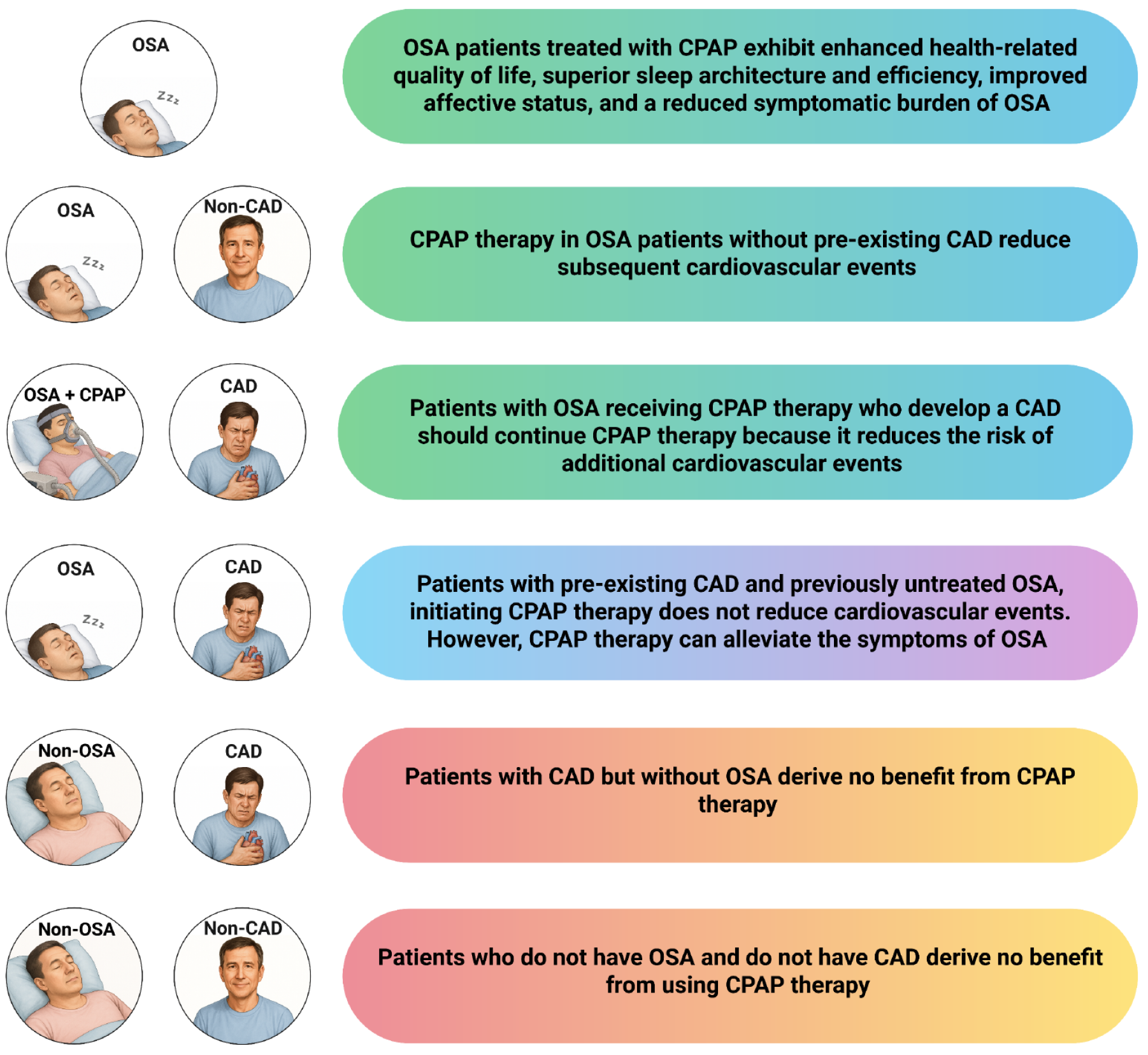
Figure 4 Impact of continuous positive airway pressure therapy on cardiovascular outcomes and symptom relief across different obstructive sleep apnea and cardiovascular disease patient profiles.
CPAP: Continuous positive airway pressure; CVD: Cardiovascular disease; OSA: Obstructive sleep apnea.
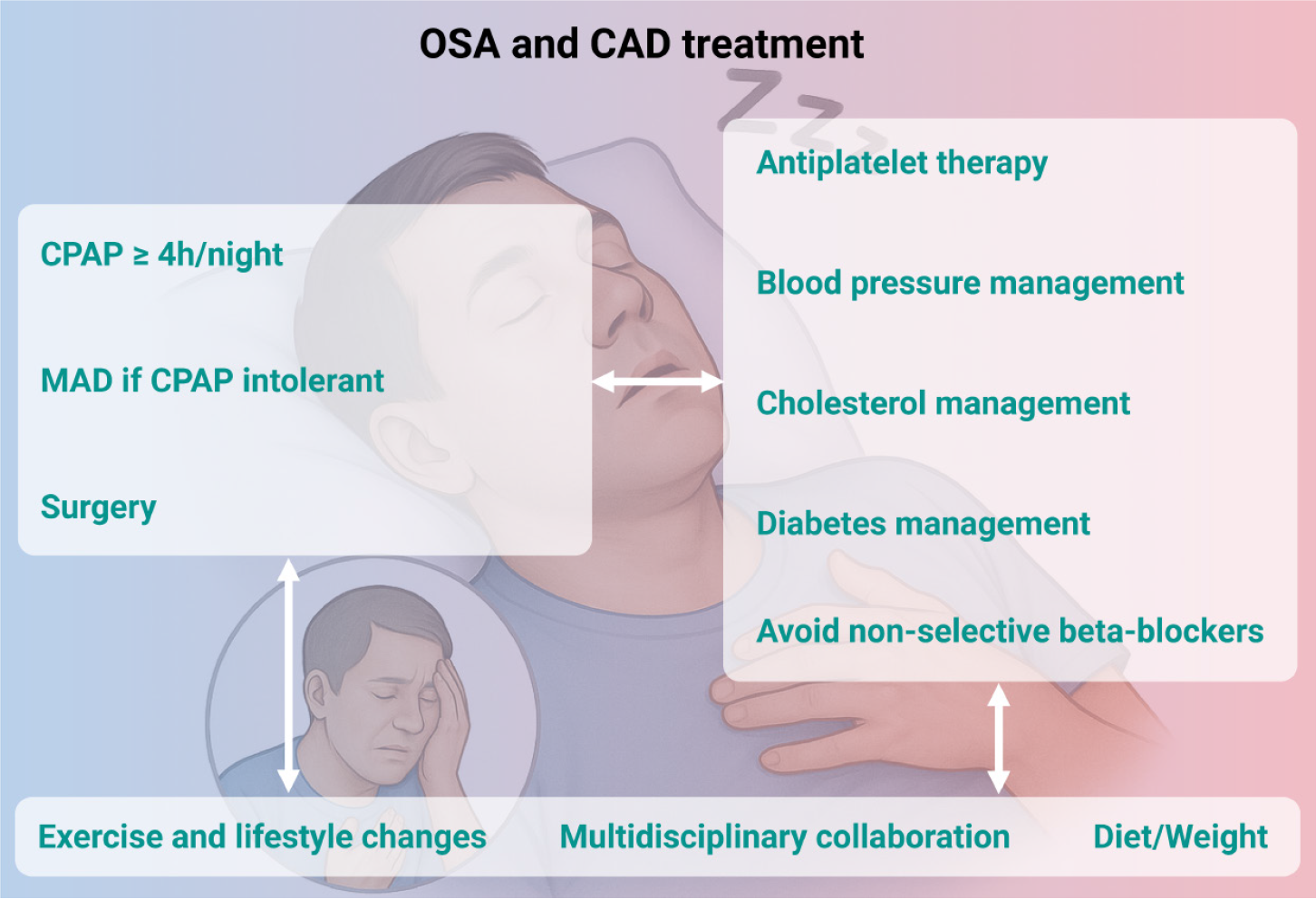
Figure 5 Integrated therapeutic strategies for managing patients with comorbid obstructive sleep apnea and coronary artery disease.
Effective treatment of obstructive sleep apnea (OSA)–coronary artery disease overlap requires a dual-pronged approach targeting both conditions. Management of OSA includes consistent use of continuous positive airway pressure (CPAP) therapy for ≥ 4 hours per night, with mandibular advancement devices or upper airway surgery considered in cases of CPAP intolerance. Cardiovascular risk factors should be concurrently addressed through antiplatelet therapy, blood pressure control, lipid and glucose management, and avoidance of non-selective beta-blockers. Lifestyle interventions—including diet, weight control, and physical activity—are essential to optimize long-term outcomes. Multidisciplinary collaboration further reinforces the effectiveness and sustainability of integrated care. CAD: Coronary artery disease; CPAP: Continuous positive airway pressure; OSA: Obstructive sleep apnea; MAD: Mandibular advancement devices.
- Citation: Luong TV, Hoang TA, Tran DH, Pham NNK, Nguyen HC, Le NHN, Dang HNN. Continuous positive airway pressure therapy for patients with obstructive sleep apnea and coronary artery disease. World J Cardiol 2025; 17(10): 107750
- URL: https://www.wjgnet.com/1949-8462/full/v17/i10/107750.htm
- DOI: https://dx.doi.org/10.4330/wjc.v17.i10.107750