Published online Jan 27, 2026. doi: 10.4240/wjgs.v18.i1.112927
Revised: October 23, 2025
Accepted: November 26, 2025
Published online: January 27, 2026
Processing time: 165 Days and 1.3 Hours
Intestinal obstruction, characterized by the impaired transit of intestinal contents due to various etiologies, constitutes a prevalent surgical emergency. In certain cases, surgical intervention becomes imperative, wherein intraoperative intestinal decompression is frequently necessitated. Ensuring effective decompression while minimizing contamination of the operative field constitutes a pivotal step that ex
To assess the clinical efficacy of cannula-assisted decompression techniques em
A retrospective cohort analysis of 70 patients diagnosed with small bowel obs
The cannula-assisted group exhibited statistically significant advantages over the conventional decompression group in terms of reduced operative duration for in
The application of cannula-assisted decompression techniques effectively facilitates intraoperative decompression of the small intestine, reduces procedural duration, mitigates surgical field contamination, and expedites post
Core Tip: This study introduces a standardized closed negative-pressure double-cannula technique for intraoperative decompression in small bowel obstruction. Compared to conventional enterotomy, this method was associated with a signi
- Citation: Zhang Q, He XH, Liu X, Ling XJ, Zhang YM. Application of a novel small intestine decompression method in patients with intestinal obstruction: A retrospective cohort study. World J Gastrointest Surg 2026; 18(1): 112927
- URL: https://www.wjgnet.com/1948-9366/full/v18/i1/112927.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v18.i1.112927
Intestinal obstruction is recognized as one of the frequently encountered acute abdominal conditions in surgical practice[1]. Clinically, it manifests as abdominal pain, distension, vomiting, and the absence of flatus and defecation. Radiological evaluations typically reveal intraluminal gas and fluid accumulation, bowel dilation, and edematous changes. In cases where conservative measures such as fasting and gastrointestinal decompression prove ineffective, surgical intervention becomes necessary. During operative management, enterotomy-based decompression is often employed to evacuate intestinal contents, reduce intraluminal pressure, relieve bowel wall edema, and facilitate the restoration of intestinal motility[2-4]. Conventionally, this technique entails a longitudinal incision made in the distal segment of the obstructed bowel, with the contents expressed into an open container. However, this method readily results in contamination of the operative field, thereby heightening the risk of postoperative infection and potentially compromising surgical success[5]. Additionally, the release of malodorous intestinal contents can significantly deteriorate the operating room environment and impose considerable discomfort on the surgical team[6].
In this context, a perforated cannula aspirator was adapted to facilitate the evacuation of intestinal contents via negative pressure suction, thereby ensuring effective intestinal decompression and minimizing contamination of the operative field. This retrospective cohort study aimed to compare the intraoperative and postoperative outcomes of a novel closed negative-pressure cannula decompression technique and conventional open enterotomy decompression in patients undergoing surgery for small bowel obstruction. We hypothesized that the cannula technique would be associated with a lower incidence of surgical field contamination, a reduced rate of surgical site infection (SSI), and a shorter intestinal decompression time.
A retrospective cohort analysis of 70 cases with small bowel obstruction admitted to the Department of General Surgery, Anqing Municipal Hospital between January 2023 and November 2024 was performed. Of these patients, 33 underwent conventional small intestine enterotomy decompression (control group), whereas 37 received small intestine enterotomy combined with cannula decompression (cannula group) (Supplementary material).
Inclusion criteria: (1) Adherence to diagnostic and treatment guidelines for intestinal obs
Exclusion criteria: (1) Severe organic comorbidities precluding surgical intervention; (2) Absence of intraoperative need for intestinal decompression due to alternative surgical findings; and (3) Presence of colonic obstruction.
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Declaration of Helsinki 1964 and later versions. This study was approved by the Ethics Committee of Anqing Municipal Hospital. Informed consent was obtained from all patients en
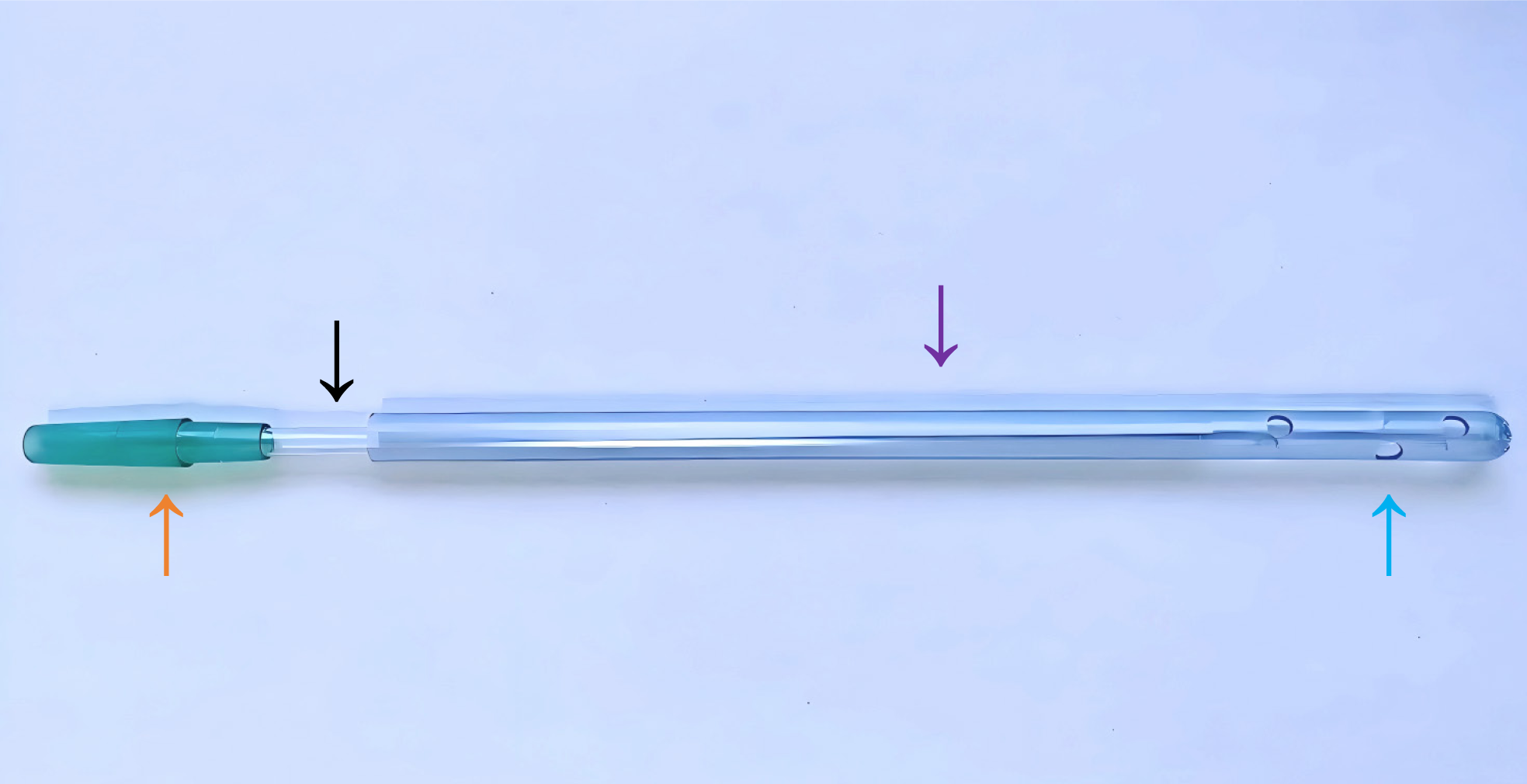
The device consists of two medical-grade polyvinyl chloride tubes of differing diameters and is designed for single use. The outer tube, measuring 2 cm in diameter, features multiple side perforations at its distal end, which serve to evenly distribute suction force and permit the entry of intestinal contents. The decompression function remains operative even when partial occlusion of the side perforations occurs. The inner tube, with a diameter of 1.5 cm, is designed with a tail end that may be connected to a negative pressure suction tube, enabling convenient replacement. An air inlet is formed at the junction between the inner and outer tubes (Figure 1).
Surgical field contamination was defined as the spillage of intestinal contents into the peritoneal cavity, onto the bowel wall, or onto instrument surfaces.
SSI: Diagnosed according to the Prevention’s National Healthcare Safety Network criteria.
All surgical procedures in both groups were performed by the same surgeon (author). Patients in both groups received combined intravenous anesthesia with endotracheal intubation, followed by a standard exploratory laparotomy incision, localization of the obstruction site, measurement of the distance from the obstruction site to the cecum, and small in
In the control group, the conventional intestinal decompression method was employed. Bilateral gauze was applied to protect the small intestine and the operative field. A site located 10 cm distal to the obstruction was selected for dec
In the cannula group, a purse-string suture using silk thread was placed at a location 10 cm distal to the obstructed intestinal segment. The intestinal wall was then incised using electrocautery, and a cannula was inserted into the proximal bowel and secured with a single knot. The distal end of the cannula was connected to a negative pressure suction device. Intestinal contents were segmentally advanced toward the cannula and collected in a container. After decompression was completed, the purse-string suture was tightened, and the small intestinal incision was covered by embedding the seromuscular layer (Figure 3).
Intraoperative decompression operation video: Intestinal contents were rapidly evacuated without contamination of the surgical field (Video).
The primary outcome measures included the number of cases involving contamination of the surgical field by intestinal contents, the volume of decompressed intestinal drainage, the time required for intestinal decompression, total operative time, and length of hospital stay. The incidence of postoperative complications was documented, including intra-abdominal infection and SSI. All patients were followed for a period of 6 months to monitor the occurrence of complications.
Continuous variables are presented as median (interquartile range) due to non-normal distribution, and compared using the Mann-Whitney U test. Categorical variables are presented as n (%) and compared using the χ² test or Fisher's exact test, as appropriate. Effect sizes are reported with 95%CI. A two-sided P < 0.05 was considered statistically significant.
The objective of the study was to assess the potential advantages of the double cannula decompression technique. The sample size was determined based on the findings of a preliminary test. Given that α = 0.05 and power = 0.8, the sample size calculation indicated that a minimum of 30 subjects per group would be required to detect statistically significant differences between the cannula technique and the conventional decompression method.
There were no statistically significant differences observed between the two groups with respect to age, sex, causes of obstruction, length of the obstructed intestine, and duration of obstruction (P > 0.05; Table 1).
| Cannula group (n = 37) | Control group (n = 33) | Value of statistics | P value | |
| Age (year) [mean (IQR)] | 60 (48, 69) | 62 (59, 68) | 0.801 | 0.423 |
| Sex | - | 0.051 | ||
| Male | 16 (43.2) | 22 (66.7) | ||
| Female | 21 (56.8) | 11 (33.3) | ||
| Cause of obstruction | - | 0.881 | ||
| Intestinal adhesions | 16 (43.2) | 12 (36.4) | ||
| Tumor | 3 (8.1) | 3 (9.1) | ||
| Intestinal foreign body | 7 (18.9) | 5 (15.2) | ||
| Inguinal hernia | 11 (29.7) | 13 (39.4) | ||
| Obstruction of intestinal tube length (cm) [mean (IQR)] | 270 (250, 300) | 280 (260, 300) | 0.050 | 0.960 |
| Obstruction time (hours) [mean (IQR)] | 76 (68, 84) | 72 (66, 76) | 1.009 | 0.316 |
The cannula group demonstrated statistically significant advantages across all key intraoperative metrics compared to the conventional group. The time required for intestinal decompression was significantly shorter in the cannula group [10 (9, 10) minutes] than in the control group [16 (15, 17) minutes], with a median difference of -6 minutes (95%CI: -7 to -5; P < 0.001). Furthermore, the volume of evacuated intraluminal contents was substantially greater in the cannula group [700 (680, 750) mL] vs the control group [580 (550, 600) mL], corresponding to a median difference of 120 mL (95%CI: 100-140; P < 0.001). Crucially, the incidence of surgical field contamination was significantly lower in the cannula group [5 (13.5%)] vs the control group [12 (36.4%)], with a relative risk of 0.37 (95%CI: 0.15-0.91; P = 0.026). Consequently, the total ope
| Cannula group (n = 37) | Control group (n = 33) | Value of statistics | P value | |
| Operative method | χ² = 1.204 | 0.548 | ||
| Intestinal adhesiolysis | 9 (24.3) | 12 (36.4) | ||
| Intestinal resection | 16 (43.2) | 12 (36.4) | ||
| Intestinal anastomosis | 12 (32.4) | 9 (27.3) | ||
| Intestinal decompression time (minutes) [mean (IQR)] | 10 (9, 10) | 16 (15, 17) | Z = 7.108 | < 0.001 |
| Reduced pressure amount (mL) [mean (IQR)] | 700 (680, 750) | 580 (550, 600) | Z = 7.197 | < 0.001 |
| Surgical field contamination | χ² = 4.953 | 0.026 | ||
| No | 32 (86.5) | 21 (63.6) | ||
| Yes | 5 (13.5) | 12 (36.4) | ||
| Operative time (minutes) [mean (IQR)] | 150 (140, 160) | 180 (170, 200) | Z = 6.183 | < 0.001 |
Postoperative recovery was notably enhanced in the cannula-assisted decompression group. The time to first post
| Cannula group (n = 37) | Control group (n = 33) | Value of statistics | P value | |
| First postoperative flatus (hours) [mean (IQR)] | 58 (56, 60) | 70 (68, 72) | Z = 7.171 | < 0.001 |
| Hospitalization days (days) [mean (IQR)] | 9 (8, 11) | 14 (13, 15) | Z = 5.971 | < 0.001 |
| Surgical site infection | χ² = 4.142 | 0.042 | ||
| No | 33 (89.2) | 23 (69.7) | ||
| Yes | 4 (10.8) | 10 (30.3) | ||
| Abdominal infection | 0 | 0 | - | - |
| Readmission | - | 0.598 | ||
| No | 36 (97.3) | 31 (93.9) | ||
| Yes | 1 (2.7) | 2 (6.1) |
Patients with small bowel obstruction typically present with proximal intestinal dilation, accumulation of gas and fluid, and edema of the bowel wall. Exploratory laparotomy has long been regarded as the standard surgical intervention for intestinal obstruction. Following the removal of obstructive factors, effective intestinal decompression is essential for reducing bowel wall edema, lowering intra-abdominal pressure, and facilitating the restoration of postoperative intestinal motility[7-9]. Conventional decompression techniques often involve open enterotomy, which presents several limitations: (1) Exteriorization of the intestine from the abdominal cavity and incision of the bowel wall elevate the risk of surgical field contamination. In patients with a shortened mesentery, intestinal exteriorization is challenging, thereby com
Considering the factors outlined above, a low-cost, time-efficient cannula decompression technique was developed for clinical use. During the design of the cannula, multiple side perforations were incorporated into the outer cannula to facilitate the entry of intestinal contents and to preserve decompression function even when partial obstruction of the side openings occurs. The inner cannula, characterized by a smaller diameter and greater length than the outer cannula, permits air entry and circulation, thereby minimizing mucosal injury caused by negative pressure suction. The distal end can be directly connected to a negative pressure suction device, enabling decompression to be performed under sealed conditions. During the decompression procedure, a purse-string suture is placed at the distal segment of the obstructed intestine, followed by a longitudinal incision approximately 1 cm in length on the intestinal wall. The double cannula is then inserted, and the purse-string suture is secured. The distal end is connected to a negative pressure suction system, facilitating rapid evacuation of intestinal contents through the cannula and achieving effective decompression. The results of this study confirmed that cannula decompression significantly reduced intraoperative time, minimized surgical field contamination, and promoted postoperative recovery. The advantages of this decompression technique can be summarized as follows: (1) Decompression is performed within the surgical field, irrespective of mesenteric length, and intestinal contents are less likely to spill, thereby preventing contamination of the operative area; (2) Negative pressure suction decompression obviates the need for repeated manual compression of the intestine and requires only main
Several considerations should be addressed during the implementation of the cannula decompression technique: (1) Negative pressure suction should be maintained between 0.02 MPa and 0.04 MPa; insufficient pressure may impair the effectiveness of decompression, whereas excessive pressure can readily lead to mucosal adhesion and subsequent injury to the intestinal lining; (2) In patients with a high content of food residue in the intestinal lumen, cannula obstruction may occur. In such cases, the cannula may be externally cleared through the intestinal wall during the procedure, and rep
In this study, the cannula decompression technique was primarily employed to manage the accumulation of fluid and gas in the proximal obstructed bowel. Its primary advantage lies in the efficient and clean reduction of intraluminal pressure, a benefit universally applicable to all types of mechanical intestinal obstruction[13,14]. However, the application strategy and specific focus of its advantages may vary depending on the underlying etiology. It is crucial to emphasize that the treatment of the primary cause remains equally important, such as herniorrhaphy, adhesiolysis, and resection of intestinal tumors. The cannula decompression must be underscored as an adjuvant technique that must be employed in conjunction with definitive surgical procedures addressing the root cause of the obstruction.
The findings of this study illustrate the clinical advantages of the cannula decompression technique in small intestine decompression surgery. Nonetheless, several limitations should be acknowledged. First, a larger sample size and an extended postoperative follow-up period are necessary to accurately assess the recurrence of small bowel obstruction following patient discharge. Second, due to the inherent limitations of retrospective cohort study designs, randomized controlled trials are planned to further validate the clinical efficacy of this technique.
In this single-center retrospective cohort study, the use of a cannula-assisted decompression technique was associated with superior intraoperative efficiency and reduced surgical site contamination compared to conventional enterotomy. These findings suggest it is a viable and promising alternative for intraoperative decompression in small bowel obs
The authors sincerely thank all the patients who participated in this study. We also extend our gratitude to the nursing staff and surgical teams of the Department of General Surgery, Anqing Municipal Hospital, for their invaluable support and collaboration in patient care and data collection. We are also grateful to colleagues in the Department of Gastroenterology for their clinical input.
| 1. | Taylor MR, Lalani N. Adult small bowel obstruction. Acad Emerg Med. 2013;20:528-544. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 106] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 2. | Ten Broek RPG, Krielen P, Di Saverio S, Coccolini F, Biffl WL, Ansaloni L, Velmahos GC, Sartelli M, Fraga GP, Kelly MD, Moore FA, Peitzman AB, Leppaniemi A, Moore EE, Jeekel J, Kluger Y, Sugrue M, Balogh ZJ, Bendinelli C, Civil I, Coimbra R, De Moya M, Ferrada P, Inaba K, Ivatury R, Latifi R, Kashuk JL, Kirkpatrick AW, Maier R, Rizoli S, Sakakushev B, Scalea T, Søreide K, Weber D, Wani I, Abu-Zidan FM, De'Angelis N, Piscioneri F, Galante JM, Catena F, van Goor H. Bologna guidelines for diagnosis and management of adhesive small bowel obstruction (ASBO): 2017 update of the evidence-based guidelines from the world society of emergency surgery ASBO working group. World J Emerg Surg. 2018;13:24. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 140] [Cited by in RCA: 309] [Article Influence: 38.6] [Reference Citation Analysis (0)] |
| 3. | Walshaw J, Smith HG, Lee MJ. Small bowel obstruction. Br J Surg. 2024;111:znae167. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 4. | Kono J, Yoshimaru K, Kondo T, Takahashi Y, Toriigahara Y, Fukuta A, Obata S, Kawakubo N, Nagata K, Matsuura T, Tajiri T. The Volume of Intestinal Decompression can Predict the Necessity of Surgical Intervention for Adhesive Small Bowel Obstruction. J Pediatr Surg. 2023;58:1252-1257. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 5. | Huston JM, Barie PS, Dellinger EP, Forrester JD, Duane TM, Tessier JM, Sawyer RG, Cainzos MA, Rasa K, Chipman JG, Kao LS, Pieracci FM, Colling KP, Heffernan DS, Lester J; Therapeutics and Guidelines Committee. The Surgical Infection Society Guidelines on the Management of Intra-Abdominal Infection: 2024 Update. Surg Infect (Larchmt). 2024;25:419-435. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 37] [Article Influence: 18.5] [Reference Citation Analysis (0)] |
| 6. | Nam SH. A novel and simple method using a transanal intestinal long tube for protecting intestinal anastomosis and decompressing the small bowel. Ann Surg Treat Res. 2017;93:137-142. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 7. | Thacker C, Lauer C, Nealon K, Wang S, Factor M. Should Surgical Services Admit Small Bowel Obstructions Managed Non-operatively? Am Surg. 2022;88:1845-1848. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 8. | M L, G B, F F, M B, M D, E PS, Jf H, A V. Enhanced recovery programs following adhesive small bowel obstruction surgery are feasible and reduce the rate of postoperative ileus: a preliminary study. Langenbecks Arch Surg. 2024;409:191. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 9. | Kam MH, Tang CL, Chan E, Lim JF, Eu KW. Systematic review of intraoperative colonic irrigation vs. manual decompression in obstructed left-sided colorectal emergencies. Int J Colorectal Dis. 2009;24:1031-1037. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 33] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 10. | Ezer A, Torer N, Colakoglu T, Colakoglu S, Parlakgumus A, Yildirim S, Moray G. Clinical outcomes of manual bowel decompression (milking) in the mechanical small bowel obstruction: a prospective randomized clinical trial. Am J Surg. 2012;203:95-100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 11. | Mintz Y, Arezzo A, Boni L, Chand M, Brodie R, Fingerhut A; and the Technology Committee of the European Association for Endoscopic Surgery. A Low-cost, Safe, and Effective Method for Smoke Evacuation in Laparoscopic Surgery for Suspected Coronavirus Patients. Ann Surg. 2020;272:e7-e8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 56] [Cited by in RCA: 59] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 12. | Limchantra IV, Fong Y, Melstrom KA. Surgical Smoke Exposure in Operating Room Personnel: A Review. JAMA Surg. 2019;154:960-967. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 80] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 13. | Wang SJ, Xue YJ, She LL, Xia Y, Lin JL. Clinical application of super-low-positioned intestinal decompression tube in the treatment of intestinal obstruction: a pilot study. Surg Endosc. 2024;38:880-887. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 14. | Itou C, Arai Y, Sone M, Sugawara S, Kimura S, Onishi Y. Percutaneous Image-Guided Transesophageal Long Intestinal Tube Placement for Palliative Decompression in Advanced Cancer Patients with Unresectable Malignant Small Bowel Obstruction. Cardiovasc Intervent Radiol. 2023;46:1000-1012. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/