Published online Sep 27, 2025. doi: 10.4240/wjgs.v17.i9.109270
Revised: June 12, 2025
Accepted: July 14, 2025
Published online: September 27, 2025
Processing time: 131 Days and 0.6 Hours
The current surgical treatments for bile duct stones (BDSs) demonstrate sub
To assess the therapeutic efficacy and safety profiles of endoscopic retrograde cholangiopancreatography (ERCP) vs common bile duct exploration (CBDE) in BDS treatment.
This study enrolled 103 consecutive patients with BDSs treated at the First People’s Hospital of Changde from January 2024 to January 2025, with 53 patients undergoing ERCP (ERCP group) and 50 receiving conventional CBDE (CBDE group). Comprehensive comparative analyses were conducted across multiple parameters, including clinical efficacy, surgical success rate, safety (bile leakage incidence, surgical site infection, acute pancreatitis, and acute cholangitis), po
The ERCP group demonstrated markedly superior overall efficacy than the CBDE group, with similar surgical success rates and comparable stone removal du
ERCP demonstrates effectiveness and safety in managing BDSs, thereby providing notable clinical benefits that support its broader implementation in medical practice.
Core Tip: The current research assessed the effectiveness and safety of endoscopic retrograde cholangiopancreatography (ERCP) in treating bile duct stones and provided valuable evidence to guide clinical decision-making. We conducted a comprehensive analysis, including therapeutic effectiveness, procedural success rates, patient safety, postoperative biochemical parameters, surgery-related metrics, and recovery outcomes, to compare ERCP with conventional common bile duct exploration, thereby confirming ERCP’s clinical advantages in enhancing clinical outcomes, improving safety and procedural efficiency, and speeding up patient recovery.
- Citation: Gong DF, Cheng L. Efficacy and safety of endoscopic retrograde cholangiopancreatography in the treatment of bile duct stones. World J Gastrointest Surg 2025; 17(9): 109270
- URL: https://www.wjgnet.com/1948-9366/full/v17/i9/109270.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v17.i9.109270
Cholelithiasis is a prevalent and high-risk gastrointestinal disorder that correlates with substantial healthcare expenditures, thereby imposing substantial health and financial challenges for patients and healthcare systems[1,2]. This condition includes gallstones and bile duct stones (BDSs), with an estimated global prevalence of 10.0%-15.0% among adults[3]. Based on epidemiological trends, the occurrence of BDSs, especially in older and middle-aged demographics, is increasing[4]. Clinically classified as intrahepatic or extrahepatic, BDSs frequently manifest as aggregated or dispersed calcifications, causing biliary strictures[5]. Without intervention, these stones can induce biliary blockages, repeated cholangitis episodes, and bacterial overgrowth in the biliary ducts, which significantly increases the likelihood of infections[6]. BDSs are challenging to effectively treat because stones often persist, symptoms tend to reappear, and patients predominantly require repeat surgeries[7].
Therapeutic outcomes for BDSs remain suboptimal with current surgical methods, driving the need for continued innovation in clinical management to optimize efficacy and patient safety[8]. Among these, common bile duct exploration (CBDE) is a gold-standard intervention, where surgeons perform an anterior wall incision (open or laparoscopic incision) on the common bile duct to facilitate stone extraction under direct visualization with choledochoscopy or forceps assistance. This method is especially effective for treating challenging intrahepatic and extrahepatic BDSs, circumventing duodenal anatomical barriers[9]. The procedure’s invasiveness and longer recovery period restrict its widespread adoption despite its higher success rate in stone clearance and decreased recurrence[10]. Evidence from a systematic review and meta-analysis revealed that CBDE carries greater risks of retained stones and bile duct leakage postoperatively compared with laparoscopic transcystic techniques[11]. Alternatively, endoscopic retrograde cholangiopancreatography (ERCP) has appeared as a minimally invasive option, utilizing duodenoscopic cannulation of the papilla with contrast-assisted stone localization. After papillary dilation (performed via balloon techniques or endoscopic sphincterotomy), stones are removed using retrieval baskets or balloons, with mechanical lithotripsy applied for larger stones[12]. The procedure’s success in complete stone clearance is operator-dependent and associated with potential adverse events, including infections, bleeding episodes, and pancreatic inflammation, in addition to a significant recurrence rate, despite being less invasive and enabling speedier recovery[13]. Evidence confirms ERCP’s clinical effectiveness and safety for choledocholithiasis while optimizing recovery through reductions in total hospitalization period, preoperative stay duration, and operative time[14]. This study compares CBDE and ERCP in terms of efficacy, surgical success rates, safety, biochemical markers, surgical metrics, and recovery outcomes. The comparative data generated will serve as an important reference for BDS intervention selection.
We retrospectively reviewed data from 103 patients with BDS treated from January 2024 to January 2025, categorized based on treatment approach into CBDE (n = 50) or ERCP (n = 53) groups. A qualified surgical team (minimum 5 years of specialized experience) performed all interventions. Under the Declaration of Helsinki guidelines, all patient data were de-identified to ensure confidentiality. Baseline demographic and clinical parameters demonstrated no significant inter-group differences (P > 0.05), thereby confirming group comparability.
Inclusion criteria were BDSs confirmed based on relevant examinations[15]; characteristic clinical manifestations (upper abdominal pain, dyspepsia, or obstructive jaundice); no previous stone interventions; procedure (CBDE or ERCP) eligibility; no outcome-affecting medications (90-day preclusion); complete and reliable clinical records. Exclusion criteria were recurrent biliary stones or biliary malignancies; acute biliary inflammation; chronic peritonitis history; previous major abdominal surgery or significant intra-abdominal adhesions; comorbid cardiopulmonary dysfunction or he
CBDE group: CBDE was performed under general anesthesia. An artificial pneumoperitoneum was first established, followed by laparoscopic insertion. The common bile duct was carefully dissected with an electrocoagulation hook. Under direct choledochoscopic visualization, the biliary tract was assessed to accurately localize stones and identify their exact number. After puncturing the duct, bile was aspirated, and choledochotomy was performed for stone removal. Finally, a drainage tube was placed, and the incision was closed with sutures.
ERCP group: After 8 hours of fasting, patients were placed in the left lateral decubitus position and administered with anesthesia. A duodenoscope was introduced orally and advanced to the major duodenal papilla. A contrast catheter was then cannulated into the bile duct, enabling bile aspiration and contrast medium injection. This facilitated detailed biliary and pancreatic ductal anatomy visualization, including the location, size, and number of stones. The optimal intervention (endoscopic sphincterotomy or papillary balloon dilation) was determined based on each patient’s anatomical characteristics. Sphincterotomy was conducted to directly incise the papilla to facilitate stone removal when papillary strictures or impacted stones were present. Conversely, balloon dilation was the technique of choice for patients demonstrating narrow yet relatively patent papillary openings. This technique effectively widens the biliary orifice to permit smooth choledochoscope and retrieval basket insertion. Stones were then fragmented with a mechanical lithotripter and completely extracted using the retrieval basket. A nasobiliary drainage tube was placed. A follow-up cholangiogram was performed on postoperative day 3 to assess for residual stones.
The CBDE and ERCP groups received standard postoperative antibiotic therapy and comprehensive perioperative care. The nursing protocol included preoperative preparation, intraoperative management (including proper patient positioning, intravenous access establishment, and electrocardiograph monitoring under the surgeon’s guidance), as well as postoperative surgical detail documentation, continuous vital sign assessment, and drainage output close monitoring.
(1) Efficacy: Treatment efficacy was assessed as cured (complete stone clearance with overall clinical symptom re
To safeguard patient privacy and data security, this study employed a data anonymization protocol with key steps as follows. Before initiating data analysis, all fields that contain personally identifiable information, including names, national identity numbers, and contact details, were systematically eliminated. Medical record numbers were used as encrypted unique identifiers, ensuring traceability while effectively preventing leakage of patient identity information. Throughout the research process, data analyses were conducted exclusively on de-identified datasets, with research personnel granted no access to the original personally identifiable information. All publicly shared data for result publication were aggregated to eliminate any risk of individual identification, thereby ensuring that only research findings and statistical summaries were disclosed. The final research report provides exclusively consolidated statistical outcomes, avoiding the disclosure of detailed information about individual patients.
GraphPad Prism version 7.0 and IBM SPSS Statistics version 20.0 was used for all statistical analysis. Categorical variables are expressed as n (%), whereas continuous variables are presented as mean ± SD of the mean. Intergroup comparisons of categorical data employed χ2 tests, whereas independent sample t-tests were conducted for continuous variables. Paired t-tests were utilized to assess within-group pre-post differences. Statistical significance was set at a P < 0.05.
No significant differences in terms of baseline characteristics, including age, gender, disease duration, stone diameter, and stone number, were observed between the CBDE and ERCP groups (P > 0.05; Table 1).
| Category | CBDE group, N = 50 | ERCP group, N = 53 | χ2/t | P value |
| Age, years | 44.50 ± 9.41 | 43.25 ± 9.46 | 0.672 | 0.503 |
| Gender | 0.418 | 0.518 | ||
| Male | 28 (56.00) | 33 (62.26) | ||
| Female | 22 (44.00) | 20 (37.74) | ||
| Disease duration, years | 3.86 ± 1.44 | 4.42 ± 1.93 | 1.662 | 0.100 |
| Stone diameter, cm | 1.87 ± 0.84 | 1.59 ± 0.68 | 1.864 | 0.065 |
| Stone number | 3.54 ± 1.16 | 3.92 ± 1.31 | 1.555 | 0.123 |
The total treatment efficacy rate was significantly higher in the ERCP group (94.34%) than in the CBDE group (74.00%, P < 0.05; Table 2).
| Category | CBDE group, N = 50 | ERCP group, N = 53 | χ2 | P value |
| Cured | 21 (42.00) | 28 (52.83) | ||
| Improved | 16 (32.00) | 22 (41.51) | ||
| Ineffective | 13 (26.00) | 3 (5.36) | ||
| Total effective rate | 37 (74.00) | 50 (94.34) | 8.783 | 0.003 |
Both groups demonstrated similar surgical success rates (P > 0.05). However, the ERCP group (3.77%) exhibited a significantly lower overall incidence of postoperative complications, including bile leakage, surgical site infection, acute pancreatitis, and acute cholangitis, compared with the CBDE group (16.00%, P < 0.05; Table 3).
| Category | CBDE group, N = 50 | ERCP group, N = 53 | χ2 | P value |
| Surgical success rate | 45 (90.00) | 50 (94.34) | 0.676 | 0.411 |
| Bile leakage | 2 (4.00) | 0 (0.00) | ||
| Surgical site infection | 3 (6.00) | 2 (3.77) | ||
| Acute pancreatitis | 1 (2.00) | 0 (0.00) | ||
| Acute cholangitis | 2 (4.00) | 0 (0.00) | ||
| Total complications | 8 (16.00) | 2 (3.77) | 4.387 | 0.036 |
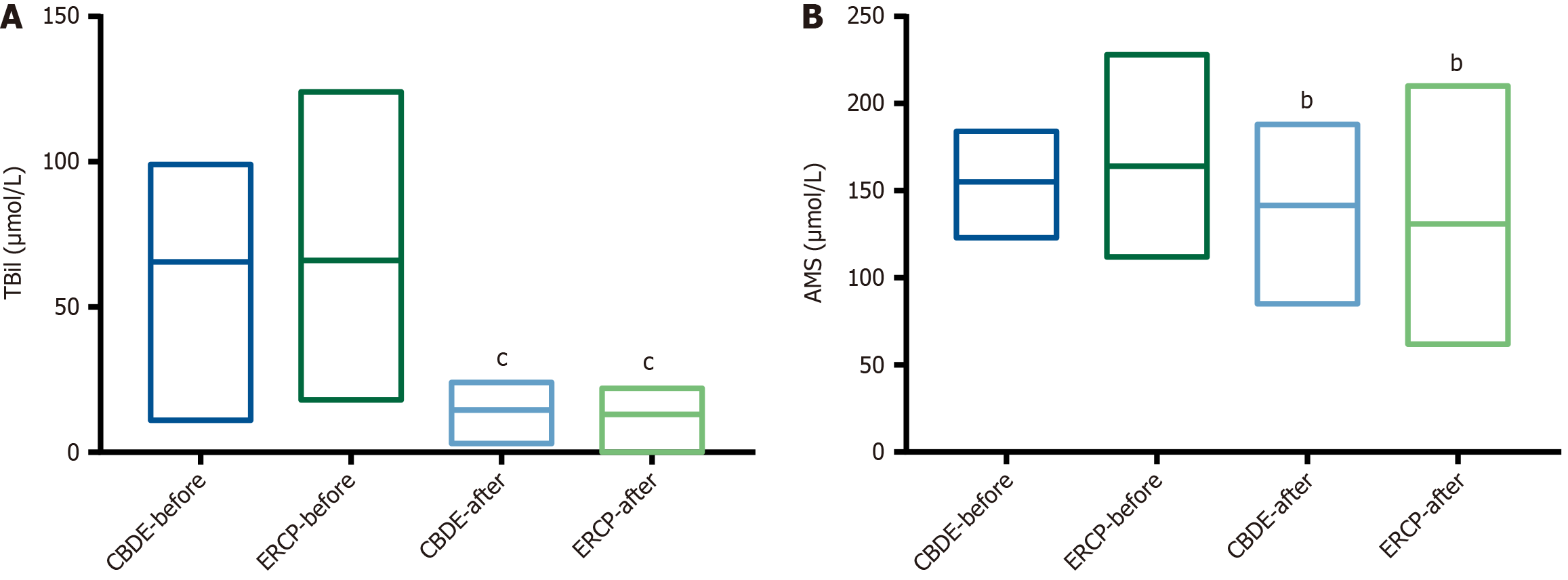
Pre-treatment TBil and AMS levels did not significantly differ between the CBDE and ERCP groups (P > 0.05). After treatment, both groups demonstrated significant reductions in TBil and AMS levels (P < 0.05), although the magnitude of improvement did not significantly differ between them (P > 0.05; Figure 1).
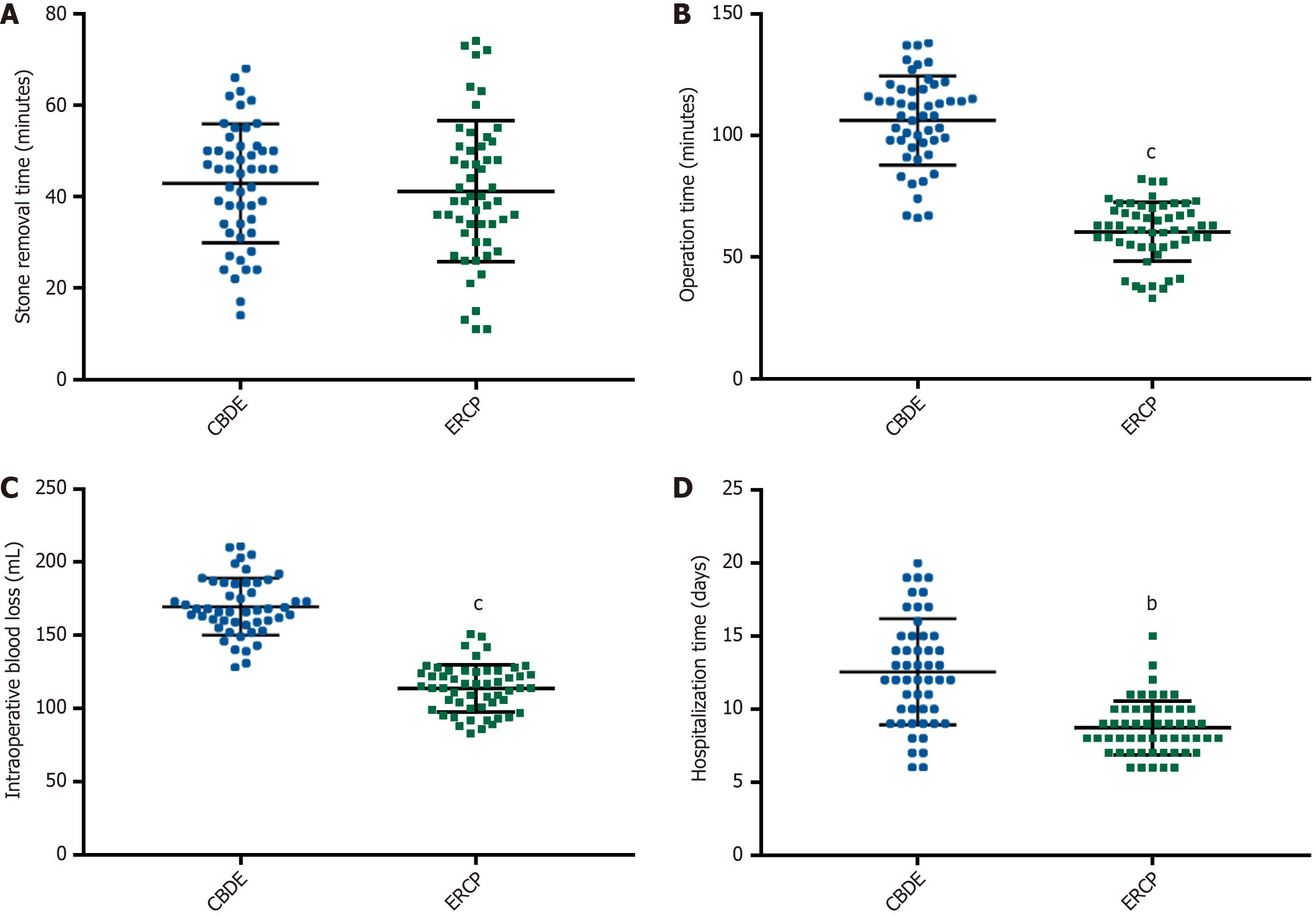
We assessed and compared key surgical parameters, including stone removal time, operation time, intraoperative blood loss, and hospitalization time, between the ERCP and CBDE groups. The results revealed that the ERCP group de
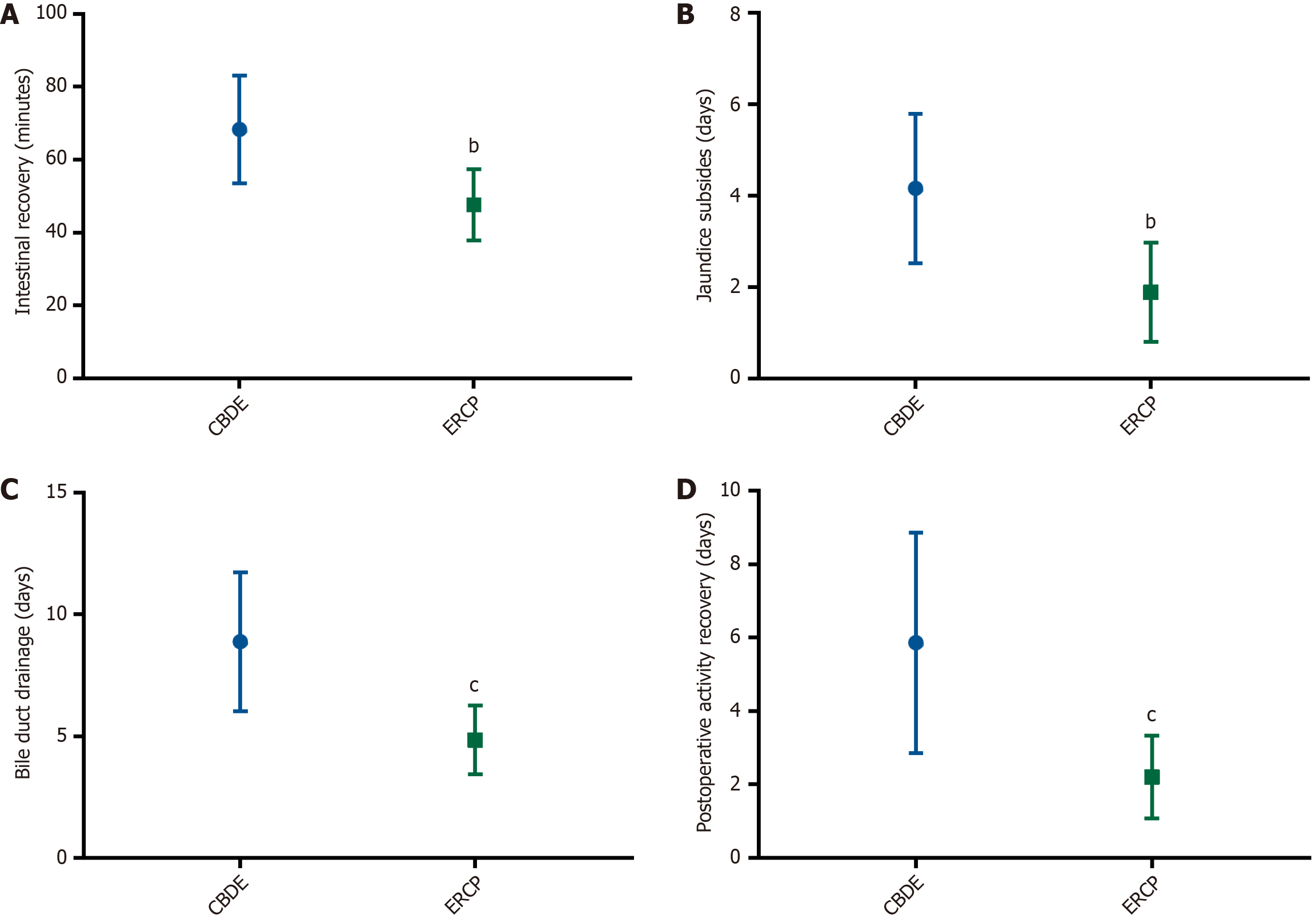
Postoperative recovery parameters, including time to intestinal recovery, jaundice resolution, biliary drainage removal, and postoperative activity recovery, were evaluated. The ERCP group demonstrated significantly faster recovery across all these measures compared with the CBDE group (P < 0.01; Figure 3).
The pathogenesis of BDSs is closely associated with age-related physiological changes and dietary habit modifications, which collectively contribute to progressive hepatobiliary function impairment, diminished digestive capacity, and gallbladder function deterioration[16]. Moreover, this condition predisposes patients to biliary stasis, thereby exacerbating cholecystitis development and accelerating lithogenesis[17]. To mitigate disease progression and promote optimal recovery, surgical approach improvement is imperative to enhance therapeutic outcomes while minimizing postoperative complications.
Our comparative analysis revealed markedly superior overall treatment efficacy for ERCP than conventional CBDE, thereby establishing ERCP’s clinical superiority in BDS treatment. During ERCP procedures, three cases experienced initial treatment failure due to varying clinical complexities. The first case involved a 65-year-old male patient presenting with a 4.2 cm impacted calculus and concomitant stricture of the distal common bile duct (luminal diameter < 3 mm). The primary ERCP attempt failed as the mechanical lithotripter basket failed to secure the stone. This patient subsequently underwent successful stone extraction through laparoscopic CBDE. The second case involved a 70-year-old female patient demonstrating intrahepatic bile duct calculi within the left hepatic duct, accompanied by aberrant biliary anatomy characterized by severe ductal angulation and tortuosity. The ERCP procedure was discontinued when cannulation attempts failed to navigate the guidewire into the targeted biliary branch. The patient eventually underwent percutaneous transhepatic cholangial drainage, followed by a second-stage surgery. The third case concerned a 58-year-old male patient with multiple BDSs (maximum diameter of 2.8 cm) and a periampullary duodenal diverticulum. The procedure was temporarily suspended after precut sphincterotomy due to a significant hemorrhage that compromised endoscopic visualization. After successful endoscopic hemostasis, delayed ERCP was successfully performed to complete the treatment.
Subsequently, the ERCP cohort demonstrated a significantly lower incidence of overall complications, including biliary leakage, surgical site infections, acute pancreatitis, and acute cholangitis, underscoring its improved safety profile, whereas both techniques demonstrated comparable surgical success rates. Biochemical marker analysis revealed equivalent efficacy between the two interventions in reducing TBil and AMS levels, thereby confirming their comparable capacity to relieve biliary obstruction and restore pancreatic function. Noteworthily, a decrease in TBil indicates successful biliary obstruction resolution and bile drainage restoration, whereas a decline in AMS indicates a protective effect on the pancreas postoperatively[18]. The observed biochemical normalization reflects distinct decompression mechanisms such as endoscopic stenting in ERCP vs surgical T-tube drainage in CBDE[19].
Notably, ERCP outperforms CBDE in terms of key surgical metrics, including operative time (shorter), intraoperative hemorrhage volume (lower), and postoperative recovery period (reduced), but their stone removal time was comparable. Moreover, patients undergoing ERCP experienced quicker jaundice resolution, earlier gastrointestinal function recovery, lower biliary drainage utilization, and faster functional recovery. This evidence substantiates ERCP’s greater procedural efficiency and safety while confirming its recovery improvement potential. Previous studies corroborate our results, with Li et al[20] revealing ERCP’s advantages in reducing both procedural duration and hospital stay for common BDSs. Likewise, study of Wang et al[21] on pediatric pancreatobiliary disorders revealed superior outcomes with ERCP vs conventional surgery, including reduced complications and accelerated recovery, aligning with our observations. However, long-term follow-up data indicate ERCP’s higher recurrence risk, with a retrospective comparative study reporting 8.9% recurrence vs 2.0% for CBDE over a 4.5-year follow-up period[22]. Zhang et al[23] conducted economic analyses and revealed comparable drug costs and total expenses between approaches, with ERCP demonstrating lower surgical/nursing expenses and CBDE exhibiting advantages in treatment/supply costs, thereby supporting ERCP’s clinical feasibility in BDS management despite its limitations in terms of recurrence.
Several surgical modalities have been assessed for BDS treatment. Thai Binh et al[24] confirmed the safety and effectiveness of percutaneous transhepatic endoscopic holmium laser lithotripsy, particularly in complex cases. Similarly, Wang et al[25] revealed that dual-modality endoscopy (combining duodenoscopy and laparoscopy) outperformed conventional laparotomy in patients with BDS, thereby providing superior efficacy, fewer postoperative complications, accelerated recovery, and mitigated inflammatory responses. Furthermore, Liu et al[26] observed that laparoscopic reoperation for BDSs provided significant clinical advantages over open surgery, including reduced intraoperative blood loss, shorter hospital stays, and lower postoperative analgesic requirements.
This study has limitations. First, the restricted participant pool may introduce potential sampling bias, emphasizing the need for broader subject recruitment in subsequent studies. Second, the absence of long-term follow-up data (e.g.,
In conclusion, ERCP demonstrates notable benefits in treating BDSs, which significantly improve clinical outcomes, procedural safety, and surgical efficiency while facilitating postoperative recovery. These results support its widespread adoption in clinical practice.
| 1. | Sebghatollahi V, Parsa M, Minakari M, Azadbakht S. A clinician's guide to gallstones and common bile duct (CBD): A study protocol for a systematic review and evidence-based recommendations. Health Sci Rep. 2023;6:e1555. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 11] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 2. | Ali FS, DaVee T, Bernstam EV, Kao LS, Wandling M, Hussain MR, Rashtak S, Ramireddy S, Guha S, Thosani N. Cost-effectiveness analysis of optimal diagnostic strategy for patients with symptomatic cholelithiasis with intermediate probability for choledocholithiasis. Gastrointest Endosc. 2022;95:327-338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 3. | Stinton LM, Shaffer EA. Epidemiology of gallbladder disease: cholelithiasis and cancer. Gut Liver. 2012;6:172-187. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 556] [Cited by in RCA: 782] [Article Influence: 55.9] [Reference Citation Analysis (0)] |
| 4. | Georgescu D, Ionita I, Lascu A, Hut EF, Dragan S, Ancusa OE, Ionita M, Calamar-Popovici D, Georgescu LA, Lighezan DF. Gallstone Disease and Bacterial Metabolic Performance of Gut Microbiota in Middle-Aged and Older Patients. Int J Gen Med. 2022;15:5513-5531. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 17] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 5. | Zhou D, Zhang B, Zhang XY, Guan WB, Wang JD, Ma F. Focal intrahepatic strictures: A proposal classification based on diagnosis-treatment experience and systemic review. World J Clin Cases. 2020;8:5902-5917. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 1] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 6. | Xia H, Zhang H, Xin X, Liang B, Yang T, Liu Y, Wang J, Meng X. Surgical Management of Recurrence of Primary Intrahepatic Bile Duct Stones. Can J Gastroenterol Hepatol. 2023;2023:5158580. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
| 7. | Ozcan N, Riaz A, Kahriman G. Percutaneous Management of Biliary Stones. Semin Intervent Radiol. 2021;38:348-355. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
| 8. | Chen ZL, Fu H. Endoscopic retrograde cholangiopancreatography, endoscopic papillary balloon dilation, and laparoscopic hepatectomy for intra- and extrahepatic bile duct stones. World J Gastrointest Surg. 2025;17:100544. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 9. | Liao JH, Li JS, Wang TL, Liu WS. Laparoscopic cholecystectomy plus common bile duct exploration for extrahepatic bile duct stones and postoperative recurrence-associated risk factors. World J Gastrointest Surg. 2024;16:3511-3519. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 10. | Ma Z, Zhou J, Yao L, Dai Y, Xie W, Song G, Meng H, Xu B, Zhang T, Zhou B, Yang T, Song Z. Safety and efficacy of laparoscopic common bile duct exploration for the patients with difficult biliary stones: 8 years of experiences at a single institution and literature review. Surg Endosc. 2022;36:718-727. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 25] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 11. | Zheng B, Lu Y, Li E, Bai Z, Zhang K, Li J. Comparison of the efficacy of LTCBDE and LCBDE for common bile duct stones: a systematic review and meta-analysis. Front Surg. 2024;11:1412334. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 12. | El Menabawey T, Mulay A, Graham D, Phillpotts S, Sethi A, Webster GJ. Predictors of success of conventional ERCP for bile duct stones and need for single-operator cholangioscopy. Endosc Int Open. 2023;11:E943-E951. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 13. | Li X, Ouyang J, Dai J. Current Gallstone Treatment Methods, State of the Art. Diseases. 2024;12:197. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 14. | Mallick R, Rank K, Ronstrom C, Amateau SK, Arain M, Attam R, Freeman ML, Harmon JV. Single-session laparoscopic cholecystectomy and ERCP: a valid option for the management of choledocholithiasis. Gastrointest Endosc. 2016;84:639-645. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 23] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 15. | Tazuma S. Gallstone disease: Epidemiology, pathogenesis, and classification of biliary stones (common bile duct and intrahepatic). Best Pract Res Clin Gastroenterol. 2006;20:1075-1083. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 262] [Cited by in RCA: 317] [Article Influence: 15.9] [Reference Citation Analysis (2)] |
| 16. | Wang Y, Lu J, Wen N, Nie G, Peng D, Xiong X, Cheng N, Li B. The role of diet and nutrition related indicators in biliary diseases: an umbrella review of systematic review and meta-analysis. Nutr Metab (Lond). 2022;19:51. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 17. | Yin Z, Shen B. Comparative study of the effect of U100 laser and pneumatic ballistic combined with percutaneous transhepatic cholangioscopic lithotomy in the treatment of intra-and extrahepatic bile duct stones and its effect on liver function. Pak J Med Sci. 2022;38:1686-1690. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 18. | Yan X, Xie F, Zhao XD, Li L, Meng JX. Short-term efficacy of early percutaneous cholecystostomy for pancreatitis and factors associated with recurrence and mortality. World J Gastroenterol. 2025;31:101163. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (4)] |
| 19. | Zhu J, Li G, Du P, Zhou X, Xiao W, Li Y. Laparoscopic common bile duct exploration versus intraoperative endoscopic retrograde cholangiopancreatography in patients with gallbladder and common bile duct stones: a meta-analysis. Surg Endosc. 2021;35:997-1005. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 24] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 20. | Li Q, Chen L, Liu S, Chen D. Comparison of Laparoscopic Common Bile Duct Exploration with Endoscopic Retrograde Cholangiopancreatography for Common Bile Duct Stones After Cholecystectomy. J Laparoendosc Adv Surg Tech A. 2022;32:992-998. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 21. | Wang XQ, Kong CH, Ye M, Diao M. Analysis of the efficacy and safety of endoscopic retrograde cholangiopancreatography for the treatment of pediatric pancreatobiliary diseases. World J Gastrointest Surg. 2024;16:3754-3763. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 22. | Al-Habbal Y, Reid I, Tiang T, Houli N, Lai B, McQuillan T, Bird D, Yong T. Retrospective comparative analysis of choledochoscopic bile duct exploration versus ERCP for bile duct stones. Sci Rep. 2020;10:14736. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 24] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 23. | Zhang R, Liu J, Li H, Zeng Q, Wu S, Tian H. Evaluation of therapeutic efficacy, safety and economy of ERCP and LTCBDE in the treatment of common bile duct stones. Front Physiol. 2022;13:949452. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 24. | Thai Binh N, Son Nam P, Quoc Hoa T, Nhan Hien P. Safety, efficacy, and feasibility of percutaneous transhepatic endoscopic holmium laser lithotripsy for bile duct stones. Eur Radiol. 2024;34:7176-7184. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 25. | Wang W, Xia H, Dai B. Comparison of the clinical effects of dual-modality endoscopy and traditional laparotomy for the treatment of intra- and extrahepatic bile duct stones. World J Gastrointest Surg. 2024;16:759-767. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 26. | Liu YY, Li TY, Wu SD, Fan Y. The safety and feasibility of laparoscopic approach for the management of intrahepatic and extrahepatic bile duct stones in patients with prior biliary tract surgical interventions. Sci Rep. 2022;12:14487. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/