Published online Sep 27, 2025. doi: 10.4240/wjgs.v17.i9.108621
Revised: May 20, 2025
Accepted: July 11, 2025
Published online: September 27, 2025
Processing time: 155 Days and 0.4 Hours
Peripherally inserted central catheters (PICCs) are crucial for patients requiring long-term intravenous therapy, especially within digestive surgery under bundled care protocols.
To evaluate and compare the efficacy, safety, and patient-reported outcomes of single-lumen vs double-lumen PICCs among patients undergoing digestive surgery within a structured bundled care framework.
This retrospective cohort study analyzed data from 249 patients who underwent digestive surgery and utilized either single-lumen (n = 117) or double-lumen (n = 132) PICCs between January 2021 and June 2024. Clinical outcomes, patient satisfaction, catheterization duration, and complication rates were compared using statistical analysis via SPSS (version 29.0). The bundled care protocol was consistently applied, focusing on standardized procedures, staff training, and patient support.
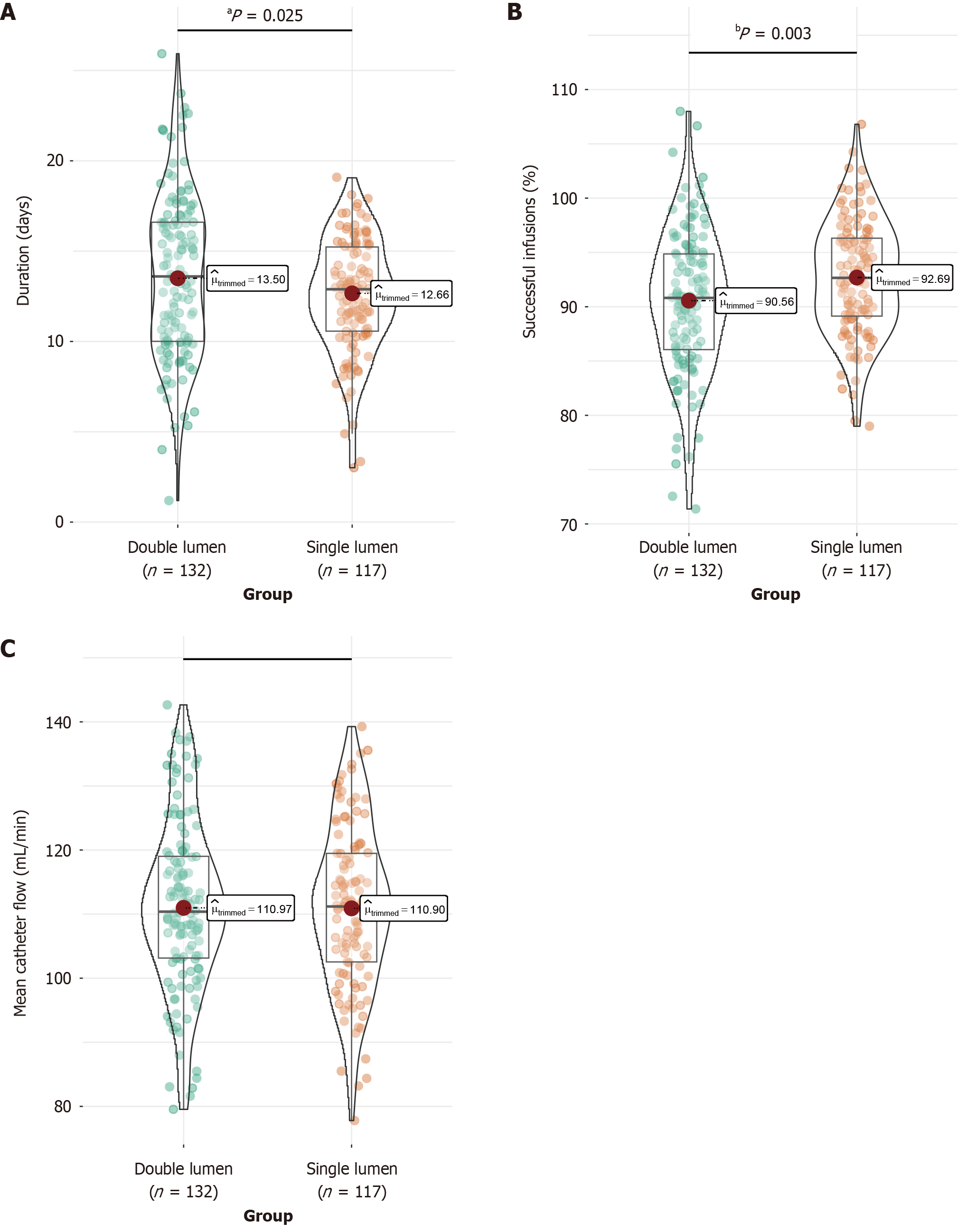
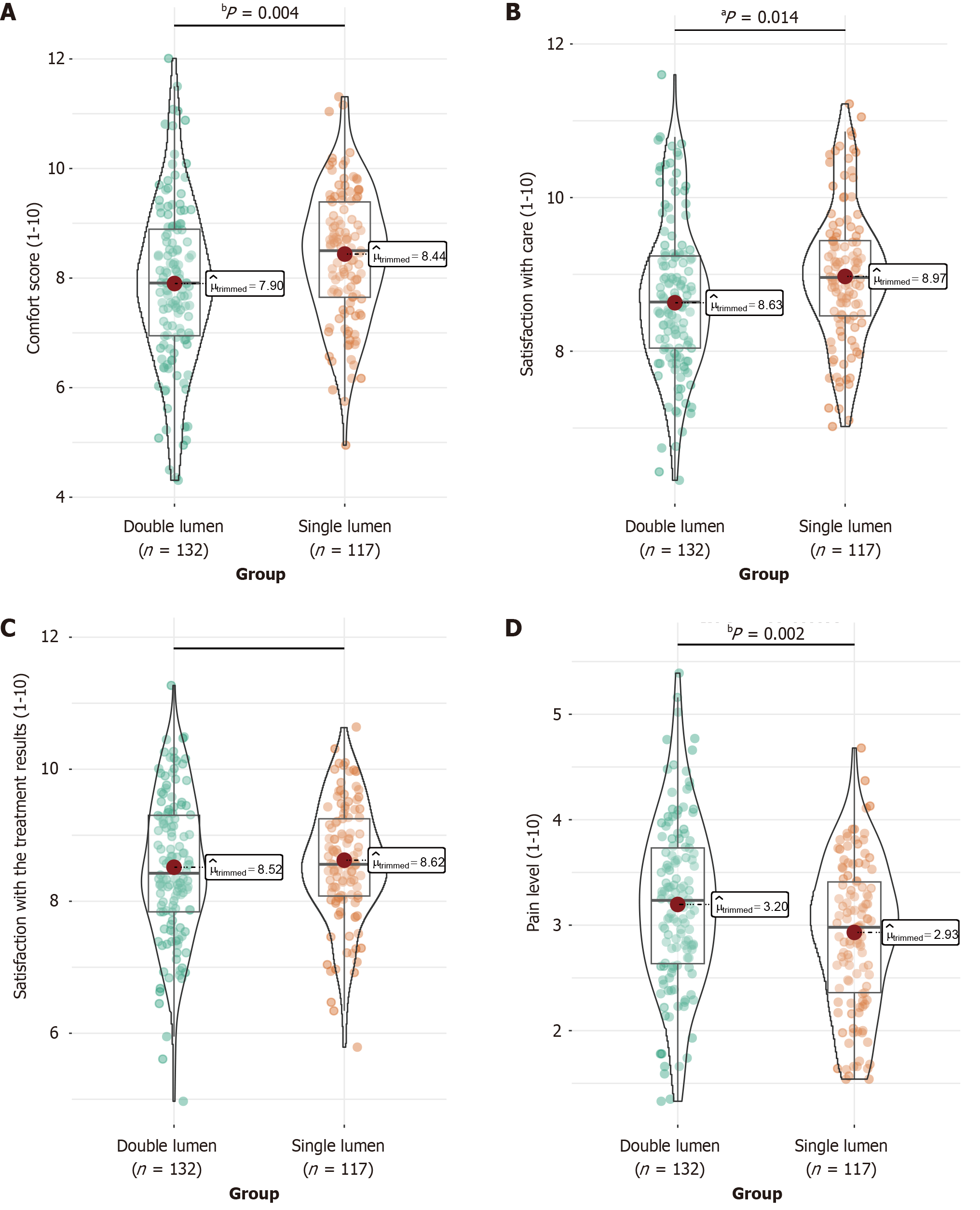
Single-lumen PICCs were associated with a significantly lower thrombosis rate (0.85%) than double-lumen PICCs (6.82%, P = 0.039). The single-lumen group experienced shorter catheterization durations (12.5 ± 3.14 days vs 13.6 ± 4.50 days, P = 0.025) and higher successful infusion rates (92.7% ± 5.32% vs 90.4% ± 6.60%, P = 0.003). This group also reported higher comfort scores (8.40 ± 1.20 vs 7.90 ± 1.50, P = 0.004) and lower pain levels (2.90 ± 0.70 vs 3.20 ± 0.80, P = 0.002). Aside from thrombosis, complication rates showed no significant difference between the groups.
Within bundled care context, single-lumen PICCs demonstrated advantages in reducing thrombosis risk, procedural efficiency, patient comfort, and satisfaction compared with double-lumen PICCs. The findings underscore the importance of considering patient-specific needs and clinical scenarios in catheter choice.
Core Tip: This study evaluates the efficacy and safety of single-lumen vs double-lumen peripherally inserted central catheters (PICCs) in digestive surgery patients under bundled care protocols. Key findings indicate that single-lumen PICCs significantly reduce thrombosis rates, shorten catheterization durations, and improve patient comfort and satisfaction compared to double-lumen PICCs. These results highlight the importance of selecting appropriate catheter types based on patient-specific needs and clinical scenarios, optimizing both procedural efficiency and patient outcomes within a structured bundled care framework.
- Citation: Ye XH, Cui RH, Xu L, Wang MJ, Ye LR, Jiang M. Efficacy of single-lumen and double-lumen peripherally inserted central catheters in patients undergoing digestive surgery within bundled care contexts. World J Gastrointest Surg 2025; 17(9): 108621
- URL: https://www.wjgnet.com/1948-9366/full/v17/i9/108621.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v17.i9.108621
Peripherally inserted central catheters (PICCs) have become an invaluable tool in the management of patients requiring long-term intravenous therapy, especially within surgical and oncological settings[1,2]. These catheters offer a reliable means of venous access, facilitating the administration of medications, parenteral nutrition, and other essential therapies over prolonged durations without frequent venipuncture[3,4]. In digestive surgical patients who often require extended postoperative care and nutritional support, PICCs were commonly utilized due to their ease of maintenance and lower risk profile than traditional central venous catheters[5].
With the advent of bundled care approaches, which emphasize the integration of standardized clinical protocols, risk management strategies, and comprehensive patient support, the outcomes of catheter use in clinical practice have been significantly enhanced[6,7]. This model of care was designed to not only improve the safety and efficacy of clinical procedures but also enhance the overall patient experience by minimizing complications through meticulous infection control and thorough staff training. Within this context, the choice between single-lumen and double-lumen PICCs becomes particularly pertinent because each presents distinct advantages and potential risks[8,9].
Single-lumen PICCs generally provide a simpler, less intrusive option, potentially associated with reduced mechanical complications and better patient comfort. Their smaller size may reduce the incidence of thrombosis, a common complication associated with indwelling vascular devices[10,11]. Conversely, double-lumen PICCs enable concurrent infusions of incompatible solutions, a necessity in certain complex medical scenarios[12]. This dual capability, while medically advantageous, poses concern due to the increased diameter of the catheter, potentially increasing the risk of vascular complications such as thrombosis[13,14].
Existing literature reflects the ongoing debate over the optimal choice of catheter lumen configuration, emphasizing the need for evidence-based guidelines to inform practice[15,16]. Previous studies have examined various aspects of PICC usage, from insertion techniques to complication management. However, comparative data specifically addressing the performance of single-lumen vs double-lumen PICCs within bundled care frameworks in patients undergoing digestive surgery are limited.
This retrospective cohort study focuses on evaluating clinical outcomes and patient-reported experiences with single-lumen and double-lumen PICCs in a digestive surgical setting, underpinned by a robust bundled care strategy.
This retrospective cohort study involved 249 patients who visited the digestive surgery department at the Quzhou Affiliated Hospital of Wenzhou Medical University, Quzhou People’s Hospital between January 2021 and June 2024. The patients utilized either single-lumen or double-lumen PICCs in bundled care contexts. They were categorized into two groups: Single-lumen group (117) and double-lumen group (132). Patient information was collected from the hospital’s case system. De-identified patient data were employed to ensure that no potential harm could come to the patients, thus allowing for a waiver of informed consent. The Ethics Review Committee of the Quzhou Affiliated Hospital of Wenzhou Medical University, Quzhou People’s Hospital approved the exemption and the research, ensuring compliance with applicable regulatory and ethical standards.
Inclusion criteria: (1) Aged 18 years or older; (2) Requiring long-term infusion therapy or nutritional support during hospitalization, aligning with clinical indications for PICC use[1]; (3) Use of single-lumen or double-lumen PICCs for more than 1 week[17]; (4) Availability of complete clinical data; and (5) Regular completion of follow-up visits.
The exclusion criteria: (1) Pregnant or lactating women; (2) Allergies to PICC materials; (3) Severe coagulation dysfunction presenting a high risk of bleeding[18]; (4) A recent history of upper limb deep vein thrombosis; (5) Diagnosis of neurological disorders or abnormal mental and cognitive states; and (6) An expected survival period of less than 3 months.
A 4Fr single-lumen PICC kit and accessories (Bard, United States, model: 3174118) were utilized in the single-lumen group, whereas a 5Fr double-lumen kit and accessories (Bard, United States, model: 3275118) were used in the double-lumen group. Both groups underwent the same catheter insertion and maintenance procedures.
During catheter insertion, the patients were positioned supine. Using ultrasound guidance, an upper arm vein was selected, and catheter length and arm circumference were measured. The upper arm was abducted at a 90° angle. The area was disinfected and draped, sterile gloves and an ultrasound probe cover were used, and each lumen of the catheter was pre-flushed with saline. The guidewire was retracted, and the catheter length was trimmed to 1 cm less than the predicted length. Ultrasound was used again to evaluate the vein, and a tourniquet was applied. The left hand held the probe to display the optimal vascular image, whereas the right hand held the puncture needle at a 60°-70° angle to the elbow. Once blood return was observed, the guidewire was advanced at approximately 20 cm. The puncture needle was withdrawn, and the Seldinger technique was employed. The puncture site was locally anesthetized, and the skin was dilated before advancing the dilator and sheath along the guidewire into the vein. The dilator was removed, and the catheter was gently introduced to the desired length. Ultrasound confirmed correct catheter tip placement, and the supporting guidewire and sheath were removed. Blood return was assessed with a syringe filled with saline, followed by pulsatile flushing of the lumen, closure with a lock, and positive pressure sealing with heparin saline. Hemostasis was achieved by compressing the puncture site, followed by securing the catheter. An X-ray was taken post-procedure to confirm catheter placement.
Regular maintenance observations were conducted post-insertion. For the first 24 hours, observations were performed once and then weekly. During maintenance, the PICC line’s end was secured with tape. The old dressing was removed from the bottom upward, and the wound was disinfected with iodine, starting from the center and moving outward in a circular motion without retraction. The disinfection area had a diameter of more than 10 cm, and the part of the catheter outside the body required disinfection. Once the iodine dried, de-iodination with alcohol was performed in a circular outward motion, covering an area larger than that disinfected with iodine. After the alcohol evaporated and dried, sterile paper tape strips (Smith & Nephew, model: IV3000) were applied horizontally to secure the fixation wings. Transparent dressings (Smith & Nephew, model: IV3000) were then used to cover the puncture site and the surrounding 10 cm of skin, with two additional paper tape strips used to cross-fix the line external to the dressing. The positive pressure connector was replaced. The catheter was flushed with 10 mL of saline pulse and then sealed with 4 mL of heparin saline. A 3M wound dressing (3M, United States, model: 3662CU) was used to cover the positive pressure connector. During each maintenance session, the patients were monitored for signs of infection, thrombosis, displacement, or occlusion.
Ultrasound examination of the upper extremity veins was conducted using high-frequency linear transducers (10-14 MHz) to ensure consistency and accuracy in thrombosis assessment. The presence of intraluminal echogenic material within a vein, causing partial or complete obstruction of blood flow, was considered indicative of thrombosis. Images were reviewed by two independent radiologists to minimize bias. In cases where clinical symptoms suggested thrombosis but ultrasound findings were inconclusive, further imaging methods, such as X-rays, were considered. These criteria were applied consistently across all patients to ensure reliable and comparable thrombosis assessments.
Both groups received a bundled care approach comprising the following components:
Formation of a bundled care team: A specialized team was established, and team members underwent training and assessment on the bundled care model. The training emphasized the risk factors and stages associated with PICC-related complications such as infections, occlusions, and dislodgement. A bundled care protocol was developed, requiring team members to strictly adhere to its principles and measures when providing patient care.
Establishment of standardized PICC procedures: Standardized procedures for the use and sealing of PICCs were implemented. Nursing staff were required to rigorously apply sterile techniques and carefully monitor the catheter insertion site and surrounding skin. Disinfection was performed from the inside out to minimize the risk of prolonged catheter exposure.
Enhanced skill training: A comprehensive set of evaluation standards for PICC procedures was developed. Nursing staff received training to master catheter assessment methods, procedural details, and precautions before using the catheter. Only those who passed the assessment were permitted to perform catheter care procedures, ensuring standardized operations.
Focus on psychological and nutritional interventions: The psychological status of the patients with PICCs was evaluated, and any negative emotions were addressed. Patient feedback was considered to develop effective nutritional support plans tailored to their needs.
Regular evaluation and update of care plans: The bundled care approach was routinely assessed and summarized. The latest medical evidence was considered for continuous updates and improvements to the care plan, ensuring patients received optimal care outcomes.
Three weeks post-catheterization, two vials of fasting venous blood were collected. One vial was drawn into an EDTA-K2 anticoagulant tube and analyzed using an automated blood cell analyzer (Mindray BC6800, Shenzhen Mindray Bio-Medical Electronics Co., China) to assess hemoglobin and C-reactive protein levels. The second vial was collected in a standard vacuum tube, allowed to clot, and then processed in a refrigerated high-speed centrifuge (TLD 12A, Hunan Xiangxi Scientific Instrument Factory, China) at 3000 rpm for 10 minutes. The serum was isolated and analyzed using a fully automated biochemical analyzer (Cobas 8000, Roche, Switzerland) to measure the levels of total cholesterol, high-density lipoprotein (HDL), low-density lipoprotein (LDL), triglycerides, blood glucose, and serum creatinine.
Respiratory function was assessed using the Vmax Spectra 229D cardiopulmonary function testing system (Becton, Dickinson and Company, United States). The patients’ normal breathing rate was recorded initially. The patients were instructed to inhale maximally and then exhale as forcefully and as quickly as possible, with the volume exhaled in the first second recorded as forced expiratory volume in 1 second (FEV1). Following a maximal inhale, the total volume exhaled as quickly and completely was recorded as forced vital capacity (FVC). The maximum flow rate achieved during forced expiration, known as peak expiratory flow (PEF), was documented. The patients then inhaled a gas mixture containing trace carbon monoxide and immediately exhaled. The concentration of carbon monoxide in the exhaled air was analyzed to determine the diffusing capacity of the lungs for carbon monoxide (DLCO).
Three weeks after catheter insertion, the patients’ heart rate variability, blood pressure variability, and blood oxygen saturation were recorded using a real-time electrocardiogram monitor (OSEN8000, Shenyang). The mean arterial pressure (MAP) was calculated using the following formula: MAP = (2 × diastolic pressure + systolic pressure)/3.
Central venous pressure (CVP) was measured through a catheter connected to a central vein. The pressure measuring tube was positioned so that its zero point aligned horizontally with the midpoint of the right atrium. Before insertion, the connecting tube and venous catheter were filled with fluid, and air bubbles were expelled. The pressure tube was filled with fluid, with the liquid level set higher than the expected venous pressure. The three-way stopcock was adjusted to connect the pressure tube to the PICC, enabling pressure measurement. When not measuring, the stopcock was turned to connect the infusion bottle to the venous catheter, which provided additional fluids and maintained catheter patency.
Three weeks following catheter placement, a survey questionnaire was administered to assess patient satisfaction across four dimensions: Comfort, satisfaction with care, satisfaction with treatment outcomes, and pain level. The first three dimensions were scored on a scale of up to 10 points, with higher scores reflecting greater satisfaction. The pain level was scored up to 10 points, evaluating the pain experienced during the catheterization process, and a higher pain score indicated a more significant impact on the patient’s normal daily activities.
Data analysis was conducted using SPSS (version 29.0) statistical software (SPSS Inc., Chicago, IL, United States). Categorical data were expressed as counts and percentages [n (%)]. For continuous data with a normal distribution, results were presented as mean ± SD. T-test was used for data analysis, and χ2 test was used for count data. A P value of less than 0.05 was considered statistically significant.
The mean ages were 55.23 ± 10.12 years for the single-lumen group and 56.57 ± 11.34 years for the double-lumen group, with no statistically significant difference (P = 0.33; Table 1). The body mass index averaged 23.78 ± 3.45 kg/m² in the single-lumen group and 23.84 ± 3.67 kg/m² in the double-lumen group (P = 0.907). The gender distribution was similar between the two groups, with females comprising 55.56% in the single-lumen group and 52.27% in the double-lumen group (P = 0.604). Smoking history, drinking history, prevalence of hypertension, and diabetes showed no significant differences between the groups (P > 0.05). Educational level attainment, characterized as junior college graduate or lower vs college graduate or higher, was not significantly different (P = 0.293). Marital status did not vary significantly, with 82.91% married in the single-lumen group and 78.79% in the double-lumen group (P = 0.411). Ethnicity distribution was similar, with the majority being Han in both groups (P = 0.723). Overall, no significant demographic differences were observed between the two groups, ensuring comparability for further efficacy evaluation.
| Single-lumen group | Double-lumen group | t/χ² | P value | |
| Age (years) | 55.23 ± 10.12 | 56.57 ± 11.34 | 0.976 | 0.33 |
| Body mass index (kg/m2) | 23.78 ± 3.45 | 23.84 ± 3.67 | 0.117 | 0.907 |
| Female/male | 65 (55.56)/52 (44.44) | 69 (52.27)/63 (47.73) | 0.269 | 0.604 |
| Smoking history (yes/no) | 32 (27.35)/85 (72.65) | 33 (25)/99 (75) | 0.178 | 0.673 |
| Drinking history (yes/no) | 41 (35.04)/76 (64.96) | 40 (30.3)/92 (69.7) | 0.635 | 0.426 |
| Hypertension (yes/no) | 26 (22.22)/91 (77.78) | 29 (21.97)/103 (78.03) | 0.002 | 0.962 |
| Diabetes (yes/no) | 21 (17.95)/96 (82.05) | 19 (14.39)/113 (85.61) | 0.581 | 0.446 |
| Educational level (junior college graduate or lower/college graduate or higher) | 75 (64.1)/42 (35.9) | 76 (57.58)/56 (42.42) | 1.107 | 0.293 |
| Marital status (married/unmarried) | 97 (82.91)/20 (17.09) | 104 (78.79)/28 (21.21) | 0.676 | 0.411 |
| Ethnicity (Han/other) | 107 (91.45)/10 (8.55) | 119 (90.15)/13 (9.85) | 0.125 | 0.723 |
In the single-lumen group, 75.21% underwent surgery for gastrointestinal tumors; 15.38% had procedures for intestinal obstruction; and 3.42% were treated for gastrointestinal trauma, 3.42% for gastroduodenal ulcer, and 2.56% for abdominal tuberculosis. In the double-lumen group, 73.48% underwent surgery for gastrointestinal tumors and 15.15% had procedures for intestinal obstruction, 4.55% for gastrointestinal trauma, 3.79% for gastroduodenal ulcer, and 3.03% for abdominal tuberculosis. No statistically significant differences were observed when evaluating the types of surgeries undergone by patients in the single-lumen and double-lumen groups within gastrointestinal surgical contexts (χ2 = 0.295, P = 0.990; Table 2). These proportions indicate a comparable distribution of surgery types between the two study groups.
| Single-lumen group (n = 117) | Double-lumen group (n = 132) | χ² | P value | |
| Gastrointestinal tumors | 88 (75.21) | 97 (73.48) | 0.295 | 0.990 |
| Intestinal obstruction | 18 (15.38) | 20 (15.15) | ||
| Gastrointestinal trauma | 4 (3.42) | 6 (4.55) | ||
| Gastroduodenal ulcer | 4 (3.42) | 5 (3.79) | ||
| Abdominal tuberculosis | 3 (2.56) | 4 (3.03) |
The mean total cholesterol levels were 190.45 ± 35.6 mg/dL in the single-lumen group and 192.77 ± 35.67 mg/dL in the double-lumen group (P = 0.61; Table 3). The HDL values averaged 55.23 ± 13.33 mg/dL for the single-lumen group and 54.12 ± 12.78 mg/dL for the double-lumen group (P = 0.504). The LDL levels were 110.65 ± 29.84 mg/dL and 112.45 ± 30.12 mg/dL for the single-lumen and double-lumen groups, respectively (P = 0.636). The triglyceride levels were comparable, with 140.32 ± 40.67 mg/dL in the single-lumen group and 138.9 ± 42.75 mg/dL in the double-lumen group (P = 0.789). The fasting blood sugar levels were 102.38 ± 12.45 mg/dL for the single-lumen group and 101.67 ± 11.98 mg/dL for the double-lumen group (P = 0.644). The C-reactive protein levels were 3.45 ± 1.67 mg/L and 3.56 ± 1.70 mg/L for the single-lumen and double-lumen groups, respectively (P = 0.595). For hemoglobin A1c, the single-lumen group had a mean of 5.87% ± 0.80% compared with 5.82% ± 0.75% in the double-lumen group (P = 0.658). Lastly, the serum creatinine levels were similar, with 1.01 ± 0.18 mg/dL in the single-lumen group and 0.98 ± 0.20 mg/dL in the double-lumen group (P = 0.33). These results indicate no significant differences in biochemical parameters between the two groups.
| Single-lumen group (n = 117) | Double-lumen group (n = 132) | t | P value | |
| Total cholesterol (mg/dL) | 190.45 ± 35.6 | 192.77 ± 35.67 | 0.511 | 0.61 |
| HDL (mg/dL) | 55.23 ± 13.33 | 54.12 ± 12.78 | 0.669 | 0.504 |
| LDL (mg/dL) | 110.65 ± 29.84 | 112.45 ± 30.12 | 0.474 | 0.636 |
| Triglycerides (mg/dL) | 140.32 ± 40.67 | 138.9 ± 42.75 | 0.268 | 0.789 |
| Fasting blood sugar (mg/dL) | 102.38 ± 12.45 | 101.67 ± 11.98 | 0.462 | 0.644 |
| C-reactive protein (mg/L) | 3.45 ± 1.67 | 3.56 ± 1.70 | 0.532 | 0.595 |
| Hemoglobin A1c (%) | 5.87 ± 0.80 | 5.82 ± 0.75 | 0.444 | 0.658 |
| Serum creatinine (mg/dL) | 1.01 ± 0.18 | 0.98 ± 0.20 | 0.976 | 0.33 |
The FEV1s were 3.21 ± 0.58 L in the single-lumen group and 3.15 ± 0.6 L in the double-lumen group (P = 0.422; Table 4). FVC was measured at 4.05 ± 0.72 L for the single-lumen group and 4 ± 0.75 L for the double-lumen group (P = 0.542). The FEV1/FVC ratio was slightly different at 79.26% ± 5.34% for the single-lumen group and 78.92% ± 5.41% for the double-lumen group (P = 0.621). PEF showed no significant difference at 480.23 ± 50.12 L/minute in the single-lumen group and 475.89 ± 49.78 L/minute in the double-lumen group (P = 0.494). The DLCOs, expressed as a percentage of the predicted value, were 85.12% ± 10.25% in the single-lumen group and 84.78% ± 10.15% in the double-lumen group (P = 0.791). The respiratory rate was similar between groups, with 16.22 ± 2.04 breaths/minute for the single-lumen group and 16.45 ± 2.10 breaths/minute for the double-lumen group (P = 0.383). These findings indicate no significant differences in respiratory function between the two groups.
| Single-lumen group (n = 117) | Double-lumen group (n = 132) | t | P value | |
| FEV1 (L) | 3.21 ± 0.58 | 3.15 ± 0.6 | 0.804 | 0.422 |
| FVC (L) | 4.05 ± 0.72 | 4 ± 0.75 | 0.611 | 0.542 |
| FEV1/FVC ratio (%) | 79.26 ± 5.34 | 78.92 ± 5.41 | 0.496 | 0.621 |
| PEF (L/minute) | 480.23 ± 50.12 | 475.89 ± 49.78 | 0.685 | 0.494 |
| DLCO (% predicted) | 85.12 ± 10.25 | 84.78 ± 10.15 | 0.265 | 0.791 |
| Respiratory rate (breaths/minute) | 16.22 ± 2.04 | 16.45 ± 2.10 | 0.873 | 0.383 |
The heart rate variations were 5.40 ± 1.30 beats/minute in the single-lumen group and 5.50 ± 1.40 beats/minute in the double-lumen group (P = 0.549; Table 5). The blood pressure variation averaged 3.40 ± 1.22 mmHg for the single-lumen group and 3.50 ± 1.30 mmHg for the double-lumen group (P = 0.557). The oxygen saturation levels were consistently high, recorded at 98.9% ± 0.53% for the single-lumen group and 98.87% ± 0.70% for the double-lumen group (P = 0.767). The MAPs were 92 ± 7.09 mmHg in the single-lumen group and 93.51 ± 6.50 mmHg in the double-lumen group, showing a trend but not reaching statistical significance (P = 0.08). CVP was comparable between groups, measuring 8.02 ± 1.56 cmH2O for the single-lumen group and 8.33 ± 1.60 cmH2O for the double-lumen group (P = 0.122). These results suggest that both catheter types maintain similar hemodynamic stability during catheterization.
| Single-lumen group (n = 117) | Double-lumen group (n = 132) | t/χ² | P value | |
| Heart rate variation (beats/minute) | 5.40 ± 1.30 | 5.50 ± 1.40 | 0.6 | 0.549 |
| Blood pressure variation (mmHg) | 3.40 ± 1.22 | 3.50 ± 1.30 | 0.588 | 0.557 |
| Oxygen saturation (%) | 98.9 ± 0.53 | 98.87 ± 0.70 | 0.297 | 0.767 |
| Mean arterial pressure (mmHg) | 92 ± 7.09 | 93.51 ± 6.50 | 1.756 | 0.08 |
| Central venous pressure (cmH2O) | 8.02 ± 1.56 | 8.33 ± 1.60 | 1.551 | 0.122 |
The catheterization duration was significantly shorter in the single-lumen group, averaging 12.5 ± 3.14 days than the 13.6 ± 4.50 days in the double-lumen group (P = 0.025; Figure 1). The single-lumen group exhibited a higher percentage of successful infusions, with a mean of 92.7% ± 5.32%, and the double-lumen group had a mean of 90.4% ± 6.60% (P = 0.003). By contrast, the mean catheter flow rate was similar between the two groups, measuring 110.98 ± 12.52 mL/minute for the single-lumen group and 111.34 ± 13.2 mL/minute for the double-lumen group, showing no significant difference (P = 0.827). These results indicate that single-lumen PICCs provide more efficient catheterization in terms of duration and infusion success than double-lumen PICCs.
The single-lumen group reported higher comfort scores (8.40 ± 1.20) than the double-lumen group (7.90 ± 1.50, P = 0.004) and greater satisfaction with care (9.00 ± 0.90 vs 8.70 ± 1.00, P = 0.014; Figure 2). No significant difference was found in satisfaction with treatment results, with scores of 8.60 ± 0.90 for the single-lumen group and 8.50 ± 1.10 for the double-lumen group (P = 0.444). The single-lumen group reported significantly lower pain levels (2.90 ± 0.70) than the double-lumen group (3.20 ± 0.80, P = 0.002). These findings suggest that patients with single-lumen PICCs experienced higher overall comfort and satisfaction and lower pain levels those with double-lumen PICCs.
The infection rate was comparable between the two groups, with 3.42% in the single-lumen group and 3.03% in the double-lumen group (P = 1; Table 6). However, the thrombosis rate was significantly higher in the double-lumen group at 6.82% than in the single-lumen group at 0.85% (P = 0.039). The rates of dislodgement were similar, occurring in 2.56% of the single-lumen group and 3.03% of the double-lumen group (P = 1). The occlusion rates were 4.27% in the single-lumen group and 2.27% in the double-lumen group, showing no significant difference (P = 0.594). Overall, total complications occurred in 11.97% of the single-lumen group and 13.64% of the double-lumen group (P = 0.694). These results indicate a significantly higher risk of thrombosis in patients with double-lumen PICCs, whereas other complication rates were not significantly different between the groups.
| Single-lumen group (n = 117) | Double-lumen group (n = 132) | t/χ² | P value | |
| Infection rate | 4 (3.42) | 4 (3.03) | 0 | 1 |
| Thrombosis | 1 (0.85) | 9 (6.82) | 4.28 | 0.039 |
| Dislodgement | 3 (2.56) | 4 (3.03) | 0 | 1 |
| Occlusion | 5 (4.27) | 3 (2.27) | 0.285 | 0.594 |
| Total complications | 14 (11.97) | 18 (13.64) | 0.155 | 0.694 |
This study aimed to compare the efficacy and overall outcomes of single-lumen vs double-lumen PICCs among patients undergoing digestive surgery within the context of a bundled care protocol. A notable finding of this study was the higher incidence of thrombosis in the double-lumen PICC group than in the single-lumen group. The low threshold for noticing statistically significant differences in thrombosis rates despite the equivalence in most other complication rates suggests a physiological or anatomical rationale. Double-lumen catheters were typically bulkier, which may compromise venous blood flow more than single-lumen catheters[19,20]. The greater surface area and dual lumens likely contribute to an increase in potential for thrombogenicity. Hemodynamic disturbance, particularly in the early phase post-catheterization, may result from the larger diameter of double-lumen catheters, thereby influencing endothelial integrity and predisposing to thrombosis[21,22]. These findings have significant clinical relevance, emphasizing the importance of selecting the most appropriate catheter type to minimize patient risk.
Complication rates, such as infections, occlusions, and dislodgement, were statistically similar across the groups, suggesting that the bundled care interventions effectively maintained standards of care and minimized the risk of common catheter-associated complications. The study’s rigorous maintenance protocol, including regular disinfectant procedures and frequent line inspections, likely mitigated the impact of having an extra lumen in terms of infection risk. The bundled care approach, with standardized insertion and maintenance protocols, likely contributed to low and comparable infection rates, reinforcing the pivotal role of such measures in catheter management[22,23].
Patient satisfaction was another critical factor that this study examined. The satisfaction scores were notably higher in the single-lumen group, and this finding may be attributed to the less intrusive nature of these catheters. The patients reported higher comfort scores and lower pain levels during the catheterization process, perhaps due to the smaller catheter size. These subjective measures reflect the importance of considering patient comfort and perceived pain in clinical decisions and support the use of single-lumen catheters when medically feasible, especially in patients more sensitive to discomfort or undergoing longer treatments.
The compatibility of single-lumen PICCs with equal hemodynamic stability as double-lumen PICCs challenges the notion that more complex catheter systems provide marked advantages in terms of physiological metrics. Both groups demonstrated stable heart rates, blood pressure, and oxygen saturation levels, indicating that either catheter type could maintain cardiac and pulmonary sufficiency postoperatively. The lack of statistical significance in these parameters suggests that single-lumen catheters offer equivalent physiological support without the added risks associated with double-lumen systems.
The duration of catheterization presents an interesting angle in understanding efficiency in clinical practice. Single-lumen PICCs demonstrated shorter catheterization duration and higher infusion success rates. This efficiency gain may reflect easier management and less technical difficulty associated with single-lumen catheters. The smaller size and lesser mechanical complexity of single-lumen catheters facilitate quicker insertion, easier maintenance, and potentially fewer malfunctions or technical issues during use. This factor can enhance workflow efficiency in busy surgical settings where the reduction in procedural time is beneficial for patients and healthcare providers.
The examination of biochemical and respiratory parameters demonstrated that the lack of significant differences between groups underscores that both catheter types can effectively support the physiological requirements of patients undergoing digestive surgery. These similar outcomes suggest that the choice between single and double-lumen PICCs could prioritize considerations other than direct biochemical or respiratory impact such as comfort, risk of thrombosis, or specific requirements for concurrent infusions.
While the study data indicate that single-lumen PICCs performed better in terms of thrombosis rates, comfort, and procedural efficiency, recognizing the indispensable role of double-lumen PICCs in specific clinical scenarios is crucial. Double-lumen PICCs offer distinct advantages in situations where multiple concurrent infusions are required, such as simultaneous administration of parenteral nutrition, antibiotics, and chemotherapy. These catheters allow for si
Of particular relevance was the bundled care approach implemented for all patients that may have contributed to the consistently positive results across both PICC types. The structured interventions - emphasizing standardized proce
The context of bundled care enables healthcare workers to focus not only on clinical but also holistic aspects of patient care, such as providing psychological and nutritional support[28,29]. This aspect of care is paramount, particularly when dealing with patients undergoing major surgical interventions, because it addresses not only the immediate clinical interventions but also the broader health determinants known to influence recovery and patient satisfaction[30,31].
One limitation of this study is the absence of multivariate analyses to control for potential confounding factors such as type of surgery, medication regimen, and baseline health status. While significant differences in thrombosis rates and other outcomes were observed between the single-lumen and double-lumen PICC groups, the lack of adjustment for these confounders may limit the generalizability of the findings. Future studies should consider incorporating multivariate analyses to better account for these variables and provide more robust evidence regarding the comparative efficacy and safety of different PICC types. Another limitation is that this study focused on short-term complications (e.g., thrombosis and infection) only and did not assess catheter-related complications (e.g., catheter breaks and fibrous sheath formation) after long-term use (> 30 days). Future studies should include longer follow-up periods to capture these important outcomes and provide a more comprehensive understanding of the risks associated with different types of PICCs.
Ultimately, this study highlights the nuanced considerations required when selecting the appropriate PICC for each patient. The single-lumen PICC shows advantages in terms of comfort, procedural efficiency, and lower thrombosis risk, making it preferable when these factors are prioritized. However, double-lumen catheters still serve a crucial purpose in clinical scenarios where multiple concurrent infusions are necessary. The findings suggest that a tailored approach, evaluating individual patient needs, the anticipated duration of catheter use, and specific clinical circumstances, is essential for optimizing care outcomes[32,33].
While this study provides a comparative analysis of single-lumen vs double-lumen PICC efficacy within the bundled care context in patients undergoing digestive surgery, future research could further explore long-term outcomes and broader patient populations to validate and extend these findings. The emphasis on and further refinement of bundled care strategies likely continue to play a vital role in enhancing PICC-related care efficacy and patient satisfaction.
| 1. | Bae HS, Kim KY, Han YM. Comparison of complications between reverse-tapered and nontapered peripherally inserted central catheters. PLoS One. 2023;18:e0285445. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 2. | D'Arrigo S, Sandroni C, Cacciola S, Dell'Anna AM, Pittiruti M, Annetta MG, Colosimo C, Antonelli M. Are single-lumen 5Fr and triple-lumen 6Fr PICCs suitable for hemodynamic assessment by trans-pulmonary thermodilution? A pilot study. Ann Intensive Care. 2020;10:165. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 3. | Bayoumi MAA, van Rens MFPT, Chandra P, Masry A, D'Souza S, Khalil AM, Shadad A, Alsayigh S, Masri RM, Shyam S, Alobaidan F, Elmalik EE. Does the antimicrobial-impregnated peripherally inserted central catheter decrease the CLABSI rate in neonates? Results from a retrospective cohort study. Front Pediatr. 2022;10:1012800. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 13] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 4. | Chasseigne V, Buisson M, Serrand C, Leguelinel-Blache G, Kinowski JM, Goupil J, Beregi JP, Frandon J. Pharmaceutical Analysis of Peripherally Inserted Central Catheter Requests Increases the Use of Single-Lumen Catheters: A Prospective Pilot Study. J Patient Saf. 2022;18:e1238-e1242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 5. | Bahl A, Karabon P, Chu D. Comparison of Venous Thrombosis Complications in Midlines Versus Peripherally Inserted Central Catheters: Are Midlines the Safer Option? Clin Appl Thromb Hemost. 2019;25:1076029619839150. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 56] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 6. | Kee J, Mears SC, Edwards PK, Lowry Barnes C. Cost Analysis and Bundled Care of Hip and Knee Replacement. J Surg Orthop Adv. 2019;28:241-249. [PubMed] [DOI] [Full Text] |
| 7. | Mastrogianni M, Katsoulas T, Galanis P, Korompeli A, Myrianthefs P. The Impact of Care Bundles on Ventilator-Associated Pneumonia (VAP) Prevention in Adult ICUs: A Systematic Review. Antibiotics (Basel). 2023;12:227. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 38] [Article Influence: 12.7] [Reference Citation Analysis (0)] |
| 8. | Chen Q, Hu YL, Li YX, Huang X. Peripherally inserted central catheter placement in neonates with persistent left superior vena cava: Report of eight cases. World J Clin Cases. 2021;9:7944-7953. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 9. | Rivera J, Donohoe E, Deady-rooney M, Douglas M, Samaniego N. Implementing a Pressure Injury Prevention Bundle to Decrease Hospital-Acquired Pressure Injuries in an Adult Critical Care Unit: An Evidence-Based, Pilot Initiative. Wound Man Prev. 2020;66:20-28. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 30] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 10. | Thomsen SL, Boa R, Vinter-Jensen L, Rasmussen BS. Safety and Efficacy of Midline vs Peripherally Inserted Central Catheters Among Adults Receiving IV Therapy: A Randomized Clinical Trial. JAMA Netw Open. 2024;7:e2355716. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 24] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 11. | Alaiev D, Krouss M, Israilov S, Musser L, Talledo J, Mestari N, Uppal A, Madaline T, Cohen G, Bravo N, Cervantes M, Contractor D, Manchego PA, Chandra K, Zaurova M, Tsega S, Cho HJ. Nudging to select single-lumen over multiple-lumen peripherally inserted central catheters (PICCs) in a large safety net system. Infect Control Hosp Epidemiol. 2023;44:1381-1385. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 12. | Maki J, Sumie M, Ide T, Nagamatsu M, Matsushita K, Shirozu K, Higashi M, Yamaura K. A pressure-resistant peripherally inserted central catheter is as useful as a central venous catheter for rapid fluid infusion: an in vitro study. BMC Anesthesiol. 2022;22:205. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 13. | Byrne D, Penwarden L. Selection of Single- Versus Double-Lumen Peripherally Inserted Central Catheters and the Influence on Alteplase Use. J Infus Nurs. 2018;41:118-121. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 14. | Fukuda S, Nakajima K, Miyazaki Y, Takahashi T, Kurokawa Y, Yamasaki M, Miyata H, Takiguchi S, Mori M, Doki Y. Use of double-lumen peripherally inserted central catheters for safer perioperative management of esophageal cancer patients. J Vasc Access. 2015;16:338-343. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 15. | Ho C, Spry C. Central Venous Access Devices (CVADs) and Peripherally Inserted Central Catheters (PICCs) for Adult and Pediatric Patients: A Review of Clinical Effectiveness and Safety [Internet]. Ottawa (ON): Canadian Agency for Drugs and Technologies in Health; 2017. [PubMed] |
| 16. | Pitiriga V, Bakalis J, Theodoridou K, Kanellopoulos P, Saroglou G, Tsakris A. Lower risk of bloodstream infections for peripherally inserted central catheters compared to central venous catheters in critically ill patients. Antimicrob Resist Infect Control. 2022;11:137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 36] [Reference Citation Analysis (0)] |
| 17. | Trautman K, Kobayashi T, McPherson C, Brust K. Defaulting peripherally inserted central catheter (PICC) orders to single lumen: A quality improvement initiative at a Midwestern academic center 2022-2023. Antimicrob Steward Healthc Epidemiol. 2023;3:e242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 18. | OʼMalley C, Sriram S, White M, Polinski C, Seng C, Schreiber MD. Feasibility and Outcomes Associated With the Use of 2.6-Fr Double-Lumen PICCs in Neonates. Adv Neonatal Care. 2019;19:E3-E8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 19. | Luo H, Jin C, Li X, Jiang Y, Zhou J. Quantified versus willful handgrip exercises for the prevention of PICC-related thrombosis: A meta-analysis and systematic review. Medicine (Baltimore). 2023;102:e32706. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 20. | Meng F, Fan S, Guo L, Jia Z, Chang H, Liu F. Incidence and risk factors of PICC-related thrombosis in breast cancer: a meta-analysis. Jpn J Clin Oncol. 2024;54:863-872. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 9] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 21. | Oza-Gajera BP, Davis JA, Farrington C, Lerma EV, Moossavi S, Sheta MA, Dwyer A, Almehmi A. PICC line management among patients with chronic kidney disease. J Vasc Access. 2023;24:329-337. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 10] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 22. | Sánchez Cánovas M, García Torralba E, Blaya Boluda N, Sánchez Saura A, Puche Palao G, Sánchez Fuentes A, Martínez Montesinos L, Poveda Ganga C, García Tomas L, Bayona Jiménez J, Cos Zapata Á, Muñoz Jurado CM, Pina Mingorance I, Caravaca Hernández MA, Vicente García V, Ayala de la Peña F. Thrombosis and infections associated with PICC in onco-hematological patients, what is their relevance? Clin Transl Oncol. 2024;26:3226-3235. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 23. | Toor H, Farr S, Savla P, Kashyap S, Wang S, Miulli DE. Prevalence of Central Line-Associated Bloodstream Infections (CLABSI) in Intensive Care and Medical-Surgical Units. Cureus. 2022;14:e22809. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 16] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 24. | Mitbander UB, Geer MJ, Taxbro K, Horowitz JK, Zhang Q, O'Malley ME, Ramnath N, Chopra V. Patterns of use and outcomes of peripherally inserted central catheters in hospitalized patients with solid tumors: A multicenter study. Cancer. 2022;128:3681-3690. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 18] [Reference Citation Analysis (0)] |
| 25. | Siddiqi A, White PB, Mistry JB, Gwam CU, Nace J, Mont MA, Delanois RE. Effect of Bundled Payments and Health Care Reform as Alternative Payment Models in Total Joint Arthroplasty: A Clinical Review. J Arthroplasty. 2017;32:2590-2597. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 176] [Cited by in RCA: 201] [Article Influence: 22.3] [Reference Citation Analysis (0)] |
| 26. | Vogel JP, Nguyen PY, Ramson J, De Silva MS, Pham MD, Sultana S, McDonald S, Adu-Bonsaffoh K, McDougall ARA. Effectiveness of care bundles for prevention and treatment of postpartum hemorrhage: a systematic review. Am J Obstet Gynecol. 2024;231:67-91. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 24] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 27. | Weil AR. Patient Costs, Bundled Payment, And More. Health Aff (Millwood). 2020;39:7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 28. | Barinaga G, Chambers MC, El-Othmani MM, Siegrist RB, Saleh KJ. Affordable Care Organizations and Bundled Pricing: A New Philosophy of Care. Orthop Clin North Am. 2016;47:707-716. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 29. | Boston-Fleischhauer CA. The Bundled Care Disruption. J Nurs Adm. 2017;47:192-194. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 30. | Curtin BM, Russell RD, Odum SM. Bundled Payments for Care Improvement: Boom or Bust? J Arthroplasty. 2017;32:2931-2934. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 50] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 31. | Gold PA, Magnuson JA, Venkat N, Krueger CA, Courtney PM. Life After BPCI: High Quality Total Knee and Hip Arthroplasty Care Can Still Exist Outside of a Bundled Payment Program. J Arthroplasty. 2022;37:1241-1246. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
| 32. | Swaminathan L, Flanders S, Horowitz J, Zhang Q, O'Malley M, Chopra V. Safety and Outcomes of Midline Catheters vs Peripherally Inserted Central Catheters for Patients With Short-term Indications: A Multicenter Study. JAMA Intern Med. 2022;182:50-58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 81] [Article Influence: 20.3] [Reference Citation Analysis (0)] |
| 33. | Mielke D, Wittig A, Teichgräber U. Peripherally inserted central venous catheter (PICC) in outpatient and inpatient oncological treatment. Support Care Cancer. 2020;28:4753-4760. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 71] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/