Published online Sep 27, 2025. doi: 10.4240/wjgs.v17.i9.107139
Revised: April 11, 2025
Accepted: July 18, 2025
Published online: September 27, 2025
Processing time: 192 Days and 7.7 Hours
Inferior mesenteric arteriovenous fistula (IMAVF) is an uncommon circulatory malformation with few reported instances. It entails a direct arteriovenous com
Over a 10-year period, only two cases of IMAVF were encountered. The initial case involved a 56-year-old male without notable prior medical conditions who experienced intermittent lower abdominal discomfort, diarrhea, and hemato
These cases emphasize the need to evaluate for vascular abnormalities in indi
Core Tip: Over the past 10 years, we have encountered this rare disease twice. Our initial experience enabled a faster diagnosis and treatment in the second case. We found that recurrent intra-abdominal infection and inflammation may lead to the development of an inferior mesenteric arteriovenous fistula and serve as key indicators in diagnosing ischemic colitis of unknown origin. Although surgical resection may offer a definitive solution, timely diagnosis could make endovascular intervention a viable alternative.
- Citation: Moon YJ, Lee SH. Inferior mesenteric arteriovenous fistula: Two case reports. World J Gastrointest Surg 2025; 17(9): 107139
- URL: https://www.wjgnet.com/1948-9366/full/v17/i9/107139.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v17.i9.107139
An arteriovenous fistula (AVF) is a pathological connection that allows blood to flow directly from the arterial to the venous system, circumventing the capillary bed. These fistulas may develop from congenital malformations, medical interventions or trauma, or occur without a clear underlying cause[1,2]. Congenital AVFs arise when primitive vascular structures fail to correctly evolve into separate arterial and venous systems during embryogenesis. Disruption of an aneurysm near major vessels may also give rise to an AVF[3]. Iatrogenic AVFs involving the inferior mesenteric vessels have been identified as complications associated with interventions involving the left colon and its vascular supply[4,5]. Traumatic AVFs can result from either blunt trauma or penetrating injuries[6]. In certain instances, AVFs emerge without an identifiable cause and are classified as idiopathic[7,8]. Although there are several published reports of AVFs involving vessels of the portal and splanchnic circulation, cases affecting the inferior mesenteric artery and vein remain exceedingly rare[1]. This case series presents two patients diagnosed with idiopathic inferior mesenteric AVF (IMAVF) over a 10-year period. Both cases were associated with ischemic colitis and were successfully managed with surgical excision. These cases highlight the clinical challenges in diagnosing and managing IMAVF and contribute to the limited literature on this rare vascular anomaly.
Case 1: In December 2014, a 56-year-old man presented with lower abdominal discomfort, loose stools, and intermittent hematochezia persisting for several months.
Case 2: In June 2024, a 76-year-old woman presented to the emergency department at our institution with left lower abdominal pain and hematochezia.
Case 1: The abdominal pain, mainly localized in the left lower quadrant, was intermittent and often cramp-like. The pain occasionally intensified after meals but did not fully resolve with defecation. Initially, the diarrhea was watery and non-bloody, occurring several times daily, but progressed to include hematochezia. No associated symptoms such as fever, nausea, or vomiting were reported. Despite persistent symptoms, no significant weight loss or change in appetite was noted.
Case 2: She had experienced multiple episodes of similar abdominal pain in the past; however, hematochezia ac
Case 1: The patient had previously been in good health with no known underlying conditions.
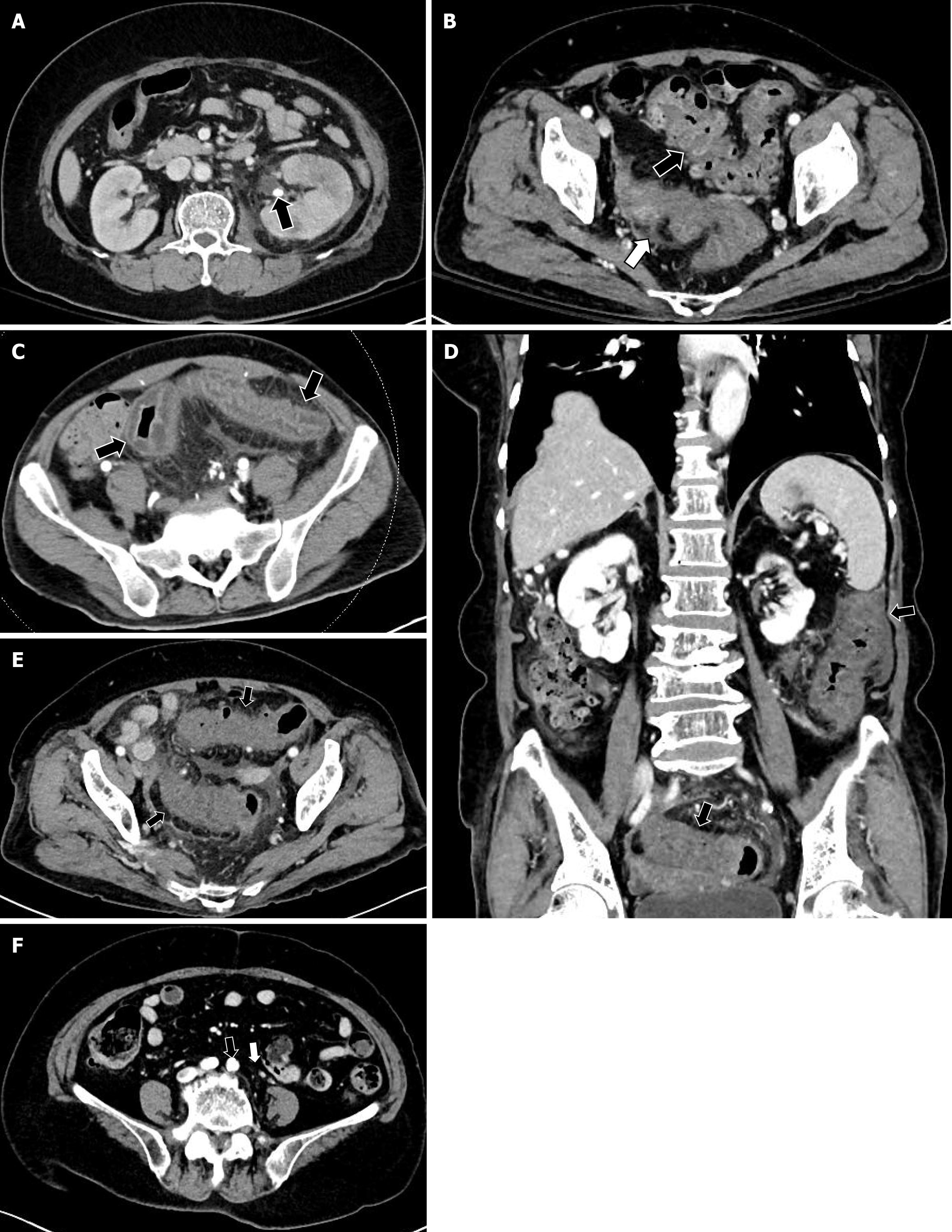
Case 2: She had a history of recurrent left-sided pyelonephritis and diverticulitis of the ascending and sigmoid colons over the past 10 years, requiring multiple hospital admissions and treatments. Treatment for acute pyelonephritis with a stone in the left renal pelvis was first provided in 2014, with two subsequent hospitalizations for the same condition (Figure 1). Hospitalization occurred twice in 2020 for diverticulitis of the ascending and sigmoid colons, which improved with fasting and antibiotic therapy (Figure 1).
Case 1: Family history was unremarkable, and the patient recalled no prior similar symptoms, abdominal surgery, or trauma.
Case 2: No relevant family history was reported. Recent travel, antibiotic use, or consumption of unusual foods was denied by the patient.
Case 1: Tenderness and reduced bowel sounds were noted in the left lower quadrant. Digital rectal examination revealed no abnormalities or clinical signs of portal hypertension.
Case 2: Diffuse tenderness was observed in the lower abdomen, most pronounced in the left lower quadrant, while costovertebral angle tenderness remained minimal bilaterally. Digital rectal examination revealed no abnormalities.
Case 1: Laboratory tests indicated an elevated erythrocyte sedimentation rate of 120 mm/hour (reference range, 1-20 mm/hour) and a high-sensitivity C-reactive protein level of 3.3 mg/dL (reference range, 0-0.500 mg/dL), with other results within normal limits. Additionally, tests for the infectious causes of diarrhea yielded no significant findings.
Case 2: Blood tests revealed elevated inflammatory markers, including an erythrocyte sedimentation rate of 61 mm/hour (reference range, 1-20 mm/hour) and a high-sensitivity C-reactive protein level of 10.05 mg/dL (reference range, 0-0.500 mg/dL), with other results within normal limits. Stool examination identified no specific infectious pathogens responsible for the diarrhea or hematochezia.
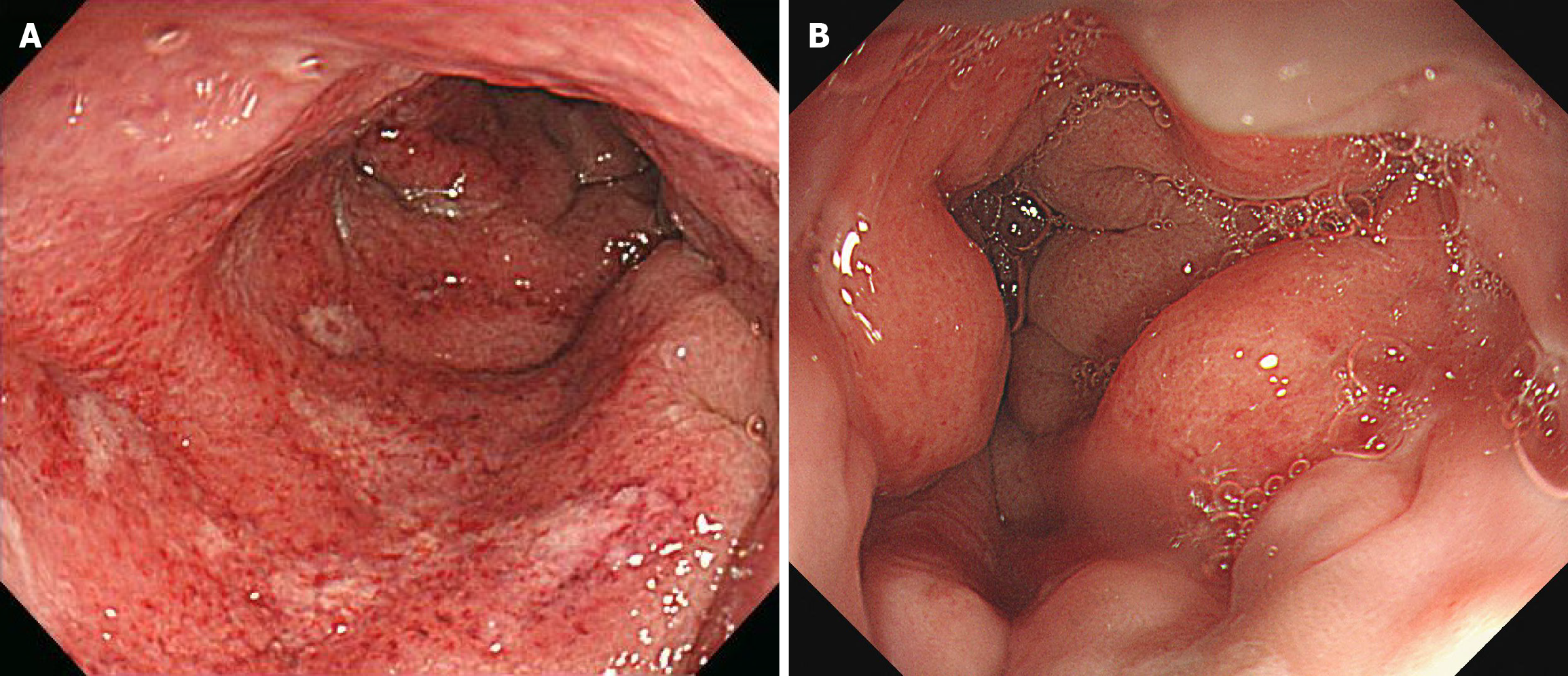
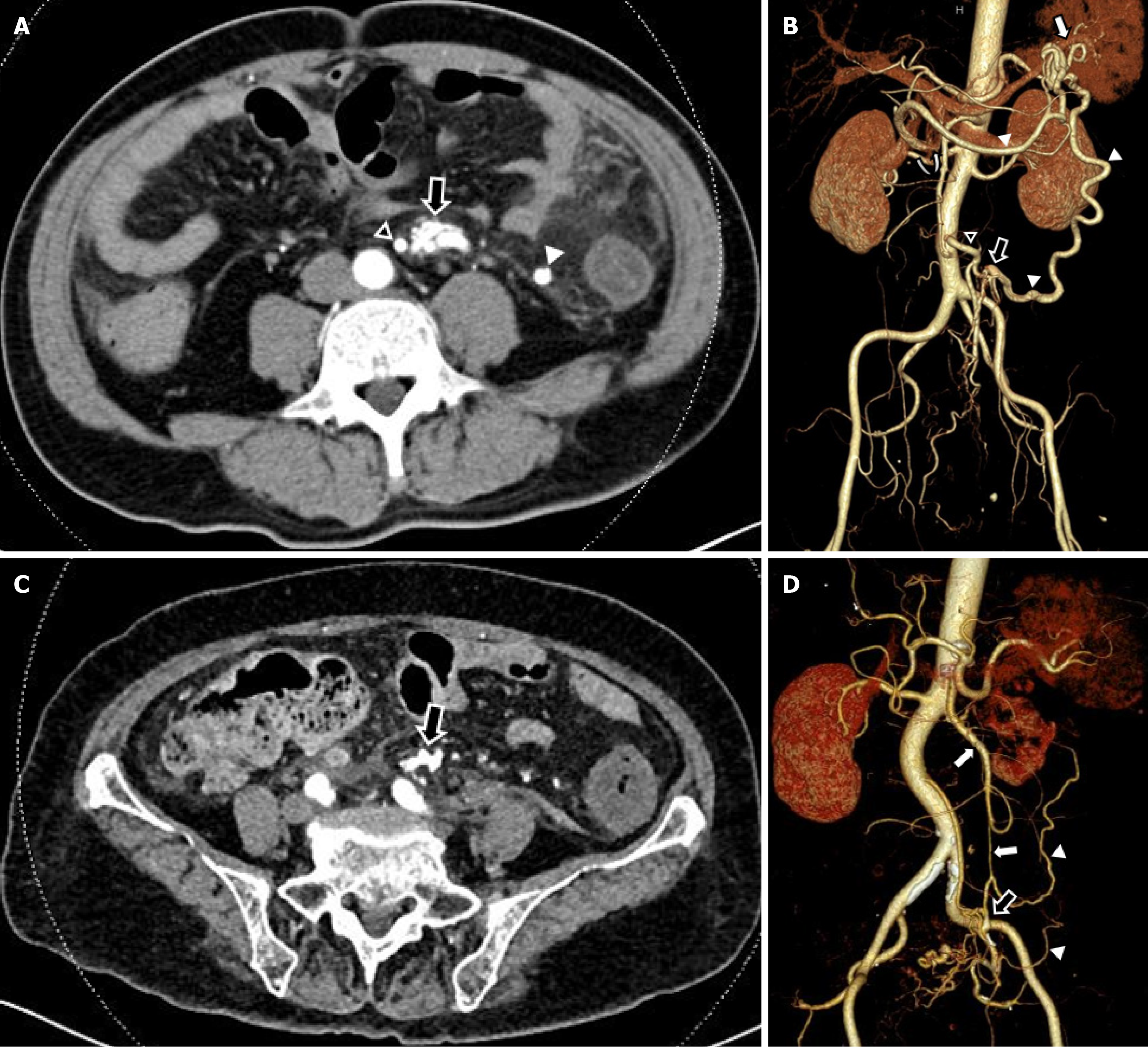
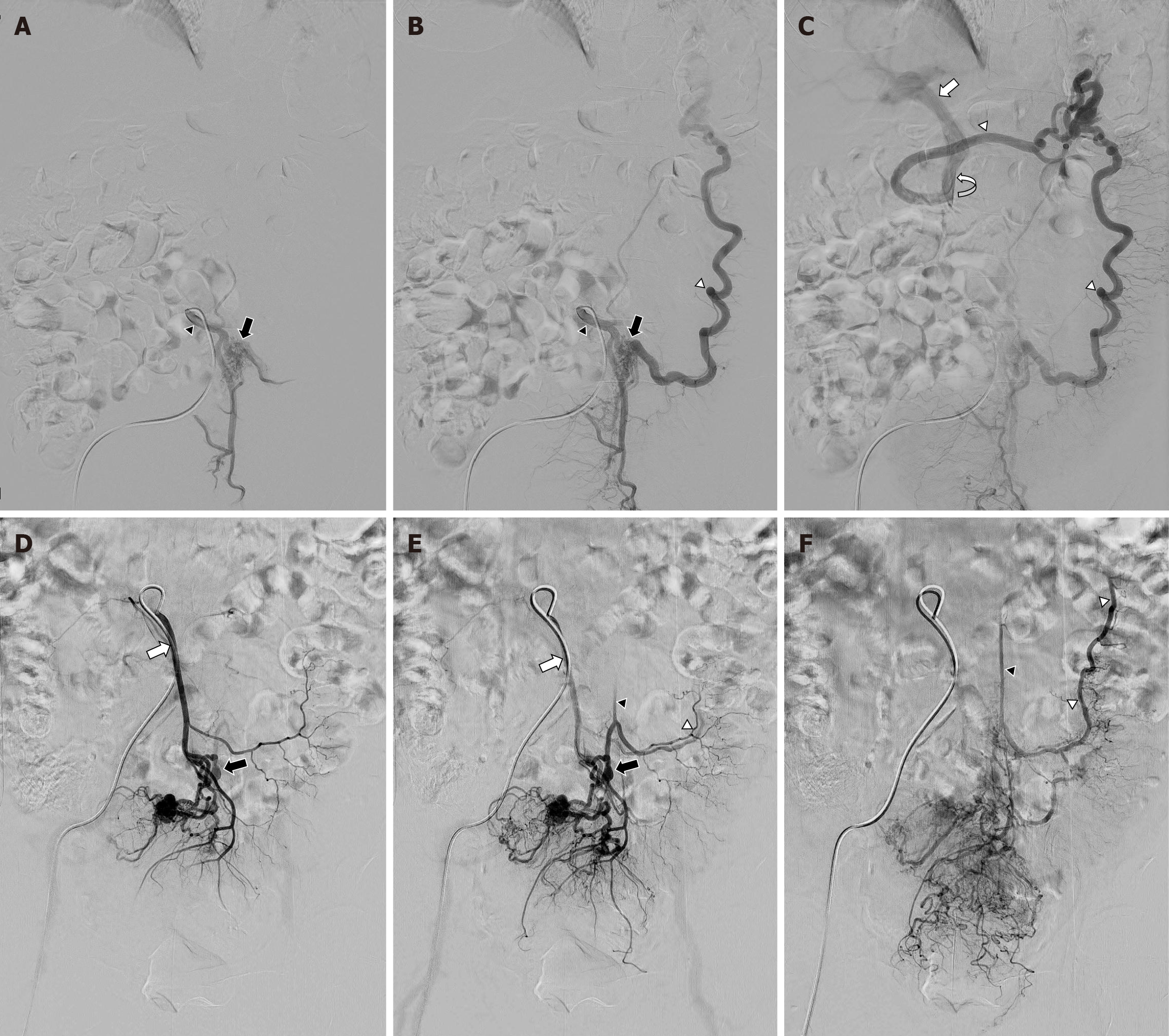
Case 1: Colonoscopy revealed mucosal abnormalities suggestive of active inflammatory colitis, involving the left colon up to the splenic flexure. Multiple round ulcers of varying sizes, covered with whitish exudates, were noted in the distal segment of the left colon (Figure 2). Multi-detector computed tomography (MDCT) revealed segmental abnormalities in the left colon, suggestive of an extensive inflammatory process, predominantly affecting the sigmoid colon (Figure 1). Tests for infectious causes produced negative results. Suspecting mesenteric ischemia, MDCT angiography was conducted, revealing an abnormal serpentine arterial configuration originating from an inferior mesenteric artery, along with flow compromise in the main trunk of the inferior mesenteric vein. Venous drainage was rerouted through a significantly dilated marginal vein, which emptied into the portal circulation during the arterial phase (Figure 3). An inferior mesenteric artery angiogram was performed to confirm the diagnosis and evaluate treatment options. An IMAVF was identified, with numerous slender, tortuous arterial branches originating from both proximal and distal segments of the inferior mesenteric artery. A single dominant draining vein was observed, directing blood into the superior me
Case 2: MDCT revealed ischemic changes throughout the left colon (Figure 1). Sigmoidoscopy disclosed edema and inflammation beginning 7 cm above the anal verge (Figure 2). Advancement of the endoscope was limited to 23 cm above the anal verge due to mucosal edema and patient discomfort. MDCT angiography revealed prominent vessels and early draining veins in the sigmoid colon mesentery, along with wall thickening in the left colon, suggestive of an AVF or malformation (Figure 3). Selective imaging demonstrated abnormal arteriovenous communication within a branch of the inferior mesenteric circulation, along with early opacification and a beaded contour of the corresponding vein (Figure 4).
The final diagnoses were: (1) Ischemic colitis; and (2) IMAVF.
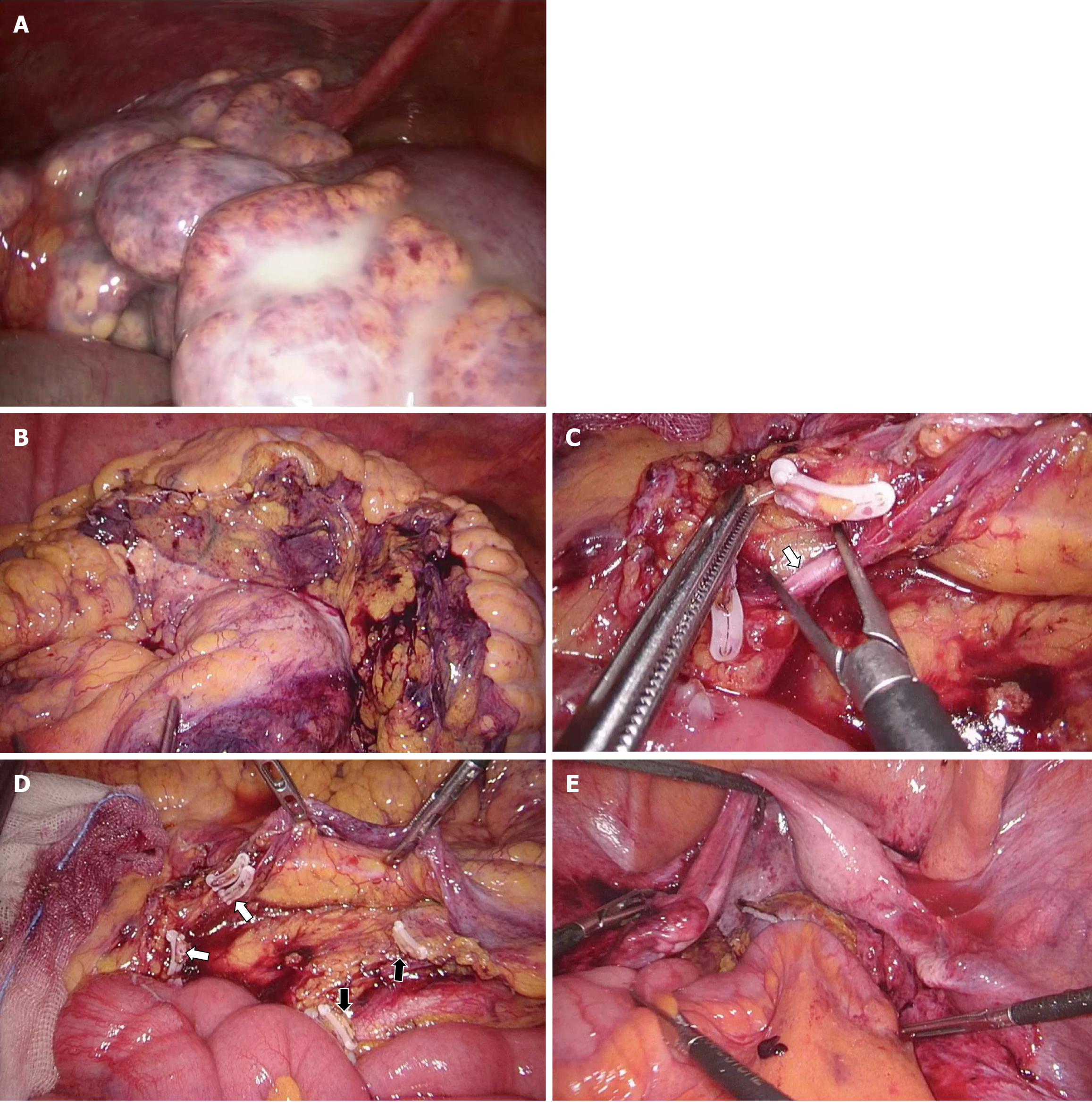
Due to the hemodynamic burden of the AVF, its complex vascular architecture, and the potential for ischemic complications, surgical resection was favored over endovascular treatment. Exploratory laparoscopy was initially attempted but converted to open surgery due to marked inflammation of the left colon (Figure 5A). Hartmann’s procedure was performed, involving resection of contiguous segments of the distal colon. Histopathological examination confirmed ischemic colitis and the presence of an AVF.
Angiographic embolization was initially considered when the AVF measured less than 8 mm. However, the presence of multiple feeding vessels, combined with uncontrolled abdominal pain, fever, and hypotension, necessitated emergency surgery. Laparoscopic exploration was performed to identify ischemic changes in the left colon segment supplied by the inferior mesenteric vessels. The affected left colon appeared pale, thickened, and stiff. The corresponding mesentery was extensively thickened and the appendices epiploicae showed signs of saponification (Figure 5B). The inferior mesenteric vein exhibited thickening and advanced arterialization (Figure 5C). Surgery was completed using a laparoscopic technique with high ligation of the inferior mesenteric artery and vein (Figure 5D). Following resection of the affected left colon, colorectal anastomosis was initially attempted using the transverse colon by ligating the middle colic vessel. However, due to extensive diverticulosis throughout the right colon, a total colectomy with side-to-end ileorectal anastomosis was performed instead (Figure 5E). A temporary ileostomy was established.
Postoperative recovery progressed without complication, allowing discharge on postoperative day eight. One year later, the diverting stoma was successfully reversed. Follow-up colonoscopy and computed tomography (CT) scan revealed no abnormalities.
The patient experienced an uncomplicated postoperative course and was discharged on postoperative day eight. Reversal of the diverting stoma was performed two months postoperatively. Follow-up colonoscopy and CT scan revealed no abnormalities.
IMAVFs are exceedingly uncommon, with roughly 40 reported instances in published medical sources as of 2021[1]. Of these, 25 were classified as congenital or idiopathic, whereas the remaining cases were typically attributed to prior surgical procedures or trauma[1]. The etiology of IMAVFs remains under debate. In the absence of prior abdominal trauma or surgical history in our patients, each lesion was initially suspected to be congenital. Although congenital origins have been suggested, recent evidence indicates that environmental factors, such as hypoxic insults, radiation exposure, epilepsy, and inflammatory processes, may also contribute to AVF formation[9]. The lack of definitive genetic or environmental markers complicates confirmation of the precise etiology. In the second case, recurrent left colonic diverticulitis and left pyelonephritis suggest inflammation as a potential cause of IMAVF. The 2020 CT scan showed no communication between the inferior mesenteric artery and vein (Figure 1). AVFs constitute abnormal connections between arteries and veins, allowing arterial blood to bypass the capillary network and flow directly into the venous system. This disruption of normal hemodynamics can reduce arterial perfusion and elevate venous pressure in the affected region[4,10]. AVFs can cause the steal phenomenon, in which blood is diverted through the fistula, reducing perfusion to the surrounding capillary network. In the gastrointestinal tract, this mechanism can precipitate colonic ischemia. Venous hypertension may further exacerbate ischemia by inducing vascular congestion and mucosal edema, thereby impairing tissue perfusion. In cases where the AVF involves the inferior mesenteric vein, abnormal shunting of arterial blood into the portal circulation can increase portal blood flow[11]. This elevation, along with an adaptive increase in resistance within the hepatic circulation, may contribute to portal hypertension[11]. Studies have reported that portal hypertension develops in up to half of individuals diagnosed with AVFs within the splanchnic circulation[3,4,11]. In a previous study, a considerable proportion of individuals with IMAVFs exhibited clinical or radiologic signs con
Diagnosis of the first patient required several months, whereas surgery was performed on the second patient within 2 weeks of symptom onset. Experience gained from the first case, alongside the history of recurrent intra-abdominal inflammation, facilitated rapid clinical suspicion in the second case. In cases where ischemic colitis presents with clinical signs and symptoms without a clear underlying cause, mesenteric AVFs should be considered as a potential etiology. Prompt recognition and appropriate treatment, guided by strong clinical suspicion, can minimize complications and reduce postoperative morbidity and mortality associated with this condition.
| 1. | Cubisino A, Schembri V, Guiu B. Inferior mesenteric arteriovenous fistula with colonic ischemia: a case report and review of the literature. Clin J Gastroenterol. 2021;14:1131-1135. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 2. | Lee S, Chung J, Ahn B, Lee S, Baek S. Inferior mesenteric arteriovenous fistula. Ann Surg Treat Res. 2017;93:225-228. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 3. | Van Way CW 3rd, Crane JM, Riddell DH, Foster JH. Arteriovenous fistula in the portal circulation. Surgery. 1971;70:876-890. [PubMed] |
| 4. | Athanasiou A, Michalinos A, Alexandrou A, Georgopoulos S, Felekouras E. Inferior mesenteric arteriovenous fistula: case report and world-literature review. World J Gastroenterol. 2014;20:8298-8303. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 27] [Cited by in RCA: 39] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 5. | Carbonell S, Ortiz S, Enriquez P, Lluis F. Arteriovenous fistula in the inferior mesenteric territory. Cir Esp. 2014;92:e23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 6. | Jeon DO, Park JS, Kim JE, Lee SJ, Cho HJ, Im SG, Kim ID, Han EM. [A case of traumatic inferior mesenteric arteriovenous fistula]. Korean J Gastroenterol. 2013;62:296-300. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 7. | Faghihi Langroudi T, Shabestari AA, Pourghorban R, Pourghorban R. Idiopathic inferior mesenteric arteriovenous fistula: a rare cause of pulsatile abdominal mass. Indian J Surg. 2015;77:84-86. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 8. | Noor M, Cooper K, Lujan H, Pena C. Arteriovenous malformation of the inferior mesenteric artery presenting as ischemic colitis. Vasc Med. 2016;21:555-557. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 9. | Tasiou A, Tzerefos C, Alleyne CH Jr, Boccardi E, Karlsson B, Kitchen N, Spetzler RF, Tolias CM, Fountas KN. Arteriovenous Malformations: Congenital or Acquired Lesions? World Neurosurg. 2020;134:e799-e807. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 32] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 10. | Kai K, Sano K, Higuchi K, Uchiyama S, Sueta H, Nanashima A. A rare case of simultaneous rectal and gastric carcinomas accompanied with inferior mesenteric arterioportal fistula: case report. Surg Case Rep. 2019;5:82. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 11. | Capron JP, Gineston JL, Remond A, Lallement PY, Delamarre J, Revert R, Veyssier P. Inferior mesenteric arteriovenous fistula associated with portal hypertension and acute ischemic colitis. Successful occlusion by intraarterial embolization with steel coils. Gastroenterology. 1984;86:351-355. [PubMed] |
| 12. | Okada K, Furusyo N, Sawayama Y, Ishikawa N, Nabeshima S, Tsuchihashi T, Kashiwagi S, Hayashi J. Inferior mesenteric arteriovenous fistula eight years after sigmoidectomy. Intern Med. 2002;41:543-548. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 21] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 13. | Bettenworth D, Rijcken E, Müller KM, Mosch-Messerich A, Heidemann J. Rare cause of upper gastrointestinal bleeding in a 27-year-old male patient. Gut. 2012;61:1367. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 14. | Nemcek AA Jr, Yakes W. SIR 2005 Annual Meeting Film Panel case: inferior mesenteric artery-to-inferior mesenteric vein fistulous connection. J Vasc Interv Radiol. 2005;16:1179-1182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/