Published online Sep 27, 2025. doi: 10.4240/wjgs.v17.i9.106654
Revised: June 19, 2025
Accepted: August 4, 2025
Published online: September 27, 2025
Processing time: 138 Days and 1.4 Hours
This study seeks to systematically assess the effects of warm acupuncture com
To evaluate the impact of warm acupuncture combined with acupoint massage on postoperative gastrointestinal function recovery after gastric cancer surgery, based on a systematic review and meta-analysis.
A comprehensive search was conducted across multiple databases, including PubMed, Cochrane Library, EMBASE, Web of Science, CNKI, Wanfang, and VIP, for relevant studies published up to January 2025. Meta-analyses were carried out using RevMan 5.4, with results presented as standardized mean difference (SMD) or odds ratio with 95% confidence interval (CI). Study heterogeneity was eva
A total of 8 randomized controlled trials involving 694 patients were included. The meta-analysis showed that warm acupuncture combined with acupoint massage significantly improved postoperative gastrointestinal function by reducing the time to first flatus (SMD = -2.14, 95%CI: -3.14 to -1.14, P < 0.0001), time to first bowel movement (SMD = -2.43, 95%CI: -3.52 to -1.34, P < 0.0001), time to bowel sounds recovery (SMD = -3.15, 95%CI:
The combination of warm acupuncture and acupoint massage markedly enhances gastrointestinal recovery following surgery.
Core Tip: This meta-analysis explores the therapeutic impact of combining warm acupuncture with acupoint massage on postoperative gastrointestinal recovery in patients after gastric cancer surgery. The findings suggest that this integrative approach enhances gastrointestinal motility restoration and supports hormonal balance more effectively than standard postoperative care. Although variability exists among the included studies, the results underscore the promise of this traditional Chinese medicine-based intervention as a supplementary treatment option, warranting further validation in well-controlled clinical environments.
- Citation: Ji HC, Nie LJ, Wu JX, Liu X, Zheng X. Effect of warm acupuncture and acupoint massage on postoperative gastrointestinal function in gastric cancer surgery patients: A meta-analysis. World J Gastrointest Surg 2025; 17(9): 106654
- URL: https://www.wjgnet.com/1948-9366/full/v17/i9/106654.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v17.i9.106654
Gastric cancer ranks among the most common causes of cancer-related mortality globally[1,2]. As reported by the World Health Organization, gastric cancer holds the third highest incidence and is the second leading cause of cancer-related deaths worldwide, with notably elevated rates in Asia, especially in China[3]. The treatment of gastric cancer primarily relies on surgical resection, chemotherapy, radiotherapy, and targeted therapy, among which surgical resection remains the primary approach for early-stage gastric cancer[4]. However, gastric cancer surgery often involves extensive resection of the stomach and surrounding tissues, leaving patients with a series of postoperative gastrointestinal dysfunctions[5,6]. These dysfunctions include nausea, vomiting, bloating, loss of appetite, and constipation, which severely impact patients’ quality of life and pose challenges to postoperative recovery[7]. Developing strategies to improve postoperative gas
Currently, the treatment of postoperative gastrointestinal dysfunction primarily depends on medication and physical therapy approaches[8]. Medications such as prokinetic drugs and antiemetics have shown some effectiveness in alleviating postoperative symptoms[9]. However, concerns have been raised about the long-term use of these medications due to their limited effectiveness and the risk of adverse side effects. Furthermore, physical therapies aimed at restoring gastrointestinal function, such as gastrointestinal massage and functional training, are also employed in clinical practice[10,11]. However, the effectiveness of these approaches varies greatly due to individual differences, and no standardized treatment protocols have been established.
In recent years, non-pharmacological approaches like warm acupuncture and acupoint massage, rooted in traditional Chinese medicine (TCM), have gained growing popularity in the postoperative rehabilitation of gastric cancer patients[12,13]. Warm acupuncture, which integrates acupuncture with heat therapy, has been found to activate targeted acupoints, helping to regulate gastrointestinal motility and relieve postoperative symptoms such as nausea and vomiting[14]. Meanwhile, acupoint massage stimulates specific meridians and acupoints through manual techniques, promoting the circulation of Qi and blood, regulating organ functions, and further improving gastrointestinal function[15,16]. Numerous clinical studies have shown that these therapies significantly promote the recovery of gastrointestinal function and reduce postoperative symptoms, with minimal side effects and high safety[17]. However, most existing research is limited to small-scale studies or isolated clinical trials, with a lack of comprehensive, large-sample meta-analyses. This gap hinders the establishment of a solid scientific foundation for these therapeutic approaches.
Accordingly, this study aims to perform a systematic review and meta-analysis to thoroughly assess the impact of combining warm acupuncture with acupoint massage on postoperative gastrointestinal function in patients with gastric cancer. We aim to synthesize the available data from randomized controlled trials (RCTs) and other relevant studies to determine whether this combined therapy can effectively improve gastrointestinal function and alleviate common postoperative symptoms, such as nausea, vomiting, bloating, and constipation. Additionally, this study will compare the efficacy of this combined therapy with conventional pharmacological or physical therapies in improving gastrointestinal function and explore its potential value in clinical treatment. Through this research, we hope to provide more scientific and reliable evidence for clinical practice and offer a novel complementary treatment option for managing postoperative gastrointestinal dysfunction in gastric cancer patients.
An extensive literature search will be carried out across multiple databases, including PubMed, the Cochrane Library, CNKI, Wanfang, and the VIP database. The search keywords will include terms such as “postoperative gastric cancer”, “gastrointestinal function”, “warm acupuncture”, “moxibustion”, and “acupoint massage” to ensure extensive coverage of studies related to postoperative recovery and gastrointestinal function improvement in gastric cancer patients. Boolean operators will be used to enhance the precision and flexibility of the search. The literature search will cover studies published from the establishment of each database up to January 2025, ensuring that the included studies reflect the latest research developments and trends. All studies meeting the inclusion criteria will undergo further screening and quality assessment to ensure the reliability of the data and the scientific rigor of the research.
Inclusion criteria: (1) The study design must be of a high level of evidence, including RCTs, cohort studies, or case-control studies; (2) The study population must consist of postoperative gastric cancer patients, and the research must explicitly focus on interventions related to postoperative recovery, gastrointestinal function restoration, or the prevention of complications; (3) The intervention must involve a combination of warm acupuncture and acupoint massage, with the intervention protocol clearly described in the study, including reproducible parameters such as intensity and frequency of the intervention; and (4) Outcome measures must include, but are not limited to, indicators of gastrointestinal function recovery (e.g., time to first flatus, time to first bowel movement, time for bowel sounds to return, and time to initiate nasogastric or jejunal feeding), as well as changes in gastrointestinal hormones (e.g., gastrin and motilin).
Exclusion criteria: (1) Studies that are not relevant to the research objectives, such as those involving populations other than postoperative gastric cancer patients, or those employing interventions that do not meet the specified requirements (e.g., studies using warm acupuncture or acupoint massage alone without their combined application); (2) Studies with incomplete data or missing key information, such as a lack of relevant data on intervention effects or unclear treatment protocols; (3) Studies of low methodological quality, including those with significant bias, serious methodological flaws, or a lack of standardized interventions such as blinding or randomization; and (4) Studies published in languages other than Chinese or English were excluded due to translation constraints. Future reviews are encouraged to incorporate a wider range of languages with the aid of professional translation services to reduce this potential bias.
In the data extraction process, the following essential details will be collected from each included study: (1) Study design, encompassing the study type, implementation procedures, and methodological specifics; (2) Intervention details, including the specific protocol for combined warm acupuncture and acupoint massage, frequency, duration, and implementation specifics; (3) Sample size; (4) Follow-up duration, i.e., the length of time after the intervention to assess both short-term and long-term treatment effects; and (5) Primary outcome measures, including gastrointestinal function recovery, changes in gastrointestinal hormones (e.g., gastrin and motilin), and the treatment improvement rate. Two independent reviewers were extracted all data, with any disagreements resolved through discussion until a consensus is achieved.
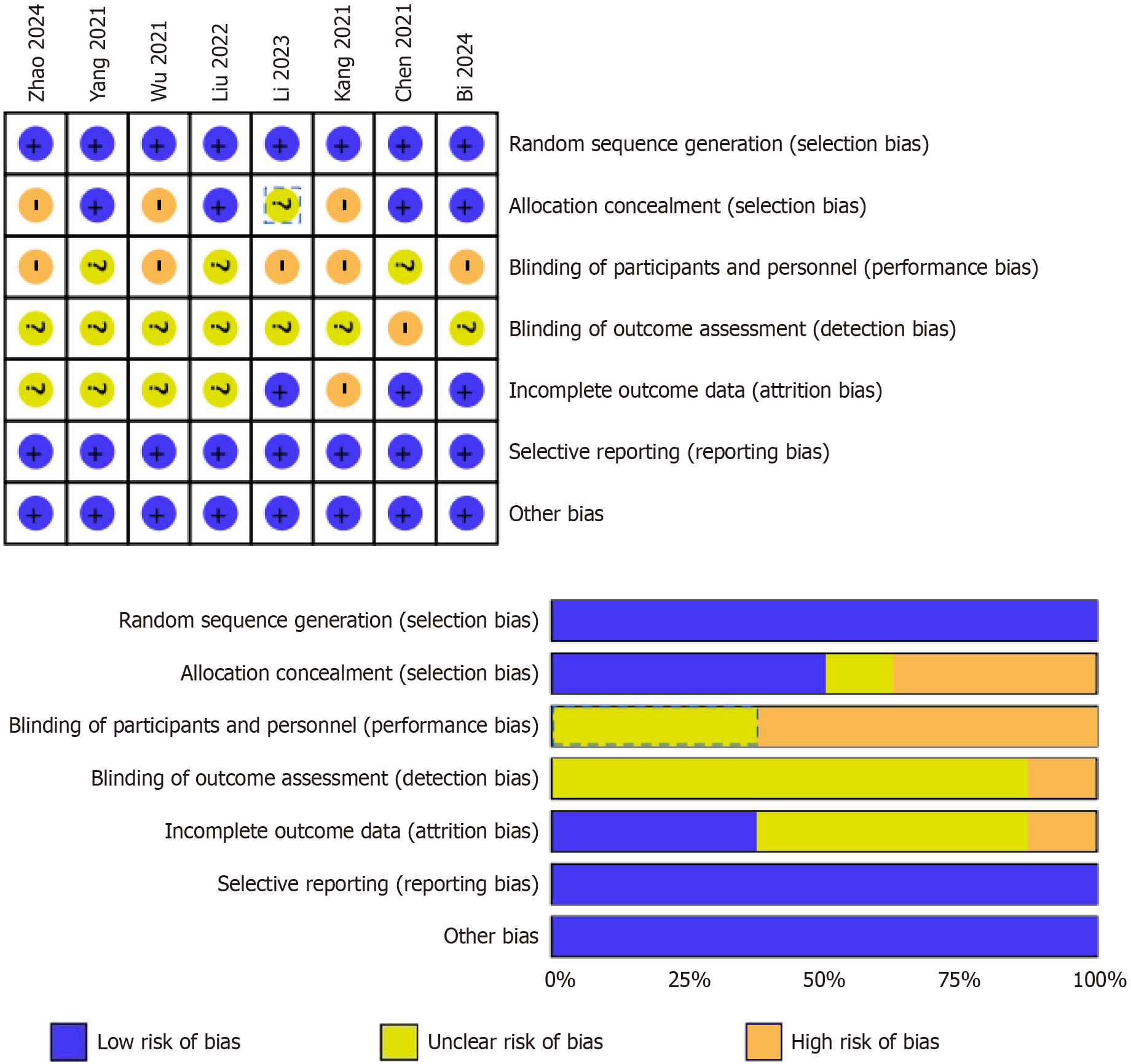
During the quality assessment phase, suitable evaluation tools were used to assess the methodological rigor of the included studies. For RCTs, the Cochrane Risk of Bias Tool[18] were used to assess the risk of bias in aspects such as random sequence generation, blinding, data completeness, and selective reporting. All evaluations were conducted independently by two reviewers. Any disagreements will be addressed through discussion or, if necessary, resolved by involving a third-party expert for arbitration.
In this study, data synthesis was performed using appropriate statistical software for a meta-analysis to quantify the effect differences across the various studies. RevMan 5.4 was used for data analysis. For continuous variables, standardized mean differences (SMDs) were employed to combine the effect sizes of the studies; for dichotomous variables, odds ratios (ORs) were used as the combined effect measure. Pooled effect sizes were calculated with 95% confidence intervals (CIs), and the aggregated results were reported accordingly. To evaluate heterogeneity among studies, the I2 statistic was employed to quantify its extent. An I2 value greater than 50% indicated substantial heterogeneity, suggesting the potential need for subgroup analysis or sensitivity analysis to explore underlying influencing factors and the robustness of the results. When the I2 value indicated low heterogeneity, a fixed-effect model was applied for the meta-analysis. Conversely, in cases of substantial heterogeneity, a random-effects model was adopted to synthesize the study results. A funnel plot was generated to evaluate the presence of potential publication bias. All statistical analyses were performed using two-sided tests, with a significant threshold of P < 0.05.
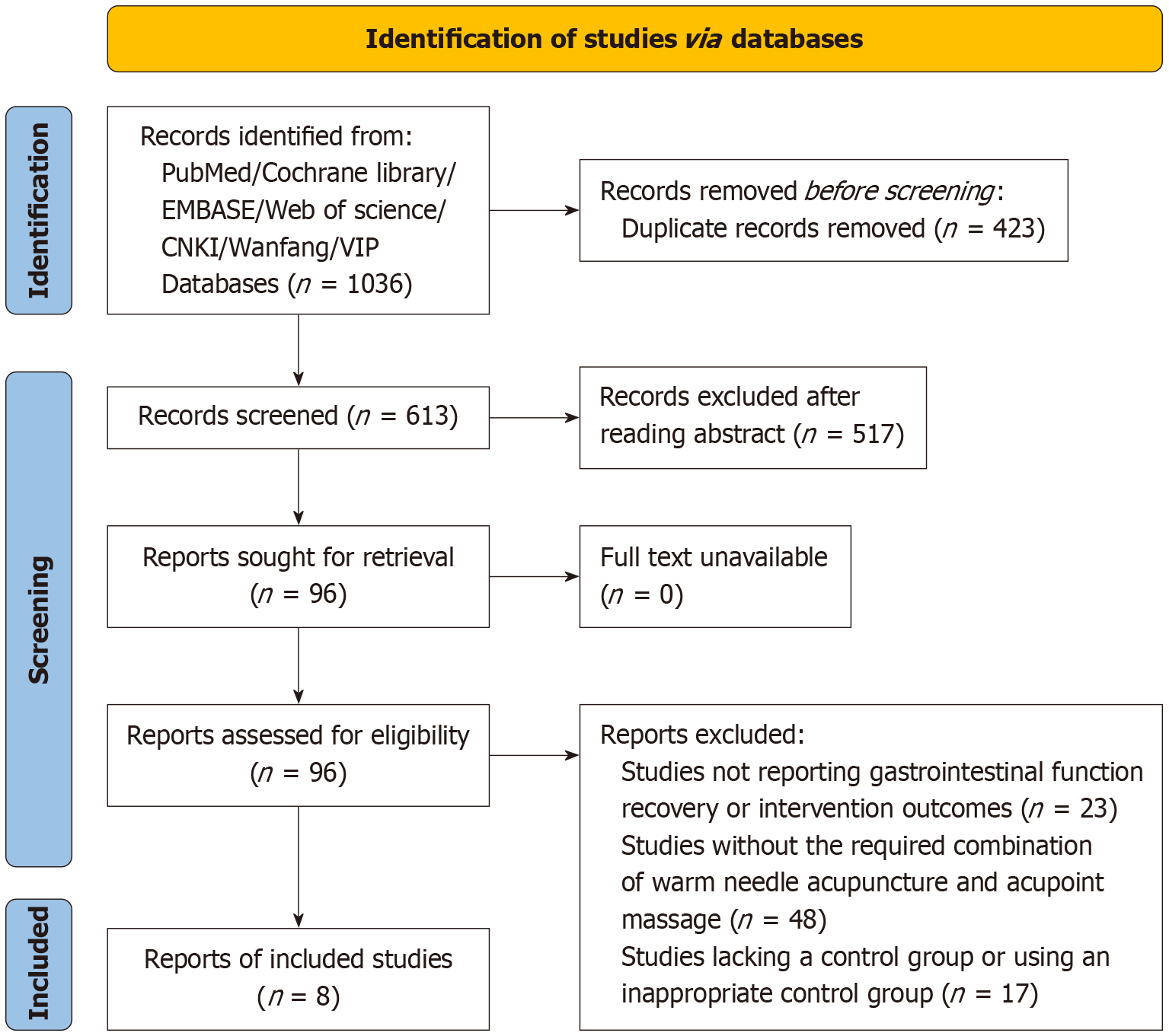
A total of 1036 records were retrieved from databases such as PubMed, Cochrane Library, EMBASE, Web of Science, CNKI, Wanfang, and VIP. After eliminating 423 duplicates, 613 records were screened by title and abstract, resulting in the exclusion of 517 studies that did not meet the inclusion criteria. Full texts of 96 studies were retrieved and assessed for eligibility, of which 87 were excluded for the following reasons: 23 studies did not report outcomes related to gas
| Ref. | Research type | Sample size | Age (mean ± SD, year) | Male/female | Surgical methods | Research period | ||||
| Observation | Control | Observation | Control | Observation | Control | Observation | Control | |||
| Chen[19], 2021 | RCT | 35 | 35 | 63.57 ± 2.18 | 63.51 ± 2.12 | 18/17 | 19/16 | 11 cases of proximal gastrectomy, 9 cases of total gastrectomy, and 15 cases of distal gastrectomy | 12 cases of proximal gastrectomy, 8 cases of total gastrectomy, and 15 cases of distal gastrectomy | January 2020 to January 2021 |
| Bi et al[20], 2024 | RCT | 33 | 33 | 56.04 ± 7.11 | 55.73 ± 7.09 | 12/21 | 18/15 | 12 cases of distal gastrectomy + gastrojejunostomy, and 21 cases of proximal gastrectomy + esophagogastrostomy | 14 cases of distal gastrectomy + gastrojejunostomy, and 19 cases of proximal gastrectomy + esophagogastrostomy | October 2020 to June 2021 |
| Zhao and Sun[21], 2024 | RCT | 58 | 57 | 60.37 ± 5.7 | 60.09 ± 5.81 | 37/21 | 35/22 | 23 cases of proximal gastrectomy, and 34 cases of distal gastrectomy | 26 cases of proximal gastrectomy, and 32 cases of distal gastrectomy | June 2020 to August 2022 |
| Wu et al[22], 2021 | RCT | 49 | 49 | 56.43 ± 10.01 | 60.09 ± 5.81 | 28/21 | 27/22 | 35 cases of open surgery, and 14 cases of laparoscopic surgery | 38 cases of open surgery, and 11 cases of laparoscopic surgery | April 2018 to November 2019 |
| Li and Zhu[23], 2023 | RCT | 29 | 30 | 61.9 ± 11.8 | 62.6 ± 12.8 | 12/17 | 12/18 | 29 cases of radical gastrectomy | 30 cases of radical gastrectomy | September 2020 to September 2022 |
| Yuan et al[24], 2021 | RCT | 41 | 41 | 55.65 ± 7.49 | 55.69 ± 7.42 | 25/16 | 27/14 | 41 cases of radical gastrectomy | 41 cases of radical gastrectomy | June 2017 to June 2019 |
| Kang et al[25], 2021 | RCT | 54 | 54 | 18-75 | 18-75 | / | / | / | / | June 2019 to January 2021 |
| Liu and Xu[26], 2022 | RCT | 48 | 48 | 63.86 ± 7.73 | 63.18 ± 7.68 | 28/20 | 31/17 | 29 cases of distal gastrectomy + gastrojejunostomy, and 19 cases of proximal gastrectomy + esophagogastrostomy | 31 cases of distal gastrectomy + gastrojejunostomy, and 17 cases of proximal gastrectomy + esophagogastrostomy | January 2019 to July 2021 |
The quality assessment revealed that all included studies exhibited a low risk of bias in random sequence generation, suggesting the use of appropriate randomization techniques. However, several studies demonstrated unclear or high risk of bias in allocation concealment, suggesting potential limitations in the process of concealing group allocation[19-26]. Performance bias, related to the blinding of participants and personnel, was high, as most studies did not fully implement blinding, which might affect the reliability of the results. Detection bias, concerning the blinding of outcome assessment, was also unclear or high in some studies. Most studies performed well in addressing incomplete outcome data, with only a few showing unclear or high risk of attrition bias[21,22,24-26]. Furthermore, none of the studies showed evidence of selective reporting, indicating a low risk of bias in this area. Most studies also demonstrated a low risk across other potential sources of bias (Figure 2).
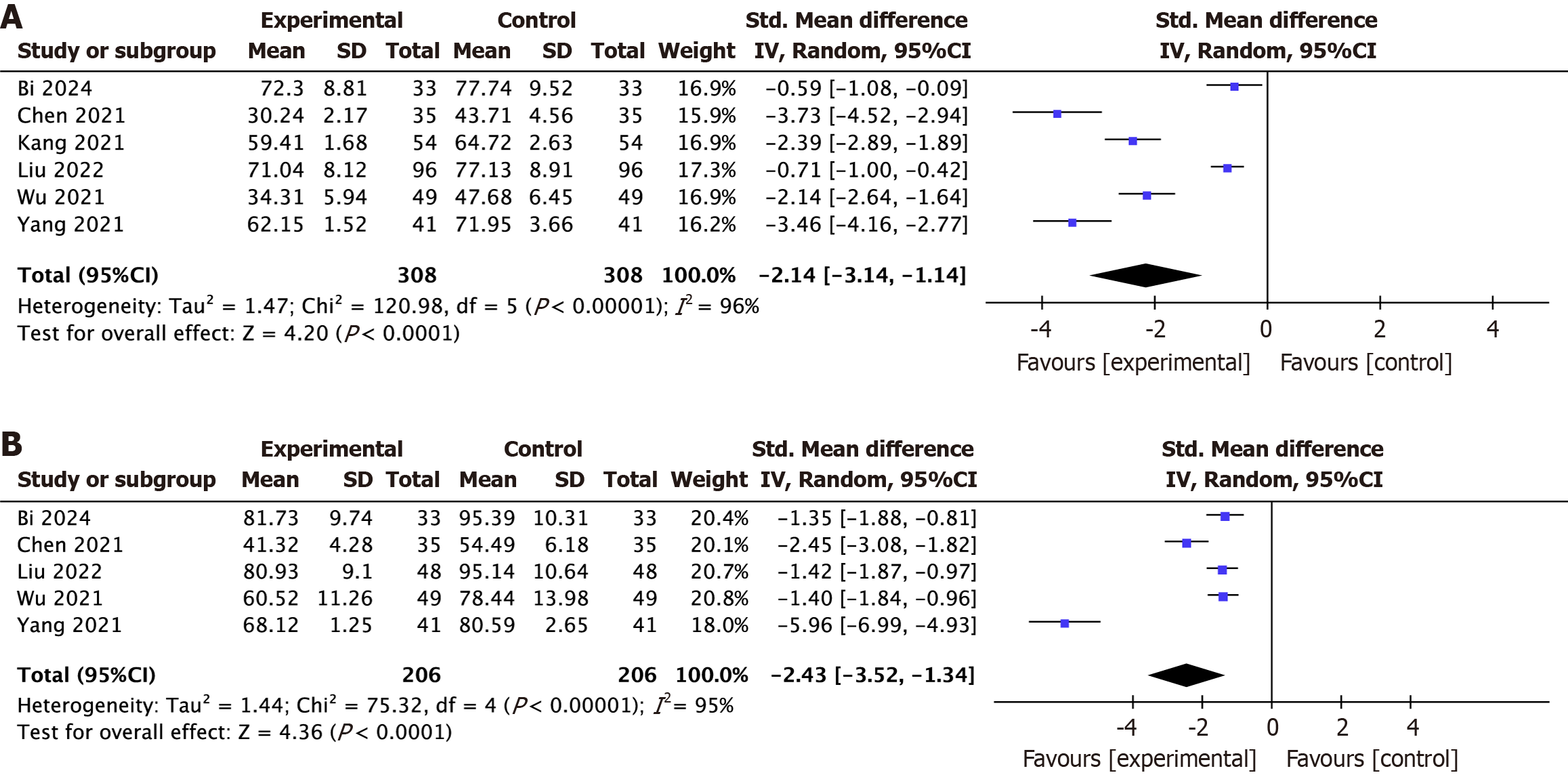
Time to first flatus: A meta-analysis was conducted to evaluate the effect of combined warm acupuncture and massage on the improvement of gastrointestinal function, specifically focusing on the time to first flatus. Six RCTs[19,20,22,24-26] involving 616 participants were included in the analysis. The pooled results demonstrated a significant reduction in the time to first flatus (SMD = -2.14, 95%CI: -3.14 to -1.14, P < 0.0001), indicating that the intervention effectively accelerated postoperative gastrointestinal recovery. However, substantial heterogeneity was observed across the studies (I2 = 96%, P < 0.00001), suggesting that the results should be interpreted with caution (Figure 3A).
Time to first bowel movement: A meta-analysis was conducted to evaluate the effect of combined warm acupuncture and acupoint massage on the time to first bowel movement. Five RCTs[19,20,22-24], comprising a total of 412 participants, were included. The analysis revealed substantial heterogeneity among the studies (I2 = 95%, P < 0.00001). The pooled results indicated that the intervention significantly reduced the time to first bowel movement (SMD = -2.43, 95%CI: -3.52 to -1.34, P < 0.0001). These findings indicate that the integration of warm acupuncture and acupoint massage is effective in enhancing postoperative gastrointestinal recovery (Figure 3B).
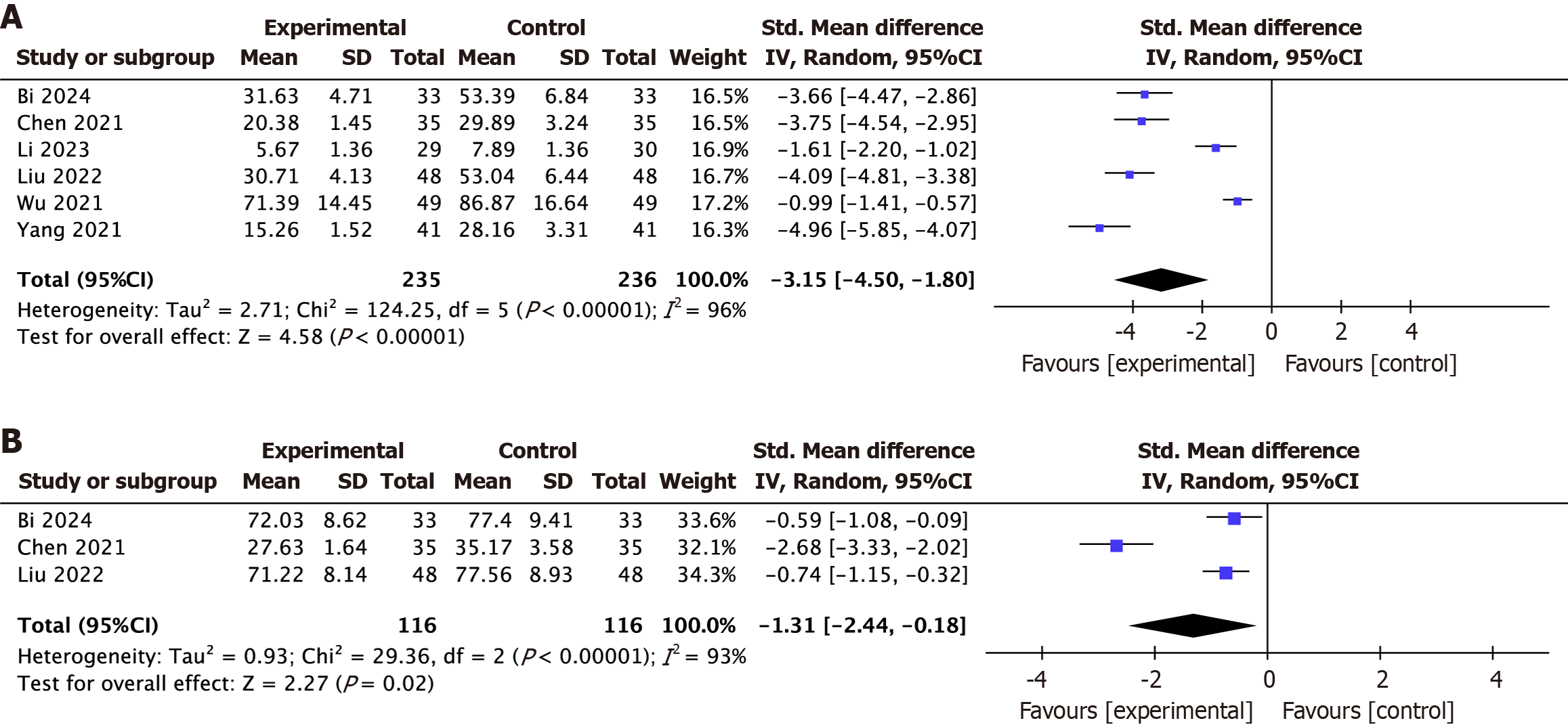
Time to bowel sounds recovery: A meta-analysis was performed to assess the impact of warm acupuncture combined with massage on the time to bowel sound recovery. Six RCTs[19,20,22-24,26], comprising 471 participants, were included. The pooled analysis demonstrated a significant reduction in recovery time (SMD = -3.15, 95%CI: -4.50 to -1.80, P < 0.00001), suggesting that the intervention markedly promotes gastrointestinal recovery. However, considerable heterogeneity was detected across the studies (I2 = 96%, P < 0.00001). This high level of heterogeneity may stem from differences in patient demographics, surgical methods, and intervention protocols may have contributed to variability (Figure 4A).
Time to initiate nasogastric or jejunal feeding: A meta-analysis was carried out to examine the effect of warm acupuncture combined with massage on the time to initiation of nasogastric or jejunal feeding. Three RCTs[19,20,26], including a total of 232 participants, were analyzed. The combined results showed a significant reduction in the time to begin enteral feeding (SMD = -1.31, 95%CI: -2.44 to -0.18, P = 0.02), suggesting that this integrative therapy may effectively facilitate earlier gastrointestinal recovery. However, high heterogeneity was observed among the studies (I2 = 93%, P < 0.00001), suggesting that differences in study design, patient characteristics, or intervention protocols may have contributed to variability (Figure 4B).
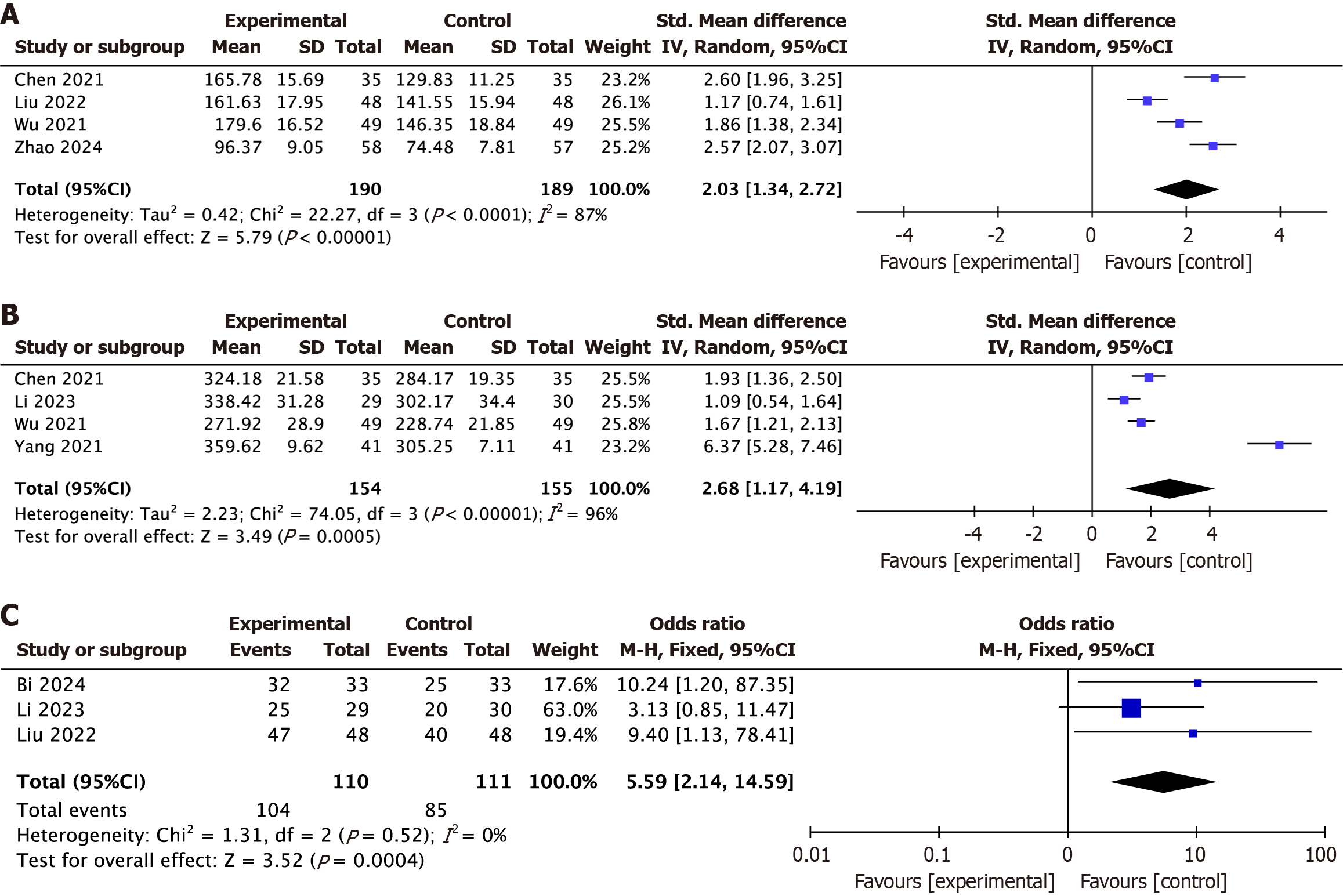
Gastrin levels: A meta-analysis was conducted to assess the effect of warm acupuncture combined with massage on postoperative levels of gastrin, an important gastrointestinal hormone. Four RCTs[19,21,22,26] involving 379 participants were included in the analysis. Moderate to high heterogeneity was detected among the included studies (I2 = 87%, P < 0.0001). The meta-analysis revealed a significant increase in gastrin levels following the intervention (SMD = 2.03, 95%CI: 1.34-2.72, P < 0.00001), indicating that the combination of warm acupuncture and massage may stimulate gastrin secretion and support gastrointestinal recovery (Figure 5A).
Motilin levels: A meta-analysis was performed to assess the impact of warm acupuncture combined with massage on postoperative motilin levels, a crucial hormone that regulates gastrointestinal motility. Four RCTs[19,20,22,25] involving 309 participants were included in the analysis. Considerable heterogeneity was found across the included studies (I2 = 96%, P < 0.00001). The pooled analysis revealed a significant elevation in motilin levels following the intervention (SMD = 2.68, 95%CI: 1.17-4.19, P = 0.0005), suggesting that the combination of warm acupuncture and massage effectively stimulates motilin secretion, thereby promoting gastrointestinal recovery (Figure 5B).
Evaluation of intervention effectiveness: A meta-analysis was conducted to evaluate the clinical effectiveness of warm acupuncture combined with massage in postoperative recovery. Three RCTs[19,20,26], encompassing 221 participants, were included. No heterogeneity was detected among the studies (I2 = 0%, P = 0.52). The pooled results demonstrated a significantly higher effectiveness rate in the intervention group (OR = 5.59, 95%CI: 2.14-14.59, P = 0.0004), indicating that this combined therapy is more effective in enhancing postoperative recovery outcomes (Figure 5C).
Sensitivity analysis was performed to assess the stability and reliability of the meta-analysis findings. By sequentially excluding individual studies and reanalyzing the pooled effect estimates, it was observed that the overall results remained consistent, indicating that no single study disproportionately influenced the findings. This suggests that the results of the meta-analysis are stable and robust.
This study systematically evaluated the effects of warm acupuncture combined with acupoint massage on gastrointestinal function recovery in gastric cancer patients after surgery. The results showed that this combined therapy significantly improved key postoperative recovery indicators, including shorter times to first flatus, first bowel movement, bowel sound recovery, and earlier initiation of nasogastric or jejunal feeding. These improvements suggest that therapy can effectively accelerate the recovery of gastrointestinal motility and reduce the duration of postoperative discomfort. Additionally, the intervention enhanced gastrointestinal hormone levels, particularly gastrin and motilin, which play essential roles in stimulating digestive functions and promoting gastrointestinal motility. The combined therapy also demonstrated superior intervention effectiveness compared to conventional pharmacological or physical treatments, further reinforcing its clinical value[19,22]. These findings highlight the potential of integrating TCM therapies into standard postoperative care for gastric cancer patients, offering a promising complementary approach to current therapeutic options.
Compared to pharmacological treatments, warm acupuncture and acupoint massage have distinct advantages, such as minimal side effects, non-invasiveness, and the ability to address multiple postoperative symptoms simultaneously, including nausea, bloating, abdominal pain, and constipation[12]. Pharmacological treatments, while effective to some extent, are often associated with undesirable side effects such as drowsiness, dry mouth, or dependency over long-term use[25,26]. Warm acupuncture works by combining the therapeutic effects of acupuncture and thermal stimulation, which synergistically improve blood circulation, regulate gastrointestinal motility, and alleviate pain and bloating[12,25]. Similarly, acupoint massage stimulates meridians and specific acupoints, facilitating Qi and blood flow, harmonizing organ function, and reducing stress and discomfort[3,25]. Together, these therapies offer a holistic, patient-centered approach that aligns with postoperative recovery needs.
However, the study also highlighted several limitations. High heterogeneity across analyses may be attributed to variations in patient characteristics (e.g., age, comorbidities), surgical methods (e.g., laparoscopic vs open surgery), and intervention protocols (e.g., frequency, duration, intensity). Methodological issues, including inadequate blinding, lack of allocation concealment, and small sample sizes, further reduce the strength of the evidence. Most studies focused on short-term outcomes like gastrointestinal motility and hormone levels, while long-term effects on survival, recurrence, and quality of life remain unclear[19,20,25]. Additionally, the exclusion of non-English and non-Chinese publications may have introduced language bias, limiting the comprehensiveness and generalizability of the results. Future reviews should expand their search to multilingual databases such as J-STAGE and SciELO to improve inclusivity. Overall, while the findings suggest that warm acupuncture combined with acupoint massage may support postoperative gastrointestinal recovery, these results should be interpreted with caution. High-quality, large-scale, and well-designed RCTs are needed to confirm efficacy and standardize treatment protocols.
In conclusion, warm acupuncture combined with acupoint massage appears to be a safe and effective complementary therapy for enhancing postoperative gastrointestinal recovery in gastric cancer patients. Based on current evidence, it is recommended to initiate treatment within 24-48 hours after surgery, with sessions conducted once or twice daily, targeting acupoints such as ST36 (Zusanli) and CV12 (Zhongwan) for 20-30 minutes per session. This approach may accelerate recovery, alleviate discomfort, and promote gastrointestinal hormone regulation, addressing key unmet needs in postoperative care. These findings support the integration of TCM into multidisciplinary clinical practice. However, further large-scale, high-quality trials are needed to validate these results, optimize treatment protocols, and clarify the long-term benefits of this therapy.
| 1. | Guo Y, Cao XS, Zhou MG, Yu B. Gastric microbiota in gastric cancer: Different roles of Helicobacter pylori and other microbes. Front Cell Infect Microbiol. 2022;12:1105811. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 29] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 2. | Feng W, Ding Y, Zong W, Ju S. Non-coding RNAs in regulating gastric cancer metastasis. Clin Chim Acta. 2019;496:125-133. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 26] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 3. | Park JS, Kim J, Elghiaty A, Ham WS. Recent global trends in testicular cancer incidence and mortality. Medicine (Baltimore). 2018;97:e12390. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 94] [Cited by in RCA: 191] [Article Influence: 23.9] [Reference Citation Analysis (0)] |
| 4. | Ji JF, Ji X, Bu ZD. [From standard to precision treatment: the development of surgery for gastric cancer]. Zhonghua Wai Ke Za Zhi. 2016;54:164-168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 5. | Yazici P, Kaya C, Isil G, Bozkurt E, Mihmanli M. Splenic infarction - A rare cause of acute abdominal pain following gastric surgery: A case series. Int J Surg Case Rep. 2015;10:88-90. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 6. | Fujishima H, Etoh T, Hiratsuka T, Akagi T, Tajima M, Shibata T, Ueda Y, Tojigamori M, Shiroshita H, Shiraishi N, Kitano S, Inomata M. Serosal and muscular layers incision technique in laparoscopic surgery for gastric gastrointestinal stromal tumors. Asian J Endosc Surg. 2017;10:92-95. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 7. | O'Gorman C, Barry A, Denieffe S, Sasiadek W, Gooney M. Nursing implications: symptom presentation and quality of life in rectal cancer patients. J Clin Nurs. 2016;25:1395-1404. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 8. | Araújo FM, DeSantana JM. Physical therapy modalities for treating fibromyalgia. F1000Res. 2019;8:F1000 Faculty Rev-F1000 Faculty2030. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 22] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 9. | Youssef AS, Parkman HP, Nagar S. Drug-drug interactions in pharmacologic management of gastroparesis. Neurogastroenterol Motil. 2015;27:1528-1541. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 10. | Fink J, Burns J, Perez Moreno AC, Kram JJF, Armstrong M, Chopp S, Maul SJ, Conway N. A Quality Brief of an Oncological Multisite Massage and Acupuncture Therapy Program to Improve Cancer-Related Outcomes. J Altern Complement Med. 2020;26:820-824. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 11. | Ho SSM, Kwong ANL, Wan KWS, Ho RML, Chow KM. Experiences of aromatherapy massage among adult female cancer patients: A qualitative study. J Clin Nurs. 2017;26:4519-4526. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 18] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 12. | Liu W, Fan Y, Wu Y, Hou X, Xue B, Li P, Zhang S, Yue Q. Efficacy of Acupuncture-Related Therapy in the Treatment of Knee Osteoarthritis: A Network Meta-Analysis of Randomized Controlled Trials. J Pain Res. 2021;14:2209-2228. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 29] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 13. | Guo H, Pan X, Zheng Y, Yang X, Xu H, Zhang Y, Sun Y, Wang Z, Ba T, Pang B, Hao T, Zhang J, Zhao X. Current state of research on acupuncture for the treatment of post-stroke dysphagia: a scoping review. Front Neurosci. 2024;18:1391576. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 14. | Unsal N, Akcaboy ZN, Soyal OB, Akcaboy EY, Mutlu NM, Gogus N. Effectiveness of Intraoperative Laser Acupuncture Combined with Antiemetic Drugs for Prevention of Postoperative Nausea and Vomiting. J Altern Complement Med. 2020;26:67-71. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 15. | Zhou Z, Wang Y, Zhang C, Meng A, Hu B, Yu H. Design and Massaging Force Analysis of Wearable Flexible Single Point Massager Imitating Traditional Chinese Medicine. Micromachines (Basel). 2022;13:370. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 16. | Meng X, Gu W, Ma F, Du Y, Zhao Q. [Acupuncture therapy for regaining consciousness in terms of acupoint location, needle insertion and needle manipulation]. Zhongguo Zhen Jiu. 2015;35:249-251. [PubMed] |
| 17. | Lu S, Wang B, Wang J, Guo Y, Li S, Zhao S, Yang Y, Feng Y, Xu Z. Moxibustion for the Treatment of Cancer and its Complications: Efficacies and Mechanisms. Integr Cancer Ther. 2023;22:15347354231198089. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 19] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 18. | Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA; Cochrane Bias Methods Group; Cochrane Statistical Methods Group. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18487] [Cited by in RCA: 26318] [Article Influence: 1754.5] [Reference Citation Analysis (4)] |
| 19. | Chen C. [Effect of moxibustion combined with acupoint massage on gastrointestinal motility and gastrointestinal hormone levels in patients after radical resection of gastric cancer]. Xiandai Yangsheng. 2021;21:31-34. [DOI] [Full Text] |
| 20. | Bi YC, Wang Y, Wang ZJ. [Effect of Preoperative Moxibustion Combined with Postoperative Acupoint Massage on Gastrointestinal Function in Patients after Gastric Cancer Surgery]. Xibu Zhongyiyao. 2024;37:154-156. [DOI] [Full Text] |
| 21. | Zhao J, Sun YY. [The effect of bilateral Zusanli acupoint moxibustion combined with acupoint massage on patients with gastrointestinal dysfunction after gastric cancer surgery and its impact on nutritional status and serum gastrointestinal hormones]. Hangkong Hangtian Yixue Zazhi. 2024;35:1109-1111. |
| 22. | Wu J, Zhang H, Mao F. [Effects of warm acupuncture combined with acupoint massage on serum gastrin, motilin level and gastrointestinal function in patients with gastric cancer after operation]. Zhongguo Linchuang Yanjiu. 2021;34:232-235. [DOI] [Full Text] |
| 23. | Li QJ, Zhu YN. [Clinical Observation of Warm Acupuncture Combined with Ear Acupoint Bean-Pressing in the Treatment of Gastroparesis Syndrome After Operation of Gastric Cancer]. Linchuang Yanjiu. 2023;31:101-104. [DOI] [Full Text] |
| 24. | Yuan WY, Yang WN, Zhu FH. [Acupuncture and moxibustion combined with herbal plaster at Shenque point can promote the recovery of gastrointestinal function in patients with gastric cancer after operation]. Shanxi Zhongyiyao Daxue Xuebao. 2021;44:93-96. |
| 25. | Kang WZ, Li Y, Ma FH, Tian Z, Zuo WH, Li QW, Hu KW, Tian YT. [Evaluation of acupoint acupuncture and moxibustion for promotion of recovery of gastrointestinal function after laparoscopic radical gastrectomy for gastric cancer]. Zhongguo Zhongliu Linchuang Yu Kangfu. 2021;28:1158-1161. [DOI] [Full Text] |
| 26. | Liu Y, Xu SH. [Effect of Preoperative Moxibustion Combined with Postoperative Acupuncture on Gastrointestinal Function of Gastric Cancer after Surgery]. Zhongguo Zhongxiyi Jiehe Waike Zazhi. 2022;28:634-638. [DOI] [Full Text] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/