Published online Mar 27, 2025. doi: 10.4240/wjgs.v17.i3.103516
Revised: December 17, 2024
Accepted: January 11, 2025
Published online: March 27, 2025
Processing time: 95 Days and 1.1 Hours
Acute appendicitis (AP) is a frequently encountered surgical emergency, and appendectomy is conventionally regarded as the predominant treatment moda
To elucidate the therapeutic effectiveness and influencing factors of laparoscopic appendectomy (LA) with mesoappendix dissection in the treatment of AP.
First, 150 patients with AP who visited Shangrao Municipal Hospital between January 2022 and June 2024 were enrolled in this study. Among them, 72 patients were assigned to the control group to receive conventional LA, whereas 78 cases were included in the observation group for LA with mesoappendix dissection. Subsequently, indicators such as therapeutic effectiveness, surgical indices (ope
Compared with the control group, the observation group had higher clinical the
Overall, LA with mesoappendix dissection has a remarkable curative effect in treating patients with AP, which is worthy of clinical promotion.
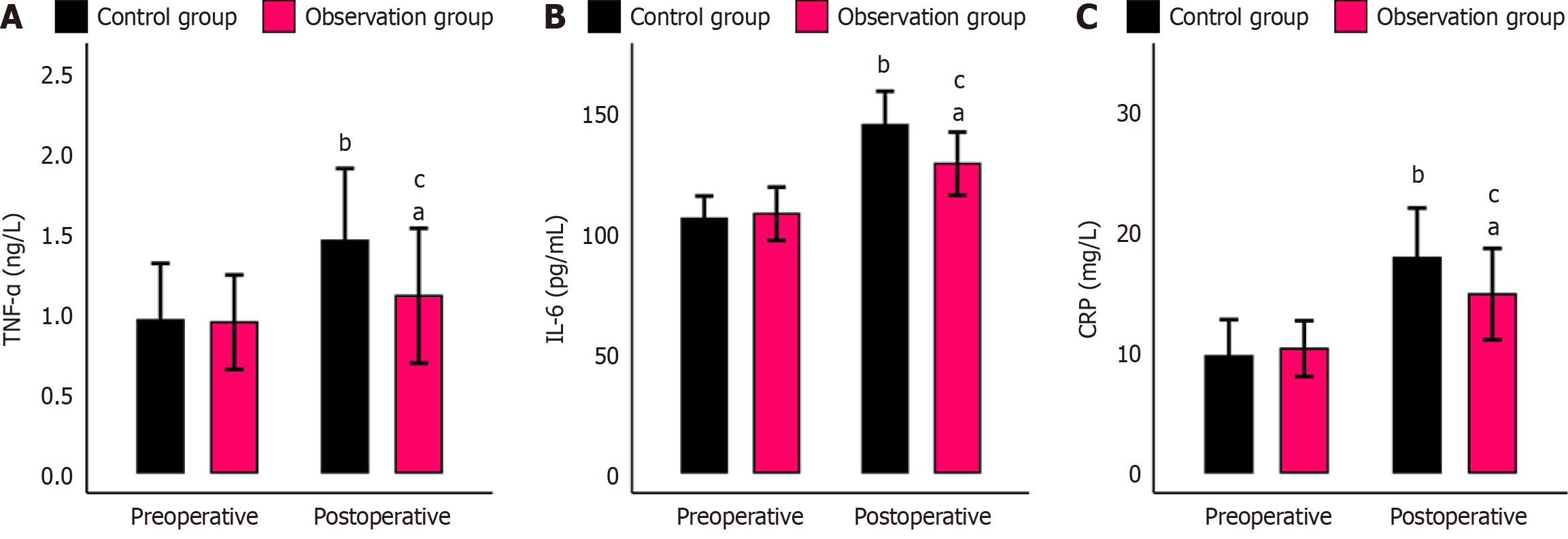
Core Tip: At present, relevant research focusing on the efficacy and influencing factors of laparoscopic appendectomy with mesoappendix dissection in treating patients with acute appendicitis is limited. In this study, 150 patients who are suffering from acute appendicitis were enrolled. Comparative analyses regarding the clinical application of conventional laparoscopic appendectomy and laparoscopic appendectomy with mesoappendix dissection were performed among these patients, taking into account therapeutic effectiveness, surgical parameters, postoperative rehabilitation, the occurrence rate of adverse events, and serum inflammatory factors. Finally, we concluded that laparoscopic appendectomy with mesoappendix dissection, when applied to treat patients with acute appendicitis, can enhance the treatment efficacy and surgical outcomes, facilitating patients’ postoperative recovery, decreasing the incidence of adverse events, and averting the excessive increase of inflammatory markers, including tumor necrosis factor-α, interleukin-6, and C-reactive protein triggered by surgical stimuli. Hence, this approach shows great potential in clinical application.
- Citation: Yuan J, Liu Q, Wu BY. Therapeutic effectiveness and influencing factors of laparoscopic appendectomy with mesoappendix dissection in the treatment of acute appendicitis. World J Gastrointest Surg 2025; 17(3): 103516
- URL: https://www.wjgnet.com/1948-9366/full/v17/i3/103516.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v17.i3.103516
Acute appendicitis (AP) is a common surgical emergency with a lifetime morbidity risk in the range of 6%-7%, with 300000 appendectomies performed annually in the United States alone[1,2]. Statistically, AP has a higher incidence in males, with a morbidity risk of 8.6%, than in females (6.7%)[3]. This disease is primarily induced by fecaliths, fecal impaction, lymphoid hyperplasia, or tumors, which can trigger edema, vascular congestion, ischemia, appendiceal perforation, and intra-abdominal abscess or generalized peritonitis[4]. The main clinical manifestations of AP include nausea, vomiting, anorexia, abdominal pain, and fever, which have diverse degrees of negative impacts on the physical health of patients[5]. Appendectomy is the first treatment option for AP. Given the development and widespread application of laparoscopic technology, laparoscopic appendectomy (LA) has advantages such as small wounds, aesthetically pleasing incisions, and rapid postoperative recovery in clinical practice[6,7]. LA involves extracting the patient’s appendix through the trocar puncture hole. However, for patients with severe swelling, LA is challenging[8,9]. Moreover, if the patient has relatively severe mesenteric edema and adhesion, then LA is often accompanied with mesenteric torsion, thereby increasing the difficulty of the operation and the risk of mesenteric bleeding at the root of the appendix[10-12]. Thus, this study aims to improve the surgical outcome of patients with AP by LA combined with mesoappendix dissection. LA with mesoappendix dissection is an improved surgical modality of conventional LA, which reduces the size of the specimen by removing the appendix root and mesoappendix, making the specimen easy to remove and reducing the risk of active bleeding[13,14]. Given the current dearth of research on the therapeutic effectiveness and influencing factors of LA with mesoappendix dissection for the treatment of AP, this study aims to conduct relevant analysis to improve surgical outcomes in such patients.
Patients were included in the study if they met the following criteria: Patients were diagnosed of AP by computerized tomography, surgical physical examination, abdominal B-ultrasound, and blood routine examination in combination with physical examination and medical history[15]; patients with acute onset; patients presented with typical clinical symptoms such as vomiting and right lower abdominal pain; patients completed the surgical indications for appendec
Both groups of patients maintained a supine position during the surgery. A three-port approach was used. First, a 10 mm trocar was placed 1 cm above the upper edge of the umbilicus, which served as the intraoperative observation port and connected to the pneumoperitoneum tube. Carbon dioxide pneumoperitoneum was routinely established with a pressure range of 11-12 mmHg. Then, a 10 mm trocar was inserted 2 cm below and parallel to the umbilicus on the midline of the patient’s left clavicle, which served as the main intraoperative operating port. A 5 mm trocar was placed at the left counter-McBurney’s point, which served as the intraoperative traction port.
The control group was treated with conventional LA. A puncture was created between the serosal surface of the appendix and the mesoappendix at the root of the patient’s appendix by using a surgical ultrasonic scalpel, and the distal end of the appendix and mesoappendix was clamped. Subsequently, the appendix and mesoappendix were sequentially severed and removed via the main operation port. Thereafter, the puncture site was disinfected with iodophor solution and routinely sutured. Both groups were treated under intraoperative conditions to determine whether an indwelling drain was placed.
For the observation group, LA combined with mesoappendix dissection was performed. A surgical ultrasonic scalpel was used to cut the mesoappendix to the serosal surface of the appendix from the end to the apex of the patient’s appendix. Then, the mesoappendix was peeled off along the serosal surface of the appendix toward the end of the appendix until the root of the appendix. Next, the appendix and distal end of the mesoappendix root were clamped. The appendix and mesoappendix were sequentially severed using the surgical ultrasonic scalpel and then removed from the main operation port (trocar). Finally, the interior of the puncture site was disinfected with iodophor solution and rou
Therapeutic effectiveness: The clinical effectiveness of the two groups was comparatively analyzed in accordance with the following criteria for efficacy determination: The complete disappearance of symptoms and signs is considered markedly effective; the partial alleviation of symptoms and signs is regarded as effective; the absence of change or aggravation of symptoms and signs is deemed ineffective. The total effective rate of treatment was measured as the sum of the number of markedly effective cases and effective cases as a percentage of the total number of cases.
Surgical indices: Operation time, intraoperative blood loss, and hospital stays were observed and recorded.
Postoperative recovery indices: The time to ambulation, gastrointestinal function recovery, and food intake of both groups of patients were observed and recorded.
Incidence rate of adverse events: The incidence of adverse reactions such as postoperative bleeding, pelvic infection, puncture site infection, and ileus was observed and recorded.
Serum inflammatory factors: Five milliliters of fasting venous blood was collected from patients before and after treatment, and the serum was centrifuged to determine the level of tumor necrosis factor (TNF)-α, interleukin (IL)-6, and C-reactive protein (CRP) levels by enzyme-linked immunosorbent assays.
Statistical analysis was conducted using SPSS 19.0, with P < 0.05 indicating statistical significance. Measurement data were statistically described as (mean ± SD), with inter-group and intra-group comparisons before and after treatment performed by using an independent sample t-test and paired t-test, respectively. Count data were represented as n (%), and a χ2 test was performed for inter-group comparisons.
No notable differences in sex, age, body mass index (BMI), time from acute attack to admission, and family medical history were found between the control and observation groups (P > 0.05; Table 1).
| General information | Control group (n = 72) | Observation group (n = 78) | χ2/t | P value |
| Sex (male/female) | 42/30 | 44/34 | 0.057 | 0.812 |
| Age (years) | 48.36 ± 6.18 | 49.03 ± 7.56 | ||
| Body mass index (kg/m2) | 23.58 ± 2.37 | 24.32 ± 2.55 | ||
| Time from acute onset to admission (hour) | 24.01 ± 3.16 | 23.64 ± 3.24 | ||
| Family medical history (without/with) | 64/8 | 67/11 | 0.303 | 0.582 |
The total number of effective cases in the control and observation groups was 60 and 74, respectively, with a markedly higher total effective rate in the observation group than in the control group (P < 0.05; Table 2).
| Therapeutic effectiveness | Control group (n = 72) | Observation group (n = 78) | χ2 | P value |
| Markedly effective | 25 (34.72) | 35 (44.87) | ||
| Effective | 35 (48.61) | 39 (50.00) | ||
| Ineffective | 12 (16.67) | 4 (5.13) | ||
| Total | 60 (83.33) | 74 (94.87) | 5.231 | 0.022 |
Compared with the control group, the operation time, intraoperative blood loss, and hospital stay in the observation group were statistically shorter (P < 0.001; Table 3).
| Surgical indices | Control group (n = 72) | Observation group (n = 78) | t | P value |
| Operation time (minute) | 50.76 ± 6.42 | 43.96 ± 4.97 | 7.285 | < 0.001 |
| Intraoperative blood loss (mL) | 37.00 ± 7.38 | 24.64 ± 6.24 | 11.104 | < 0.001 |
| Hospital stay (day) | 7.24 ± 2.63 | 5.47 ± 1.73 | 4.905 | < 0.001 |
The observation group had markedly shorter time to postoperative ambulation, gastrointestinal function recovery, and food intake than the control group (P < 0.001; Table 4).
| Postoperative recovery index | Control group (n = 72) | Observation group (n = 78) | t | P value |
| Time to ambulation (hour) | 27.90 ± 4.80 | 22.37 ± 3.98 | 7.703 | < 0.001 |
| Time to gastrointestinal function recovery (day) | 3.42 ± 1.32 | 2.15 ± 0.90 | 6.930 | < 0.001 |
| Time to food intake (day) | 3.76 ± 1.27 | 2.69 ± 1.02 | 5.709 | < 0.001 |
By counting the incidence of adverse events such as postoperative bleeding, pelvic infection, puncture site infection, and ileus in the two groups, we found that the total incidence of adverse events was significantly lower in the observation group than in the control group (P < 0.05; Table 5).
| Postoperative recovery indexes | Control group (n = 72) | Observation group (n = 78) | χ2 | P value |
| Postoperative bleeding | 5 (6.94) | 2 (2.56) | ||
| Pelvic infection | 3 (4.17) | 1 (1.28) | ||
| Puncture site infection | 3 (4.17) | 0 (0.00) | ||
| Ileus | 1 (1.39) | 0 (0.00) | ||
| Total | 12 (16.67) | 3 (3.85) | 6.838 | 0.009 |
The two groups showed the same preoperative TNF-α, IL-6, and CRP levels (P > 0.05). Postoperatively, these indexes evidently increased in both groups but with lower levels in the observation group than in the control group (all P < 0.05; Figure 1).
Based on logistic regression analysis, sex, age, BMI, time from acute attack to admission, family medical history, preoperative TNF-α, preoperative IL-6, preoperative CRP, and treatment modality were considered to be not independent factors influencing patient efficacy (P > 0.05; Table 6).
| Factor | β | SE | Wald | P value | Exp (β) | 95%CI |
| Sex | -0.088 | 0.566 | 0.024 | 0.876 | 0.915 | 0.302-2.777 |
| Age | -0.015 | 0.044 | 0.122 | 0.726 | 0.985 | 0.904-1.073 |
| Body mass index (kg/m2) | -0.109 | 0.116 | 0.883 | 0.347 | 0.897 | 0.714-1.126 |
| Time from acute onset to admission (hour) | 0.144 | 0.105 | 1.902 | 0.168 | 1.155 | 0.941-1.418 |
| Family medical history | -0.214 | 0.916 | 0.054 | 0.816 | 0.808 | 0.134-4.861 |
| Preoperative TNF-α (ng/L) | -0.872 | 0.941 | 0.859 | 0.354 | 0.418 | 0.066-2.643 |
| Preoperative IL-6 (pg/mL) | -0.007 | 0.030 | 0.058 | 0.809 | 0.993 | 0.937-1.052 |
| Preoperative CRP (mg/L) | 0.065 | 0.115 | 0.319 | 0.572 | 1.067 | 0.852-1.335 |
| Treatment modality | 1.214 | 0.621 | 3.820 | 0.051 | 3.368 | 0.997-11.380 |
The etiology of AP is intricate. Factors such as diet, genetics, ischemia, inflammation, and fecalith-induced lumen obstruction serve as risk factors for the occurrence of AP[16]. The pathological mechanism of AP entails appendiceal dilation resulting from the obstruction of the appendiceal orifice, thereby influencing the normal drainage of its contents. The stagnant contents and increased bacterial load in the appendix can initiate excessive inflammation, which leads to appendiceal infection and inflammation, thereby triggering AP[17,18]. Timely and effective surgical intervention for this disease is conducive to averting serious complications such as appendiceal perforation[19]. In this study, LA with meso
First, the total effective rate of treatment in the observation group of patients undergoing LA with mesoappendix dissection was remarkably high, indicating that LA with mesoappendix dissection for patients with AP can maximize the therapeutic efficacy and facilitate the amelioration of patients’ symptoms and signs. In addition, the operation time, intraoperative blood loss, hospital stay, time to ambulation, gastrointestinal function recovery, and food intake in patients with AP treated by LA with mesoappendix dissection were significantly less, indicating that this therapeutic approach can improve the surgical outcomes of patients with AP and promote postoperative recovery compared with conventional LA. Moreover, LA with mesoappendix dissection can simplify intraoperative hemostasis compared with conventional LA, which is conducive to shortening the operation time[20]. Meanwhile, this therapy can separate and remove the ap
Notwithstanding the demonstration of the clinical effectiveness, safety, and other clinical advantages of LA with mesoappendix dissection in patients with AP, this study still has several limitations that necessitate further amelioration. First, the sample recruitment for this study was confined to a single center, and the temporal scope of the investigation was hindered. The expansion of the research sample pool by incorporating data from multiple centers over a more prolonged period would incontrovertibly augment the accuracy and reliability of the research findings. Second, the allocation of surgical modalities in this study might be susceptible to biases caused by the age of patients upon admission, the duration of symptom manifestation, and the predilection of the surgeons involved. Finally, relevant investigations regarding immune-related indices are lacking. The supplementation of such analyses could provide deeper insights into the potential influence of the two surgical methods on the immune function of patients. Future research initiatives will be directed toward progressively enhancing and refining this study by addressing the aforementioned concerns.
Based on the results, LA with mesoappendix dissection for the treatment of patients with AP can enhance curative efficacy and surgical outcomes, facilitate postoperative rehabilitation, decrease the incidence of adverse events, and prevent excessive elevation of inflammatory markers such as TNF-α, IL-6, and CRP caused by surgical stimulation, indicating its great potential for clinical applications.
| 1. | Chaochankit W, Boocha A, Samphao S. Negative appendectomy rate in patients diagnosed with acute appendicitis. BMC Surg. 2022;22:404. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 22] [Reference Citation Analysis (0)] |
| 2. | Smith HF. A review of the function and evolution of the cecal appendix. Anat Rec (Hoboken). 2023;306:972-982. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 3. | Alotaibi AM, Alfawaz M, Felemban L, Moshref L, Moshref R. Complicated appendicitis increases the hospital length of stay. Surg Open Sci. 2022;9:64-68. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 15] [Reference Citation Analysis (0)] |
| 4. | Pineda Villeda RH, Flores Reyes DL, Suazo Rivera JF. Acute Appendicitis: Epidemiological, Clinical, Surgical, and Post-surgical Characteristics in a Honduran General Hospital. Cureus. 2023;15:e40428. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 5. | Li GM, Zhou H, Liang MY, Wu SY, Jiang FX, Wang ZL. Diagnostic role of multislice spiral computed tomography combined with clinical manifestations and laboratory tests in acute appendicitis subtypes. J Investig Med. 2023;71:17-22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 6. | Stöß C, Nitsche U, Neumann PA, Kehl V, Wilhelm D, Busse R, Friess H, Nimptsch U. Acute Appendicitis: Trends in Surgical Treatment—A Population-Based Study of Over 800 000 Patients. Dtsch Arztebl Int. 2021;118:244-249. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 7. | Henriksen SR, Christophersen C, Rosenberg J, Fonnes S. Varying negative appendectomy rates after laparoscopic appendectomy: a systematic review and meta-analysis. Langenbecks Arch Surg. 2023;408:205. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 20] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 8. | Moriguchi T, Machigashira S, Sugita K, Kawano M, Yano K, Onishi S, Yamada K, Yamada W, Masuya R, Kawano T, Nakame K, Mukai M, Kaji T, Ieiri S. A Randomized Trial to Compare the Conventional Three-Port Laparoscopic Appendectomy Procedure to Single-Incision and One-Puncture Procedure That Was Safe and Feasible, Even for Surgeons in Training. J Laparoendosc Adv Surg Tech A. 2019;29:392-395. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 13] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 9. | Kang DB, Lee SH, Lee SY, Oh JT, Park DE, Lee C, Choi DH, Park WC, Lee JK. Application of single incision laparoscopic surgery for appendectomy in children. J Korean Surg Soc. 2012;82:110-115. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 10. | Xie F, Wang L, Chen L, Li S, Shen Q, Li X, Liu T, Chen Y, Wang D. Clinical Characteristics of Pediatric Patients With Septic Shock Caused by Acute Appendicitis: A Case Series. Pediatr Emerg Care. 2023;39:511-515. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 11. | Li XL, Zhang QM, Zhang WP, Liu TT. Mini-Incision Open Appendectomy with Incision Skin Tissue Retractor vs. Laparoscopic Appendectomy: A Retrospective Study of the Management of Child Acute Appendicitis. Adv Ther. 2018;35:2176-2185. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 12. | Zhang N, Li Y, Zhou R. Comparison of Single-Person Laparoscopic Appendectomy Using a Novel Brace-Assisted Camera Holding System and Conventional Laparoscopic Appendectomy: A Neural Network Algorithm Analysis. Contrast Media Mol Imaging. 2022;2022:5915670. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 13. | Lee JS, Hong TH. Comparison of various methods of mesoappendix dissection in laparoscopic appendectomy. J Laparoendosc Adv Surg Tech A. 2014;24:28-31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 19] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 14. | Bartenstein A, Cholewa D, Boillat C, Zachariou Z. Dissection of the appendix with ultrasound-activated scalpel: an experimental study in pediatric laparoscopic appendectomy. J Laparoendosc Adv Surg Tech A. 2010;20:199-204. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 15. | Moris D, Paulson EK, Pappas TN. Diagnosis and Management of Acute Appendicitis in Adults: A Review. JAMA. 2021;326:2299-2311. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 178] [Cited by in RCA: 209] [Article Influence: 41.8] [Reference Citation Analysis (112)] |
| 16. | Song MY, Ullah S, Yang HY, Ahmed MR, Saleh AA, Liu BR. Long-term effects of appendectomy in humans: is it the optimal management of appendicitis? Expert Rev Gastroenterol Hepatol. 2021;15:657-664. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 20] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 17. | Petruzziello C, Saviano A, Ojetti V. Probiotics, the Immune Response and Acute Appendicitis: A Review. Vaccines (Basel). 2023;11:1170. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 15] [Reference Citation Analysis (0)] |
| 18. | Monsonis B, Mandoul C, Millet I, Taourel P. Imaging of appendicitis: Tips and tricks. Eur J Radiol. 2020;130:109165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 16] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 19. | Baek HN, Jung YH, Hwang YH. Laparoscopic versus open appendectomy for appendicitis in elderly patients. J Korean Soc Coloproctol. 2011;27:241-245. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 11] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 20. | Davila D, Russek K, Franklin ME Jr. Laparoscopic appendectomy: vascular control of the appendicular artery using monopolar cauterization versus clips. J Laparoendosc Adv Surg Tech A. 2012;22:165-167. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 21. | Hori T, Machimoto T, Kadokawa Y, Hata T, Ito T, Kato S, Yasukawa D, Aisu Y, Kimura Y, Sasaki M, Takamatsu Y, Kitano T, Hisamori S, Yoshimura T. Laparoscopic appendectomy for acute appendicitis: How to discourage surgeons using inadequate therapy. World J Gastroenterol. 2017;23:5849-5859. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 21] [Cited by in RCA: 22] [Article Influence: 2.4] [Reference Citation Analysis (5)] |
| 22. | Poprom N, Wilasrusmee C, Attia J, McEvoy M, Thakkinstian A, Rattanasiri S. Comparison of postoperative complications between open and laparoscopic appendectomy: An umbrella review of systematic reviews and meta-analyses. J Trauma Acute Care Surg. 2020;89:813-820. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 37] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 23. | Xiao Z, Wu L, Li J, He S, Chen J, Li L, Xu D, Kang Y. Application of transumbilical single-incision laparoscopy in the treatment of complicated appendicitis in overweight/obese adolescents. BMC Pediatr. 2024;24:593. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 24. | Di Saverio S, Mandrioli M, Sibilio A, Smerieri N, Lombardi R, Catena F, Ansaloni L, Tugnoli G, Masetti M, Jovine E. A cost-effective technique for laparoscopic appendectomy: outcomes and costs of a case-control prospective single-operator study of 112 unselected consecutive cases of complicated acute appendicitis. J Am Coll Surg. 2014;218:e51-e65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 43] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 25. | Zhang P, Zhang Q, Zhao H, Li Y. Factors affecting the length of hospital stay after laparoscopic appendectomy: A single center study. PLoS One. 2020;15:e0243575. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 26. | Sobczak J, Burzyńska M, Sikora A, Wysocka A, Karawani J, Sikora JP. Post-Traumatic Stress Response and Appendicitis in Children-Clinical Usefulness of Selected Biomarkers. Biomedicines. 2023;11:1880. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 27. | Liu J, Chen G, Mao X, Jiang Z, Jiang N, Xia N, Lin A, Duan G. Single-incision laparoscopic appendectomy versus traditional three-hole laparoscopic appendectomy for acute appendicitis in children by senior pediatric surgeons: a multicenter study from China. Front Pediatr. 2023;11:1224113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 28. | Zhang A, Zhang Y, Fan N, Hui Y, Zhou Y, Zeng L, Wang C, Shang L, Qi K, He X, Lin Y, Jiang X. Modified endoscopic retrograde appendicitis therapy vs. laparoscopic appendectomy for uncomplicated acute appendicitis in children. Dig Endosc. 2024;36:1012-1020. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/