Published online Dec 27, 2025. doi: 10.4240/wjgs.v17.i12.113408
Revised: September 13, 2025
Accepted: November 7, 2025
Published online: December 27, 2025
Processing time: 122 Days and 22.8 Hours
Esophageal cancer surgery is associated with a high risk of postoperative pulmo
To evaluate the effects of early postoperative "Liuzijue" training on pulmonary function and pneumonia incidence following radical esophagectomy.
This retrospective study included 306 patients who underwent esophagectomy. The control group (n = 163) received standard care, consisting of abdominal breathing, incentive spirometry, and early ambulation. The intervention group (n = 143) received the same standard care plus twice-daily "Liuzijue" training for 14 days. Primary outcomes were the incidence of pneumonia (defined by Centers for Disease Control and Prevention criteria) and changes (Δ) in forced vital capa
The "Liuzijue" intervention was associated with a significantly lower incidence of pneumonia (11.9% vs 24.5%, P = 0.005; relative risk = 0.48). Significant improvements were observed in ΔFVC (+502.1 mL vs +326.5 mL, P < 0.001), ΔFEV1 (+701.7 mL vs +434.4 mL, P < 0.001), and ΔMVV (+19.4 L/minute vs +14.4 L/minute, P < 0.001). Absolute FEV1 values on postoperative day 14 were higher in the intervention group (2270.8 mL vs 2066.1 mL, P = 0.021), along with significantly lower Borg dyspnea/fatigue scores (P = 0.045). No significant differences were observed in changes in diffusing capacity of the lung for carbon monoxide, total lung capacity, or 6-minute walk distance.
Early initiation of "Liuzijue" training after esophagectomy is associated with reduced pneumonia incidence and accelerated recovery of key pulmonary function parameters. These findings support the integration of "Liuzijue" into enhanced recovery after surgery protocols for esophageal cancer patients.
Core Tip: Early postoperative "Liuzijue" Qigong training significantly reduces the risk of postoperative pneumonia and accelerates the recovery of core pulmonary function parameters in patients undergoing radical esophagectomy. As a low-intensity intervention, it integrates coordinated breathing techniques with vocalization to enhance postoperative respiratory muscle function. This approach is particularly well-suited for incorporation into enhanced recovery after surgery pathways, offering a safe, feasible, and effective adjunct to conventional respiratory rehabilitation strategies.
- Citation: Bai Y, Zhang ZL, Qiao L, Shi LL, Wang J, Nian H, Du QC, Tian ZH, Yao ZL, Wu YB. "Liuzijue" Qigong training enhances early pulmonary function recovery after esophageal cancer surgery. World J Gastrointest Surg 2025; 17(12): 113408
- URL: https://www.wjgnet.com/1948-9366/full/v17/i12/113408.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v17.i12.113408
Esophageal cancer, a highly aggressive malignancy of the digestive tract, has shown a steadily increasing global incidence in recent years, particularly in specific high-risk regions[1]. According to global statistics, it ranks as the seventh leading cause of cancer-related death worldwide, imposing substantial physical and psychological burdens on patients and placing significant economic strain on healthcare systems[2]. Currently, surgical resection combined with radiotherapy and chemotherapy constitutes the primary treatment approach for esophageal cancer. Although these modalities have improved survival outcomes, the rate of postoperative complications remains high. Among them, respiratory complications – such as pneumonia and atelectasis – are especially common and are major contributors to intensive care unit readmission and increased mortality[3]. Therefore, identifying effective postoperative rehabilitation strategies, particularly those targeting pulmonary function recovery, is critically important.
Conventional rehabilitation approaches have notable limitations. While preoperative inspiratory muscle training (IMT) has been widely studied, its effectiveness in patients undergoing esophagectomy remains controversial and lacks specificity for early postoperative respiratory recovery[4-6]. In recent years, fast-track surgery-based respiratory interventions – such as diaphragmatic breathing and incentive spirometry – have demonstrated benefits in promoting lung function recovery. However, these methods often require equipment or intense patient effort, potentially limiting adherence and tolerance during the early postoperative period[7]. Under these circumstances, the traditional Chinese Qigong practice known as "Liuzijue" (Six-Character Formula) has emerged as a promising low-intensity intervention. By integrating specific vocalizations (Xu, He, Hu, Xi, Chui, Si) with coordinated respiratory movements, "Liuzijue" effectively regulates breathing patterns, enhances diaphragmatic activity, and facilitates sputum clearance[8]. Despite its potential, the application of "Liuzijue" in postoperative management of esophageal cancer remains underdeveloped and insufficiently systematized. Most existing studies focus on chronic respiratory diseases – such as chronic obstructive pulmonary disease (COPD) – or neurological rehabilitation, with a marked lack of high-quality randomized controlled trials (RCTs) evaluating its efficacy in enhancing pulmonary recovery after esophagectomy. Notably, evidence regarding its impact during the critical early postoperative phase (within two weeks) remains limited[9,10].
This study aims to address this research gap through a single-center retrospective analysis to investigate, for the first time, the effects of early postoperative "Liuzijue" training on key pulmonary function parameters – forced expiratory volume in 1 second (FEV1), forced vital capacity (FVC), and maximum voluntary ventilation (MVV) – and on the incidence of postoperative pneumonia within the first two weeks following esophagectomy. It further seeks to compare its efficacy with that of conventional rehabilitation strategies. By doing so, this research intends to provide evidence-based support for respiratory rehabilitation in esophageal cancer patients, promote the integration of "Liuzijue" into enhanced recovery after surgery (ERAS) protocols, and ultimately improve both quality of life and long-term clinical outcomes.
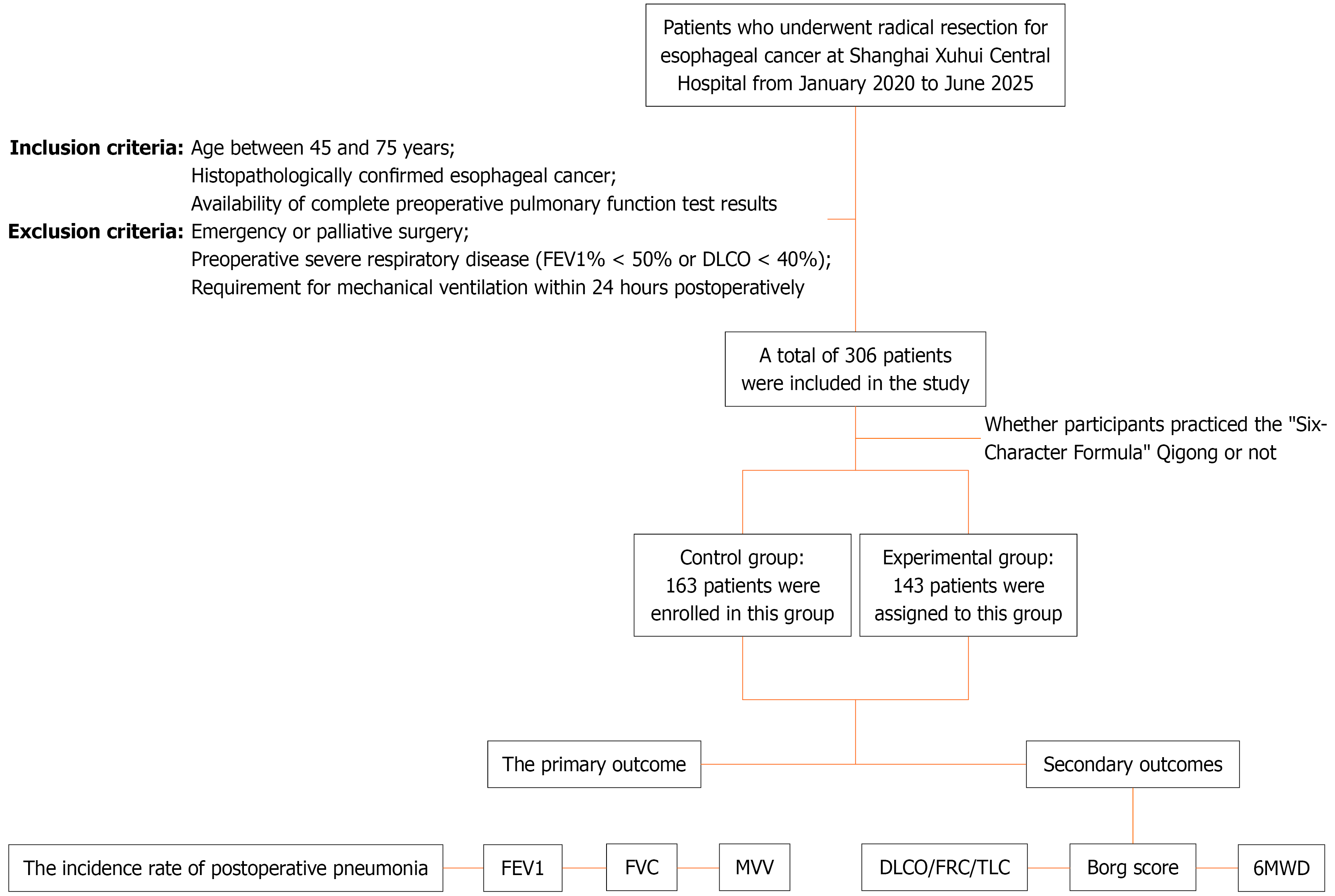
This study employed a single-center retrospective design to systematically analyze clinical data from 306 patients who underwent radical esophagectomy at our institution between January 2020 and June 2025 (Figure 1). Data were extracted from the electronic medical record system to compare the effects of conventional postoperative care (control group, n = 163) vs conventional care supplemented with "Liuzijue" Qigong training (experimental group, n = 143) on early pulmonary function recovery after surgery. The study protocol was approved by Ethics Committee of Shanghai Xuhui Central Hospital, with a waiver of informed consent.
Eligible participants were adults aged 45-75 years with pathologically confirmed esophageal cancer who underwent radical esophagectomy, including transthoracic esophagectomy (TTE), Ivor Lewis procedure, or three-port minimally invasive McKeown esophagectomy, and had complete preoperative pulmonary function evaluations. Exclusion criteria included emergency or palliative surgery, severe preoperative respiratory impairment [FEV1 < 50% predicted or diffusing capacity of the lung for carbon monoxide (DLCO) < 40% predicted], or requirement for mechanical ventilation within 24 hours postoperatively. A total of 306 patients were included, with balanced baseline characteristics (Table 1). The mean age was 58.55 ± 7.58 years; 60.5% (185/306) were male, and the average body mass index (BMI) was 24.03 ± 1.42 kg/m². There were no statistically significant differences in surgical approach distribution (P = 0.997), and preoperative pulmonary function parameters were comparable between groups (all P > 0.05).
| Variable | Overall (n = 306) | Control group (n = 163) | Experimental group (n = 143) | P value |
| Age | 58.55 ± 7.58 | 58.43 ± 7.60 | 58.69 ± 7.58 | 0.938 |
| Sex | 0.733 | |||
| Male | 185 | 100 (61.35) | 85 (59.44) | |
| Female | 121 | 63 (38.65) | 58 (40.56) | |
| Body mass index | 24.03 ± 1.42 | 23.97 ± 1.41 | 24.11 ± 1.43 | 0.907 |
| Smoking | 0.649 | |||
| Yes | 137 | 71 (43.56) | 66 (46.15) | |
| No | 167 | 92 (56.44) | 77 (53.85) | |
| Surgical technique | 0.997 | |||
| Transthoracic esophagectomy | 250 | 133 (81.60) | 117 (81.82) | |
| Ivor Lewis procedure | 39 | 21 (12.88) | 18 (12.59) | |
| Three-port minimally invasive McKeown esophagectomy | 17 | 9 (5.52) | 8 (5.59) | |
| Surgical duration (minute) | 194.62 ± 35.91 | 194.06 ± 36.13 | 195.27 ± 35.77 | 0.927 |
| Intraoperative blood loss | 100.38 ± 23.02 | 99.40 ± 23.13 | 101.50 ± 22.93 | 0.786 |
| Postoperative pneumonia | 0.005 | |||
| Yes | 57 | 40 (24.54) | 17 (11.89) | |
| No | 249 | 123 (75.46) | 126 (88.11) |
The control group received standard postoperative respiratory rehabilitation starting 24 hours after surgery, consisting of three daily sessions of abdominal breathing training (10 minutes each), incentive spirometry (15 breaths per session, twice daily), and early ambulation (≥ 30 minutes/day beginning on postoperative day 2). The experimental group received identical standard care plus twice-daily "Liuzijue" Qigong training. The Qigong intervention began 24 hours post-surgery and continued through postoperative day 14, with two 30-minute sessions daily (at 08:00 and 16:00). Each session involved sequential vocalization of the six sounds – "Xu, He, Hu, Si, Chui, Xi" – synchronized with a controlled breathing rhythm (4-second inhalation, 6-second exhalation) and coordinated guiding movements. To ensure fidelity, certified Qigong instructors provided on-site instruction and supervision during the first three sessions. Patients also received standardized instructional videos for reinforcement during self-practice.
Primary outcomes were: (1) Incidence of postoperative pneumonia, defined according to Centers for Disease Control and Prevention criteria; and (2) Changes in pulmonary function parameters – FVC, FEV1, and MVV – from baseline (within 48 hours preoperatively) to postoperative day 14. Secondary outcomes included changes in DLCO, functional residual capacity, total lung capacity (TLC), 6-minute walk distance (6MWD), and Borg Dyspnea Scale scores. All outcomes were assessed at two time points: (1) Preoperatively (baseline); and (2) Postoperative day 14. The 14th postoperative day was designated as the primary endpoint. A 90-day follow-up period was maintained to monitor long-term complications, including anastomotic leakage and delayed-onset pneumonia.
Statistical analyses were conducted using Statistical Package for the Social Sciences version 26.0. Continuous variables are presented as mean ± SD; for non-normally distributed data (assessed via Kolmogorov-Smirnov test, P ≤ 0.05), median (range) was used. Normality was evaluated using the Kolmogorov-Smirnov test, and homogeneity of variance was tested using Levene’s test. For normally distributed data with equal variances, independent samples t-tests were applied for intergroup comparisons. Categorical variables are expressed as frequency (percentage) and compared using the χ² test. To adjust for potential baseline imbalances, analysis of covariance was used to compare changes in pulmonary function parameters (Δvalues = postoperative value – preoperative value). All tests were two-tailed, with statistical significance set at α = 0.05.
A total of 306 patients who underwent radical esophagectomy for esophageal cancer were included in this study, with 163 assigned to the control group and 143 to the experimental group. As shown in Table 1, no significant differences were observed between groups in demographic characteristics (mean age: 58.55 ± 7.58 years; 60.5% male), clinical baseline data (BMI: 24.03 ± 1.42 kg/m²; smoking rate: 44.8%), surgical parameters (operation time: 194.62 ± 35.91 minutes; intraoperative blood loss: 100.38 ± 23.02 mL), or distribution of surgical approaches (TTE: 81.7%) (all P > 0.05). These results indicate good baseline comparability between the two groups. Notably, the incidence of postoperative pneumonia was significantly lower in the experimental group (11.9%, 17/143) than in the control group (24.5%, 40/163) (P = 0.005). This corresponds to an absolute risk reduction of 12.7% (95%CI: 3.7%-21.6%) and a relative risk (RR) reduction of 52% (RR = 0.48, 95%CI: 0.29%-0.83), indicating a clinically meaningful benefit of the "Liuzijue" Qigong intervention.
As presented in Table 2, preoperative pulmonary function and exercise capacity were comparable between the two groups (all P > 0.05). Key parameters – including FVC (3515.4 ± 840.6 mL vs 3491.9 ± 845.2 mL), FEV1 (2767.8 ± 740.8 mL vs 2705.2 ± 717.4 mL), and DLCO (19.9 ± 5.8 mL/minute/mmHg vs 19.8 ± 5.3 mL/minute/mmHg) – showed no significant differences. MVV (121.2 ± 39.3 L/minute vs 113.6 ± 37.4 L/minute, P = 0.084) did not differ significantly but remained within a clinically acceptable range (difference < 6.5%). Exercise tolerance, assessed by 6MWD (448.4 ± 7.9 m vs 449.7 ± 7.4 m) and Borg fatigue score [1 (0-2) vs 1 (0-3)], was also similar across groups. These findings support that subsequent between-group differences in pulmonary function changes (Δvalues) reflect the effect of the intervention rather than baseline imbalances.
| Variable | Overall (n = 306) | Control group (n = 163) | Experimental group (n = 143) | P value |
| Forced vital capacity | 3502.9 ± 841.8 | 3491.9 ± 845.2 | 3515.4 ± 840.6 | 0.808 |
| FEV1 | 2734.4 ± 727.9 | 2705.2 ± 717.4 | 2767.8 ± 740.8 | 0.454 |
| FEV1 to forced vital capacity ratio | 90.0 ± 17.6 | 90.4 ± 17.8 | 89.5 ± 17.5 | 0.675 |
| Diffusing capacity of the lung for carbon monoxide | 19.8 ± 5.6 | 19.8 ± 5.3 | 19.9 ± 5.8 | 0.860 |
| Maximum voluntary ventilation | 117.2 ± 38.4 | 113.6 ± 37.4 | 121.2 ± 39.3 | 0.084 |
| Total lung capacity | 5964.4 ± 1146.7 | 5928.8 ± 1108.0 | 6005.1 ± 1192.0 | 0.562 |
| Functional residual capacity | 2236.8 ± 428.0 | 2230.9 ± 427.3 | 2243.4 ± 430.3 | 0.799 |
| 6-minute walk distance | 449.1 ± 7.6 | 449.7 ± 7.4 | 448.4 ± 7.9 | 0.143 |
| Modified Borg scale | 1 (0-3) | 1 (0-3) | 1 (0-2) | 0.821 |
At the 14-day postoperative assessment (Table 3), the experimental group demonstrated significantly higher FEV1 values (2270.8 ± 797.2 mL) compared to the control group (2066.1 ± 740.5 mL) (P = 0.021), representing a 9.9% improvement. The median Borg dyspnea/fatigue score was lower in the experimental group [2 (0-4) vs 2 (1-3), P = 0.045], indicating better subjective respiratory recovery. However, no significant differences were observed in FVC (3265.4 ± 861.3 mL vs 3013.3 ± 813.6 mL, P = 0.115) or DLCO (17.1 ± 5.9 mL/minute/mmHg vs 17.0 ± 5.9 mL/minute/mmHg, P = 0.880), which may be attributable to the relatively short postoperative recovery period.
| Variable | Overall (n = 306) | Control group (n = 163) | Experimental group (n = 143) | P value |
| Forced vital capacity | 3094.4 ± 841.4 | 3265.4 ± 861.3 | 3013.3 ± 813.6 | 0.115 |
| FEV1 | 2734.4 ± 727.9 | 2270.8 ± 797.2 | 2066.1 ± 740.5 | 0.021 |
| FEV1 to forced vital capacity ratio | 85.6 ± 10.1 | 85.1 ± 10.7 | 86.0 ± 9.3 | 0.418 |
| Diffusing capacity of the lung for carbon monoxide | 17.1 ± 5.9 | 17.1 ± 5.9 | 17.0 ± 5.9 | 0.880 |
| Maximum voluntary ventilation | 100.4 ± 35.6 | 99.1 ± 35.5 | 101.9 ± 35.7 | 0.507 |
| Total lung capacity | 5624.4 ± 1106.5 | 5622.3 ± 1110.3 | 5626.8 ± 1106.1 | 0.972 |
| Functional residual capacity | 2976.4 ± 592.8 | 2990.1 ± 606.8 | 2960.7 ± 578.2 | 0.664 |
| 6-minute walk distance | 404.2 ± 14.6 | 404.9 ± 14.2 | 403.4 ± 15.0 | 0.379 |
| Modified Borg scale | 2 (0-4) | 2 (1-3) | 2 (0-4) | 0.045 |
The experimental group showed significantly greater improvements in key pulmonary function parameters than the control group (Table 4). Accelerated lung volume recovery: ΔFVC was significantly greater in the experimental group (+502.1 ± 35.0 mL) than in the control group (+326.5 ± 26.7 mL) (P < 0.001), representing a 53.8% increase, suggesting enhanced lung expansion capacity following Qigong training. Enhanced expiratory function: ΔFEV1 improvement was significantly higher in the experimental group (+701.7 ± 47.1 mL) than in the control group (+434.4 ± 90.3 mL) (P < 0.001), with a 61.5% increase, indicating reduced airway resistance and improved sputum clearance. Improved respiratory muscle endurance: ΔMVV increased more in the experimental group (+19.4 ± 11.7 L/minute) than in the control group (+14.4 ± 10.1 L/minute) (P < 0.001), a 34.7% improvement, suggesting enhanced diaphragmatic endurance. Secondary outcomes, including Δ6MWD and ΔTLC, did not differ significantly between groups (P > 0.05), potentially due to early postoperative activity limitations or insufficient sensitivity of the measurement tools.
| Variable | Overall (n = 306) | Control group (n = 163) | Experimental group (n = 143) | P value |
| ∆Forced vital capacity | 408.5 ± 93.0 | 326.5 ± 26.7 | 502.1 ± 35.0 | < 0.001 |
| ∆FEV1 | 559.3 ± 152.5 | 434.4 ± 90.8 | 701.7 ± 47.1 | < 0.001 |
| ∆FEV1 to forced vital capacity ratio | 4.4 ± 19.9 | 5.3 ± 20.4 | 3.5 ± 19.3 | 0.435 |
| ∆Diffusing capacity of the lung for carbon monoxide | 2.7 ± 1.8 | 2.6 ± 1.8 | 2.8 ± 1.8 | 0.305 |
| ∆Maximum voluntary ventilation | 16.8 ± 11.1 | 14.4 ± 10.1 | 19.4 ± 11.7 | < 0.001 |
| ∆Total lung capacity | 340.0 ± 699.8 | 306.4 ± 675.8 | 378.2 ± 726.7 | 0.371 |
| ∆Functional residual capacity | -739.6 ± 733.4 | -759.2 ± 736.4 | -717.3 ± 731.9 | 0.619 |
| ∆6-minute walk distance | 45.0 ± 12.6 | 44.9 ± 12.7 | 45.0 ± 12.5 | 0.896 |
| ∆Modified Borg scale | -1.0 (-2 to 1) | -1.0 (-2 to 1) | -1.0 (-2 to 1) | 0.815 |
This study is the first to demonstrate a reduction in the incidence of postoperative pulmonary complications (PPCs) associated with the "Liuzijue" Qigong training intervention. Previous evidence indicates that preoperative IMT can enhance diaphragmatic excursion (DE); however, this improvement has not consistently translated into significant gains in lung function or sustained reductions in PPCs[6,11]. Importantly, research on integrated interventions for gastrointes
Although preoperative IMT has been shown to improve DE, with effects lasting up to three months postoperatively, it has not significantly improved core pulmonary function parameters such as FEV1 and FVC[6,13-15]. For example, in patients undergoing cardiac surgery, IMT enhances diaphragmatic function without producing statistically significant changes in FEV1 or FVC[4]. The coordinated inhalation-exhalation rhythm in "Liuzijue" Qigong training may compensate for the limitations of IMT by promoting more balanced ventilation distribution. Moreover, the weak association between respiratory training and improvements in diaphragmatic endurance – such as changes in MVV – suggests that surgical trauma, including diaphragmatic nerve inhibition or pleural adhesions, may attenuate the benefits of preoperative interventions[16,17].
The control group followed the standard ERAS protocol, which includes abdominal breathing and incentive spirometry and has demonstrated efficacy in improving pulmonary function. However, the experimental group, which incorporated "Liuzijue" Qigong into the regimen, exhibited more pronounced improvements in lung function recovery. This difference may be attributed to the low-intensity, equipment-free nature of the intervention – consisting of two 30-minute sessions daily – featuring gentle movements suitable for postoperative patients and avoiding the high respiratory load associated with incentive spirometry[18,19]. At 14 days post-surgery, the experimental group showed a 9.9% higher FEV1 than the control group, confirming its short-term clinical benefit. In patients after lung cancer surgery, respiratory training – including Qigong-based interventions – has been shown to significantly reduce pneumonia incidence and improve FEV1[20]. A recent study on post-coronavirus disease 2019 rehabilitation highlighted the feasibility of home-based pulmonary rehabilitation using portable lung function monitoring devices, suggesting that "Liuzijue" Qigong, due to its minimal technical requirements, may be particularly well-suited for such settings[21].
The findings of this study demonstrate that "Liuzijue" Qigong training significantly reduces postoperative pneumonia incidence and improves key pulmonary function parameters, including ΔFEV1, ΔFVC, and ΔMVV. Notably, the ΔFEV1 improvement of 267.3 mL exceeds the minimal clinically important difference for COPD (100-140 mL) and falls within the critical range (200-400 mL) associated with reduced respiratory mortality in surgical populations, further supported by its association with a 52% reduction in pneumonia risk[20]. However, no significant differences were observed in secondary outcomes such as ΔDLCO, Δ6MWD, or ΔTLC. This is consistent with existing literature indicating that pulmonary function recovery remains incomplete at three months post-surgery[6,22]. At 14 days postoperatively, physical limitations – including incision pain and indwelling drainage tubes – likely hindered improvements in 6MWD, a finding aligned with results from previous IMT studies[11,23]. Although the Borg dyspnea/fatigue score showed a statistically significant improvement (P = 0.045), the lower scores in the experimental group are consistent with reports of improved respiratory-related fatigue following structured rehabilitation interventions[24].
The "Qi-regulating" mechanism of "Liuzijue" Qigong training in traditional Chinese medicine (TCM), which involves modulating the flow of Qi through specific vocalizations, demonstrates a plausible correspondence with modern physiological effects. This mechanism comprises three key components: (1) Prolonged exhalation and shortened inhalation (6-second exhalation/4-second inhalation), which activates the parasympathetic nervous system and reduces respiratory rate[8]; (2) The vibratory effects of consonant sounds such as "Xu" (Hsu) and "Hu" on the airways, enhancing mucociliary clearance – a mechanism analogous to the "active cycle of breathing technique" in Western respiratory therapy[9]; and (3) Diaphragm-engaged abdominal breathing, which improves oxygenation efficiency and aligns with the TCM concept of "replenishing lung Qi" through the principle of "Qi sinking to the dantian" and "earth nurturing metal". Consequently, the observed reduction in pneumonia risk and improvement in pulmonary function represent a clinical translation of traditional Qi regulation into contemporary neuro-respiratory physiological pathways.
This study employed a single-center retrospective design, which may introduce selection bias due to institution-specific clinical practices. Future multi-center RCTs are needed to confirm the generalizability of these findings. Additionally, limiting follow-up to 14 days post-surgery restricts the ability to assess long-term recovery trajectories of key pulmonary parameters such as DLCO and exercise tolerance. Mechanistic insights are further limited by the absence of direct measurements of diaphragmatic motion and sputum clearance. Future studies should incorporate advanced techniques – such as ultrasound imaging and respiratory biomechanics analysis – to better elucidate the physiological pathways underlying the effects of the "Six-Character Formula".
"Liuzijue" Qigong training significantly reduces the incidence of postoperative pneumonia and accelerates recovery of core pulmonary function parameters in patients undergoing esophagectomy, with a favorable safety profile. These findings suggest that traditional Qigong may serve as a valuable adjunct to postoperative respiratory rehabilitation in the context of esophageal cancer surgery.
We gratefully acknowledge the invaluable contributions of all colleagues in the Department of Thoracic Surgery at Shanghai Xuhui Central Hospital. Their dedicated efforts in clinical data collection and patient management were instrumental in the successful execution of this study.
| 1. | Morgan E, Soerjomataram I, Rumgay H, Coleman HG, Thrift AP, Vignat J, Laversanne M, Ferlay J, Arnold M. The Global Landscape of Esophageal Squamous Cell Carcinoma and Esophageal Adenocarcinoma Incidence and Mortality in 2020 and Projections to 2040: New Estimates From GLOBOCAN 2020. Gastroenterology. 2022;163:649-658.e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 796] [Cited by in RCA: 755] [Article Influence: 188.8] [Reference Citation Analysis (1)] |
| 2. | Li P, Jing J, Liu W, Wang J, Qi X, Zhang G. Spatiotemporal Patterns of Esophageal Cancer Burden Attributable to Behavioral, Metabolic, and Dietary Risk Factors From 1990 to 2019: Longitudinal Observational Study. JMIR Public Health Surveill. 2023;9:e46051. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 13] [Reference Citation Analysis (0)] |
| 3. | Singh P, Gossage J, Markar S, Pucher PH, Wickham A, Weblin J, Chidambaram S, Bull A, Pickering O, Mythen M, Maynard N, Grocott M, Underwood T; AUGIS/POQI Pulmonary Consensus Group. Association of Upper Gastrointestinal Surgery of Great Britain and Ireland (AUGIS)/Perioperative Quality Initiative (POQI) consensus statement on intraoperative and postoperative interventions to reduce pulmonary complications after oesophagectomy. Br J Surg. 2022;109:1096-1106. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 4. | Assouline B, Cools E, Schorer R, Kayser B, Elia N, Licker M. Preoperative Exercise Training to Prevent Postoperative Pulmonary Complications in Adults Undergoing Major Surgery. A Systematic Review and Meta-analysis with Trial Sequential Analysis. Ann Am Thorac Soc. 2021;18:678-688. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 68] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
| 5. | Smyth E, O'Neill LM, Kearney N, Sheill G, Brennan L, Wade S, Grehan S, Begic S, Egaña M, Ryan R, Fitzmaurice GJ, Murphy RT, McKittrick M, Doyle SL, Walsh C, Ravi N, Donohoe CL, Reynolds JV, Hussey J, Guinan EM. Preoperative Exercise to Improve Fitness in Patients Undergoing Complex Surgery for Cancer of the Lung or Esophagus (PRE-HIIT): A Randomized Controlled Trial. Ann Surg. 2025;282:690-698. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 6. | Mizusawa H, Higashimoto Y, Shiraishi O, Shiraishi M, Sugiya R, Noguchi M, Kanki K, Kimura T, Ishikawa A, Yasuda T. Preoperative inspiratory muscle training preserved diaphragmatic excursion after esophagectomy: a randomized-controlled trial. Esophagus. 2025;22:331-339. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 7. | Zheng Y, Mao M, Li F, Wang L, Zhang X, Zhang X, Wang H, Zhou H, Ji M, Wang Y, Liu L, Zhu Q, Reinhardt JD, Lu X. Effects of enhanced recovery after surgery plus pulmonary rehabilitation on complications after video-assisted lung cancer surgery: a multicentre randomised controlled trial. Thorax. 2023;78:574-586. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 14] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 8. | Zhang Y, Wang C, Yang J, Qiao L, Xu Y, Yu L, Wang J, Ni W, Wang Y, Yao Y, Yong Z, Ding S. Comparing the Effects of Short-Term Liuzijue Exercise and Core Stability Training on Balance Function in Patients Recovering From Stroke: A Pilot Randomized Controlled Trial. Front Neurol. 2022;13:748754. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 9. | Zheng Y, Zhang Y, Li H, Qiao L, Fu W, Yu L, Li G, Yang J, Ni W, Yong Z, Wang Y, Fan H. Comparative Effect of Liuzijue Qigong and Conventional Respiratory Training on Trunk Control Ability and Respiratory Muscle Function in Patients at an Early Recovery Stage From Stroke: A Randomized Controlled Trial. Arch Phys Med Rehabil. 2021;102:423-430. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 26] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 10. | Wang C, Yu L, Yang J, Wang RW, Zheng YN, Zhang Y. Effectiveness of LiuZiJue Qigong versus traditional core stability training for poststroke patients complicated with abnormal trunk postural control: study protocol for a single-center randomized controlled trial. Trials. 2020;21:254. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 11. | Mizusawa H, Higashimoto Y, Shiraishi O, Shiraishi M, Sugiya R, Noguchi M, Fujita S, Kimura T, Ishikawa A, Yasuda T. ASO Visual Abstract: Inspiratory Muscle Training Before Esophagectomy Increases Diaphragmatic Excursion – A Randomized Controlled Trial. Ann Surg Oncol. 2024;31:9362-9363. [RCA] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 12. | Kleef R, Dank M, Herold M, Agoston EI, Lohinszky J, Martinek E, Herold Z, Szasz AM. Comparison of the effectiveness of integrative immunomodulatory treatments and conventional therapies on the survival of selected gastrointestinal cancer patients. Sci Rep. 2023;13:20360. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 13. | Babu TA, Hashim Z, Neyaz Z, Mani VE, Jain N, Bhatia E, Mishra A, Sahoo SK. Nonsurgical hypoparathyroidism is associated with skeletal muscle dysfunction and restrictive lung disease. Eur J Endocrinol. 2023;189:141-148. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 14. | Adolf Helmy M, Magdy Milad L, Hasanin A, Mostafa M. The novel use of diaphragmatic excursion on hospital admission to predict the need for ventilatory support in patients with coronavirus disease 2019. Anaesth Crit Care Pain Med. 2021;40:100976. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 18] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 15. | Zhang YS, Zhang K, Huang L, Wei JX, Bi ZT, Xiao JH, Huang J, Luo CS, Li YD, Zhang JM. The effects of respiratory muscle training on respiratory function and functional capacity in patients with early stroke: a meta-analysis. Eur Rev Aging Phys Act. 2024;21:4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 11] [Reference Citation Analysis (0)] |
| 16. | Zeng W, Yuan Y, Kong S, Qu J, Wang X, Zhou X, Yang F, Fan J. Modified diaphragmatic plication prevents and rectifies dyspnea with diaphragmatic eventration caused by phrenicotomy or injuries associated with extended mediastinal surgeries. Int J Surg. 2025;111:4993-5001. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 17. | Fogagnolo A, Grasso S, Dres M, Azzolina D, Dalla Corte F, Dolci G, Tamburini N, De Paoli G, Murgolo F, Pedarzani E, Andalò A, Volta CA, Savino S. Impact of early high flow nasal oxygen on diaphragmatic function and pulmonary complications after thoracic surgery: A randomized clinical trial. J Clin Anesth. 2025;106:111945. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 18. | Balvardi S, Pecorelli N, Castelino T, Niculiseanu P, Alhashemi M, Liberman AS, Charlebois P, Stein B, Carli F, Mayo NE, Feldman LS, Fiore JF Jr. Impact of Facilitation of Early Mobilization on Postoperative Pulmonary Outcomes After Colorectal Surgery: A Randomized Controlled Trial. Ann Surg. 2021;273:868-875. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 28] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 19. | Brat K, Sova M, Homolka P, Plutinsky M, Genzor S, Pokorna A, Dosbaba F, Imrichova B, Chovanec Z, Mitas L, Mikulaskova M, Svoboda M, Olson L, Cundrle I; study group. Multimodal prehabilitation before lung resection surgery: a multicentre randomised controlled trial. Br J Anaesth. 2025;135:188-196. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 10] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 20. | Ding Q, Ma F, Ma X, Zhu X. Breathing exercises for patients with early-stage lung cancer: a meta-analysis. Syst Rev. 2024;13:243. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 21. | Xu Q, Fang Y, Jing Q, Hu N, Lin K, Pan Y, Xu L, Gao H, Yuan M, Chu L, Ma Y, Xie Y, Chen J, Wang L. A portable triboelectric spirometer for wireless pulmonary function monitoring. Biosens Bioelectron. 2021;187:113329. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 95] [Cited by in RCA: 46] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 22. | Cui J, Gao M, Huang H, Huang X, Zeng Q. Dexmedetomidine Improves Lung Function by Promoting Inflammation Resolution in Patients Undergoing Totally Thoracoscopic Cardiac Surgery. Oxid Med Cell Longev. 2020;2020:8638301. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 23. | Turan A, Khanna AK, Brooker J, Saha AK, Clark CJ, Samant A, Ozcimen E, Pu X, Ruetzler K, Sessler DI. Association Between Mobilization and Composite Postoperative Complications Following Major Elective Surgery. JAMA Surg. 2023;158:825-830. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 32] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 24. | Ennis S, Lobley G, Worrall S, Evans B, Kimani PK, Khan A, Powell R, Banerjee P, Barker T, McGregor G. Effectiveness and Safety of Early Initiation of Poststernotomy Cardiac Rehabilitation Exercise Training: The SCAR Randomized Clinical Trial. JAMA Cardiol. 2022;7:817-824. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 19] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/