Published online Nov 27, 2025. doi: 10.4240/wjgs.v17.i11.111233
Revised: August 7, 2025
Accepted: October 9, 2025
Published online: November 27, 2025
Processing time: 151 Days and 3.1 Hours
Esophageal cancer is a malignancy that originates in the epithelium of the esophageal mucosa and has a high mortality rate. Although radiotherapy is the primary treatment modality, it can easily lead to nutritional deterioration and psychological distress, affecting treatment efficacy and quality of life. Currently, there are relatively few postoperative rehabilitation interventions for esophageal cancer. As such, it is particularly important to develop a systematic and comprehensive intervention model to improve the quality of life and nutritional status of patients.
To evaluate exercise, nutritional, and psychological interventions on the postoperative nutritional and mental status of patients with esophageal cancer.
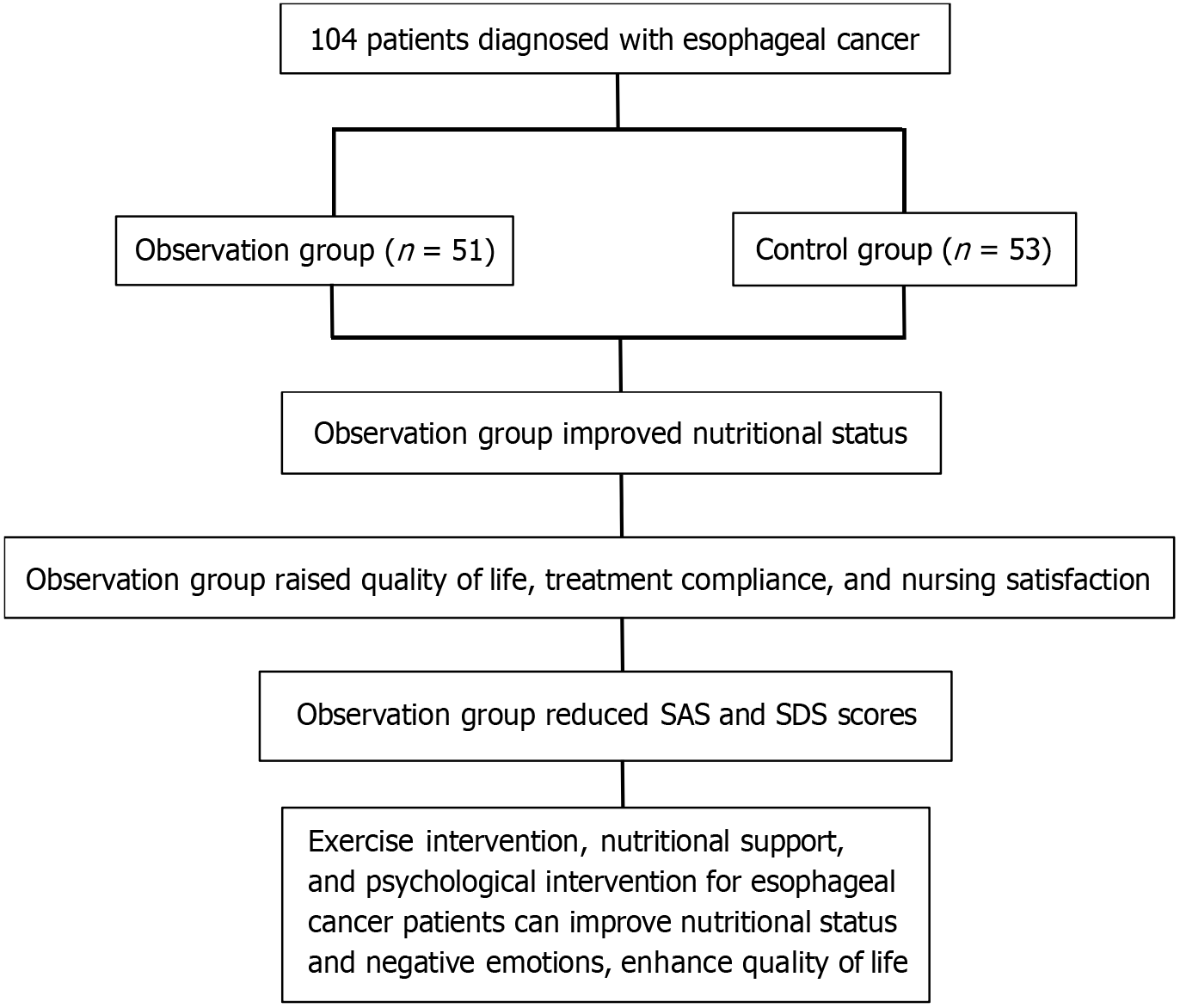
Data from 104 patients, who were diagnosed with postoperative esophageal cancer between August 2023 and February 2024, were retrospectively analyzed. Patients were divided into 2 groups using a random numbers table: control [routine nursing measures (n = 53)]; and observation [routine nursing + exercise, nutritional support, and psychological interventions (n = 51)]. Nutritional status, anxiety and depression, quality of life, incidence of complications, treatment compliance, and satisfaction with nursing care were compared between the two groups.
Serum albumin, prealbumin, hemoglobin, transferrin, and World Health Organization Quality of Life-Brief Version scores were higher in the observation group than those in the control group. After treatment, Self-rating Anxiety Scale, Self-rating Depression Scale, and Hamilton Anxiety and Depression Scale scores in the observation group were lower than those in the control group. No significant differences were observed in the incidence of complications between the observation and control groups. The observation group exhibited more satisfaction with nursing care and treatment compliance than the control group.
Exercise, nutritional support, and psychological interventions effectively improves the nutritional status and negative emotions of patients undergoing radiotherapy for esophageal cancer, and enhances treatment compliance and satisfaction with nursing.
Core Tip: This retrospective study evaluated the effect of postoperative multimodal interventions (exercise, nutritional, and psychological support) combined with routine nursing in patients who underwent radiotherapy for esophageal cancer between August 2023 and February 2024. Data from 104 patients were divided into two groups: Control (routine nursing); and observation (multimodal intervention). The intervention group exhibited significantly improved nutritional status (higher albumin, prealbumin, hemoglobin, and transferrin levels), reduced anxiety and depression (lower scores on validated assessment tools), enhanced quality of life, and greater satisfaction with nursing and treatment compliance compared with the control group. This multimodal approach ameliorated nutrition-related decline and psychological distress.
- Citation: Tang SH, Cao QQ, Xu XW, Feng MJ, Lu QJ, Sun J, Zhong K. Effect of exercise, nutritional, and psychological interventions on postoperative nutritional and mental status of patients with esophageal cancer. World J Gastrointest Surg 2025; 17(11): 111233
- URL: https://www.wjgnet.com/1948-9366/full/v17/i11/111233.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v17.i11.111233
Esophageal cancer is a malignancy originating from the esophageal squamous epithelium and columnar epithelium[1]. Its incidence and mortality rates rank sixth and fourth, respectively, among all malignant tumors[2,3]. The development of esophageal cancer is, in large part, related to factors including diet and lifestyle habits, infection(s), genetics, and long-term consumption of excessively hot foods[4]. It generally has non-specific symptoms in the early stages; however, as the disease progresses to the middle and late stages, it mainly manifests as difficulties with swallowing, reflux, and pain[5,6]. Long-term swallowing difficulties can affect digestion and the absorption of food, leading to malnutrition, significant weight loss, and severe emaciation[7,8]. Radiotherapy is an important method of treating esophageal cancer in clinical practice[9,10]. However, due to the need for long-term radiotherapy and chemotherapy treatment, patients with eso
Data from 104 patients, who were diagnosed with esophageal cancer between July 2023 and January 2024, were included. Patients were divided into 2 groups using a random numbers table: Control [routine nursing measures (n = 53)]; and observation (routine nursing measures + exercise, nutritional support, and psychological interventions (n = 51)]. There were no statistically significant differences (P > 0.05) between the two groups in terms of sex, age, pathological type, tumor location, tumor-node-metastasis stage, and body mass index before treatment (Table 1). There was no significant difference in comorbidities or nutritional and psychological status between the two groups before treatment. The present study was approved by the Ethics Committee of Changhai Hospital (Shanghai, China). Before starting the trial, all the patients provided written informed consent. A flow-diagram illustrating patient flow through the study is presented in Figure 1.
| Characteristics | Observation group (n = 51) | Control group (n = 53) | t/χ2 | P value |
| Sex | ||||
| Male (%) | 55 (28/51) | 58 (31/53) | 0.1362 | 0.712 |
| Female (%) | 45 (23/51) | 42 (22/53) | - | - |
| Age (year), mean ± SD | 53.69 ± 8.13 | 54.16 ± 7.97 | 0.2651 | 0.792 |
| Pathological type | ||||
| Squamous cell carcinoma (%) | 39 (20/51) | 40 (21/53) | 0.0022 | 0.966 |
| Adenocarcinoma (%) | 31 (16/51) | 34 (18/53) | ||
| Adenosquamous carcinoma (%) | 30 (15/51) | 26 (12/53) | ||
| TNM staging | ||||
| I (%) | 47 (24/51) | 43 (22/51) | 0.3252 | 0.569 |
| II (%) | 53 (27/51) | 57 (31/51) | - | - |
| BMI (kg /m2), mean ± SD | 21.33 ± 2.16 | 21.36 ± 2.18 | 0.0691 | 0.945 |
Inclusion criteria: Fulfill the diagnostic criteria in the Guidelines for Standardized Diagnosis and Treatment of Esophageal Cancer[17]; clinically treated with surgery; successfully completed surgery and received radiotherapy; and provided informed written consent to participate.
Exclusion criteria: Severe liver and kidney dysfunction; merge patients with other tumors; combined mental illnesses; combined nutritional and metabolic diseases; and poor compliance.
Patients diagnosed with esophageal cancer were divided into treatment and control groups using a random numbers table. The control group received only routine nursing measures, including familiarizing themselves with the hospital environment upon admission, accompanying patients to familiarize themselves with the ward environment, and introducing the attending physician and nurses. Before treatment, patients and their families were informed about radiation therapy, possible adverse reactions, complications during treatment, and precautions that need to be taken to cooperate. Food should be mild in temperature; cold liquids should be avoided, and spicy and irritating foods should be avoided. Nurses explained the method of medication administration, precautions, and common toxic side effects. Patients were advised to choose appropriate exercises based on their physical condition. The interventions were performed over a period of 28 days. The observation group received an exercise intervention, nutritional support, and psychological intervention based on the control group.
Exercise intervention: Based on patient age, sex, physical condition, and other factors, develop a personalized and standardized exercise plan for the patient and guide them to engage in aerobic exercises such as Tai Chi, yoga, and brisk walking. Each exercise included a warm-up (5 minutes), aerobic exercises (≥ 15 minutes), and relaxation exercise (5 minutes). Exercise for 20-30 minutes each time, 3-4 times per week, controls the exercise intensity within 50%-70% of the maximum heart rate; target heart rate = (220 - age) × 50%-70%. The exercise intensity was 50%-55% of the target heart rate in the first week, 55%-60% of the target heart rate in the second and third weeks, and 60%-70% of the target heart rate in the fourth week. Exercise is generally performed in the morning or afternoon, and should not be performed after a full meal or when hungry. The duration of exercise and amount were controlled, and excessive fatigue was avoided.
Nutritional support: With the help of clinical nutritionists, personalized recipes were developed for patients based on their nutritional and energy needs, personal taste preferences, and market availability. The specific steps were as follows: Calculate based on standard weight (weight = height - 105); determine the daily exchange amount based on reference energy requirements and dietary nutrient intake per kg; and determine the proportion of fat, protein, and carbohydrates in the food based on the patient’s demand for the three major production nutrients. Food selection order: Staple food first, vegetables later, meat dishes later, and finally, calculate cooking oil; develop specific recipes based on the calculated quantity and variety of food. Oral nutritional supplements are administered according to the patients’ food intake and dietary structure. Intravenous nutrition was provided to those who could not take them orally. The target nutritional intake is (20-35) kcal/kg/day, fat (1.0-1.39 g/kg/day), protein (1.2-2.0 g/kg/day), and carbohydrates (3-5 g/kg/day). In addition to a regular diet, appropriate medicinal dishes such as Huangqi Yam Soup for replenishing qi and blood, and Bird’s Nest Snow Ear Soup for clearing the lungs and nourishing the stomach are provided to supplement nutrition.
Psychological interventions: (1) Assessment of psychological status: Communicate with patients through psychotherapists to understand their negative emotions and analyze their causes and, based on this, develop a psychological support intervention plan; (2) Talk cures: Encourage patients to vent their negative thoughts. Communicate with psychotherapists through language to express thoughts. The therapist listens attentively and provides positive feedback, taking effective measures to alleviate the patient’s negative thoughts; (3) Health education: Devote attention to health education, clearly educate the patients in the basic knowledge of esophageal cancer, and inform them of the precautions during radiotherapy and possible adverse reactions during and after radiotherapy to eliminate patient concerns and pessimistic psychology as early as possible, thereby improving their compliance in the treatment process. During the entire treatment process, attention is devoted to changes in patient emotions and strengthening communication with them; (4) Relaxation training: Psychotherapists use language guidance and music therapy to help patients relax for 30 minutes per session, 1-2 times per day; and (5) Family and social support: Guide the patient’s family members to participate in psychological intervention, deal with the patient’s psychological problems from multiple aspects, and alleviate the patient’s negative emotions. Joint intervention by nursing staff and family members should be used to enhance patients’ psychological support and make nursing measures more humane. Encourage patients who have recovered well to communicate with friends, share treatment experiences, and enhance their confidence. The interventions were performed over a period of 28 days.
Nutritional indicators: Using an automated biochemical analyzer (Hitachi Corporation, Japan), serum albumin (ALB), prealbumin (PA), hemoglobin (Hb), and transferrin (TRF) concentrations were measured in the morning fasting venous blood of the two groups of patients.
Self-rating Anxiety Scale and Self-rating Depression Scale scores: These scales both consist of 20 items, each rated on a scale of 1-4 based on feelings over the past week. The total score ranges from 0 to 80, with higher scores indicating more severe anxiety and depression.
Hamilton Anxiety Scale and Hamilton Depression Scale scores: The Hamilton Anxiety Scale (HAM-A) comprises 14 diagnostic criteria for anxiety disorders. Participants rated each item they had experienced in the past on a scale of 0-4. The total HAM-A score ranges from 0 point to 56 points; the higher the HAM-A score, the more severe the anxiety symptoms. The Hamilton Depression Scale (HAM-D) comprises 17 diagnostic criteria for anxiety disorders. Participants rated each item they had experienced in the past on a scale of 0-4. The total HAM-D score ranges from 0 point to 68 points; the higher the HAM-D score, the more severe the depressive symptoms.
Quality of life: The World Health Organization Quality of Life Assessment Short Form (WHOQOL-BREF) was used to evaluate patient quality of life. This short form includes 6 items: Physical, independent, mental, social, environmental, and spiritual. Each item is scored on a scale of 0 to 20, with higher scores indicating better quality of life.
Incidence of esophageal cancer complications in the two groups: The incidence of complications were recorded for each group.
Treatment compliance: Compliance was defined as follows: Full compliance (≥ 80% completion of various intervention measures); partial compliance (60% to 79% completion of various intervention measures); non-compliance (< 60%). Total compliance rate = (full compliance + partial compliance)/total number of cases × 100.
Satisfaction with nursing: This metric was compared between the two groups.
Statistical analysis was performed using SPSS version 25.0 (IBM Corporation, Armonk, NY, United States). Experimental data are expressed as mean ± SD. Data that satisfied normal distribution and homogeneity of variances were compared using the independent samples t-test. Count data are expressed as number and percentage (%), and were compared using the χ2 test. Differences with P < 0.05 were considered to be statistically significant.
There were no statistical differences between the two groups in nutritional indices after admission (P > 0.05). After treatment, however, ALB, PA, Hb, and TRF levels were higher in the observation group than those in the control group (P < 0.05) (Table 2).
| Group | ALB (g /L)) | PA (mg /L) | Hb (g /L) | TRF (g /L) | ||||
| Before treatment | After treatment | Before treatment | After treatment | Before treatment | After treatment | Before treatment | After treatment | |
| Observation group (n = 51) | 32.67 ± 2.41 | 41.26 ± 1.54a | 182.23 ± 3.24 | 242.15 ± 3.04a | 120.26 ± 3.48 | 172.65 ± 4.13a | 1.60 ± 0.16 | 2.74 ± 0.45a |
| Control group (n = 53) | 32.16 ± 2.52 | 38.14 ± 1.67a | 183.31 ± 3.17 | 203.63 ± 3.98a | 120.17 ± 3.75 | 142.25 ± 4.66a | 1.59 ± 0.22 | 2.02 ± 0.37a |
| t | 1.065 | 10.00 | 1.734 | 56.00 | 0.128 | 35.54 | 0.248 | 8.991 |
| P value | 0.289 | < 0.0001 | 0.086 | < 0.0001 | 0.899 | < 0.0001 | 0.805 | < 0.0001 |
The Self-rating Anxiety Scale (SAS) and Self-rating Depression Scale (SDS) scores after admission did not differ significantly between the 2 groups (P > 0.05). However, 28 days later, these scores were lower in the observation group than those in the control group, with a prominent statistical difference (P < 0.05) (Table 3).
Before treatment, there was no significant difference in HAM-A and HAM-D scores between the observation and control groups (P > 0.05). After treatment, however, these scores decreased in both groups, and were significantly lower in the observation group (P < 0.05) (Table 4).
Before treatment, the WHOQOL-BREF scores of the two groups exhibited no statistically significant differences (P > 0.05). After treatment, however, these scores increased in both groups, and were significantly higher in the observation group (P < 0.05) (Table 5).
| Group | Physiological function | Psychological function | Social relationships | |||
| Before treatment | After treatment | Before treatment | After treatment | Before treatment | After treatment | |
| Observation group (n = 51) | 7.45 ± 2.34 | 16.25 ± 2.69a | 8.15 ± 2.14 | 18.63 ± 2.69a | 9.93 ± 3.61 | 17.29 ± 2.96a |
| Control group (n = 53) | 7.41 ± 2.47 | 11.23 ± 2.37a | 8.18 ± 2.03 | 12.15 ± 2.38a | 9.95 ± 3.75 | 13.85 ± 3.05a |
| t | 0.086 | 10.20 | 0.074 | 13.13 | 0.029 | 5.893 |
| P value | 0.931 | < 0.0001 | 0.941 | < 0.0001 | 0.977 | < 0.0001 |
| Group | Environment | Independent | Spiritual world | |||
| Before treatment | After treatment | Before treatment | After treatment | Before treatment | After treatment | |
| Observation group (n = 51) | 8.40 ± 2.34 | 16.73 ± 2.78a | 9.15 ± 2.45 | 19.45 ± 2.36a | 10.25 ± 3.64 | 16.67 ± 2.84a |
| Control group (n = 53) | 8.39 ± 2.40 | 13.03 ± 2.96a | 9.20 ± 2.33 | 14.16 ± 2.74a | 10.26 ± 3.15 | 12.85 ± 2.27a |
| t | 0.022 | 6.633 | 0.108 | 10.65 | 0.015 | 7.648 |
| P value | 0.983 | < 0.0001 | 0.915 | < 0.0001 | 0.988 | < 0.0001 |
After treatment, the incidence of complications did not differ significantly between the observation (54.9%) and control (66%) groups (Table 6).
| Group | Case | Number of vomiting (%) | Number of diarrhea (%) | Number of allergies (%) | Number of bone marrow suppression (%) |
| Observation group | 51 | 6 (11.76) | 1 (1.96) | 10 (19.61) | 11 (21.57) |
| Control group | 53 | 8 (15.09) | 2 (3.77) | 12 (22.64) | 13 (24.53) |
| χ2 | - | - | - | - | 1.350 |
| P value | - | - | - | - | 0.245 |
After treatment, the total compliance rate in the observation group (92.16%) was higher than that in the control group (71.70%) (P < 0.05) (Table 7).
| Group | Case | Fully compliance (%) | Partial compliance (%) | Non-compliance (%) | Total compliance rate (%) |
| Observation group | 51 | 35 (68.63) | 12 (23.53) | 4 (7.84) | 47 (92.16) |
| Control group | 53 | 24 (45.28) | 14 (26.42) | 15 (28.30) | 38 (71.70) |
| χ2 | - | - | - | - | 7.286 |
| P value | - | - | - | - | 0.007 |
Throughout treatment, satisfaction with nursing was higher among the observation group (94.12%) than that in the control group (75.47%) (P < 0.05) (Table 8).
| Group | Case | Very satisfied (%) | Basically satisfied (%) | Unsatisfied (%) |
| Observation group | 51 | 30 (58.82) | 18 (35.29) | 3 (5.88) |
| Control group | 53 | 26 (49.06) | 14 (26.42) | 13 (24.53) |
| χ2 | - | - | - | 6.941 |
| P value | - | - | - | 0.008 |
Esophageal cancer has the characteristics of insidious onset and rapid disease course, which is not easy to be found in the early stage[18]. Presently, esophageal cancer has become one of the high incidence malignant tumor diseases, and the high mortality rate[19]. Currently, the main clinical treatment of esophageal cancer is surgical treatment and radiotherapy, which can effectively prolong the life of patients and have a definite clinical effect[20]. However, such treatment methods are often accompanied by obvious adverse reactions, affecting the health of patients[21,22]. Clinical studies have found that patients with malignant tumors, such as esophageal cancer, often experience severe malnutrition, the manifestations of which are closely related to disease stage and treatment plan[23].
Eighty percent of patients experience weight loss, malnutrition, and negative psychological emotions after radiation therapy, which further increases the risk for postoperative infection. The incidence of complications has a negative impact on the quality of life, making radiotherapy difficult to complete[24]. Research has shown that approximately 20% of patients with cancer die from malnutrition and related complications, rather than the malignant tumor itself[25]. Related studies have shown that providing specific nutritional support and psychological intervention is beneficial for improving patients’ nutritional and psychological status, accelerating their recovery, and active cooperation with treatment[26]. As a result, selecting appropriate nursing interventions to effectively improve patient mental health and nutritional status is of great significance for improving clinical treatment outcomes.
Serum levels of ALB, PA, Hb, and TRF are important objective indicators of nutritional status in clinical practice[27]. Our results revealed that after intervention, the serum levels of ALB, PA, Hb, and TRF in the observation group were significantly higher than those in the control group, suggesting that exercise, nutritional support, and psychological interventions have a more significant effect on improving the nutritional status of patients with esophageal cancer undergoing radiotherapy. The SAS, SDS, HAM-A, and HAM-D are simple, effective, and highly recognized assessment tools in clinical practice. It consists of 20 items and can effectively evaluate the degree of anxiety and depression in patients and their changes during the treatment process[28]. The WHOQOL-BREF it is used to evaluate individuals’ health-related factors. It has the advantages of high reliability, validity, and responsiveness and is a widely used and recognized psychological measurement tool in clinical practice[29]. Our results indicated that after the intervention, the SAS, SDS, HAM-A, and HAM-D scores of the observation group were significantly lower than those of the control group, and the WHOQOL-BREF scores were markedly higher than those of the control group. This was mainly attributed to the fact that exercise, nutritional support, and psychological interventions are new nursing intervention models. Corresponding psychological nursing work was conducted in 3 parts to enhance patients’ understanding of radiotherapy treatment, strengthen their confidence, and avoid anxiety and fear caused by erroneous cognition. Additionally, the effective implementation of exercise intervention, nutritional support, and psychological intervention enables patients to face the clinical treatment of esophageal cancer with a more positive attitude, strengthens the overall treatment effect, and provides them with a better quality of life. Moreover, exercise, nutritional support, and psychological interventions can promote the overall improvement of clinical treatment outcomes for patients, improve their actual experience during the treatment process, and enhance treatment compliance and nursing satisfaction.
Nevertheless, the sample size included in this study was limited, and the research on the treatment mechanisms was not in-depth. In the future, a larger sample size is needed to explore the effects of exercise, nutritional support, and psychological interventions on cancer-related fatigue in patients with esophageal cancer.
In summary, exercise, nutritional support, and psychological interventions for patients with esophageal cancer can effectively improve nutritional status and negative emotions, such as anxiety and depression; enhance quality of life, treatment compliance, and nursing satisfaction; and have certain clinical promotion value.
| 1. | Huang FL, Yu SJ. Esophageal cancer: Risk factors, genetic association, and treatment. Asian J Surg. 2018;41:210-215. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 286] [Cited by in RCA: 580] [Article Influence: 58.0] [Reference Citation Analysis (0)] |
| 2. | Mwachiro M, White R. Management of Esophageal Cancer Treatment in Resource-Limited Settings. Thorac Surg Clin. 2022;32:397-404. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 3. | Iyer R, Wilkinson N, Demmy T, Javle M. Controversies in the multimodality management of locally advanced esophageal cancer: evidence-based review of surgery alone and combined-modality therapy. Ann Surg Oncol. 2004;11:665-673. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 44] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 4. | Bhatt A, Kamath S, Murthy SC, Raja S. Multidisciplinary Evaluation and Management of Early Stage Esophageal Cancer. Surg Oncol Clin N Am. 2020;29:613-630. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 5. | Borggreve AS, Kingma BF, Domrachev SA, Koshkin MA, Ruurda JP, van Hillegersberg R, Takeda FR, Goense L. Surgical treatment of esophageal cancer in the era of multimodality management. Ann N Y Acad Sci. 2018;1434:192-209. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 113] [Article Influence: 14.1] [Reference Citation Analysis (0)] |
| 6. | Zhou N, Hofstetter WL. Prognostic and therapeutic molecular markers in the clinical management of esophageal cancer. Expert Rev Mol Diagn. 2020;20:401-411. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 16] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 7. | Won E, Ilson DH. Management of localized esophageal cancer in the older patient. Oncologist. 2014;19:367-374. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 39] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 8. | Gao P, Tsai C, Yang Y, Xu Y, Zhang C, Zhang C, Wang L, Liu H, Wang Z. Intraoperative radiotherapy in gastric and esophageal cancer: meta-analysis of long-term outcomes and complications. Minerva Med. 2017;108:74-83. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 15] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 9. | Fujita H. Ways and tradition of Japan in esophageal surgery for cancer. Gen Thorac Cardiovasc Surg. 2020;68:1187-1192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 10. | Sardaro A, Ferrari C, Carbonara R, Altini C, Lavelli V, Rubini G. Synergism Between Immunotherapy and Radiotherapy in Esophageal Cancer: An Overview of Current Knowledge and Future Perspectives. Cancer Biother Radiopharm. 2021;36:123-132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 11. | Xi M, Lin SH. Recent advances in intensity modulated radiotherapy and proton therapy for esophageal cancer. Expert Rev Anticancer Ther. 2017;17:635-646. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 28] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 12. | Zhang M, Wu AJ. Radiation techniques for esophageal cancer. Chin Clin Oncol. 2017;6:45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 13. | Wu AJ, Bosch WR, Chang DT, Hong TS, Jabbour SK, Kleinberg LR, Mamon HJ, Thomas CR Jr, Goodman KA. Expert Consensus Contouring Guidelines for Intensity Modulated Radiation Therapy in Esophageal and Gastroesophageal Junction Cancer. Int J Radiat Oncol Biol Phys. 2015;92:911-920. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 108] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 14. | Li J, Jia Y, Cheng Y, Wang J. Chemoradiotherapy vs radiotherapy for nonoperative early stage esophageal cancer: A seer data analysis. Cancer Med. 2020;9:5025-5034. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 15. | Miyamoto T, Yamamoto N, Nishimura H, Koto M, Tsujii H, Mizoe JE, Kamada T, Kato H, Yamada S, Morita S, Yoshikawa K, Kandatsu S, Fujisawa T. Carbon ion radiotherapy for stage I non-small cell lung cancer. Radiother Oncol. 2003;66:127-140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 174] [Cited by in RCA: 152] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 16. | Ono T. Review of clinical results of charged-particle therapy for esophageal cancer. Esophagus. 2021;18:33-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 17. | Uhlenhopp DJ, Then EO, Sunkara T, Gaduputi V. Epidemiology of esophageal cancer: update in global trends, etiology and risk factors. Clin J Gastroenterol. 2020;13:1010-1021. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 502] [Article Influence: 83.7] [Reference Citation Analysis (1)] |
| 18. | Xu HT, Miao J, Liu JW, Zhang LG, Zhang QG. Prognostic value of circulating tumor cells in esophageal cancer. World J Gastroenterol. 2017;23:1310-1318. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 13] [Cited by in RCA: 15] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 19. | Bo Y, Lu Y, Zhao Y, Zhao E, Yuan L, Lu W, Cui L, Lu Q. Association between dietary vitamin C intake and risk of esophageal cancer: A dose-response meta-analysis. Int J Cancer. 2016;138:1843-1850. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 33] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 20. | Li K, Zhang B. The association of dietary β-carotene and vitamin A intake on the risk of esophageal cancer: a meta-analysis. Rev Esp Enferm Dig. 2020;112:620-626. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 14] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 21. | Gomez HL, Doval DC, Chavez MA, Ang PC, Aziz Z, Nag S, Ng C, Franco SX, Chow LW, Arbushites MC, Casey MA, Berger MS, Stein SH, Sledge GW. Efficacy and safety of lapatinib as first-line therapy for ErbB2-amplified locally advanced or metastatic breast cancer. J Clin Oncol. 2008;26:2999-3005. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 264] [Cited by in RCA: 253] [Article Influence: 14.1] [Reference Citation Analysis (0)] |
| 22. | Fan S, Wang T, Zhang QY, Wang J, Su J, Liu Z. Safety and clinical activity of cadonilimab, an anti PD-1/CTLA-4 bispecific antibody, for patients with persistent, recurrent, or metastatic cervical cancer (R/M CC): A retrospective, real-world study. J Clin Oncol. 2024;42:e17522-e17522. [DOI] [Full Text] |
| 23. | Fan J, Liu Z, Mao X, Tong X, Zhang T, Suo C, Chen X. Global trends in the incidence and mortality of esophageal cancer from 1990 to 2017. Cancer Med. 2020;9:6875-6887. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 93] [Article Influence: 15.5] [Reference Citation Analysis (0)] |
| 24. | Thoresen L, Fjeldstad I, Krogstad K, Kaasa S, Falkmer UG. Nutritional status of patients with advanced cancer: the value of using the subjective global assessment of nutritional status as a screening tool. Palliat Med. 2002;16:33-42. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 91] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 25. | Pinto E, Cavallin F, Scarpa M. Psychological support of esophageal cancer patient? J Thorac Dis. 2019;11:S654-S662. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 25] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 26. | Reintam Blaser A, Starkopf J, Alhazzani W, Berger MM, Casaer MP, Deane AM, Fruhwald S, Hiesmayr M, Ichai C, Jakob SM, Loudet CI, Malbrain ML, Montejo González JC, Paugam-Burtz C, Poeze M, Preiser JC, Singer P, van Zanten AR, De Waele J, Wendon J, Wernerman J, Whitehouse T, Wilmer A, Oudemans-van Straaten HM; ESICM Working Group on Gastrointestinal Function. Early enteral nutrition in critically ill patients: ESICM clinical practice guidelines. Intensive Care Med. 2017;43:380-398. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 346] [Cited by in RCA: 502] [Article Influence: 55.8] [Reference Citation Analysis (0)] |
| 27. | Jiang Z, Luo J, Xu M, Cong Z, Ji S, Diao Y, Xu Y, Shen Y. Safety analysis of early oral feeding after esophagectomy in patients complicated with diabetes. J Cardiothorac Surg. 2021;16:56. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 28. | Chen M, Huang J, Zhu Z, Zhang J, Li K. Systematic review and meta-analysis of tumor biomarkers in predicting prognosis in esophageal cancer. BMC Cancer. 2013;13:539. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 76] [Cited by in RCA: 80] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 29. | Chang CY, Lee LJ, Wang JD, Lee CT, Tai CM, Tang TQ, Lin JT. Health-related quality of life in patients with Barrett's esophagus. Health Qual Life Outcomes. 2016;14:158. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 12] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/