Published online Oct 27, 2025. doi: 10.4240/wjgs.v17.i10.106389
Revised: July 1, 2025
Accepted: August 25, 2025
Published online: October 27, 2025
Processing time: 153 Days and 23.1 Hours
Postoperative complications (POCs) can arise in patients who underwent surgery for gastric cancer (GC). Effective nursing may help in minimizing these negative outcomes.
To elucidate the influence of fast-track rehabilitation (FTR) plus humanized nursing on gastrointestinal (GI) function and quality of life (QOL) of patients who underwent GC surgery.
The study participants were 102 patients admitted between December 2018 and December 2020 for GC surgery, of which 52 and 50 patients who received FTR + humanized nursing (research group) and routine nursing (control group), respec
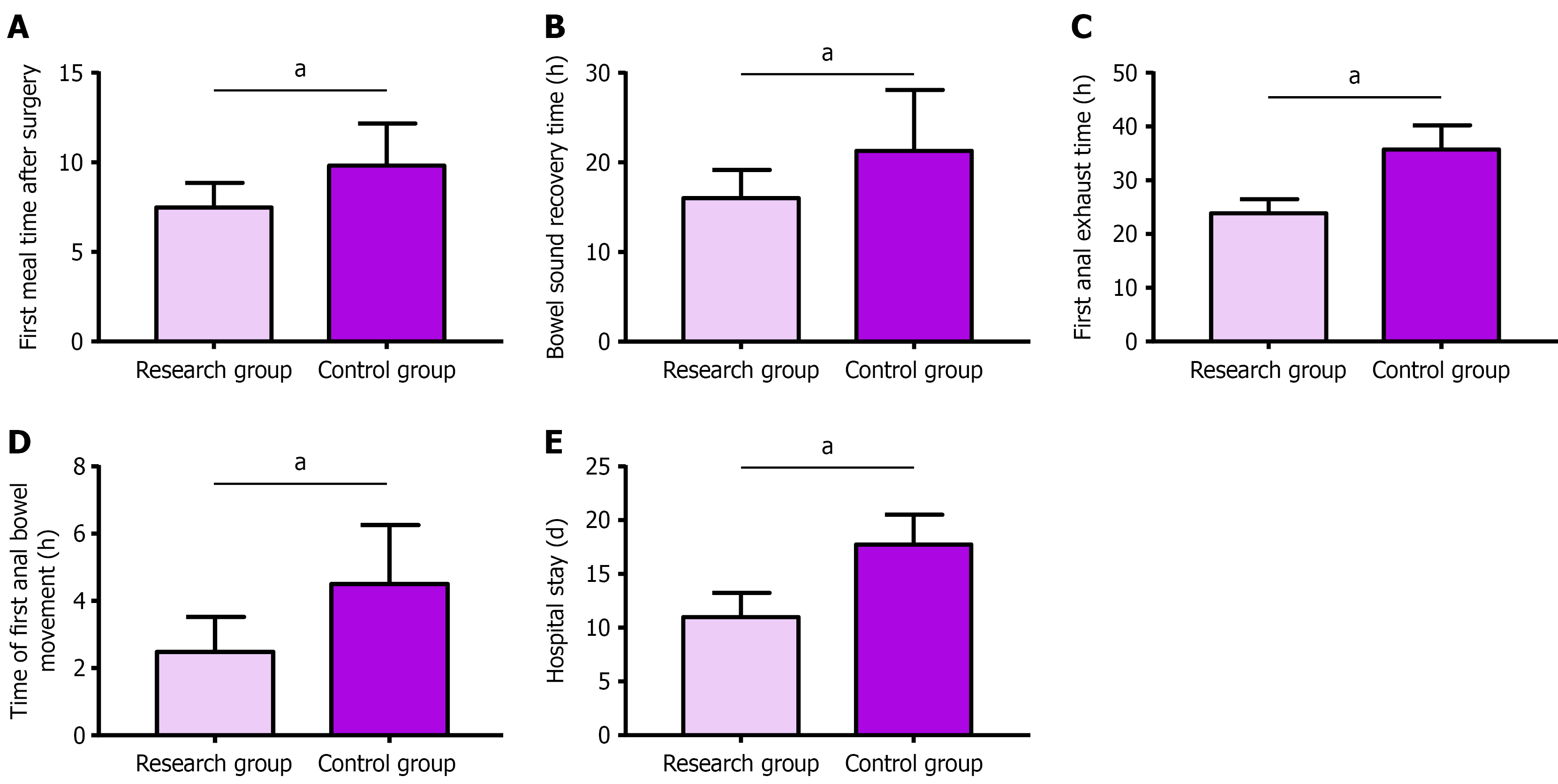
Compared with the control group, the research group had better GI function, which was mainly manifested by earlier food intake, shorter bowel sound reco
FTR + humanized nursing not only improve the GI function and QOL of patients undergoing GC surgery but also reduce the incidence of POCs and improve nursing satisfaction. Thus, this intervention deserves popularization in clinical practice.
Core Tip: Few studies have examined how fast-track rehabilitation (FTR) accompanied by humanized nursing affects gastrointestinal recovery and quality of life of patients who underwent gastric cancer (GC) surgery. This clinical study of 102 patients who underwent GC surgery compared outcomes between patients receiving FTR with humanized nursing and those receiving standard care. Through a series of analyses, this study revealed the greater clinical benefits of FTR plus humanized care, which is an effective alternative for optimizing postoperative care in patients who underwent GC surgery.
- Citation: Li H, Gao HJ, Wan MD, Wang WZ, Wu X. Fast-track rehabilitation plus humanized nursing improves gastrointestinal function and quality of life in post-surgical gastric cancer patients. World J Gastrointest Surg 2025; 17(10): 106389
- URL: https://www.wjgnet.com/1948-9366/full/v17/i10/106389.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v17.i10.106389
Gastric cancer (GC) is the fifth most common malignancy that accounts for 6% of all cancers worldwide[1]. It has a complicated pathogenesis and is related to various comprehensive factors such as genetic susceptibility, environmental factors, and dietary habits[2]. More than 1 million new GC cases and 783000 deaths have been reported[3], and surgical resection is still the preferred treatment for GC[4]. Despite continuous optimization in imaging, surgical equipment, and perioperative management in recent years, the postoperative morbidity rate is still at 20%-30%[5]. Moreover, the potential postoperative complications (POCs) negatively affect the quality of life (QOL) of patients, prolong the length of hospital stay (LOS), and increase hospitalization costs[6,7]. Therefore, this study attempts to provide effective clinical nursing interventions for patients undergoing GC surgery to contribute to postoperative rehabilitation, reduction of compli
Studies have pointed out that high-quality nursing is of great help in the rehabilitation of patients who underwent GC surgery[8]. Fast-track rehabilitation (FTR) is a comprehensive nursing intervention model based on the multidisciplinary cooperation of various fields, such as nursing, anesthesia, surgery, and nutrition, which can improve patients’ surgical experience and mitigate POC risk according to objective methods that have been repeatedly verified during the perio
This retrospective study enrolled 102 patients who underwent GC surgery between December 2018 and December 2020. Of these, 52 patients received FTR + humanized nursing (research group), whereas 50 received routine care (control group). General data, such as age and sex, were similar in the two cohorts (P > 0.05), suggesting the feasibility of follow-up research (Table 1).
| Factors | n | Research group (n = 52) | Control group (n = 50) | χ2/t | P value |
| Age (years old), mean ± SD | 102 | 53.90 ± 7.15 | 53.24 ± 7.59 | 0.452 | 0.652 |
| Sex | 0.394 | 0.530 | |||
| Male | 58 | 28 (53.85) | 30 (60.00) | ||
| Female | 44 | 24 (46.15) | 20 (40.00) | ||
| Pathological stage | 0.146 | 0.703 | |||
| I-II | 55 | 29 (55.77) | 26 (52.00) | ||
| III | 47 | 23 (44.23) | 24 (48.00) | ||
| Tumor site | 0.197 | 0.906 | |||
| Gastric antrum | 51 | 26 (50.00) | 25 (50.00) | ||
| Gastric body | 29 | 14 (26.92) | 15 (30.00) | ||
| Stomach fundus | 22 | 12 (23.08) | 10 (20.00) | ||
| Surgical methods | 3.000 | 0.223 | |||
| Total gastrectomy | 16 | 5 (9.62) | 11 (22.00) | ||
| Proximal gastrectomy | 23 | 13 (25.00) | 10 (20.00) | ||
| Distal gastrectomy | 63 | 34 (65.38) | 29 (58.00) | ||
| Educational background | 0.594 | 0.441 | |||
| Below high school | 43 | 20 (38.46) | 23 (46.00) | ||
| High school and above | 59 | 32 (61.54) | 27 (54.00) | ||
| Family history of gastric cancer | 0.118 | 0.732 | |||
| Without | 77 | 40 (76.92) | 37 (74.00) | ||
| With | 25 | 12 (23.08) | 13 (26.00) |
The eligible patients were patients who were diagnosed with GC confirmed by clinicopathological examination and gastroscopy and who had no operative contraindications, psychological illness, or mental disorders. Conversely, patients who had severe heart, lung, and kidney dysfunction, malignant tumors, gastrostomy or jejunostomy, coagulation abnormalities and autoimmune deficiency, and incomplete medical records were excluded.
The control group received routine care, which included preoperative health education, routine fasting and water prohibition, bowel preparation, catheter placement, and postoperative diet guidance. The research group adopted FTR + humanized nursing, with the following main measures: (1) Preoperative nursing measures: The nutritional status of the patients was assessed, and corresponding preoperative dietary guidance was given, such as giving priority to digestible and high-quality protein foods 3 days before surgery, quitting smoking, and drinking. Nurses always consider a kind attitude and soft language when communicating with patients and their families. In addition, to help them establish correct treatment attitude and motivate their active cooperation with the treatment while improving their self-care ability, health education was conducted to inform patients about the operation, preoperative precautions, postoperative potential complications, and corresponding treatment measures. Furthermore, the patient’s disease- or treatment-related negative emotions were eased, and psychological counseling was provided. Patients were also urged and instructed to fast 6 hours preoperatively and take 200 mL of 5% glucose orally 2 hours preoperatively. Moreover, before the surgery, the nursing staff adjusted the moderate temperature of the operating room to make the environment comfortable, clean, and quiet; (2) Intraoperative nursing measures: Nurses kept patients warm during the operation, and intravenous fluids were warmed in advance for use. When small tumors (T1-T2) were confined to the primary site without serosal invasion or nodal spread (N0; confirmed intraoperatively), the omission of a surgical drain was considered, provided the anastomosis demonstrated robust perfusion and tension-free suturing. This strategy aimed to minimize complications and hasten rehabilitation, with absorbable sutures utilized for closure. In all other scenarios, routine drain placement adjacent to the anastomosis remained standard to assess postoperative hemorrhage, leakage, or intra-abdominal infections. Intraoperatively, nurses paid close attention to the patient’s vital signs and promptly informed the doctors of any unexpected situation to avoid accidents; and (3) Postoperative nursing measures: Postoperatively, patients were given analgesic drugs continuously, with the dosage adjusted appropriately according to the doctor’s advice and pain severity. The infusion volume was strictly controlled. When the infusion was stopped, the indwelling catheter was withdrawn 24 hours postoperatively. Besides, the patient was given 500 mL of warm saline orally 6 hours after awakening from anesthesia, and to provide gradual, small, and frequent meals, a liquid diet was started. On the day after surgery, patients were encouraged to move their limbs properly in bed and turn over regularly. On day 3, they can get out of bed and ambulate, avoiding strenuous exercise. The nursing staff paid a return visit on postoperative day 3 asked the patient for the presence of pain, checked the incision, and informed the patient of the postoperative recovery to build the patient’s confidence in recovery.
In the research group, nursing staff received standardized training in FTR and humanized care communication strategies, and all participants demonstrated competency through formal evaluation[15,16]. No such training was implemented for control group staff. Qualification criteria mandated: (1) Finishing an undergraduate degree or higher; (2) Having ≥ 5 years of general surgical experience; and (3) Participating in ≥ 3 GC surgery cases requiring perioperative care.
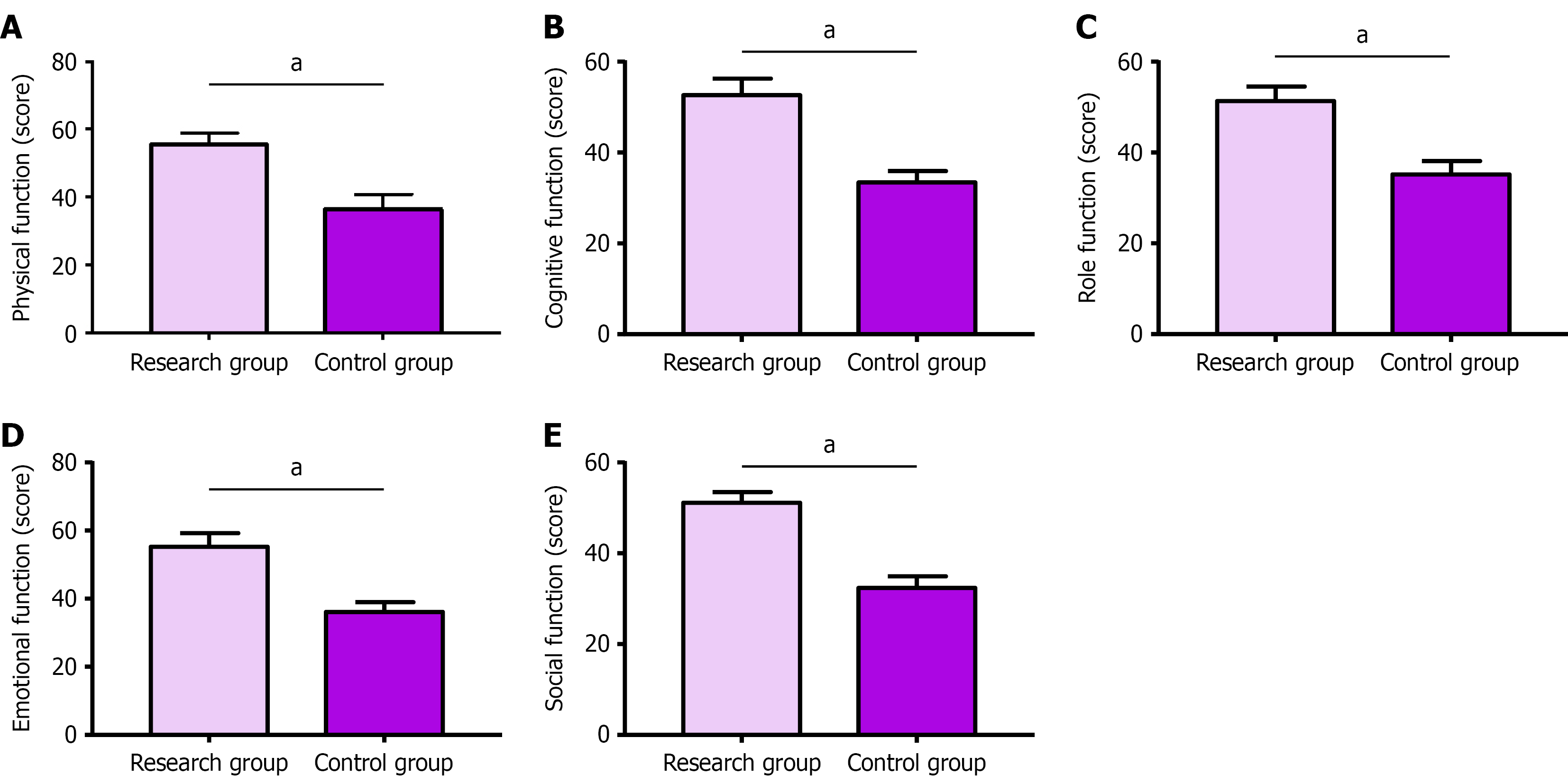
The GI function, QOL, POCs, and nursing satisfaction of the two groups were observed and recorded. GI function recovery was compared between the groups by recording the patients’ first postoperative oral food intake, bowel sound recovery time, first anal exhaust and defecation time, and LOS. After 3 months of nursing care, patients’ QOL was evaluated according to the European Organization for Research and Treatment of Cancer Core QOL questionnaire (QLQ-C30). This scale mainly includes physical, cognitive, role, emotional, and social functioning. Higher scores (range, 0-60 points) represent better QOL. POCs mainly observed and recorded included abdominal distension, infection, GI bleeding, anastomotic leakage (AL), and deep vein thrombosis (DVT), and the overall incidence was calculated. Finally, patients were asked to fill in the self-made questionnaire of nursing satisfaction to understand their level of satisfaction.
This study used IBM SPSS Statistics version 21.0 (IBM Corp., Armonk, NY, United States). The n (%) and mean ± SD were used to represent counting and measurement data, respectively. Among them, χ2 test was used for comparisons of counting data, whereas the independent-samples t-test was employed for between-group comparisons of measurement data. P < 0.05 is regarded as significant.
The general data of both groups were comparable (Table 1): No significant between-group difference was noted in age, sex, pathological stage, tumor location, surgical method, educational background, family history of GC, and other information (P > 0.05).
GI function recovery indexes of both groups, such as earlier postoperative oral food intake, bowel sound recovery time, time to first postoperative anal exhaustion and bowel movement, and LOS, were observed and recorded (Figure 1). The aforementioned five indexes were significantly shorter in the research group than in the control group (P < 0.05).
The QLQ-C30 scale was used to evaluate patients’ QOL and determine the influence of the two care modalities on patients’ QOL (Figure 2). The results revealed that the QLQ-C30 scores of the research group, in terms of physical, cognitive, role, emotional, and social functions, were significantly higher than those in the control group (P < 0.05).
The incidence of POCs in the two groups was recorded and analyzed (Table 2). The total incidence rates of abdominal distension, infection, GI bleeding, AL, and DVT were significantly lower in the research group than in the control group (7.69% vs 24.00%, P < 0.05).
| Categories | Research group (n = 52) | Control group (n = 50) | χ2 value | P value |
| Abdominal distension | 2 (3.85) | 3 (6.00) | ||
| Infection | 1 (1.92) | 3 (6.00) | ||
| Gastrointestinal bleeding | 1 (1.92) | 3 (6.00) | ||
| Anastomotic leakage | 0 (0.00) | 2 (4.00) | ||
| Deep vein thrombosis | 0 (0.00) | 1 (2.00) | ||
| Total incidence | 4 (7.69) | 12 (24.00) | 5.126 | 0.024 |
The nursing satisfaction of the research group was 88.46%, which was significantly higher than that of the control group (72.00%, P < 0.05; Table 3).
| Categories | Research group (n = 52) | Control group (n = 50) | χ2 value | P value |
| Very satisfied | 28 (53.85) | 21 (42.00) | ||
| Satisfied | 18 (34.62) | 15 (30.00) | ||
| Dissatisfied | 6 (11.54) | 14 (28.00) | ||
| Nursing satisfaction | 46 (88.46) | 36 (72.00) | 4.382 | 0.036 |
GC is a prevalent GI malignancy, and many patients are often malnourished, which leads to a slow recovery after GC surgery[17]. Thus, effective nursing intervention significantly improves GI function and promotes the recovery of patients following GC surgery. This study mainly adopts two nursing methods for patients undergoing GC surgery: Routine nursing (control group) and FTR + humanized nursing (research group). First, an intergroup comparison of GI function recovery was conducted, and compared with the control group, the research group exhibited shorter first oral food intake, bowel sound recovery time, time to first postoperative anal exhaustion and bowel movement, and LOS. This finding suggests that combined nursing interventions have a superior improvement effect on GI function recovery of patients who underwent GC surgery. The reason is that conventional nursing mainly provides basic nursing services such as preoperative health education, fasting and water prohibition, intestinal preparation, and postoperative diet guidance; thus, providing more detailed and humanized nursing needs is challenging. The combined nursing is characterized by rapid recovery and humanization and involves a series of nursing services covering diet, living habits, health cognition, POC prevention, psychological support, operating room nursing, and pain management before, during, and after the operation with patients as the center, providing patients with a good experience in the whole treatment process. According to Chen et al[18], fast-track nursing shortens postoperative LOS, reduces medical costs, and inhibits CRP secretion compared with conventional nursing, and these findings are similar to the results of this study. In the QOL evaluation, the QLQ-C30 score, based on the assessment of physical, cognitive, role, emotional, and social functions, was used to analyze the effects of the two nursing interventions. Unsurprisingly, compared with conventional nursing, FTR + humanized nursing significantly improved the QOL of patients with GC based on the above dimensions. Yang et al[19] reported that FTR positively influenced the rehabilitation and QOL of patients following kidney stone surgery, similar to our research results. Humanized nursing applied to patients with mental disorders also contributed to the enhanced QOL by alleviating their negative psychology[20]. Conversely, the POCs and nursing satisfaction of the two nursing methods were also investigated. In this study, the main POCs were abdominal distension, infection, and GI bleeding, followed by AL and DVT, which were similar to the observations of Hu et al[21] and Lin et al[22]. In the present study, the incidence of POCs was significantly lower overall in the research group than in the control group. This finding indicated that the combined nursing intervention is significantly safe in GC surgery and can effectively reduce POC risk. Finally, compared with the control group, the research group had obvious advantages in nursing satisfaction, suggesting that FTR + humanized nursing is more popular among patients who underwent GC surgery than conventional nursing. This observation can be attributed to the multi-aspect high-quality detailed nursing provided to patients who underwent GC surgery which fully considers and channels patients’ psychological problems to improve their treatment compliance, and reduces postoperative stress and potential complications. In the study by Lee et al[23], a significant decrease in healthcare costs was observed with FTR compared with standard rehabilitation in patients who underwent elective gastrectomy. Clinical evidence from the study by Wang et al[24] also showed that patients who underwent lung surgery and received humanized nursing experienced reduced economic stress. These findings suggest potential economic advantages when integrating both approaches for GC surgery cases.
Several limitations should be addressed in future research. First, the small cohort (n = 102) might weaken the significance and limit broader application. Second, the single-center design risks selection bias and restricts the broader relevance of the outcomes. Third, the role of external support networks (e.g., family or community) in patient recovery outcomes was overlooked. Future studies incorporating these elements could better elucidate their role in nursing efficacy. Finally, data regarding extended patient outcomes, such as delayed complications (anastomotic stenosis) or shifts in life quality metrics, were lacking. Thus, future studies should prioritize this to evaluate the lasting clinical impli
In summary, FTR + humanized nursing has certain advantages in the care of patients who underwent surgery for GC. It can significantly improve patients’ GI function and QOL and is associated with a lower incidence of complications and higher nursing satisfaction, providing a new choice for the clinical management of such patients.
| 1. | Gullo I, Grillo F, Mastracci L, Vanoli A, Carneiro F, Saragoni L, Limarzi F, Ferro J, Parente P, Fassan M. Precancerous lesions of the stomach, gastric cancer and hereditary gastric cancer syndromes. Pathologica. 2020;112:166-185. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 93] [Cited by in RCA: 113] [Article Influence: 18.8] [Reference Citation Analysis (1)] |
| 2. | Eusebi LH, Telese A, Marasco G, Bazzoli F, Zagari RM. Gastric cancer prevention strategies: A global perspective. J Gastroenterol Hepatol. 2020;35:1495-1502. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 178] [Article Influence: 29.7] [Reference Citation Analysis (0)] |
| 3. | Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394-424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53206] [Cited by in RCA: 56694] [Article Influence: 7086.8] [Reference Citation Analysis (135)] |
| 4. | Smyth EC, Nilsson M, Grabsch HI, van Grieken NC, Lordick F. Gastric cancer. Lancet. 2020;396:635-648. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1150] [Cited by in RCA: 3311] [Article Influence: 551.8] [Reference Citation Analysis (6)] |
| 5. | Kanda M, Ito S, Mochizuki Y, Teramoto H, Ishigure K, Murai T, Asada T, Ishiyama A, Matsushita H, Tanaka C, Kobayashi D, Fujiwara M, Murotani K, Kodera Y. Multi-institutional analysis of the prognostic significance of postoperative complications after curative resection for gastric cancer. Cancer Med. 2019;8:5194-5201. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 43] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 6. | Chen X, Zhang W, Sun X, Shi M, Xu L, Cai Y, Chen W, Mao C, Shen X. Metabolic syndrome predicts postoperative complications after gastrectomy in gastric cancer patients: Development of an individualized usable nomogram and rating model. Cancer Med. 2020;9:7116-7124. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 7. | Wang S, Xu L, Wang Q, Li J, Bai B, Li Z, Wu X, Yu P, Li X, Yin J. Postoperative complications and prognosis after radical gastrectomy for gastric cancer: a systematic review and meta-analysis of observational studies. World J Surg Oncol. 2019;17:52. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 51] [Cited by in RCA: 100] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 8. | Zhang Y, Wang X, Yang H. Effect of traditional Chinese medicine nursing on postoperative patients with gastric cancer and its impact on quality of life. Am J Transl Res. 2021;13:5589-5595. [PubMed] |
| 9. | Song R, Chen C, Shang L. Efficacy and Satisfaction Evaluation of Rapid Rehabilitation Nursing Intervention in Patients with Laparoscopic Myomectomy. J Oncol. 2022;2022:9412050. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 10. | Liang H, Huang J, Tong J, Wang J. Application of Rapid Rehabilitation Nursing in Thoracic Surgery Nursing. J Healthc Eng. 2021;2021:6351170. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 11. | Yu T, Zhou H. Unsupervised Data Mining and Effect of Fast Rehabilitation Nursing Intervention in Fracture Surgery. J Healthc Eng. 2022;2022:7087844. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 12. | Song L, Jin Q, Zhu L, Liu Z, Cheng W. Application of Rapid Rehabilitation Surgical Nursing Combined With Continuous Nursing in Self-Care Ability, Medication Compliance and Quality of Life of Renal Transplant Patients. Front Surg. 2022;9:844533. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 11] [Reference Citation Analysis (0)] |
| 13. | Wang M, Gu X, Yu J, Zhang Y, Chen S. A clinical appraisal of the different types of enteral nutrition support and humanized nursing among cerebral apoplexy ICU patients on mechanical ventilation. Am J Transl Res. 2021;13:9472-9478. [PubMed] |
| 14. | Yan C, Zhou L, Kang X. Effect of humanized care in the treatment of neonatal jaundice and its effect on oxygen saturation. Am J Transl Res. 2021;13:4908-4914. [PubMed] |
| 15. | Özçelik M. Implementation of ERAS Protocols: In Theory and Practice. Turk J Anaesthesiol Reanim. 2024;52:163-168. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 16. | Amsalem D, Martin A, Mosheva M, Soul O, Korotkin L, Ziv A, Gothelf D, Gross R. Delivering Difficult News: Simulation-Enhanced Training Improves Psychiatry Residents' Clinical Communication Skills. Front Psychiatry. 2021;12:649090. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 17. | Xu R, Chen XD, Ding Z. Perioperative nutrition management for gastric cancer. Nutrition. 2022;93:111492. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 54] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 18. | Chen ZX, Liu AH, Cen Y. Fast-track program vs traditional care in surgery for gastric cancer. World J Gastroenterol. 2014;20:578-583. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 34] [Cited by in RCA: 36] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 19. | Yang L, Liu Q, Chi Q, Li J. Effect of rapid rehabilitation nursing on improvement of quality of life after super-miniPCNL and risk analysis for postoperative complications. Am J Transl Res. 2022;14:5146-5154. [PubMed] |
| 20. | Bao L, Shi C, Lai J, Zhan Y. Impact of humanized nursing care on negative emotions and quality of life of patients with mental disorders. Am J Transl Res. 2021;13:13123-13128. [PubMed] |
| 21. | Hu J, Wang LL, Li Y. Effects of high-quality nursing intervention on negative emotions, postoperative complications and gastrointestinal function in patients with gastric cancer surgery. Am J Transl Res. 2022;14:1652-1662. [PubMed] |
| 22. | Lin Y, Shen C, Guo XK, Li Y, Wang DD, Chen X, Wang Z, Wu K, Tao KX, Wu CQ. [Safety evaluation of hyperthermic intraperitoneal chemotherapy in patients with local advanced gastric cancer after radical resection for prevention of peritoneal metastasis]. Zhonghua Wei Chang Wai Ke Za Zhi. 2022;25:48-55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 23. | Lee Y, Yu J, Doumouras AG, Li J, Hong D. Enhanced recovery after surgery (ERAS) versus standard recovery for elective gastric cancer surgery: A meta-analysis of randomized controlled trials. Surg Oncol. 2020;32:75-87. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 72] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 24. | Wang QL, Wang ZB, Zhu JF. Operation room nursing based on humanized nursing mode combined with nitric oxide on rehabilitation effect after lung surgery. World J Clin Cases. 2024;12:3368-3377. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/