Published online Dec 27, 2024. doi: 10.4240/wjgs.v16.i12.3835
Revised: October 12, 2024
Accepted: October 23, 2024
Published online: December 27, 2024
Processing time: 76 Days and 1.1 Hours
Colostomy is important in the treatment of colorectal cancer. However, surgical site wound infections after colostomy seriously affect patients’ physical recovery and quality of life.
To investigate the ability of high-quality nursing care to prevent surgical site wound infections and reduce post-colostomy complications in patients with co
Eighty patients with colorectal cancer who underwent colostomy at our hospital between January 2023 and January 2024 were selected as research subjects. The random number table method was used to divide the participants into control and research groups (n = 40 each). The control group received routine nursing care, while the research group received high-quality nursing care. The differences in indicators were compared between groups.
The baseline characteristics did not differ between the research (n = 40) and control (n = 40) groups (P > 0.05). The incidences of wound infection, inflammation, and delayed wound healing were significantly lower in the research (5.00%) vs control (25.00%) group (P = 0.028). The incidence of postoperative complications, including fistula stenosis, fistula hemorrhage, fistula prolapse, peristome dermatitis, urinary retention, pulmonary infection, and intestinal ob
High-quality nursing interventions can effectively reduce the risk of wound infections and complications in patients undergoing colostomy, promote their postoperative recovery, and improve their satisfaction with the nursing care received.
Core Tip: Colostomy is important for the treatment of colorectal cancer. Surgical site wound infections after colostomy seriously affect patients' physical recovery and quality of life. Here we investigated the effect of high-quality nursing care on postoperative wound infection and complication rates among patients with colorectal cancer treated with colostomy and found that it can effectively reduce their risk of postoperative wound infection and complications, promote their postoperative recovery, and improve their nursing care satisfaction.
- Citation: Cheng Y, Chen YX. Effects of high-quality nursing on surgical site wound infections after colostomy in patients with colorectal cancer. World J Gastrointest Surg 2024; 16(12): 3835-3842
- URL: https://www.wjgnet.com/1948-9366/full/v16/i12/3835.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v16.i12.3835
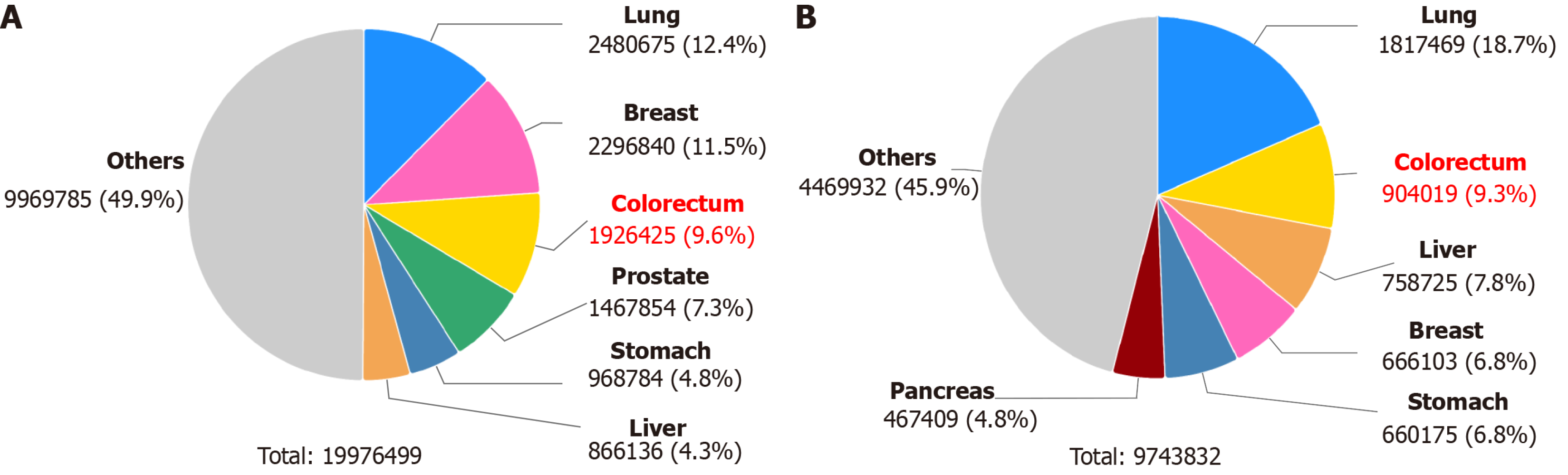
Colorectal cancer is among the most common malignancies of the digestive system worldwide[1-3]. According to data released by the International Agency for Research on Cancer in 2022, colorectal cancer will account for 9.6% of all cancers in terms of incidence (third most common) and 9.3% of all cancers in terms of mortality (second most common) worldwide[4] (Figure 1). In recent years, the incidence and mortality rates of colorectal cancer have remained high, and colostomy remains an important surgical treatment[5,6]. Colostomy involves the surgical removal of the diseased tissue and creation of an artificial vent in the abdominal wall to allow the patient to defecate[7]. However, patients often face a range of postoperative challenges, such as pain, wound infections, wound care difficulties, and psychological stress, that greatly affect their postoperative recovery and quality of life[8-10]. A surgical site wound infection is a common and serious complication of colostomy that may lead to prolonged hospitalization, increased medical costs, and even life-threatening conditions[11,12]. The traditional nursing model pays attention to patients' physiological needs but neglects their psychological and emotional needs. However, psychological adaptation and emotional management are equally important for colostomy patients. In the traditional nursing model, insufficient communication and education occur between nurses and patients, leading to insufficient knowledge of and skills regarding stoma care and affecting patients' self-management abilities. Moreover, the traditional nursing model often lacks an interprofessional multidisciplinary teamwork mechanism that can meet the patients’ comprehensive needs. With the continuous development of nursing concepts, high-quality patient-centered nursing models have gradually gained attention and become a new trend in comprehensive nursing care[13-15].
High-quality nursing care emphasizes individualized and holistic nursing services that aim to improve quality and patient satisfaction via comprehensive nursing interventions provided during the pre-, intra-, and postoperative periods[16,17]. Specific measures include preoperative psychological counseling, postoperative wound care, nutritional support, stoma care counseling, personalized health education, and post-discharge follow-up and support[18]. This model focuses on the patient's physical, psychological, and social needs and seeks to provide comprehensive nursing support[19].
This study aimed to investigate the effect of high-quality nursing care on post-colostomy surgical site wound infections and complications among patients with colorectal cancer and evaluate its effect on their postoperative recovery indices. We hope that a comparison of the clinical effects of conventional and high-quality nursing will provide a scientific basis and reference for the postoperative care of patients with colorectal cancer.
A pre-calculation using G.Power 3.1 with an effect size of d = 0.8, α = 0.05, 1-β = 0.8 resulted in a required sample size of 52. This study was approved by our hospital's ethics committee and included 80 patients with colorectal cancer who underwent colostomy at our hospital between January 2023 and January 2024. Each participant provided written informed consent. The research subjects were divided into control and research groups (n = 40 each) using the random number table method. An intergroup comparison of the baseline data revealed no statistically significant differences (P > 0.05; Table 1).
| Classification | Control group (n = 40) | Research group (n = 40) | χ2/t | P value |
| Gender | 0.051 | 0.822 | ||
| Male | 21 | 23 | ||
| Female | 19 | 17 | ||
| Age (year) | 56.73 ± 3.27 | 57.38 ± 3.45 | 0.126 | 0.872 |
| BMI (kg/m2) | 23.57 ± 2.48 | 23.82 ± 2.74 | 0.757 | 0.406 |
| Tumor location | 0.200 | 0.447 | ||
| Colon | 21 | 18 | ||
| Rectum | 19 | 22 | ||
| TNM staging | 0.495 | 0.781 | ||
| I | 10 | 12 | ||
| II | 18 | 15 | ||
| III | 12 | 13 | ||
| Duke’s staging | 0.915 | 0.633 | ||
| A | 22 | 26 | ||
| B | 12 | 10 | ||
| C | 6 | 4 |
The inclusion criteria were as follows: (1) Confirmed pathological diagnosis; (2) No hematological immune system diseases; (3) No mental abnormalities or compliance issues; (4) No other important organ function impairments; (5) No drug allergies; and (6) Willingness and ability to provide informed consent. The exclusion criteria were as follows: (1) Serious physical ailments that could affect the study outcomes; (2) Combination of other tumors and heart failure; (3) Presence of other malignant tumors; (4) Family or personal history of psychiatric disorders; (5) Inability to communicate effectively; and (6) Early study withdrawal or transfer to another hospital.
Prior to the study's commencement, all nurses in our hospital received uniform training in nursing knowledge and professional education to ensure that they possessed consistent knowledge and standards of care and skills and avoid variations in care quality due to subjective perceptions. Patients in the control group received routine nursing care, the main components of which were conventional nursing practices, condition observations, and routine health education. Patients in the research group received high-quality nursing services based on routine care as follows.
Quality life care: The clinical nursing staff ensured that the ward environment was quiet, clean, warm, and comfortable and instructed the patients and their families to mark their personal belongings and limit noise in the ward area. At the same time, nursing staff reminded patients to follow a reasonable schedule to ensure that they rested adequately. Patients with sleep disorders were advised to play soft music before bedtime to help them fall asleep.
High-quality psychological care: To ensure that the patients experienced a stable psychological state before and after surgery, the nursing staff conducted meticulous psychological assessments and provided appropriate psychological counseling through effective communication. Postoperatively, the patients were regularly visited and provided high-quality nursing services so they felt cared for, supported, and less anxious. Simultaneously, nurses answered the patients' questions in a timely manner using easy-to-understand language and maintained a friendly attitude to build patients’ trust, enhance their confidence in the medical process, and improve their cooperation with the subsequent nursing care.
Stoma quality care: Post-colostomy, the color of the intestinal segment of the stoma was observed to ensure that the stoma was free of bleeding, necrosis, or retraction. Regular cleaning was performed to prevent inflammation. The nurse chose an appropriate stoma bag and ensured that the surrounding skin remained clean and protected to avoid skin irritation. The nurse then instructed the patient to defecate. As most patients experience stomal discomfort after surgery that features a series of physiological and psychological effects on their defecation ability and reduces their quality of life, the nursing staff guided the patients to defecate to reduce this discomfort.
Dietary care: According to individual differences and eating habits, the nurses formulated a personalized diet plan, encouraged the patients to choose easy-to-digest fluids and soft foods, and instructed the patients to avoid eating cold and overly stimulating foods to prevent negative effects on their normal gastrointestinal tract function. The patients were advised to ingest small meals frequently in the early postoperative period with a focus on a balanced diet to ensure sufficient nutritional intake and avoid overeating. Moreover, the patients were encouraged to ingest a fiber-rich diet to maintain smooth intestinal tract function.
Health education: Postoperatively, each patient's stoma status was closely monitored, and appropriate health education was provided. From the 2nd to 7th postoperative days, under the guidance of the attending physician, the patients and their family members were allowed to participate in the process of changing the stoma bag, provided detailed nursing instructions, and instructed to monitor for stomal changes. From the 8th to 11th postoperative days, the patients and their family members were instructed to independently change and clean the stoma bag. Pre-discharge, the patients were clearly informed of the contact information for follow-up consultations and advised about out-of-hospital nursing guidance.
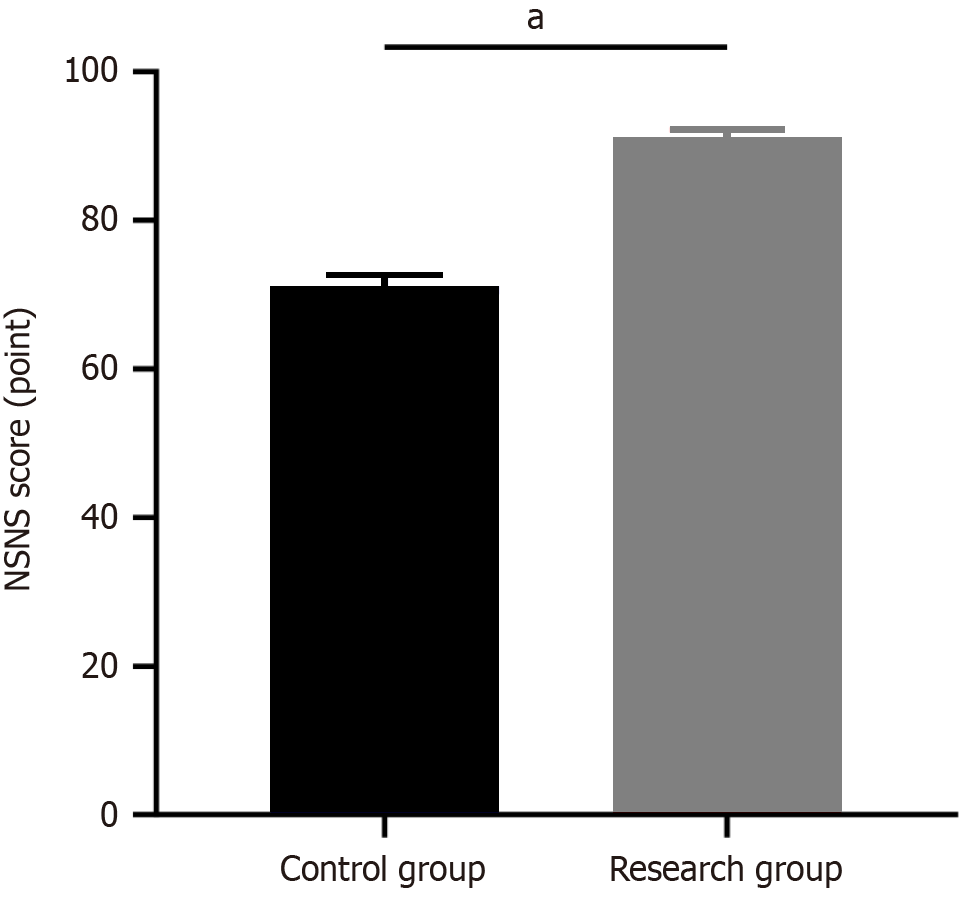
The follow-up and observation indices include the following: (1) Incidence of wound infection, inflammation, and delayed wound healing in both groups; (2) Occurrence of complications in both groups, including fistula stenosis, peristome dermatitis, fistula bleeding, intestinal obstruction, fistula prolapse, urinary retention, and lung infection; (3) Postoperative recovery indices including time to first flatus, time to first bowel movement, and average number of days of hospitalization; and (4) Postoperative patient satisfaction evaluated using the 19-item Newcastle satisfaction with nursing scale (NSNS; total score range, 0–95 points), with a higher overall score indicating higher satisfaction with nursing care.
GraphPad Prism version 8.0 was used for the data analysis and graphing. Counted data are expressed as n (%) and were analyzed using the χ2 test. When the theoretical frequency in the χ2 test was < 5, a continuity-corrected χ2 test was used. Measurement data are expressed as mean ± SD and were analyzed using an independent samples t-test. Values of P < 0.05 were considered statistically significant.
General clinical data such as sex (P = 0.822), age (P = 0.872), body mass index (P = 0.406), tumor location (P = 0.447), Tumor Node Metastasis stage (P = 0.781), and Duke′s stage (P = 0.633) did not differ significantly between groups on the t-test or χ2 test (P > 0.05; Table 1).
The overall incidences of wound infections, wound inflammation, and delayed wound healing were significantly lower in the research vs control group (5.00% vs 25.00%, respectively; P = 0.028; Table 2).
| Classification | Wound infection | Wound inflammation | Delayed wound healing | Overall incidence |
| Control group (n = 40) | 4 (10.00) | 4 (10.00) | 2 (5.00) | 10 (25.00) |
| Research group (n = 40) | 1 (2.50) | 1 (2.50) | 0 | 2 (5.00) |
| χ2 | 4.804 | |||
| P value | 0.028 |
Complications including fistula stenosis, fistula hemorrhage, fistula prolapse, peristome dermatitis, urinary retention, pulmonary infection, and intestinal obstruction were significantly less common in the research vs control group (5.00% vs 27.50%, respectively; P = 0.015; Table 3).
| Classification | Control group (n = 40) | Research group (n = 40) | χ2 | P value |
| Fistula stenosis | 2 (5.00) | 1 (2.50) | ||
| Fistula hemorrhage | 1 (2.50) | 0 | ||
| Fistula prolapse | 2 (5.00) | 0 | ||
| Peristome dermatitis | 1 (2.50) | 0 | ||
| Urine retention | 2 (5.00) | 1 (2.50) | ||
| Pulmonary infection | 2 (5.00) | 0 | ||
| Intestinal obstruction | 1 (2.50) | 0 | ||
| Overall incidence | 11 (27.50) | 2 (5.00) | 5.878 | 0.015 |
Time to first exhaust (51.40 ± 2.22 vs 63.80 ± 2.66, respectively; P < 0.001), time to first bowel movement (61.30 ± 2.21 vs 71.80 ± 2.74, respectively; P < 0.001), and mean length of hospital stay (7.94 ± 0.77 vs 10.44 ± 0.63, respectively; P < 0.001) were significantly shorter in the research vs control group (Table 4).
| Classification | First exhaust (hour) | First bowel movement (hour) | Average hospital stays (day) |
| Control group (n = 40) | 63.80 ± 2.66 | 71.80 ± 2.74 | 10.44 ± 0.63 |
| Research group (n = 40) | 51.40 ± 2.22 | 61.30 ± 2.21 | 7.94 ± 0.77 |
| t value | 11.32 | 9.43 | 7.53 |
| P value | < 0.001 | < 0.001 | < 0.001 |
The mean NSNS score was significantly higher in the research (91.22 ± 0.96) vs control (71.13 ± 1.52) group (P < 0.001; Figure 2).
Individual living and eating habits generally lack health and scientific guidance, leading to a series of digestive diseases[20-22]. Colorectal cancer, a common clinical malignant tumor of the digestive tract, shows an increasing trend in annual incidence, posing a serious threat to human health and safety[23-25]. The treatment of colorectal cancer mainly relies on a surgical approach to remove the tumor, for which a colostomy is important[26,27]. In clinical practice, an increasing number of patients with cancer undergo colostomy. However, the complexity of colorectal cancer, technical difficulty of surgery, and trauma caused by the surgery itself easily trigger physiological stress reactions and psychological fear in patients, leading to an increased risk of postoperative complications that seriously affect the recovery process[28,29].
In current medical care practices, some clinical nursing staff lack empathy and pay insufficient attention to patients' postoperative recovery and psychological adjustments, leading to decreased patient satisfaction rates. High-quality nursing service, on the other hand, is a comprehensive nursing framework that focuses on patients’ needs and aims for consistent improvement, comprehensiveness, and personalization of every nursing process. It also aims to create a physically and mentally supportive recovery environment for patients, effectively alleviate their negative emotions, enhance their trust in nursing staff, and motivate them to proactively participate in the treatment plan, thus optimizing overall treatment efficacy[30-32]. Our hospital has implemented high-quality nursing interventions for patients un
This study investigated the effects of high-quality nursing care on surgical site wound infections and complications after colostomy in patients with colorectal cancer. We found that the incidence of wound infection, wound inflammation, and delayed wound healing was significantly lower in the research vs control group (P = 0.028), as was the incidence of postoperative complications, including fistula stenosis, fistula hemorrhage, fistula prolapse, peristome dermatitis, urinary retention, pulmonary infection and intestinal obstruction (P = 0.015), which may be related to the emphasis on preventing complications in the quality care model, such as strict aseptic operation, proper wound management, standardized incision care, and rational use of antibiotics and analgesic drugs, which helps reduce the risk of postoperative wound infection and complications. This study also assessed the ability of high-quality nursing to improve patients' postoperative recovery indicators and found that the time to first exhaust, time to first bowel movement, and average length of hospital stay of patients were significantly shorter in the research group (P < 0.001), suggesting that early and appropriate limb movement and rehabilitation training under the high-quality nursing model can help promote blood circulation, reduce muscle atrophy, and promote the restoration of intestinal function, thereby accelerating the patients' postoperative recovery process. Moreover, personalized nutritional and psychological support may play an important role in postoperative recovery. Finally, nursing care satisfaction was evaluated using the NSNS, which showed significantly higher satisfaction rates in the research vs control group (P < 0.001), suggesting that patients generally favor high-quality vs traditional nursing care if the cost is the same.
This high-quality nursing model has obvious advantages in postoperative wound management for colostomy patients, as it can effectively prevent wound infections, reduce complications, and promote postoperative recovery. The wide application of this model is expected to provide a more effective strategy for the postoperative care of patients undergoing colostomy, thereby improving their recovery experience and quality of life. Future studies could further explore the cost-effectiveness of the high-quality nursing model and investigate its long-term impact on quality of life.
Although this study is novel, it has some limitations, including its relatively small sample size, subjectivity in case exclusion and inclusion criteria, and relatively short follow-up period. Moreover, other less important confounding factors may have biased the experimental results. Therefore, larger and better-designed clinical trials are needed to verify our findings.
In conclusion, this study demonstrated that the use of high-quality nursing interventions for the prevention of post-colostomy wound infections is effective and can reduce the risk of complications, promote postoperative recovery, and improve patient satisfaction with nursing care. High-quality nursing care is expected to become a more effective strategy for the postoperative care of colostomy patients. In the future, it may be integrated into the standard postoperative care program. Healthcare institutions should strengthen the construction and collaboration of multidisciplinary teams and improve nursing care integration to better implement high-quality nursing care.
| 1. | Eng C, Yoshino T, Ruíz-García E, Mostafa N, Cann CG, O'Brian B, Benny A, Perez RO, Cremolini C. Colorectal cancer. Lancet. 2024;404:294-310. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 193] [Article Influence: 96.5] [Reference Citation Analysis (0)] |
| 2. | Patel SG, Dominitz JA. Screening for Colorectal Cancer. Ann Intern Med. 2024;177:ITC49-ITC64. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 48] [Reference Citation Analysis (2)] |
| 3. | Klimeck L, Heisser T, Hoffmeister M, Brenner H. Colorectal cancer: A health and economic problem. Best Pract Res Clin Gastroenterol. 2023;66:101839. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 117] [Article Influence: 39.0] [Reference Citation Analysis (0)] |
| 4. | Bray F, Laversanne M, Sung H, Ferlay J, Siegel RL, Soerjomataram I, Jemal A. Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2024;74:229-263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5690] [Cited by in RCA: 12367] [Article Influence: 6183.5] [Reference Citation Analysis (6)] |
| 5. | Martellucci J, Balestri R, Brusciano L, Iacopini V, Puccini M, Docimo L, Cianchi F, Buccianti P, Prosperi P. Ileostomy versus colostomy: impact on functional outcomes after total mesorectal excision for rectal cancer. Colorectal Dis. 2023;25:1686-1693. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 6. | Merritt C, Maldonado P. Management of the Difficult Stoma. Surg Clin North Am. 2024;104:579-593. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Reference Citation Analysis (0)] |
| 7. | Emmanuel A, Chohda E, Lapa C, Miles A, Haji A, Ellul J. Defunctioning Stomas Result in Significantly More Short-Term Complications Following Low Anterior Resection for Rectal Cancer. World J Surg. 2018;42:3755-3764. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 33] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 8. | Ayaz-Alkaya S. Overview of psychosocial problems in individuals with stoma: A review of literature. Int Wound J. 2019;16:243-249. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 150] [Article Influence: 18.8] [Reference Citation Analysis (0)] |
| 9. | Yang S, Tang G, Zhang Y, Wei Z, Du D. Meta-analysis: loop ileostomy versus colostomy to prevent complications of anterior resection for rectal cancer. Int J Colorectal Dis. 2024;39:68. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 13] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 10. | Chen C, Liu J. Enhancing Nosocomial Infection Control through the Implementation of High-Quality Nursing Practices. Altern Ther Health Med. 2024;30:300-305. [PubMed] |
| 11. | Murken DR, Bleier JIS. Ostomy-Related Complications. Clin Colon Rectal Surg. 2019;32:176-182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 95] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
| 12. | Chang Z, Liu L, She C, Ren W, Chen H, Zhou C. A meta-analysis examined the effect of stoma on surgical site wound infection in colorectal cancer. Int Wound J. 2023;20:1578-1583. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Reference Citation Analysis (1)] |
| 13. | Hu J, Wang LL, Li Y. Effects of high-quality nursing intervention on negative emotions, postoperative complications and gastrointestinal function in patients with gastric cancer surgery. Am J Transl Res. 2022;14:1652-1662. [PubMed] |
| 14. | Liu J, Lin J, Gao T, Shi F. Observation on the effect of high-quality nursing in patients with coronary heart disease and its effect on cardiac function. Panminerva Med. 2021;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 15. | Zhai Y, Wang X. Study on the effect of high-quality nursing intervention mode on the improvement of emotional status of breast cancer patients. Panminerva Med. 2022;64:295-296. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 16. | Zhang Q, Wan R, Liu C. The impact of intense nursing care in improving anxiety, depression, and quality of life in patients with liver cancer: A systematic review and meta-analysis. Medicine (Baltimore). 2020;99:e21677. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 25] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 17. | Wang Z. Application of High-Quality Nursing Intervention Based on Humanistic Care Combined with the Project Teaching Method in Patients with Acute Leukemia Undergoing Chemotherapy. J Healthc Eng. 2022;2022:2972037. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 18. | Juanamasta IG, Aungsuroch Y, Gunawan J. A Concept Analysis of Quality Nursing Care. J Korean Acad Nurs. 2021;51:430-441. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
| 19. | Flagg AJ. The role of patient-centered care in nursing. Nurs Clin North Am. 2015;50:75-86. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 29] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 20. | Thanikachalam K, Khan G. Colorectal Cancer and Nutrition. Nutrients. 2019;11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 231] [Cited by in RCA: 516] [Article Influence: 73.7] [Reference Citation Analysis (0)] |
| 21. | Peng J, Xu H, Tang X. Global Inequalities in the Burden of Digestive Diseases From 1990 to 2019: Findings From the Global Burden of Disease Study 2019. Gastroenterology. 2024;166:223-224.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 14] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 22. | Khan S, Sebastian SA, Parmar MP, Ghadge N, Padda I, Keshta AS, Minhaz N, Patel A. Factors influencing the quality of life in inflammatory bowel disease: A comprehensive review. Dis Mon. 2024;70:101672. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 22] [Reference Citation Analysis (0)] |
| 23. | Brenner H, Chen C. The colorectal cancer epidemic: challenges and opportunities for primary, secondary and tertiary prevention. Br J Cancer. 2018;119:785-792. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 149] [Cited by in RCA: 212] [Article Influence: 26.5] [Reference Citation Analysis (0)] |
| 24. | Roncucci L, Mariani F. Prevention of colorectal cancer: How many tools do we have in our basket? Eur J Intern Med. 2015;26:752-756. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 81] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 25. | Yu B, Kang J, Lei H, Li Z, Yang H, Zhang M. Immunotherapy for colorectal cancer. Front Immunol. 2024;15:1433315. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 13] [Reference Citation Analysis (0)] |
| 26. | Simard J, Kamath S, Kircher S. Survivorship Guidance for Patients with Colorectal Cancer. Curr Treat Options Oncol. 2019;20:38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 24] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 27. | Huang S, Chen DC, Perera M, Lawrentschuk N. Role of diverting colostomy and reconstruction in managing Fournier's gangrene-a narrative review. BJU Int. 2024;134:534-540. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 28. | Yilmaz E, Çelebi D, Kaya Y, Baydur H. A Descriptive, Cross-sectional Study to Assess Quality of Life and Sexuality in Turkish Patients with a Colostomy. Ostomy Wound Manage. 2017;63:22-29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 19] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 29. | Zhang Q, Liu F, Li Y, Ji L, Yu Y, Yang X. Effect of transverse colostomy versus ileostomy in colorectal anastomosis on post-operative wound complications: A meta-analysis. Int Wound J. 2024;21:e14428. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (1)] |
| 30. | McCarthy B, Fitzgerald S, O'Shea M, Condon C, Hartnett-Collins G, Clancy M, Sheehy A, Denieffe S, Bergin M, Savage E. Electronic nursing documentation interventions to promote or improve patient safety and quality care: A systematic review. J Nurs Manag. 2019;27:491-501. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 69] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 31. | Maliqi B, Hinton R, Chowdury M, Roder-DeWan S, Eluwa A, Kassa M. Prepared health systems provide quality care at all times. BMJ. 2023;380:e072698. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 32. | Wang M, Sun Y, Zhang M, Yu R, Fu J. Effects of high-quality nursing care on quality of life, survival, and recurrence in patients with advanced nonsmall cell lung cancer. Medicine (Baltimore). 2022;101:e30569. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 14] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/