Published online Dec 27, 2024. doi: 10.4240/wjgs.v16.i12.3666
Revised: August 27, 2024
Accepted: October 11, 2024
Published online: December 27, 2024
Processing time: 148 Days and 7 Hours
Hepatolithiasis is a common disease where stones are located in the intrahepatic bile duct. Hepatolithiasis is a disease with regional characteristics. The compli
Core Tip: Hepatolithiasis refers to the primary stones above the confluence of the left and right hepatic ducts, and its main component is brown bile pigment stones. Hepatolithiasis is a disease with regional characteristics. At present, there is no exact explanation for the etiology of hepatolithiasis. Studies at home and abroad suggest that it may be related to lifestyle, biliary bacterial infection, biliary parasite infection, biliary anatomical variation, gene mutation and abnormal gene expression and other factors.
- Citation: Ye YQ, Li PH, Wu Q, Yang SL, Zhuang BD, Cao YW, Xiao ZY, Wen SQ. Evolution of surgical treatment for hepatolithiasis. World J Gastrointest Surg 2024; 16(12): 3666-3674
- URL: https://www.wjgnet.com/1948-9366/full/v16/i12/3666.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v16.i12.3666
Hepatolithiasis refers to primary stones above the confluence of the left and right hepatic ducts, and its main component is brown bile pigment stones. Hepatolithiasis is a disease with regional characteristics. The incidence of hepatolithiasis in Asia is higher than in Europe and America[1]. In recent years, the Japanese literature has reported an incidence of hepatolithiasis showing a downwards trend annually[2], but the outlook in China is still not optimistic, where the incidence in the population is 2%-25%[1], especially in the southwestern region.
Hepatolithiasis is characterized by concealed onset, long disease course, easy recurrence, and many serious complications; the two most serious complications are intrahepatic cholangiocarcinoma and liver cirrhosis. According to the literature, the incidence of intrahepatic cholangiocarcinoma in patients with hepatolithiasis is 1.3%-23.3%[2-6], and the incidence of liver cirrhosis in patients with hepatolithiasis is 3.7%-14.1%[3,7,8]. These two factors are the main causes of death in patients with hepatolithiasis. Therefore, early diagnosis of hepatolithiasis and appropriate treatment methods for intervention are helpful for reducing the incidence of complications, improving prognosis and improving the median survival time of patients[9-12]. At present, there is no exact explanation for the aetiology of hepatolithiasis. Studies at home and abroad suggest that it may be related to lifestyle, biliary bacterial infection[13-21], biliary parasite infection, biliary anatomical variation, gene mutation and abnormal gene expression and other factors[22-31].
At present, the main treatment for hepatolithiasis is surgery, of which there are many methods. Each method has its own advantages and disadvantages. Depending on the characteristics of each case, a suitable surgical method is chosen to obtain the best treatment effect[32-44].
Hepatolithiasis generally shows a segmental distribution, so hepatectomy is a more effective means for the treatment of hepatolithiasis[45]. Since the first reported the success of partial hepatectomy in two patients with hepatolithiasis in 1956, partial hepatectomy has been widely used in the clinic and has achieved good curative effects. It is one of the main surgical methods for treating hepatolithiasis and can achieve the purpose of removing the focus, contact stricture and hepatolithiasis. At present, partial hepatectomy can be roughly divided into two types: Laparotomy and laparoscopic hepatectomy. Laparotomy for hepatectomy is a lengthy procedure, but the technology is mature, so it is the most widely practiced technique in the clinic[45].
In recent years, Li et al[46] conducted a single-center eight-year empirical study. Fifty-six patients with bilateral hepatolithiasis underwent hepatectomy combined with choledochoscopy for intrahepatic bile duct exploration and lithotripsy. The overall initial success rate was 85.7%, and the final clearance rate was 92.9%. Postoperative complications occurred in 15 patients (26.8%), 14 of whom were treated conservatively, and only 1 patient died of liver failure. Fifty-five patients were followed-up, among which 52 of them had stones removed completely during the first operation, and only 3 patients had residual stones. Among the 52 patients whose stones were removed, 7 (13.5%) experienced recurrence. The incidence of postoperative acute cholangitis was 10.9%. This study revealed that IHBDIL combined with hepatectomy is a safe and effective treatment for complex bilateral hepatolithiasis. However, this study involved a small number of samples and was based in a single center; thus, a larger sample size is needed to confirm the feasibility of this method.
Laparoscopic hepatectomy is a technique that has gradually developed in recent years and has been adopted by an increasing number of physicians because of its rapid recovery, relatively low degree of trauma, low degree of blood loss and low incidence of postoperative complications. Laparoscopic hepatectomy can be combined with laparoscopic ul
For patients with intrahepatic and extrahepatic biliary obstruction, Yang et al[49] selected 26 patients with hepatolithiasis, including 25 patients with left hepatolithiasis and 1 patient with right hepatolithiasis. Among the 26 patients, 18 had abdominal pain with jaundice, and 8 had abdominal pain with fever. All 26 patients underwent laparoscopic he
Li et al[50] conducted a meta-analysis of open hepatectomy and laparoscopic hepatectomy (involving 1329 cases). The results revealed that intraoperative blood loss in the laparoscopic treatment group was significantly lower [weighted average difference (WMD): 61.56, 95% confidence interval (95%CI): 14.91-108.20, P = 0.01], the recovery of intestinal function was faster (WMD: 0.98, 95%CI: 0.47-1.48, P = 0.01), and the length of hospital stay was shorter (WMD: 3.32, 95%CI: 2.32-4.32, P < 0.00001). In addition, the analysis revealed that there was no significant difference in operation time (WMD: 21.49, 95%CI: 0.27-43.24, P = 0.05), residual stone rate [odds ratio (OR): 0.79, 95%CI: 0.50-1.25, P = 0.31] or stone recurrence rate (OR: 0.34, 95%CI: 0.11-1.08, P = 0.07) between the two groups. In addition, through subgroup analysis, the results of this study show that the effect of laparoscopy in the treatment of hepatolithiasis in the left lateral lobe and left side is satisfactory.
Liu et al[51] conducted a meta-analysis (involving 1352 patients). The results revealed that intraoperative blood loss was significantly lower in patients with hepatolithiasis in the laparoscopic group [standardized mean difference (SMD):
Therefore, the safety and postoperative recovery speed of laparoscopic hepatectomy are better than those of open hepatectomy[52-55]. However, some studies have shown[56,57] that laparoscopic hepatectomy takes longer than open hepatectomy, which is contrary to the results of the previous two studies and may be related to the technical proficiency of surgeons.
The main inducing factor of hepatolithiasis is bile duct stricture. Plentz and Malek[58] reported that an average of 24.3% of patients with hepatolithiasis in China also have bile duct stricture. If the bile duct stricture is not removed during operation, even if the stones are removed, there is a high possibility of recurrence because the bile flow velocity will change at the bile duct stricture, and an eddy current may form when the bile flows through this location. It can also stagnate here, providing conditions for the formation of stones. Therefore, the bile duct stricture must be removed during operation. From the invention of Y-shaped anastomosis, which was proposed by Roux in 1897, to the invention of choledochoduodenojejunostomy and Roux-en-Y anastomosis in recent years, this method has improved many times and has achieved good results in patients with hepatolithiasis with bile duct stricture. At present, the most used surgical methods to solve biliary stricture are choledochojejunal Roux-en-Y anastomosis and modified choledochojejunal loop anastomosis[59]. Laparotomy or laparoscopy can also be used.
In recent years, Ejaz et al[60] had modified this method and proposed transantral choledochojejunostomy. A retrospective analysis of 392 patients (70 patients in the improved group and 322 patients in the control group) revealed that there was no significant difference in hospital stay, intraoperative blood loss or incidence of postoperative complications between the two groups compared with traditional choledochojejunostomy (P > 0.05). The incidence of gastric emptying disturbance in the improved group significantly decreased [2 (2.9%) vs 32 (9.9%), P = 0.003], and the time interval of eating fluid postoperation significantly decreased [(64.7 ± 16.3) vs (76.1 ± 24.6) h, P = 0.041]. Gastaca et al[61] proposed the high choledochojejunostomy method. However, regardless of how the operation is improved, its role in treating hepatolithiasis should be "unobstructed drainage" rather than removing choledocholithiasis through choledochojejunostomy. The implementation of choledochojejunostomy can lead to many complications, such as reflux cholangitis[62], biliary infection, anastomotic stricture, and bile duct carcinogenesis[63]. The main causes of these complications are the loss of sphincter function and changes in the intestinal anatomical structure, so clinicians should fully understand the indications for choledochojejunostomy and not perform the operation blindly. For patients with hepatolithiasis, choledocholithiasis should be removed, and the bile duct stricture should be corrected as much as possible before choledochojejunostomy; otherwise, the intrahepatic lesions may not be relieved, and the intestinal contents could flow back into the bile duct, aggravating biliary infection and causing biliary carcinogenesis[64], which can endanger the lives of patients. Moreover, to avoid the occurrence of residual stones and the recurrence of postoperative bile duct stricture, Roux-en-Y anastomosis with a subcutaneous blind loop can be performed. Post-operation, reexamination or cholangiography can be performed through the subcutaneous blind loop, and the biliary stricture can be dilated through this channel to avoid secondary operation.
Cui et al[65] proposed that to preserve the function of the sphincter of Oddi and minimize residual intrahepatic bile duct stones, subcutaneous choledochoplasty should be used. According to their study, 24% (32/146) of patients with recurrent or residual stones can undergo biliary drainage, stone removal and stricture dilatation through the subcu
Laparoscopic choledochojejunostomy is currently advocated for in the clinic, but it has some technical difficulties and requires long-term in-depth study by surgeons[66,67]. Compared with open choledochojejunostomy, laparoscopic choledochojejunostomy can better expose the operative visual field and anatomical structure. Laparoscopic choledochojejunostomy is considered a safe and effective surgical method[67-70].
This operation is one of the most basic surgical procedures for treating hepatolithiasis. Traditional choledocholithotomy relies only on the experience of surgeons to remove stones, which has great limitations, and thus, the rate of postoperative residual stones is as high as 30%. At present, choledocholithotomy requires choledochoscopy combined with cho
Percutaneous transhepatic punctures can be dated back to 1937. Huard and Hop[73] established a channel via percu
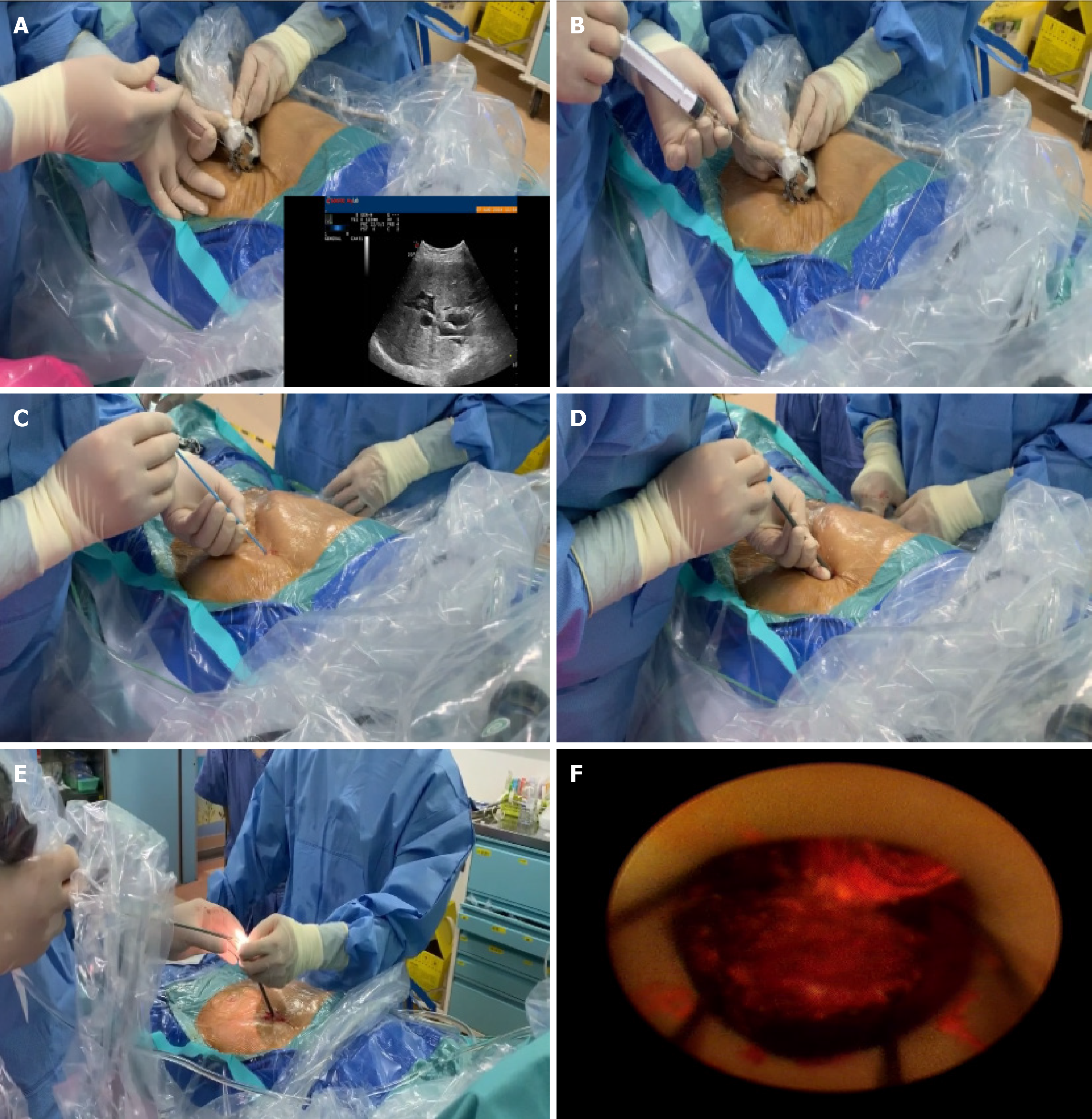
Wang et al[76] conducted a comparative study of traditional PTCSs and PTCSLs. A retrospective study was conducted on 118 patients with hepatolithiasis (51 patients treated with PTCS and 67 patients treated with PTCSL) from 2007 to 2014, and the efficacy and safety of the two groups were compared. The results revealed that there was no significant difference in operation time, intraoperative blood loss or blood transfusion between the two groups, and the stone clearance rate in the PTCSL group was significantly better than that in the PTCS group (P = 0.021; OR = 0.201; 95%CI: 0.051-0.785). The recurrence rate of stones was 9% in the PTCSL group and 22% in the PTCS group. The hospitalization time of the PTCSL group was also significantly shorter than that of the PTCS group (P = 0.001; OR = 1.337; 95%CI: 1.132-1.58). Traditional PTCS operation no longer meets the clinical needs for the treatment of hepatolithiasis, but PTOBF is an ideal method for the treatment of hepatolithiasis because of its good curative effect and high safety (Figure 1).
At present, liver transplantation (LT) is considered the last line of defence for the treatment of hepatolithiasis[77]. For patients with hepatolithiasis, the indications for LT are as follows: (1) Patients with primary hepatolithiasis secondary to decompensated biliary cirrhosis complicated with portal hypertension; (2) Diffuse hepatolithiasis of the whole liver combined with recurrent cholangitis, bile duct stricture and obstructive jaundice, which cannot be completely removed by partial hepatectomy, choledochojejunostomy or choledochoscopy, seriously affecting quality of life; and (3) Those who have undergone many operations where the focus of the stone cannot be removed. LT can be used for the treatment of hepatolithiasis, and the quality of life of patients undergoing LT is one of the conditions used to evaluate the suitability of the operation.
McLean et al[78] conducted a questionnaire survey on the quality of life of LT patients with liver diseases. The results revealed that the overall quality of life of LT patients significantly improved after long-term treatment, and the average therapeutic effect was 6.3 (95%CI: 2.1-10.9). Moreover, LT is affected by many factors, such as a shortage of liver sources, high cost of operation, difficulty of LT, many postoperative complications and immune repulsion reactions[79,80], which restrict the development of the operation. Although many researchers worldwide have made progress in recent years to reduce the risks associated with LT[81], there is still a long way to go.
With the continuous updates and development of medical technology, the treatment of hepatolithiasis has improved. Surgical treatment is still the most effective method for hepatolithiasis. Although there are many surgical methods at present, instead of separating these surgical methods, doctors should formulate a set of accurate surgical plans according to the condition of the patient and combine the advantages of the various surgical methods to achieve the clinical goal of removing lesions and stones, correcting stenosis, unobstructing drainage, preventing recurrence, and improving the quality of life of patients.
| 1. | Kim HJ, Kim JS, Joo MK, Lee BJ, Kim JH, Yeon JE, Park JJ, Byun KS, Bak YT. Hepatolithiasis and intrahepatic cholangiocarcinoma: A review. World J Gastroenterol. 2015;21:13418-13431. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 74] [Cited by in RCA: 107] [Article Influence: 9.7] [Reference Citation Analysis (3)] |
| 2. | Suzuki Y, Mori T, Yokoyama M, Nakazato T, Abe N, Nakanuma Y, Tsubouchi H, Sugiyama M. Hepatolithiasis: analysis of Japanese nationwide surveys over a period of 40 years. J Hepatobiliary Pancreat Sci. 2014;21:617-622. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 68] [Article Influence: 5.7] [Reference Citation Analysis (2)] |
| 3. | Suzuki Y, Mori T, Abe N, Sugiyama M, Atomi Y. Predictive factors for cholangiocarcinoma associated with hepatolithiasis determined on the basis of Japanese Multicenter study. Hepatol Res. 2012;42:166-170. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 38] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 4. | Tazuma S, Nakanuma Y. Clinical features of hepatolithiasis: analyses of multicenter-based surveys in Japan. Lipids Health Dis. 2015;14:129. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 15] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 5. | Tabrizian P, Jibara G, Shrager B, Schwartz ME, Roayaie S. Hepatic resection for primary hepatolithiasis: a single-center Western experience. J Am Coll Surg. 2012;215:622-626. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 55] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 6. | Kim HJ, Kim JS, Suh SJ, Lee BJ, Park JJ, Lee HS, Kim CD, Bak YT. Cholangiocarcinoma Risk as Long-term Outcome After Hepatic Resection in the Hepatolithiasis Patients. World J Surg. 2015;39:1537-1542. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 35] [Article Influence: 3.2] [Reference Citation Analysis (1)] |
| 7. | Pu Q, Zhang C, Ren R, Huang Z, Jin K, Cao G, Zhu M, Zeng Y, Zhao W. Choledochoscopic lithotripsy is a useful adjunct to laparoscopic common bile duct exploration for hepatolithiasis: a cohort study. Am J Surg. 2016;211:1058-1063. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 8. | Park JS, Jeong S, Lee DH, Bang BW, Lee JI, Lee JW, Kwon KS, Kim HK, Shin YW, Kim YS, Park SG. Risk factors for long-term outcomes after initial treatment in hepatolithiasis. J Korean Med Sci. 2013;28:1627-1631. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 31] [Article Influence: 2.4] [Reference Citation Analysis (2)] |
| 9. | Cha BH, Jang MJ, Lee SH. Alcohol Consumption Can Reduce the Risk of Gallstone Disease: A Systematic Review with a Dose-Response Meta-Analysis of Case-Control and Cohort Studies. Gut Liver. 2019;13:114-131. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 27] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 10. | Chang CM, Chiu THT, Chang CC, Lin MN, Lin CL. Plant-Based Diet, Cholesterol, and Risk of Gallstone Disease: A Prospective Study. Nutrients. 2019;11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 32] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 11. | Ryu S, Chang Y, Kim YS, Kim HJ. Prolonged sitting increases the risk of gallstone disease regardless of physical activity: a cohort study. Scand J Gastroenterol. 2018;53:864-869. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 12. | Zhang YP, Zhao YL, Sun YL, Zhu RT, Wang WJ, Li J. Physical Activity and the Risk of Gallstone Disease: A Systematic Review and Meta-analysis. J Clin Gastroenterol. 2017;51:857-868. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 21] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 13. | Shen H, Ye F, Xie L, Yang J, Li Z, Xu P, Meng F, Li L, Chen Y, Bo X, Ni M, Zhang X. Metagenomic sequencing of bile from gallstone patients to identify different microbial community patterns and novel biliary bacteria. Sci Rep. 2015;5:17450. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 45] [Cited by in RCA: 81] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 14. | Schneider J, De Waha P, Hapfelmeier A, Feihl S, Römmler F, Schlag C, Algül H, Schmid RM, Wantia N, Huber W, Weber A. Risk factors for increased antimicrobial resistance: a retrospective analysis of 309 acute cholangitis episodes. J Antimicrob Chemother. 2014;69:519-525. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 27] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 15. | Stewart L, Ponce R, Oesterle AL, Griffiss JM, Way LW. Pigment gallstone pathogenesis: slime production by biliary bacteria is more important than beta-glucuronidase production. J Gastrointest Surg. 2000;4:547-553. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 41] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 16. | Stewart L, Oesterle AL, Erdan I, Griffiss JM, Way LW. Pathogenesis of pigment gallstones in Western societies: the central role of bacteria. J Gastrointest Surg. 2002;6:891-903; discussion 903. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 50] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 17. | Maki T. Pathogenesis of calcium bilirubinate gallstone: role of E. coli, beta-glucuronidase and coagulation by inorganic ions, polyelectrolytes and agitation. Ann Surg. 1966;164:90-100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 332] [Cited by in RCA: 328] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 18. | Pan S, Li X, Jiang P, Jiang Y, Shuai L, He Y, Li Z. Variations of ABCB4 and ABCB11 genes are associated with primary intrahepatic stones. Mol Med Rep. 2015;11:434-446. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 22] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 19. | Pavithra S, Rao U, Mohan P, Venkataraman J. Bactibilia in pigment gallstone disease: A report from the Indian subcontinent. Dig Liver Dis. 2010;42:231-232. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 20. | Sung JY, Leung JW, Shaffer EA, Lam K, Costerton JW. Bacterial biofilm, brown pigment stone and blockage of biliary stents. J Gastroenterol Hepatol. 1993;8:28-34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 79] [Article Influence: 2.4] [Reference Citation Analysis (1)] |
| 21. | Prouty AM, Schwesinger WH, Gunn JS. Biofilm formation and interaction with the surfaces of gallstones by Salmonella spp. Infect Immun. 2002;70:2640-2649. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 247] [Cited by in RCA: 255] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 22. | Huang MH, Chen CH, Yen CM, Yang JC, Yang CC, Yeh YH, Chou DA, Yueh SK, Yang YY, Nien CK. Relation of hepatolithiasis to helminthic infestation. J Gastroenterol Hepatol. 2005;20:141-146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 37] [Article Influence: 1.8] [Reference Citation Analysis (1)] |
| 23. | Rana SS, Bhasin DK, Nanda M, Singh K. Parasitic infestations of the biliary tract. Curr Gastroenterol Rep. 2007;9:156-164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 52] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 24. | Lee CF, Lee WC, Wu RC, Chen TC. Intrahepatic Duct Stones Harboring Ascariasis Ova: A Case Report. Medicine (Baltimore). 2016;95:e3139. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 25. | Leung JW, Yu AS. Hepatolithiasis and biliary parasites. Baillieres Clin Gastroenterol. 1997;11:681-706. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 35] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 26. | ASAKURA S. Crystallographic studies on the eggs of various human parasites. I. Observation with polarization microscope. Tohoku J Exp Med. 1956;64:105-115. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 27. | Lim JH. Oriental cholangiohepatitis: pathologic, clinical, and radiologic features. AJR Am J Roentgenol. 1991;157:1-8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 91] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 28. | Schulman A. Intrahepatic biliary stones: imaging features and a possible relationship with ascaris lumbricoides. Clin Radiol. 1993;47:325-332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 16] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 29. | Pilankar KS, Amarapurkar AD, Joshi RM, Shetty TS, Khithani AS, Chemburkar VV. Hepatolithiasis with biliary ascariasis--a case report. BMC Gastroenterol. 2003;3:35. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 30. | Choi D, Lim JH, Lee KT, Lee JK, Choi SH, Heo JS, Choi DW, Jang KT, Lee NY, Kim S, Hong ST. Gallstones and Clonorchis sinensis infection: a hospital-based case-control study in Korea. J Gastroenterol Hepatol. 2008;23:e399-e404. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 41] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 31. | Rim HJ. Clonorchiasis: an update. J Helminthol. 2005;79:269-281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 224] [Cited by in RCA: 199] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 32. | Pauli-Magnus C, Lang T, Meier Y, Zodan-Marin T, Jung D, Breymann C, Zimmermann R, Kenngott S, Beuers U, Reichel C, Kerb R, Penger A, Meier PJ, Kullak-Ublick GA. Sequence analysis of bile salt export pump (ABCB11) and multidrug resistance p-glycoprotein 3 (ABCB4, MDR3) in patients with intrahepatic cholestasis of pregnancy. Pharmacogenetics. 2004;14:91-102. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 201] [Cited by in RCA: 188] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 33. | Chen R, Wang J, Tang S, Zhang Y, Lv X, Wu S, Yang Z, Xia Y, Chen D, Zhan S. Role of polymorphic bile salt export pump (BSEP, ABCB11) transporters in anti-tuberculosis drug-induced liver injury in a Chinese cohort. Sci Rep. 2016;6:27750. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 13] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 34. | Marschall HU, Katsika D, Rudling M, Einarsson C. The genetic background of gallstone formation: an update. Biochem Biophys Res Commun. 2010;396:58-62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 26] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 35. | Gan L, Pan S, Cui J, Bai J, Jiang P, He Y. Functional analysis of the correlation between ABCB11 gene mutation and primary intrahepatic stone. Mol Med Rep. 2019;19:195-204. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 36. | Lee JY, Kim JS, Moon JM, Lim SA, Chung W, Lim EH, Lee BJ, Park JJ, Bak YT. Incidence of Cholangiocarcinoma with or without Previous Resection of Liver for Hepatolithiasis. Gut Liver. 2013;7:475-479. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 20] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 37. | Ni ZK, Lin D, Wang ZQ, Jin HM, Li XW, Li Y, Huang H. Precision Liver Resection: Three-Dimensional Reconstruction Combined with Fluorescence Laparoscopic Imaging. Surg Innov. 2021;28:71-78. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 38. | Acalovschi M, Tirziu S, Chiorean E, Krawczyk M, Grünhage F, Lammert F. Common variants of ABCB4 and ABCB11 and plasma lipid levels: a study in sib pairs with gallstones, and controls. Lipids. 2009;44:521-526. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 27] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 39. | Kubitz R, Dröge C, Stindt J, Weissenberger K, Häussinger D. The bile salt export pump (BSEP) in health and disease. Clin Res Hepatol Gastroenterol. 2012;36:536-553. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 147] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 40. | Martinez-Lopez E, Curiel-Lopez F, Hernandez-Nazara A, Moreno-Luna LE, Ramos-Marquez ME, Roman S, Panduro A. Influence of ApoE and FABP2 polymorphisms and environmental factors in the susceptibility to gallstone disease. Ann Hepatol. 2015;14:515-523. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 20] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 41. | Kubitz R, Dröge C, Kluge S, Stindt J, Häussinger D. Genetic variations of bile salt transporters. Drug Discov Today Technol. 2014;12:e55-e67. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 42. | Hu G, He P, Liu Z, Chen Q, Zheng B, Zhang Q. Diagnosis of ABCB11 gene mutations in children with intrahepatic cholestasis using high resolution melting analysis and direct sequencing. Mol Med Rep. 2014;10:1264-1274. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 16] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 43. | Tai Y, Xie Y, Tang CW. Compound heterozygous mutations of ABCB11 responsible for benign recurrent intrahepatic cholestasis. J Dig Dis. 2015;16:299-302. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 44. | Park JS, Ko JS, Seo JK, Moon JS, Park SS. Clinical and ABCB11 profiles in Korean infants with progressive familial intrahepatic cholestasis. World J Gastroenterol. 2016;22:4901-4907. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 8] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 45. | Tan J, Tan Y, Chen F, Zhu Y, Leng J, Dong J. Endoscopic or laparoscopic approach for hepatolithiasis in the era of endoscopy in China. Surg Endosc. 2015;29:154-162. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 29] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 46. | Li EL, Yuan RF, Liao WJ, Feng Q, Lei J, Yin XB, Wu LQ, Shao JH. Intrahepatic bile duct exploration lithotomy is a useful adjunctive hepatectomy method for bilateral primary hepatolithiasis: an eight-year experience at a single centre. BMC Surg. 2019;19:16. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 16] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 47. | Jin RA, Wang Y, Yu H, Liang X, Cai XJ. Total laparoscopic left hepatectomy for primary hepatolithiasis: Eight-year experience in a single center. Surgery. 2016;159:834-841. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 30] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 48. | Gong Y, Tang Y, Geng Y, Zhou Y, Yu M, Huang B, Sun Z, Tang H, Jian Z, Hou B. Comparative safety and effectiveness of ultrasound-guided radiofrequency ablation combined with preoperative three-dimensional reconstruction versus surgical resection for solitary hepatocellular carcinoma of 3-5 cm. J Cancer. 2019;10:5568-5574. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 49. | Yang J, Zhang F, Du X, Wang A, Lv S, Fang Z. Laparoscopic hepatectomy combined with endoscopic papillary balloon dilation for complex bile duct stones. ANZ J Surg. 2018;88:E522-E525. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 50. | Li H, Zheng J, Cai JY, Li SH, Zhang JB, Wang XM, Chen GH, Yang Y, Wang GS. Laparoscopic VS open hepatectomy for hepatolithiasis: An updated systematic review and meta-analysis. World J Gastroenterol. 2017;23:7791-7806. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 27] [Cited by in RCA: 42] [Article Influence: 4.7] [Reference Citation Analysis (1)] |
| 51. | Liu X, Min X, Ma Z, He X, Du Z. Laparoscopic hepatectomy produces better outcomes for hepatolithiasis than open hepatectomy: An updated systematic review and meta-analysis. Int J Surg. 2018;51:151-163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 31] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 52. | Lee KF, Fong AK, Chong CC, Cheung SY, Wong J, Lai PB. Robotic Liver Resection For Primary Hepatolithiasis: Is It Beneficial? World J Surg. 2016;40:2490-2496. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 53. | Ye YQ, Cao YW, Li RQ, Li EZ, Yan L, Ding ZW, Fan JM, Wang P, Wu YX. Three-dimensional visualization technology for guiding one-step percutaneous transhepatic cholangioscopic lithotripsy for the treatment of complex hepatolithiasis. World J Gastroenterol. 2024;30:3393-3402. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 6] [Reference Citation Analysis (1)] |
| 54. | Kim YK, Han HS, Yoon YS, Cho JY, Lee W. Laparoscopic approach for right-sided intrahepatic duct stones: a comparative study of laparoscopic versus open treatment. World J Surg. 2015;39:1224-1230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 22] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 55. | Tian J, Li JW, Chen J, Fan YD, Bie P, Wang SG, Zheng SG. The safety and feasibility of reoperation for the treatment of hepatolithiasis by laparoscopic approach. Surg Endosc. 2013;27:1315-1320. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 23] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 56. | Wu TJ, Wang F, Lin YS, Chan KM, Yu MC, Lee WC. Right hepatectomy by the anterior method with liver hanging versus conventional approach for large hepatocellular carcinomas. Br J Surg. 2010;97:1070-1078. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 48] [Article Influence: 3.0] [Reference Citation Analysis (1)] |
| 57. | Langenhuijsen J, Birtle A, Klatte T, Porpiglia F, Timsit MO. Surgical Management of Adrenocortical Carcinoma: Impact of Laparoscopic Approach, Lymphadenectomy, and Surgical Volume on Outcomes-A Systematic Review and Meta-analysis of the Current Literature. Eur Urol Focus. 2016;1:241-250. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 27] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 58. | Plentz RR, Malek NP. Clinical presentation, risk factors and staging systems of cholangiocarcinoma. Best Pract Res Clin Gastroenterol. 2015;29:245-252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 61] [Article Influence: 5.5] [Reference Citation Analysis (1)] |
| 59. | Gadelhak N, Shehta A, Hamed H. Diagnosis and management of choledochal cyst: 20 years of single center experience. World J Gastroenterol. 2014;20:7061-7066. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 32] [Cited by in RCA: 29] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 60. | Ejaz A, Spolverato G, Kim Y, Dodson R, Sicklick JK, Pitt HA, Lillemoe KD, Cameron JL, Pawlik TM. Long-term health-related quality of life after iatrogenic bile duct injury repair. J Am Coll Surg. 2014;219:923-32.e10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 36] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 61. | Gastaca M, Matarranz A, Muñoz F, Valdivieso A, Aguinaga A, Testillano M, Bustamante J, Terreros I, Suarez MJ, Montejo M, Ortiz de Urbina J. Biliary complications in orthotopic liver transplantation using choledochocholedochostomy with a T-tube. Transplant Proc. 2012;44:1554-1556. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 19] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 62. | Said A, Safdar N, Lucey MR, Knechtle SJ, D'Alessandro A, Musat A, Pirsch J, Kalayoglu M, Maki DG. Infected bilomas in liver transplant recipients, incidence, risk factors and implications for prevention. Am J Transplant. 2004;4:574-582. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 50] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 63. | Jo JH, Chung MJ, Park JY, Bang S, Park SW, Kim KS, Lee WJ, Song SY, Chung JB. High serum CA19-9 levels are associated with an increased risk of cholangiocarcinoma in patients with intrahepatic duct stones: a case-control study. Surg Endosc. 2013;27:4210-4216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 13] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 64. | Tocchi A, Mazzoni G, Liotta G, Lepre L, Cassini D, Miccini M. Late development of bile duct cancer in patients who had biliary-enteric drainage for benign disease: a follow-up study of more than 1,000 patients. Ann Surg. 2001;234:210-214. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 186] [Cited by in RCA: 178] [Article Influence: 7.1] [Reference Citation Analysis (1)] |
| 65. | Cui L, Xu Z, Ling XF, Wang LX, Hou CS, Wang G, Zhou XS. Laparoscopic hepaticoplasty using gallbladder as a subcutaneous tunnel for hepatolithiasis. World J Gastroenterol. 2014;20:3350-3355. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 3] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 66. | Hori T, Oike F, Furuyama H, Machimoto T, Kadokawa Y, Hata T, Kato S, Yasukawa D, Aisu Y, Sasaki M, Kimura Y, Takamatsu Y, Naito M, Nakauchi M, Tanaka T, Gunji D, Nakamura K, Sato K, Mizuno M, Iida T, Yagi S, Uemoto S, Yoshimura T. Protocol for laparoscopic cholecystectomy: Is it rocket science? World J Gastroenterol. 2016;22:10287-10303. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 19] [Cited by in RCA: 15] [Article Influence: 1.5] [Reference Citation Analysis (1)] |
| 67. | Lee JS, Hong TH. Laparoscopic choledochojejunostomy in various hepatobiliary and pancreatic surgeries: a single surgeon's experience. J Laparoendosc Adv Surg Tech A. 2015;25:305-310. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 68. | Chander J, Mangla V, Vindal A, Lal P, Ramteke VK. Laparoscopic choledochoduodenostomy for biliary stone disease: a single-center 10-year experience. J Laparoendosc Adv Surg Tech A. 2012;22:81-84. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 17] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 69. | Chen D, Zhu A, Zhang Z. Total laparoscopic Roux-en-Y cholangiojejunostomy for the treatment of biliary disease. JSLS. 2013;17:178-187. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 17] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 70. | Hori T, Aisu Y, Yamamoto M, Yasukawa D, Iida T, Yagi S, Taniguchi K, Uemoto S. Laparoscopic approach for choledochojejunostomy. Hepatobiliary Pancreat Dis Int. 2019;18:285-288. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 71. | Lu MD, Yin XY, Huang JF. Intraoperative liver ultrasound: the Chinese experience. Ultrasound Q. 2001;17:63-68. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 72. | Hatanaka H, Yamamoto H, Yano T, Ushio J, Tomiyama T, Wada S, Sakamoto H, Okada M, Tamada K, Sugano K. Double-balloon endoscopy for hepatolithiasis with multiple stones associated with reflux of intestinal contents into the bile duct in a patient with Roux-en-Y hepaticojejunostomy. Dig Endosc. 2012;24:479. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 73. | Atkinson M, Happey MG, Smiddy FG. Percutaneous transhepatic cholangiography. New Methods Diagn Res. 1960;1:357-365. |
| 74. | Takada T, Uchiyama K, Yasuda H, Hasegawa H. Indications for the choledochoscopic removal of intrahepatic stones based on the biliary anatomy. Am J Surg. 1996;171:558-561. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 11] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 75. | Chen C, Huang M, Yang J, Yang C, Yeh Y, Wu H, Chou D, Yueh S, Nien C. Reappraisal of percutaneous transhepatic cholangioscopic lithotomy for primary hepatolithiasis. Surg Endosc. 2005;19:505-509. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 49] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 76. | Wang P, Sun B, Huang B, Xie J, Liu Y, Zhu C, Ye C, Zhou Z. Comparison Between Percutaneous Transhepatic Rigid Cholangioscopic Lithotripsy and Conventional Percutaneous Transhepatic Cholangioscopic Surgery for Hepatolithiasis Treatment. Surg Laparosc Endosc Percutan Tech. 2016;26:54-59. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 32] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 77. | Lorio E, Patel P, Rosenkranz L, Patel S, Sayana H. Management of Hepatolithiasis: Review of the Literature. Curr Gastroenterol Rep. 2020;22:30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 48] [Article Influence: 8.0] [Reference Citation Analysis (2)] |
| 78. | McLean KA, Drake TM, Sgrò A, Camilleri-Brennan J, Knight SR, Ots R, Adair A, Wigmore SJ, Harrison EM. The effect of liver transplantation on patient-centred outcomes: a propensity-score matched analysis. Transpl Int. 2019;32:808-819. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 79. | Stravitz RT, Lee WM. Acute liver failure. Lancet. 2019;394:869-881. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 513] [Cited by in RCA: 631] [Article Influence: 90.1] [Reference Citation Analysis (0)] |
| 80. | Yau AA, Farouk SS. Severe hypercalcemia preceding a diagnosis of Pneumocystis jirovecii pneumonia in a liver transplant recipient. BMC Infect Dis. 2019;19:739. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 81. | Martins PN, Selzner M, Dayangac M, Ling Q, Ng KT, Huang KT, Taner T, Mas VR, Ekser B. What Is Hot and New in Basic Science in Liver Transplantation in 2018? Report of the Basic Science Committee of the International Liver Transplantation Society. Transplantation. 2019;103:654-659. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/