Published online Dec 27, 2020. doi: 10.4240/wjgs.v12.i12.549
Peer-review started: July 23, 2020
First decision: October 6, 2020
Revised: October 16, 2020
Accepted: November 12, 2020
Article in press: November 12, 2020
Published online: December 27, 2020
Processing time: 151 Days and 11.5 Hours
Simple hepatic cysts are relatively common in adults, and mostly appear as asymptomatic incidental radiologic findings. Occasionally, a large cyst will cause symptoms. Elevations in the serum biomarkers protein induced by vitamin K absence (PIVKA)-II, cancer antigen (CA) 12-5, and CA19-9 are often associated with malignant tumors in the liver or bile ducts. This is the first report to describe a case of hepatic cyst with elevated levels of PIVKA-II and CA12-5.
An 84-year-old Chinese woman was admitted with gradual abdominal distension. Her symptoms started 1 year ago, and she had poor appetite and a weight loss of 5 kg within the past 2 wk. She denied any symptoms associated with abdominal pain, fever and chills, nausea and vomiting, etc. The abdomen was enlarged, more in the right upper quadrant, without tenderness. Laboratory examination showed significantly increased serum levels of PIVKA-II, CA12-5, and CA19-9. A computed tomography scan revealed multiple round cysts in the liver with clear boundaries. The largest cyst was 20.1 cm × 12.2 cm × 19.6 cm in size, located in the right lobe of the liver with mild dilatation of the intrahepatic bile duct, but there was no contrast enhancement. Percutaneous drainage on the largest hepatic cyst and polycinnamol sclerosing agent injection into the cyst cavity were performed. After treatment, the patient’s symptoms relieved and the elevated serum tumor makers reduced to the normal levels dramatically.
The present report identifies an unusual case of a giant hepatic cyst with marked elevation of serum tumor marker levels of PIVKA-II, CA12-5, and CA19-9. After treatment, these three serum markers dramatically decreased to normal levels. The mechanisms for the elevation of these tumor markers may be as follows: (1) A giant hepatic cyst compresses the liver, causing injury to the hepatocytes, which may lead to secretion of a large amount of PIVKA-II; and (2) Some tumor-associated antigens, such as carcinoembryonic antigen, CA19-9, CA12-5, and CA15-3, are expressed on inflammatory cells.
Core Tip: Simple hepatic cysts typically appear as asymptomatic benign tumors of the liver without elevation of any diagnostic serum biomarkers. However, over the years, a few cases of simple hepatic cysts with elevated tumor markers have been reported in the world. Here, we report a case of giant simple hepatic cyst with elevation of multiple serum cancer biomarkers, including protein induced by vitamin K absence-II, cancer antigen (CA) 12-5, and CA19-9.
- Citation: Zhang JW, Peng C, Ye YS, Li W. Giant simple hepatic cyst with multiple elevated serum tumor markers: A case report. World J Gastrointest Surg 2020; 12(12): 549-554
- URL: https://www.wjgnet.com/1948-9366/full/v12/i12/549.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v12.i12.549
Simple hepatic cysts are generally regarded as congenital malformations. This is a relatively common finding in adults, with a reported incidence ranging from 3.5% to 10%[1]. These cysts are usually small in size with abdominal symptoms occurring in less than 20% of the patients. Complications such as mass effect, rupture, hemorrhage, obstructive jaundice, and infection are rare, but may lead to the emergence of symptoms[2]. Overall, simple hepatic cysts are benign and lack serum biomarkers for diagnosis. A giant simple hepatic cyst is uncommon[3,4]. Serum protein induced by vitamin K absence (PIVKA)-II, cancer antigen (CA) 12-5, and cancer antigen CA19-9 are recognized as biomarkers for malignant tumor. These biomarkers are associated with hepatocellular carcinoma and bile duct carcinoma. Here, we report a rare case of giant simple hepatic cyst with marked elevation of serum PIVKA-II, CA12-5, and CA19-9 levels. We have found only one previous report of hepatic cyst with elevation of serum CA19-9[5]. To the best of our knowledge, the present report is the first to describe a case of giant simple hepatic cyst with elevated serum cancer biomarker levels of PIVKA-II, CA12-5, and CA19-9.
An 84-year-old Chinese woman was admitted with gradual abdominal distension.
The patient’s symptoms started 1 year ago. And she had poor appetite and a weight loss of 5 kg within the past 2 wk. She denied any symptoms associated with abdominal pain, fever and chills, nausea and vomiting, etc.
There was no prior history of trauma, hepatitis, allergy, or alcohol or tobacco usage.
No special.
Physical examination showed that she was in medium nutritional status with an icteric appearance. Vital signs were within normal ranges. The abdomen was asymmetrically enlarged, more in the right upper quadrant, without tenderness. Bowel movements occurred about 3-4 times per minute.
Laboratory examination showed significantly increased serum levels of PIVKA-II (> 30000 mAU/mL; reference: < 32 mAU/mL), CA12-5 (428 U/mL; reference: < 35 U/mL), and CA19-9 (51.67 U/mL; reference: < 39 U/mL). Serum aspartate aminotransferase (AST) (97.03 IU/L; reference: < 40 IU/L), alanine aminotransferase (ALT) (64.73 IU/L; reference: < 40 IU/L), total bilirubin (TBIL) (61.19 µmol/L; reference: < 21 µmol/L), and direct bilirubin (DBIL) (36.42 µmol/L; reference: < 3.4 µmol/L) levels were moderately increased. Serum prothrombin time (PT) (33.3 s; reference: 11.0-15.0 s) and activated partial thromboplastin time (aPTT) (54.0 s; reference: 28.0-43.5 s) levels were also elevated slightly. However, serum albumin (ALB) (23.88 g/L; reference: > 35 g/L), prealbumin (PLAB) (17.3 mg/L; reference: 180-390 mg/L), and choline esterase (CHE) levels (1750 IU/L; reference: 3000-13000 IU/L) were significantly low.
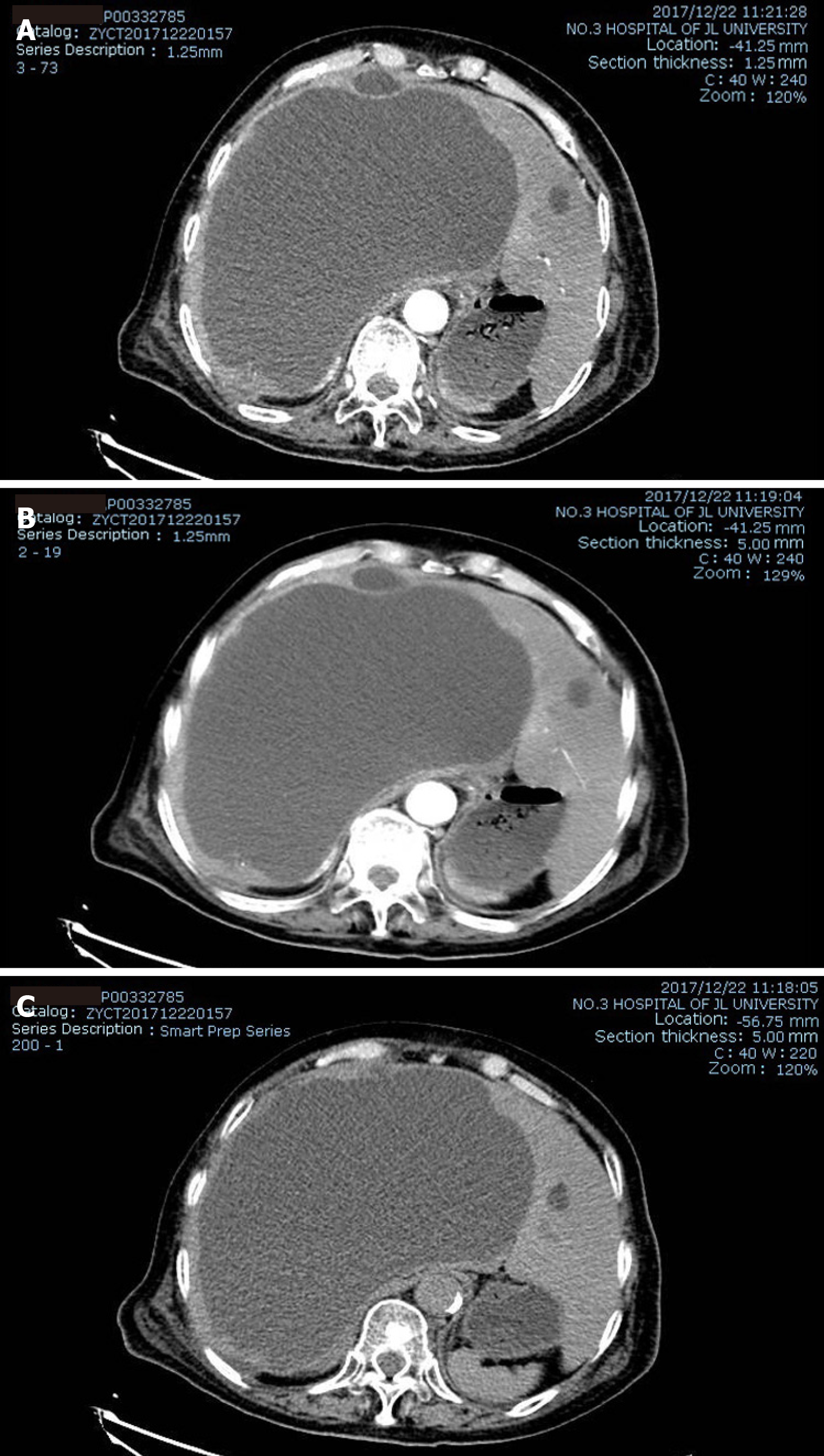
Following an initial abdominal ultrasound examination, an enhanced computed tomography (CT) scan was performed, which revealed multiple round cysts in the liver with clear boundaries. The largest cyst was located in the right lobe of the liver, with mild dilatation of the intrahepatic bile duct, and a size of approximately 20.1 cm × 12.2 cm × 19.6 cm. There was no contrast enhancement in either the arterial or venous phase (Figure 1).
Taking into account all of the patient’s symptoms, signs, and radiology examinations, a clinical diagnosis of simple hepatic cyst was established.
We performed percutaneous drainage on the largest hepatic cyst and injected polycinnamol sclerosing agent into the cyst cavity. Approximately 1150 mL of yellowish green liquid was drained the first day. The cystic fluid was examined, with the results showing some inflammatory cells, but no bacteria, neoplastic cells, or parasites.
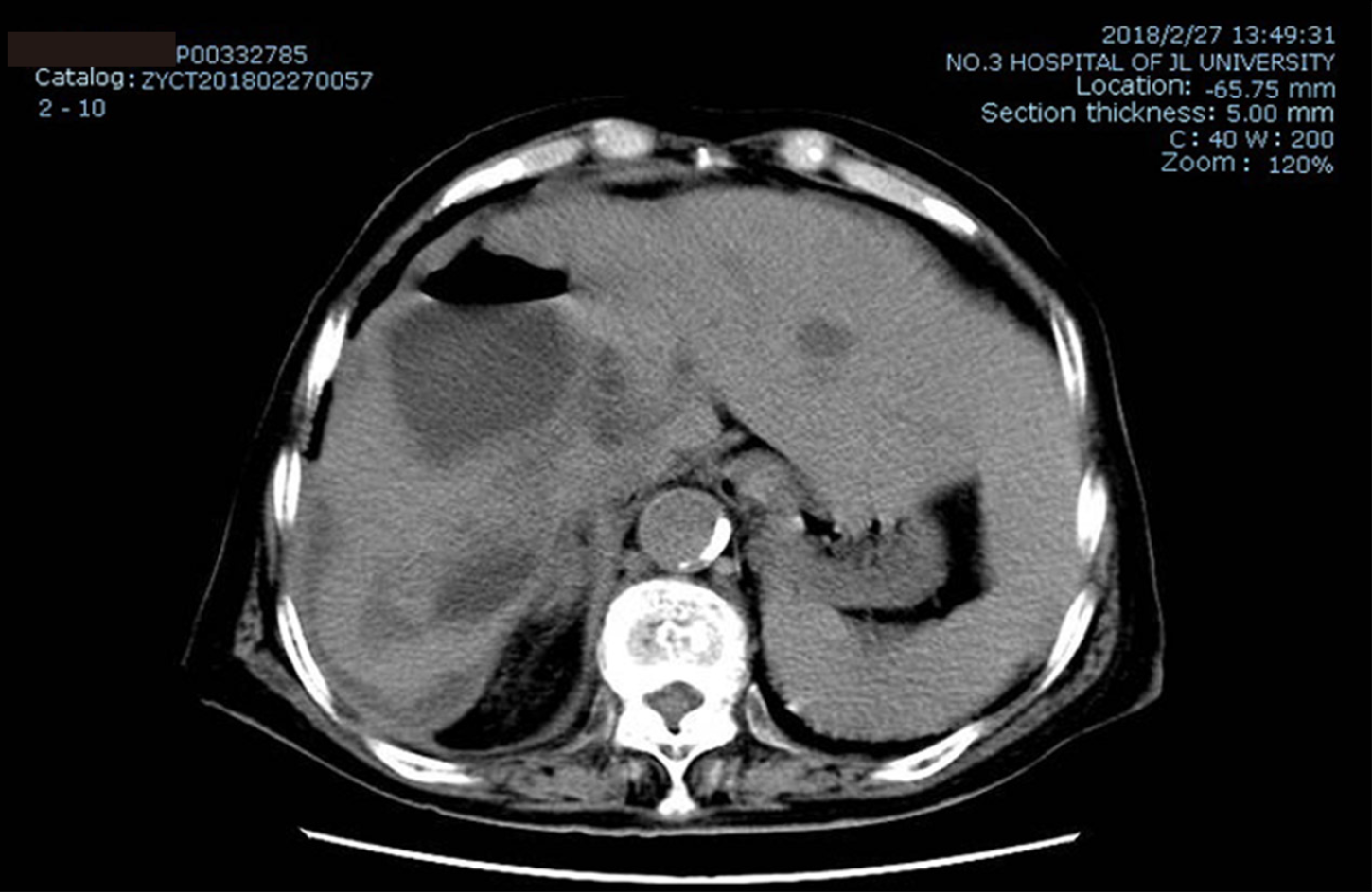
After 1 wk of drainage, the patient's symptoms of abdominal distension and early satiety were gradually eased. Follow-up at 2 mo post cyst drainage found that the size of the cyst had been much reduced, from 20.1 cm × 19.6 cm to 8.7 cm × 6.1 cm (Figure 2), and the serum tests for liver function, coagulating function, PIVKA-II, and CA19-9 revealed that the levels were restored to normal ranges. The serum CA12-5 level remained slightly higher (84.5 U/mL; reference: < 35 U/mL) than normal, but it was significantly reduced from the previous level of 428 U/mL (Table 1).
| Before drainage | After drainage | Reference | |
| Size of the cyst | 20.1 cm × 19.6 cm | 8.7 cm × 6.1 cm | |
| PIVKA-II | > 30000 mAU/mL | Normal | < 32 mAU/mL |
| CA12-5 | 428 U/mL | 84.5 U/mL | < 35 U/mL |
| CA19-9 | 51.67 U/mL | Normal | < 39 U/mL |
Simple hepatic cysts are typically asymptomatic benign tumors of the liver. These cysts usually contain serous fluid, do not communicate with the biliary tree, and do not have separations. PIVKA II, also known as des-gamma-carboxy prothrombin (DCP), is an abnormal prothrombin molecule that is increased in malignant liver disease. During the malignant transformation of hepatocytes, the vitamin K-dependent carboxylase system becomes impaired, which leads to the production of PIVKA II[6,7]. CA12-5, which is derived from the coelomic epithelium including the endometrium, fallopian tubes, ovaries, and peritoneum, is commonly used for the diagnosis of epithelial cell ovarian cancer[8]. CA19-9 is a glycoprotein macromolecule that can be elevated in digestive system tumors and in patients with benign hepatobiliary and gastrointestinal diseases[9,10].
Interestingly, in the present case, there were three tumor markers, including PIVKA-II, CA12-5, and CA19-9, that were elevated and then significantly decreased after decompression. The underlying mechanisms are unclear, and no previous reports have been published on this phenomenon. We propose that the elevation of ALT, AST, and TBIL levels in this patient might have resulted from the mass effect of liver compression by the giant hepatic cyst. This further led to liver function impairment, resulting in decreased levels of serum ALB and CHE as well as poor coagulation function. The giant hepatic cyst of the present patient compressed the intrahepatic bile ducts and caused obstructive jaundice. A similar case was reported by Mehtsun et al[11]. All of the present patient’s laboratory indexes returned to normal ranges after intra-cystic drainage, further confirming that this series of liver function changes was indeed induced by the mass effect of the giant hepatic cyst.
Yanai et al[5] reported a case of simple hepatic cyst with elevated CA19-9, while cases of hepatic cysts with elevated PIVKA-II or CA12-5 have not previously been reported. We speculate that the mechanisms for the elevation of these tumor markers may be as follows: (1) A giant hepatic cyst compresses the liver, causing injury to the hepatocytes, which may lead to secretion of a large amount of PIVKA-II; (2) Some tumor-associated antigens, such as carcinoembryonic antigen (CEA), CA19-9, CA12-5, and CA15-3, are expressed on inflammatory cells[12,13]. We found inflammatory cells in the patient’s cystic fluid, so we conjecture that elevated serum CA19-9 and CA12-5 levels are non-specific and might be due to the effect of inflammation; and (3) Although the exfoliative cytology examination of the patient’s cystic fluid did not have a positive finding, CT scan showed no typical characteristics of serous tumor, and the tumor marker levels were significantly decreased after treatment. Therefore, the possible existence of serous tumors could not be completely ruled out because of lack of pathological examination of the cyst wall.
In summary, to the best of our knowledge, this is the first report of a giant simple hepatic cyst associated with the elevation of serum tumor marker levels of PIVKA-II, CA12-5, and CA19-9. This case revealed that an abnormal elevation of tumor markers is possible in the benign condition of giant hepatic cyst. A significant decline in the levels of these markers can serve as a tool to evaluate the effectiveness of treatment.
The present report identifies an unusual case of giant hepatic cyst with marked elevation of serum tumor marker levels of PIVKA-II, CA12-5, and CA19-9. After treatment, these three serum markers dramatically decreased to normal levels. The mechanisms for the elevation of these tumor markers may be as follows: (1) A giant hepatic cyst compresses the liver, causing injury to the hepatocytes, which may lead to secretion of a large amount of PIVKA-II; and (2) Some tumor-associated antigens, such as CEA, CA19-9, CA12-5, and CA15-3, are expressed on inflammatory cells.
| 1. | Garcea G, Rajesh A, Dennison AR. Surgical management of cystic lesions in the liver. ANZ J Surg. 2013;83:516-522. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 2. | Blonski WC, Campbell MS, Faust T, Metz DC. Successful aspiration and ethanol sclerosis of a large, symptomatic, simple liver cyst: case presentation and review of the literature. World J Gastroenterol. 2006;12:2949-2954. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 46] [Cited by in RCA: 44] [Article Influence: 2.2] [Reference Citation Analysis (2)] |
| 3. | Asuquo M, Nwagbara V, Agbor C, Otobo F, Omotoso A. Giant simple hepatic cyst: a case report and review of relevant literature. Afr Health Sci. 2015;15:293-298. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 4. | Day RJ, Sanchirico PJ, Pfeiffer DC. Giant hepatic cyst as a cause of gastric outlet obstruction. Radiol Case Rep. 2019;14:1088-1092. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 5. | Yanai H, Tada N. A simple hepatic cyst with elevated serum and cyst fluid CA19-9 levels: a case report. J Med Case Rep. 2008;2:329. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 6. | Carr BI, Kanke F, Wise M, Satomura S. Clinical evaluation of lens culinaris agglutinin-reactive alpha-fetoprotein and des-gamma-carboxy prothrombin in histologically proven hepatocellular carcinoma in the United States. Dig Dis Sci. 2007;52:776-782. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 94] [Article Influence: 4.9] [Reference Citation Analysis (1)] |
| 7. | Inagaki Y, Tang W, Makuuchi M, Hasegawa K, Sugawara Y, Kokudo N. Clinical and molecular insights into the hepatocellular carcinoma tumour marker des-γ-carboxyprothrombin. Liver Int. 2011;31:22-35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 104] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 8. | Hirsch M, Duffy J, Davis CJ, Nieves Plana M, Khan KS; International Collaboration to Harmonise Outcomes and Measures for Endometriosis. Diagnostic accuracy of cancer antigen 125 for endometriosis: a systematic review and meta-analysis. BJOG. 2016;123:1761-1768. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 92] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 9. | Liu X, Cai H, Wang Y. Prognostic significance of tumour markers in Chinese patients with gastric cancer. ANZ J Surg. 2014;84:448-453. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 31] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 10. | Zhong W, Yu Z, Zhan J, Yu T, Lin Y, Xia ZS, Yuan YH, Chen QK. Association of serum levels of CEA, CA199, CA125, CYFRA21-1 and CA72-4 and disease characteristics in colorectal cancer. Pathol Oncol Res. 2015;21:83-95. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 63] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 11. | Mehtsun WT, Patel MS, Markmann JF, Hertl M, Vagefi PA. Obstructive jaundice caused by a giant non-parasitic hepatic cyst. Ann Hepatol. 2015;14:267-269. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 12. | Szekanecz E, Sándor Z, Antal-Szalmás P, Soós L, Lakos G, Besenyei T, Szentpétery A, Simkovics E, Szántó J, Kiss E, Koch AE, Szekanecz Z. Increased production of the soluble tumor-associated antigens CA19-9, CA125, and CA15-3 in rheumatoid arthritis: potential adhesion molecules in synovial inflammation? Ann N Y Acad Sci. 2007;1108:359-371. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 44] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 13. | Liu CC, Yang H, Zhang R, Zhao JJ, Hao DJ. Tumour-associated antigens and their anti-cancer applications. Eur J Cancer Care (Engl). 2017;26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 49] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/Licenses/by-nc/4.0/
Manuscript source: Unsolicited manuscript
Corresponding Author's Membership in Professional Societies: American Society of Transplantation; The International Society for Experimental Microsurgery; The American Association of Immunologist; Transplantation Immunology Branch, Chinese Society for Immunology, China; Hepatobiliary-Pancreatic Surgery Committee of Chinese Research Hospital Association; Hepatocellular Cancer Specialist Committee, Chinese Medical Association; Digestive Surgery Committee of Chinese Research Hospital Association.
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Pfeiffer DC S-Editor: Gao CC L-Editor: Wang TQ P-Editor: Li JH