©The Author(s) 2025.
World J Gastrointest Surg. Dec 27, 2025; 17(12): 113029
Published online Dec 27, 2025. doi: 10.4240/wjgs.v17.i12.113029
Published online Dec 27, 2025. doi: 10.4240/wjgs.v17.i12.113029
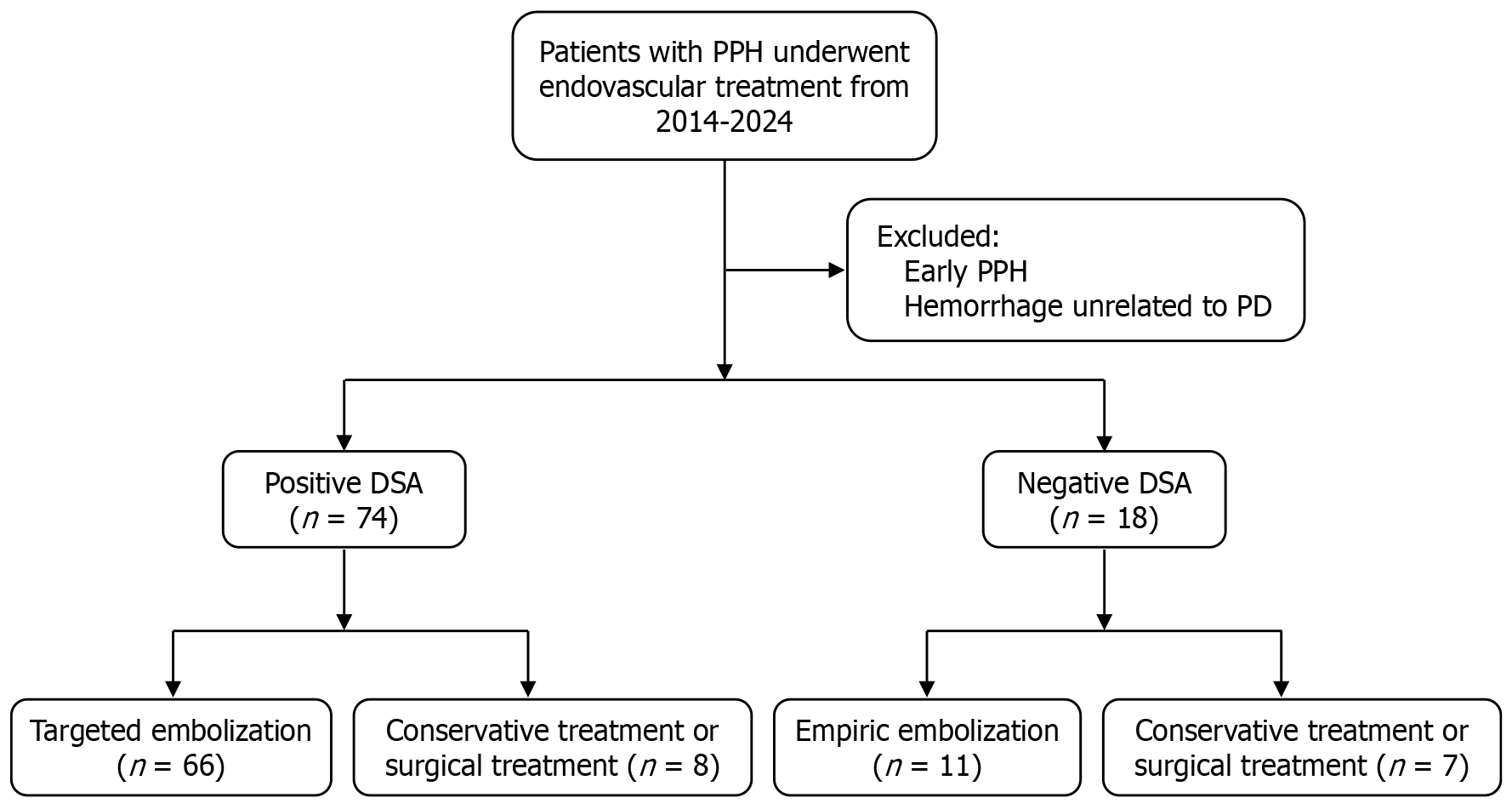
Figure 1 Flow diagram of patient selection and treatment allocation for delayed post-pancreatectomy hemorrhage.
PPH: Post-pancreatectomy hemorrhage; PD: Pancreaticoduodenectomy; DSA: Digital subtraction angiography.
Figure 2 Endovascular management of post-pancreaticoduodenectomy arterial pseudoaneurysms.
A and B: A 61-year-old male patient who underwent radical pancreaticoduodenectomy for bile duct cancer presented with acute hemorrhage from the gastroduodenal artery stump on postoperative day 27. Conventional hepatic angiography demonstrated a large pseudoaneurysm at the gastroduodenal artery stump with active contrast extravasation, associated with a drop in hemoglobin concentration (A); targeted embolization of the common hepatic artery achieved successful hemostasis (B); C and D: A 62-year-old male patient underwent radical pancreaticoduodenectomy combined with segmental resection of the transverse colon for a duodenal malignancy. Postoperatively, he developed intra-abdominal infection and presented with gastrointestinal bleeding on postoperative day 14, receiving both interventional treatment and laparotomy for debridement and drainage. The patient ultimately died from respiratory failure on postoperative day 77. Digital subtraction angiography revealed a pseudoaneurysm of the common hepatic artery (C); after placement of a covered stent in the common hepatic artery, follow-up angiography confirmed complete exclusion of the pseudoaneurysm while preserving distal hepatic arterial flow (D).
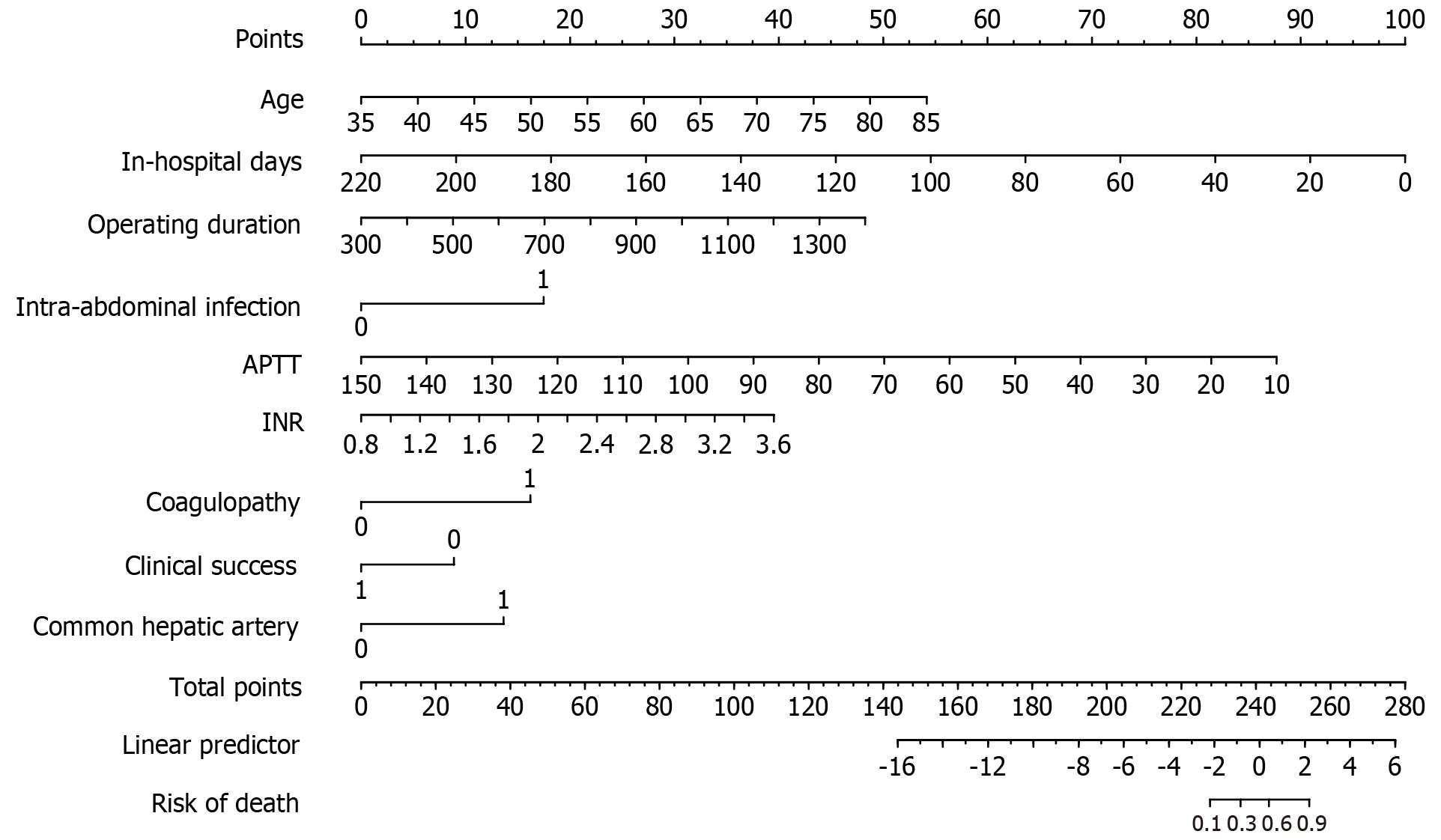
Figure 3 Nomogram for predicting the probability of mortality within 6 months following endovascular treatment for delayed post-pancreatectomy hemorrhage.
Locate the corresponding value on the horizontal axis of age, draw a vertical line upward on this horizontal axis to determine the points obtained for this patient, and repeat this process for the horizontal axis of other predictors. Then, sum the points of the nine parameters to calculate the total points. Find its position on the horizontal axis of total points and draw a vertical line downward to determine the risk of mortality within 6 months after endovascular management of delayed post-pancreatectomy hemorrhage. APTT: Activated partial thromboplastin time; INR: International normalized ratio.
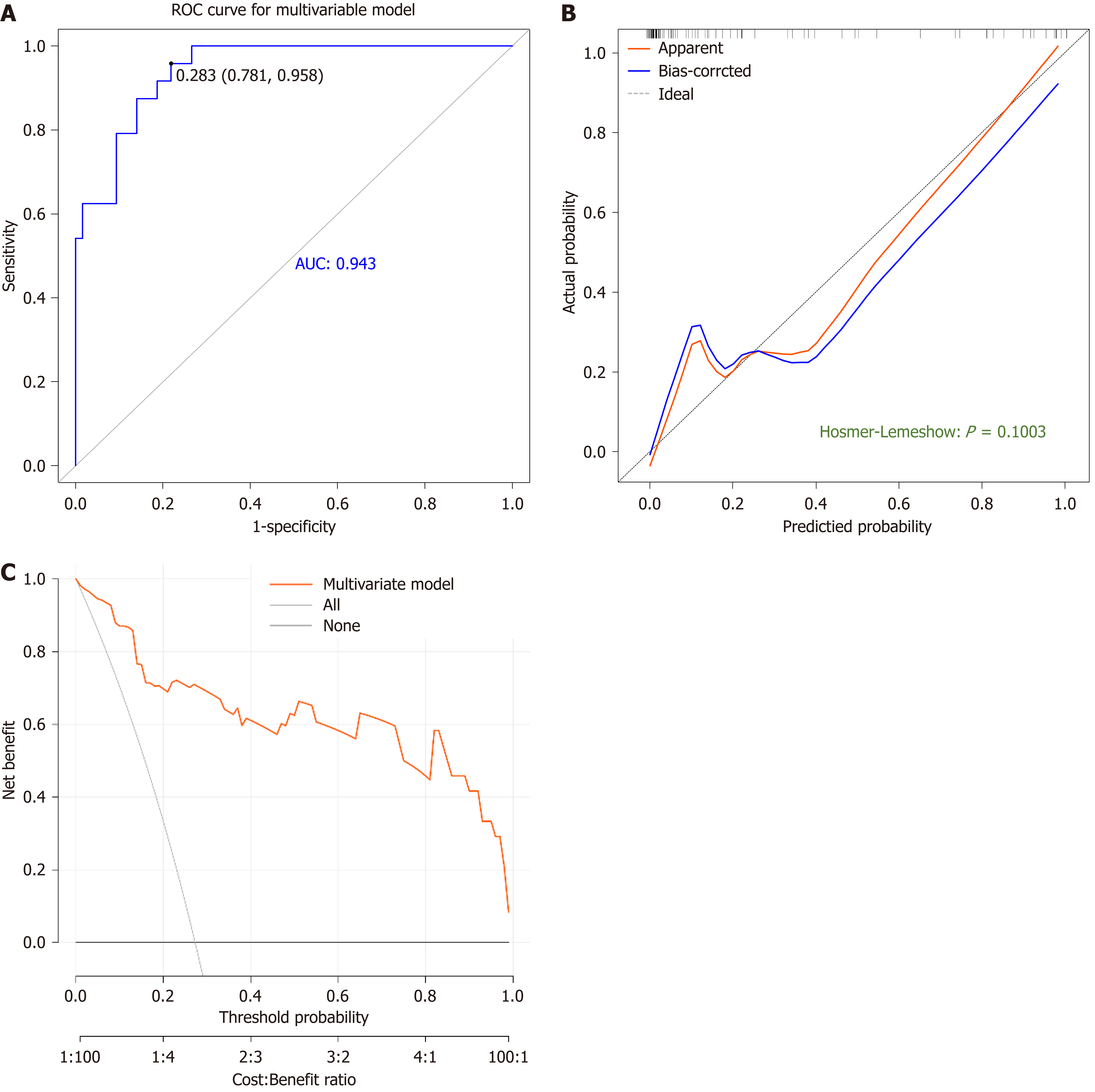
Figure 4 Performance evaluation of the nomogram predicting six-month mortality after endovascular treatment for delayed post-pan
- Citation: Deng DW, Leng AX, He Q, Zhou CG. Nomogram for prediction of six-month mortality following endovascular treatment of delayed post-pancreatectomy hemorrhage. World J Gastrointest Surg 2025; 17(12): 113029
- URL: https://www.wjgnet.com/1948-9366/full/v17/i12/113029.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v17.i12.113029