©The Author(s) 2025.
World J Gastrointest Surg. Dec 27, 2025; 17(12): 112175
Published online Dec 27, 2025. doi: 10.4240/wjgs.v17.i12.112175
Published online Dec 27, 2025. doi: 10.4240/wjgs.v17.i12.112175
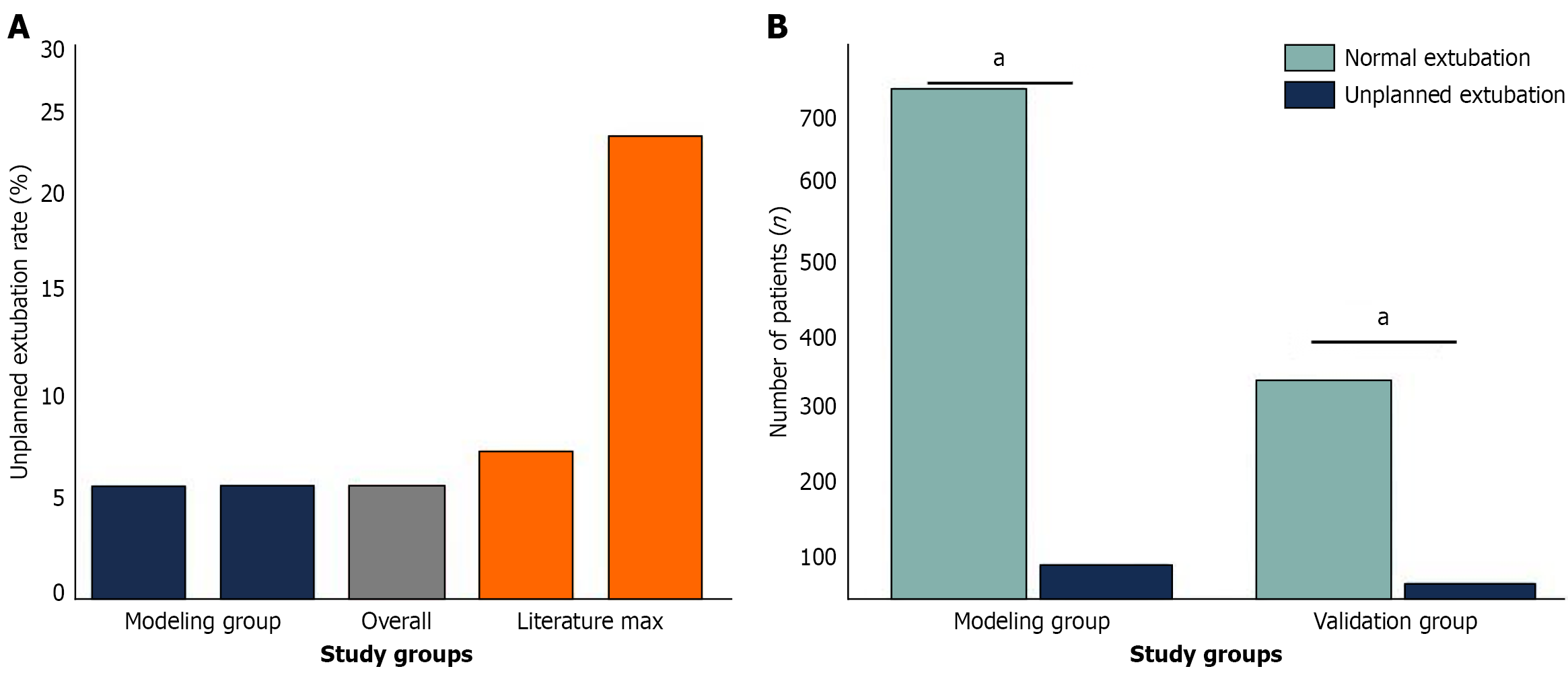
Figure 1 Incidence rates and patient demographics of unplanned extubation across study cohort and literature X-comparison.
This ratio reflected the occurrence rates and patient distribution of unplanned extubation in various study groups, and it suggested that compared with the maximum incidence rate (25%) reported in the literature the modeling group (6.11%) and validation group (6.12%) had a significantly reduced unplanned extubation incidence. A: The comparative incidence rates are summarized; B: The actual number of patients in each group included 687 patients in the model group (42 for unplanned, 645 for normal extubation) and 294 patients in the validation group (18 for unplanned, 276 for normal extubation). aP < 0.05.
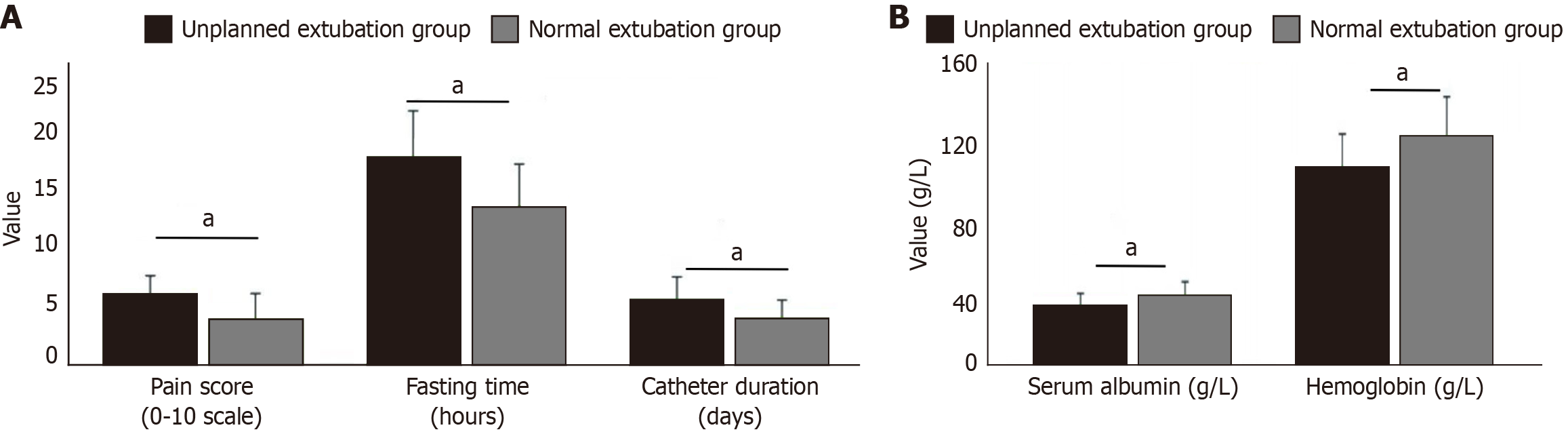
Figure 2 Comparison of clinical manifestations and laboratory parameters of unplanned and spontaneous extubation groups.
A: Pain score, length of fasting, and duration of catheterization; B: Serum albumin levels and hemoglobin levels A (P < 0.05 for all measurements). Patients with unplanned extubation were in poorer condition and with a worse nutrition status than normal extubation. aP < 0.05.
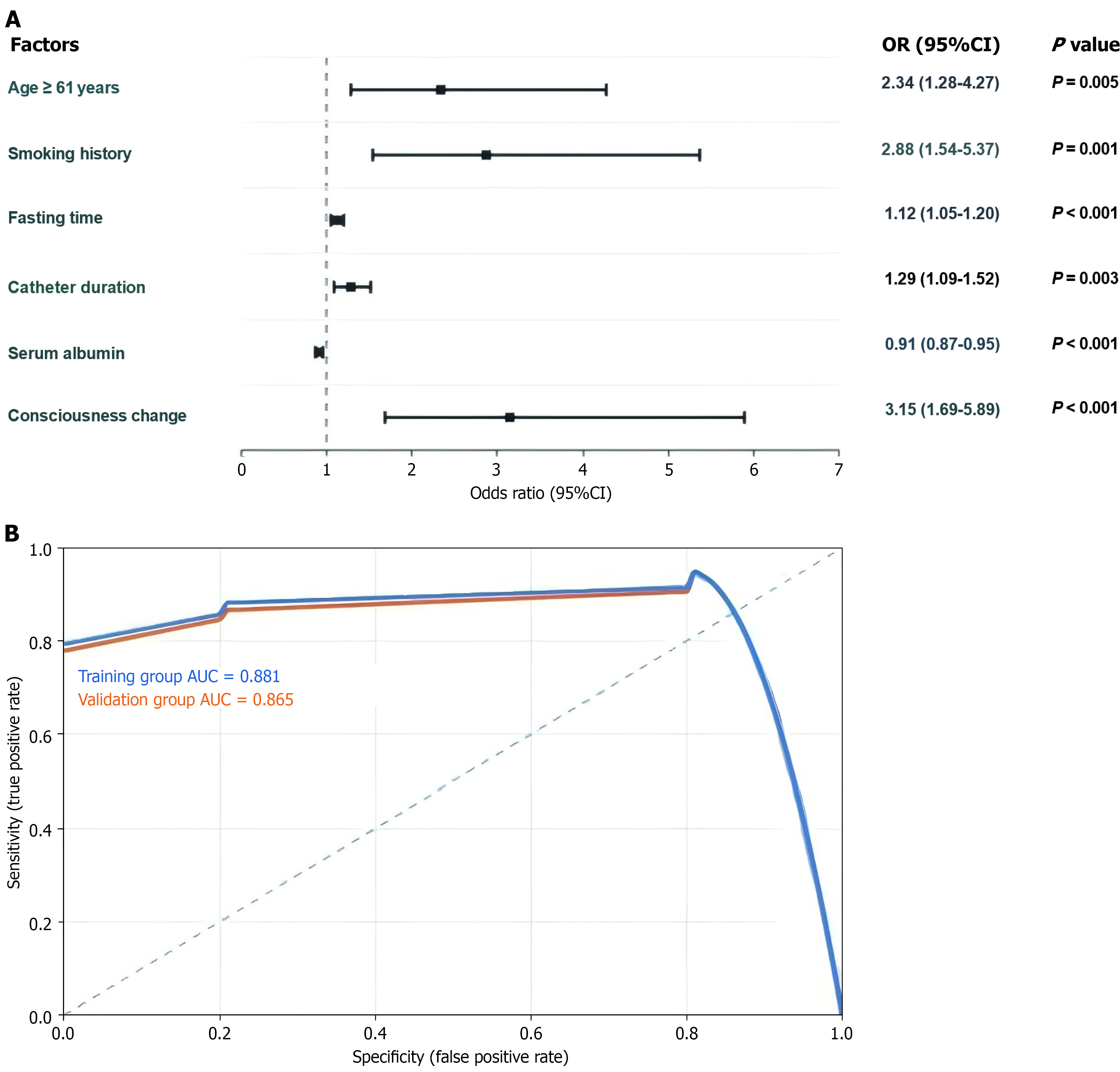
Figure 3 Logistic regression analysis and receiver operating characteristic curve of risk factors for unplanned nasobiliary tube extubation.
This image provides a total assessment of risk factors for unintended extubation of nasobiliary tubes. A: A forest plot of six independent risk factors, including their odds ratios and confidence intervals, among which consciousness change was the riskiest [odds ratio = 3.157], and serum albumin was a protector (odds ratio = 0.91); B: The receiver operating characteristic curve validation that showed a good construct validity with an area under the curve of 0.881 in the training group and 0.865 in the validation group. The model had good discrimination in both studies, and all the risk factors were significant (P < 0.05). The area under the curves was far above the reference line. OR: Odds ratio; CI: Confidence interval; AUC: Area under the curve.
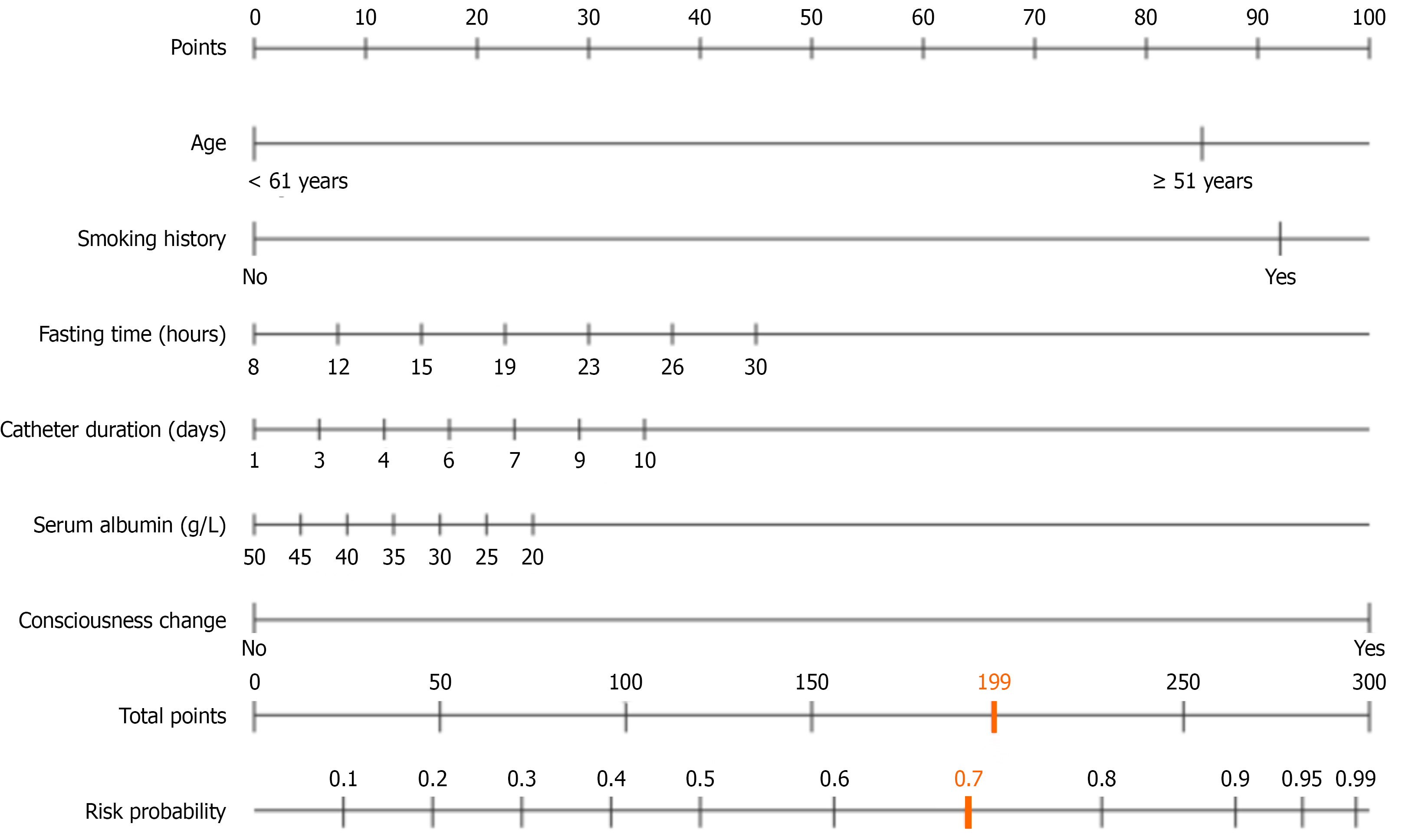
Figure 4 Clinical risk assessment nomogram.
This is a medical risk assessment nomogram that calculates risk probability based on multiple clinical variables including age, smoking history, fasting time, catheter duration, serum albumin levels, and consciousness changes. The patient’s total score of 159 points corresponds to a high-risk threshold of approximately 0.8 (80%) probability for an adverse medical outcome. Orange represents the high-risk cutoff value.
- Citation: Li WJ, Mi N, Huang X, Liu CS, Zhang ST, Liao Y, Yu Y. Predicting unplanned extubation risk in patients with endoscopic nasobiliary drainage. World J Gastrointest Surg 2025; 17(12): 112175
- URL: https://www.wjgnet.com/1948-9366/full/v17/i12/112175.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v17.i12.112175