©The Author(s) 2025.
World J Gastrointest Surg. Nov 27, 2025; 17(11): 109002
Published online Nov 27, 2025. doi: 10.4240/wjgs.v17.i11.109002
Published online Nov 27, 2025. doi: 10.4240/wjgs.v17.i11.109002
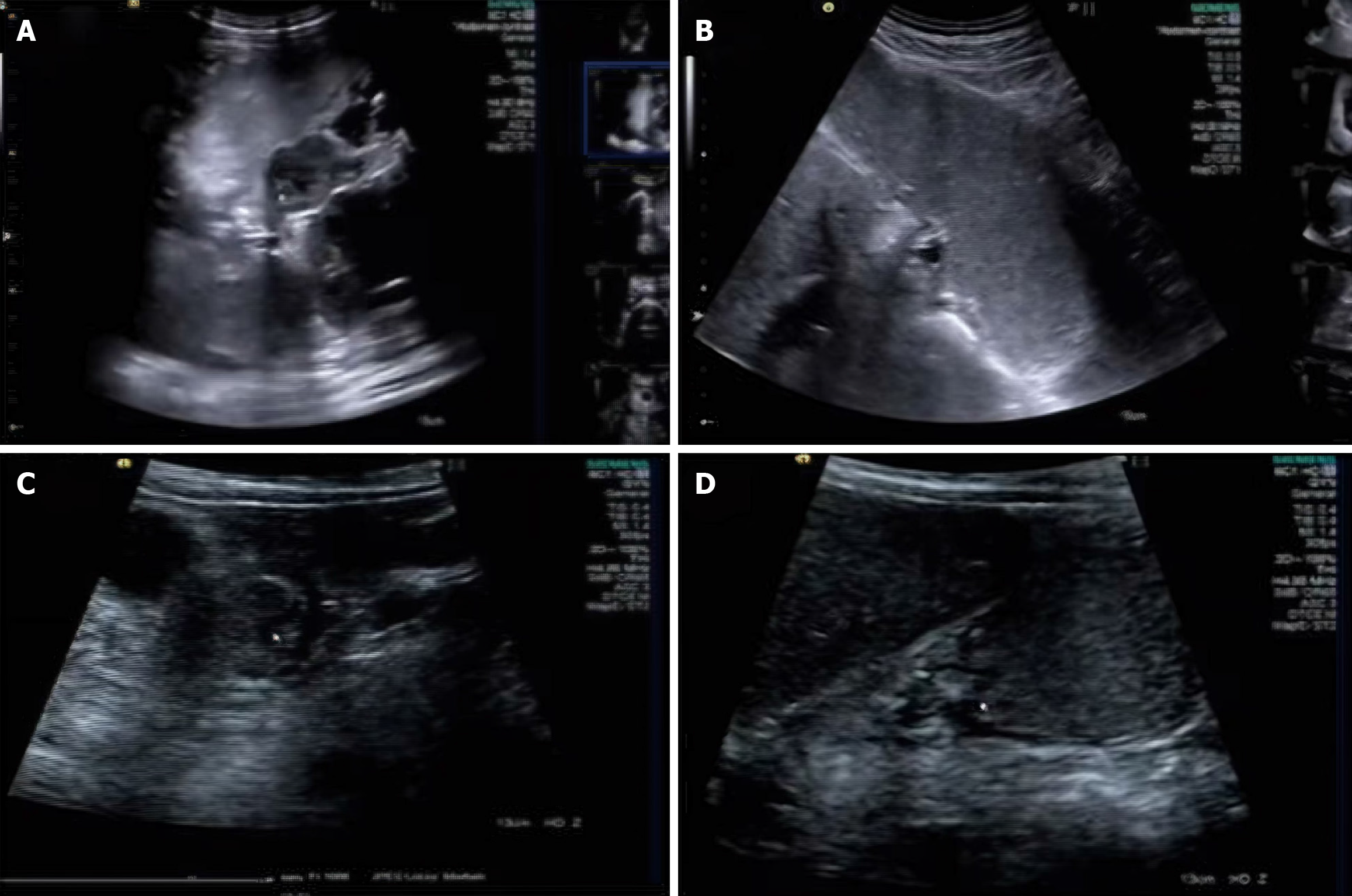
Figure 1 Preoperative gastrointestinal ultrasound localization images.
A: Preoperative gastrointestinal ultrasound localization of tumors in the greater curvature of the stomach; B: Preoperative gastrointestinal ultrasound localization of tumors in the lesser curvature of the stomach; C: Gastric mucosal layer tumor; D: Gastric antral tumor.
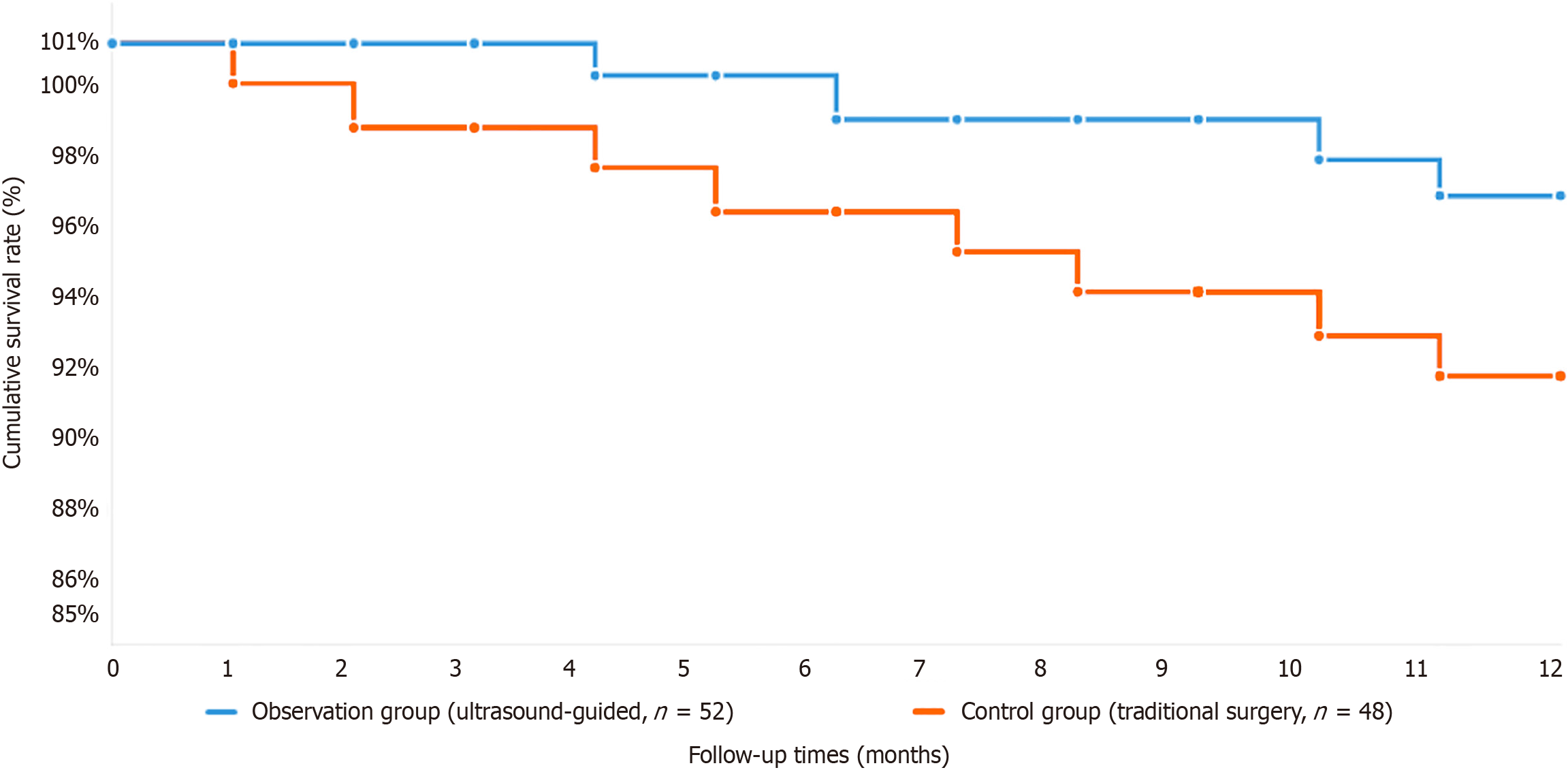
Figure 2 Kaplan-Meier survival analysis comparing 1-year survival rates between ultrasound-guided and conventional surgical approaches in early gastric cancer patients.
The blue line represents the observation group (ultrasound-guided precise localization technology, n = 52), and the red line represents the control group (conventional surgical treatment, n = 48). The analysis revealed superior survival outcomes in the ultrasound-guided group, with a 1-year survival rate of 96.2% compared with 91.7% in the control group, although the difference did not reach statistical significance (P > 0.05, log-rank test).
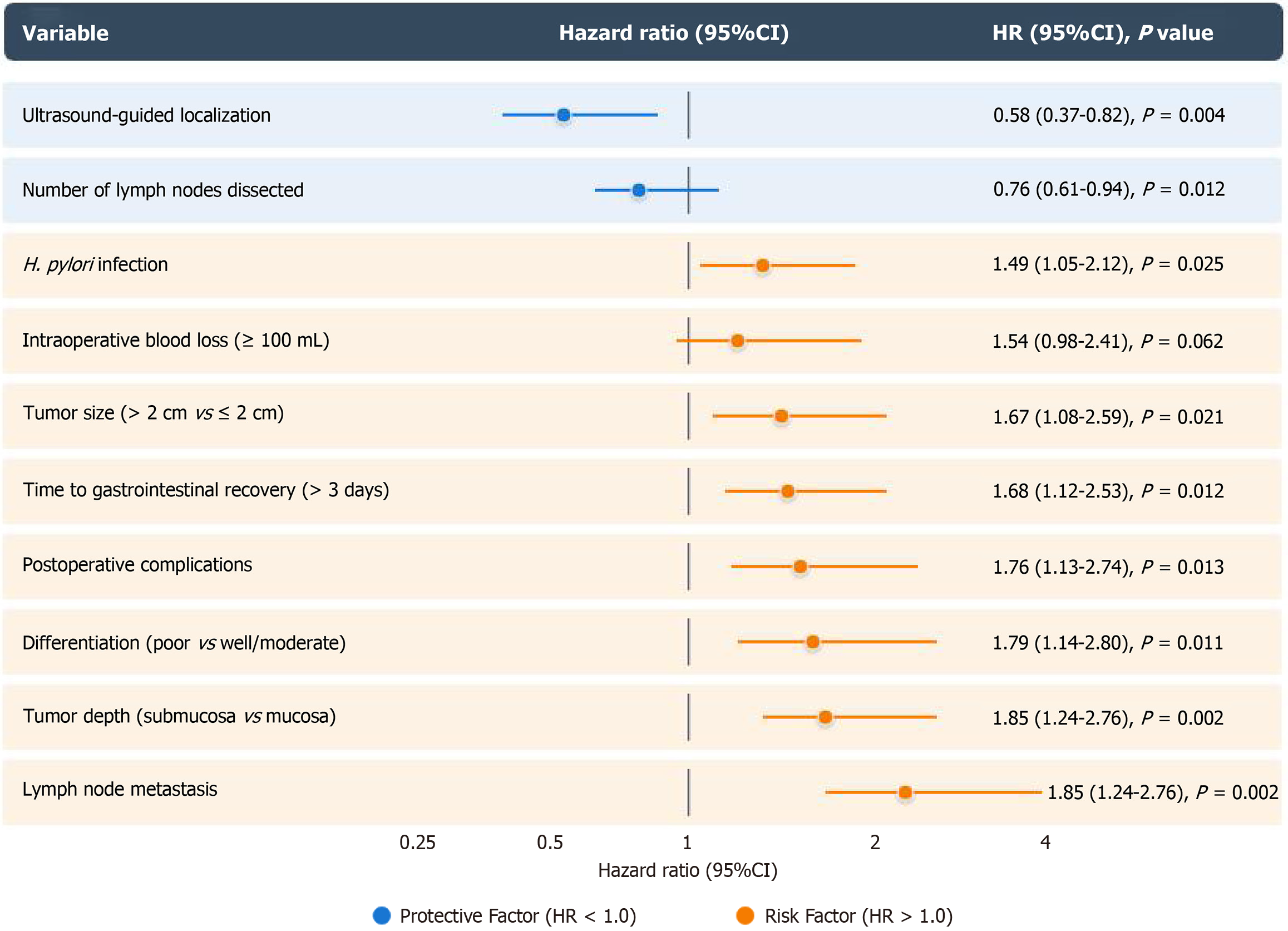
Figure 3 Cox proportional hazards regression analysis of survival.
Ultrasound-guided localization [hazard ratio (HR) = 0.58] and adequate lymph node removal (HR = 0.76) significantly improved survival in early gastric cancer patients. The risk factors included lymph node metastasis (HR = 2.46), deep tumor invasion (HR = 1.85), poor differentiation (HR = 1.79), complications (HR = 1.76), delayed recovery (HR = 1.68), large tumors (HR = 1.67), and Helicobacter pylori infection (HR = 1.49). Ultrasound guidance enhances surgical precision and thoroughness, leading to better patient outcomes. CI: Confidence interval; HR: Hazard ratio; H. pylori: Helicobacter pylori.
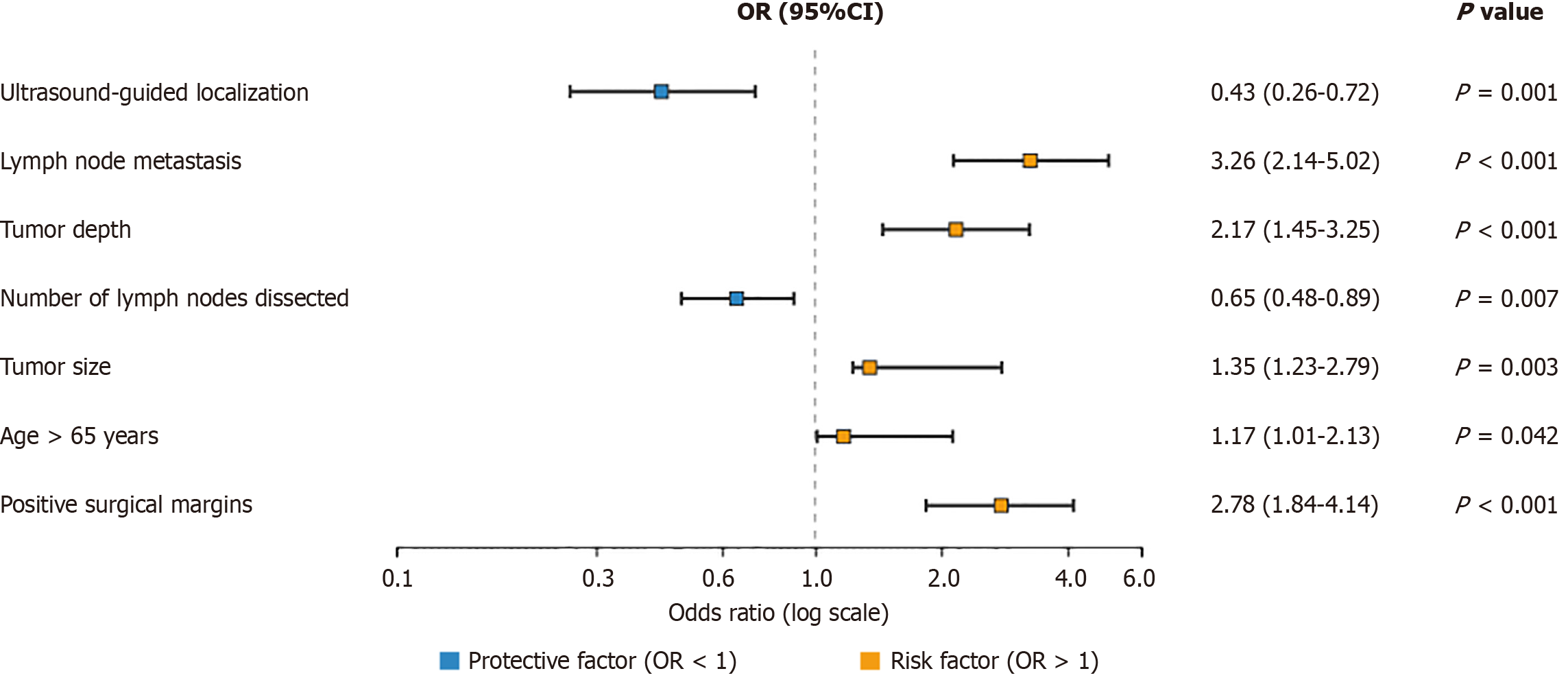
Figure 4 Logistic regression analysis of recurrence risk.
Through logistic regression analysis of factors associated with cancer recurrence, we found that precise ultrasound-guided localization significantly reduced the risk of recurrence [odds ratio (OR) = 0.43, 95% confidence interval (CI): 0.26-0.72; P = 0.001]. Other significant factors included lymph node metastasis (OR = 3.28, 95%CI: 2.14-5.02, P < 0.001), tumor depth (OR = 2.17, 95%CI: 1.45-3.25, P < 0.001), number of lymph nodes dissected (OR = 0.65, 95%CI: 0.48-0.89, P = 0.007), tumor size (OR = 1.85, 95%CI: 1.23-2.79, P = 0.003), age > 65 years (OR = 1.47, 95%CI: 1.01-2.13, P = 0.042), and positive surgical margins (OR = 2.76, 95%CI: 1.84-4.14, P < 0.001). OR: Odds ratio.
- Citation: Chen SY, Hu M, Feng ZB, Xu Q, Wang Y. Application of ultrasound-guided localization technology in early gastric cancer surgery and prognostic analysis. World J Gastrointest Surg 2025; 17(11): 109002
- URL: https://www.wjgnet.com/1948-9366/full/v17/i11/109002.htm
- DOI: https://dx.doi.org/10.4240/wjgs.v17.i11.109002