Published online Apr 15, 2017. doi: 10.4239/wjd.v8.i4.135
Peer-review started: November 29, 2016
First decision: January 16, 2017
Revised: February 9, 2017
Accepted: February 28, 2017
Article in press: March 2, 2017
Published online: April 15, 2017
Processing time: 137 Days and 21 Hours
Foot infection is a well recognized risk factor for major amputation in diabetic patients. The osteomyelitis is one of the most common expression of diabetic foot infection, being present approximately in present in 10%-15% of moderate and in 50% of severe infectious process. An early and accurate diagnosis is required to ensure a targeted treatment and reduce the risk of major amputation. The aim of this review is to report a complete overview about the management of diabetic foot osteomyelitis. Epidemiology, clinical aspects, diagnosis and treatment are widely described according to scientific reccomendations and our experience.
Core tip: Diabetic foot osteomyelitis is a current topic in the field of diabetic foot. Bone infection is a recognized risk factor for minor and major amputation. An accurate description about the diagnosis and treatment is useful to help physicians in the management of osteomyelitis in patients affected by diabetic foot ulcers.
- Citation: Giurato L, Meloni M, Izzo V, Uccioli L. Osteomyelitis in diabetic foot: A comprehensive overview. World J Diabetes 2017; 8(4): 135-142
- URL: https://www.wjgnet.com/1948-9358/full/v8/i4/135.htm
- DOI: https://dx.doi.org/10.4239/wjd.v8.i4.135
Approximately 60% of diabetic foot ulcers (DFUs) are complicated by infection[1]. In more than two-thirds of the cases, infection is the main cause for major lower limb amputation in diabetic patients with foot ulceration[2-5]. Infections may complicate DFUs in both neuropathic and ischemic ulcers.
However, the simultaneous presence of peripheral arterial disease (PAD) and infection influence the evolution of DFUs, increasing the risk of non-healing and major amputation[1]. Therefore, in the case of diabetic foot infection (DFI) and limb ischemia, , it is mandatory an early performing revascularization to allow an adequate blood flow in the area of the infection.
Even if a large variety of bacteria may colonize foot ulcers, infection is considered only if an inflammatory reaction develops due to the interaction between bacteria and host tissues. Colonization is usually limited to skin surface, while infection is generally characterized by the involvement of subcutaneous or deepest tissues. The severity of infection is related to location, depth (fascia, muscles, tendons, joints or bone), presence of necrosis and/or gangrene.
The diagnosis of infection is usually clinical while the microbiological characterization allows to detect the bacteria involved and drive the targeted antibiotic treatment.
Gram positive bacteria as staphylococcus aureus are the most involved in DFI. Nowadays, the resistance to antibiotics is increasing in diabetic population and multi-resistant organisms (MDRO) are common in DFI. Hospitalization, surgical procedures and long antibiotic therapy induce the development of MDRO or methicillin-resistant Staphylococcus aureus (MRSA)[6-8]. Osteomyelitis is a common DFUs infection, being present in 10%-15% of moderate and in 50% of severe infections[9]. The ulcers complicated by osteomyelitis often require surgical treatments and a long antibiotic therapy too[10-12].
Osteomyelitis is usually due to non-healing ulcers and it is associated with high risk of major amputation[13-15].
Diabetic foot osteomyelitis (DFO) is mostly the consequence of a soft tissue infection that spreads into the bone, involving the cortex first and then the marrow. The possible bone involvement should be suspected in all DFUs patients with infection clinical findings, in chronic wounds and in case of ulcer recurrence.
Osteomyelitis can affect any bone but most frequently the forefoot (90%), followed by the midfoot (5%) and the hindfoot (5%). Forefoot have a better prognosis than midfoot and hindfoot osteomyelitis. Above the ankle amputation risk is significantly higher for hindfoot (50%), than midfoot (18.5%) and forefoot (0.33%)[16-18]. An early and accurate diagnosis is required to ensure an effective treatment and reduce the risk of minor and major amputation[19,20].
The microorganisms involved in DFI show a various epidemiology depending on the characteristics of the patient, the clinical risk factors, the wounds (extension and depth) and the microenvironment.
The epidemiology of osteomyelitis reflects the one found in soft tissue infections, rarely mono-microbial and more often poly-microbial. S. aureus (up to 50% of cases), S. epidermidis (about 25%), Streptococci (about 30%) and Enterobacteriaceae (up to 40%) are the most commonly detected bacteria in DFO[21,22]. Among the Gram negative, Escherichia coli, Klebsiella pneumoniae and Proteus, are the most common microorganism followed by Pseudomonas aeruginosa. The rate of anaerobes is usually low[21,22]. Also DFO show an increased MDRO mainly MRSA or extended-spectrum of beta-lactamase-producing[6-8]. The multi-drug resistance is a current topic for clinicians with significant influence on antibiotic approach.
The diagnosis should be first based on clinical signs of infection supported by laboratory, microbiological and radiological evaluation. However, the diagnosis remains a challenge and DFO is often not recognized easily in its initial phase.
Infected wounds usually show purulent secretions or at least two signs of inflammation (swelling, erythema, blood serum secretion or simply blood with or without bone fragments)[14]. However, DFO can occur without any local sign of inflammation. Systemic symptoms such as fever and malaise are rare, especially in case of chronic osteomyelitis.
Various clinical findings can help clinicians in detecting bone infection. Two specific clinical signs are predictive of osteomyelitis. The first is the width and depth of the foot ulcer. An ulcer larger than 2 cm2 has a sensitivity of 56% and a specificity of 92%. Deep ulcers (> 3 mm) are more easily associated with an underlying osteomyelitis than superficial ulcers (82% vs 33%)[23].
A second diagnostic criterion to detect DFO is the “probe-to-bone test” (PTB). PBT is performed probing the ulcer area with a sterile blunt probe. If the probe reaches the bone surface the PTB is considered positive. In a study involving 75 diabetic patients, PTB showed a sensitivity of 66%, a specificity of 85% and a positive predictive value of 89%[24]. The same test, evaluated in a subsequent prospective study of 1666 diabetic patients and compared with the culture of infected bones, was found to have a sensitivity of 87%, a specificity of 91%, a positive predictive value of only 57% and a negative predictive value of 98%[25].
Therefore, in the presence of infected ulcers, a positive PTB test is highly suggestive of osteomyelitis, but a negative test does not exclude it. Instead, in presence of an ulcer without clinical signs of infection, a positive test may be not specific for osteomyelitis while a negative PBT test should exclude a bone infection[26].
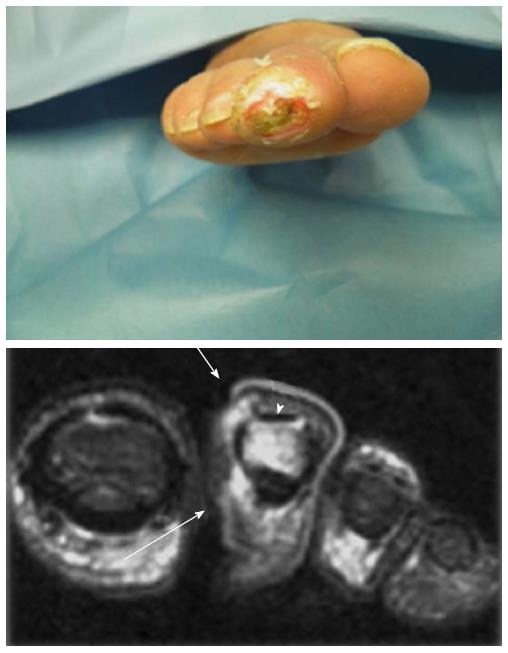
The combination of the PTB test with X-ray improve the sensitivity and specificity in the diagnosis of DFO[27,28]. Bone infection is also considered in case of visible or exposed bone or discharge of bone fragments (Figures 1 and 2).
Serum inflammatory markers as white blood cells (WBC), C-reactive protein, erythrocyte sedimentation rate (ESR) and procalcitonin (PCT) are usually higher in DFO than soft-tissue infections. However, WBC and procalctitonin may be negative while ESR > 60 mm/h and/or CRP > 3.2 mg/dL in the presence of an ulcer deeper than > 3 mm are significantly predictive of DFO[29]. Furthermore, WBC, CRP and PCT values return to their normal range approximately in three weeks after the treatment in both of soft-tissue and bone infection, while ESR usually remains high only in case of osteomyelitis[30].
Radiological tests are usually required to detect bone involvement in case of suspect osteomyelitis without clinical signs of infection, to confirm the clinical suspicion and detect the affected bone/bones and to distinguish DFO from soft tissue infection. X-ray is the first instrumental tool although it’s arduous to detect the infectious process during the initial phase. Clear signs related to osteomyelitis are generally not evident until 30%-50% of the bone has not been involved; usually this condition happens after 2-3 wk. X-ray DFO imaging are usually characterized by osteopenia, erosion of cortical bone, cortical lysis, osteolysis, periosteal thickening, bone sequestration[31,32]. Radiological criteria of bone healing include: Well-organized consolidation of periosteum, reduction of bone lucency, reduction of pathological fractures related to bone infection, neoformation of mineralized bone in the areas destroyed by the infection[33].
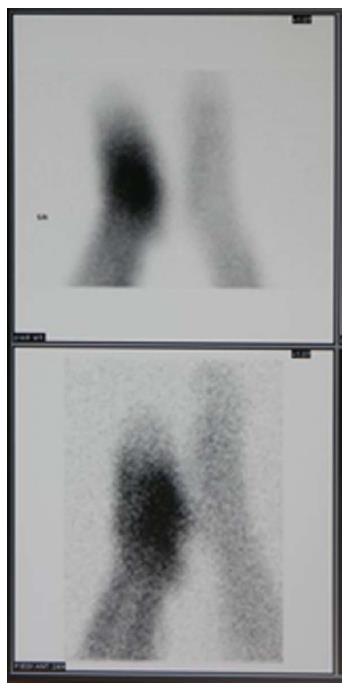
Scintigraphic examinations are more sensitive than X-ray, especially during the earliest stage of bone infection and the follow-up. However, the common limitation is the low specificity in the discrimination between soft tissues and bone infection[34]. The specificity of leucocyte scan is better than triple-phase bone scan even if the spatial resolution can be a limiting factor. However, labeled leukocyte imaging are more useful than bone scan for diagnosis, evaluation of bone affected and follow-up during medical treatment[35,36].
More recently, it has been shown that combined 99mTc white blood cell-labeled single-photon emission computed tomography and computed tomography (99mTc WBC labelled-SPECT/CT) imaging provide good spatial resolution with the three-dimensional CT-scan images and WBC uptake intensity yielding more information about the location and extension of infection[37,38]. Particularly, the role of 99mTc WBC labeled-SPECT/CT has been positively evaluated to identify the complete resolution of infection during the follow-up of patients treated by antibiotics[39] (Figure 3).
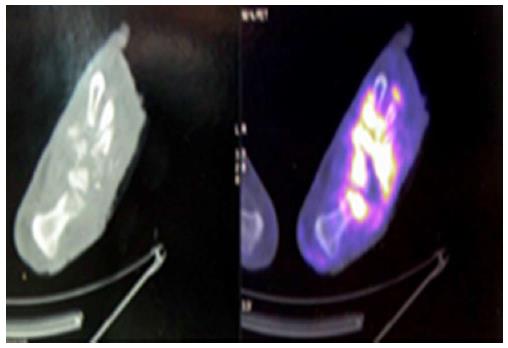
The positron emission tomography-computed tomography (PET/CT) with fluorine-18-fluorodeoxyglucose (18F-FDG) is an excellent hybrid imaging that can be used in the diagnosis of DFO and to distinguish bone from soft tissues infections. 18F-FDG is a non-specific tracer to evaluate intracellular glucose metabolism; its uptake in increased in the areas of infection and inflammation[40-42] (Figure 4).
Magnetic resonance imaging (MRI) with gadolinium shows very high sensitivity (90%), and specificity (85%) in the diagnosis of DFO. The gadolinium uptake allows to distinguish between soft tissues and bone better than CT and scintigraphic methods[43,44]. The typical changes in the bone marrow predictive for osteomyelitis are low signal intensity on T1-weighted sequences and high signal intensity on T2-weighted sequences. These findings may be already evident 3 d after the onset of infection. The major limit is the reduced resolution in the evaluation of cortical bone that does not allow to highlight few cases of infection such as osteitis or to distinguish other causes of bone injury[45,46].
The guidelines suggest that the diagnosis of DFO include the combination of different diagnostic tests, such as PTB, serum inflammatory markers, X-ray, MRI or radionuclide scanning. X-ray should be always the first imaging evaluation; when more specific imaging are required, MRI is the first choice while white blood cell-labelled radionuclide scan, SPECT/CT and 18F-FDG PET/CT are used only if MRI is contraindicated[21,22] (Figures 5-7).
The gold standard for the diagnosis of osteomyelitis is the bone biopsy which provides histological and microbiological findings[21,22]. Histological criteria are: Bone erosion, marrow edema, fibrosis, necrosis, presence of inflammatory cells (both acute and chronic), seizure. Furthermore, the bone biopsy allows to identify precisely the bacteria involved in the infectious process and to evaluate the susceptibility to antibiotic therapy. The bone can be removed by a percutaneous approach through a not infected skin or during the open surgical procedures. In case of bone infection, superficial swab shows a low sensitivity, in fact a reliable correspondence between bacteria isolated form bone biopsy and swab culture is approximately of 38%[47]. Therefore, superficial swab should not be used in case of DFO. Bone biopsy is the most accurate test (preferably after 10 d of antibiotic suspension) even if in several cases it is not technically feasible. However, a recent study showed that the pathogens isolated from culture of deep tissues (removed from the area closest to the bone) are very similar to those obtained from bone biopsy (74.3% vs 82.8%)[48].
The treatment of DFO remains a hot topic in the field of diabetic foot. Over the years the most debated theories have been surgical or antibiotic therapy as first approach.
Nowadays the treatment of osteomyelitis is not completely standardized and evaluated case by case. Therefore, the guidelines broadly recommend the specific conditions for surgical or medical approach combined with conservative surgery. Conservative surgery means usually a procedure in which only the infected bone and the non-viable soft tissues are removed without any amputation[16].
Tan et al[49] have shown that an aggressive surgical approach with minor amputation reduces the risk of major amputation above the ankle and reduce the length of hospitalization and associated costs. The Authors report that forefoot amputation reduces the risk of major amputation in comparison to medical therapy performed for 3 d[49]. However, antibiotic therapy was performed only for 3 d and it is well known that DFO can require long antibiotic therapy.
Although an aggressive surgical approach could be mandatory under some circumstances, retrospective studies have shown that conservative treatment associated with prolonged antibiotic therapy is effective to promote wound healing and reduce the risk of major amputation and of ulcers recurrence[16,50,51].
Ha Van et al[50] have compared the conservative surgical treatment, defined as the resection of limited part of infected bone (phalanx and/or metatarsal head), associated with antibiotic therapy against antibiotic therapy alone. The conservative approach was more effective in terms of ulcer healing (78% vs 57%) and healing time (181 ± 30 d vs 462 ± 98 d, P < 0.008) compared to antibiotic therapy alone. Furthermore, the length of antibiotic therapy was significantly reduced in the group treated by conservative approach than the group treated by antibiotic alone (111 ± 121 d vs 246.9 ± 232 d, P < 0.007)[50].
Antibiotic therapy is widely used in association to surgical approach, both for minimal or extended procedures; however, several studies have reported many cases of DFO treated only by antibiotic therapy without surgery. Some Authors have reduced the role of surgery to treat bone infection, mainly in case of chronic osteomyelitis[52-54].
A recent prospective randomized clinical study has compared conservative surgery (removal of bone without amputation of any part of the foot) and antibiotic therapy alone. Severe infection, patients with PAD and severe co-morbidity were excluded. Osteomyelitis were located in the forefoot. The surgical group received empirical antibiotic therapy after the procedure. The group treated by antibiotics alone received for 90 d a targeted treatment according to the microbiological culture of deep soft tissues localized near the bone. The patient were followed for 12 mo after wound healing The rate of wound healing and healing time for respectively surgical and medical groups was similar (86.3% vs 75%) and (6 wk vs 7 wk). Only 16.6% of subjects treated by antibiotics alone required a secondary surgical approach. No patient received major amputation[55].
Also the optimal duration of antibiotic therapy is not completely defined. The Infectious Disease Society of America (IDSA) considers 4-6 wk adequate when the infected bone is not completely removed by surgery while at least 3 mo in case of antibiotic therapy alone[21]. However, the recent report of International Working Group of Diabetic Foot (IWGDF) suggested 6 wk of antibiotic therapy if the infected bone was not removed by surgery and no more than a week if infected bone was resected[22]. Lately, the aim is to reduce the duration of antibiotic therapy. In fact, prolonged use of antibiotics increases the risk of bacterial resistance, side effects and costs.
A prospective randomized study compared two groups of not ischemic patients with DFUs on the forefoot complicated by osteomyelitis treated with antibiotic therapy respectively for 6 or 12 wk. At the beginning antibiotic therapy was empirical and then driven by microbiological results. Sixty-six percent of patients resolved the osteomyelitis and there was not a significant difference between the two groups. Furthermore, the group treated for 12 wk showed more side effects than the group treated for six weeks[56].
A significant aspect is to define the resolution of bone infection. Nowadays, there are no tests correlated to long-term resolution of osteomyelitis. The IWGDF suggest that a decrease of serum inflammatory markers, especially ESR, associated with the resolution of soft tissue infection, healing and positive evolution of radiological signs can be used to stop antibiotic therapy.
Chronic osteomyelitis is associated with a high percentage of recurrence despite a long antibiotic therapy. The rate of infection recurrence is approximately of 30%[31,54]. Recurrence might be related to the incomplete resection of infected bone or to resistant microorganisms persistently remaining in their biofilm[57]. The recurrence of DFO has to be considered in case of ulcer reappearance within 12 mo after the first healing. Furthermore, recurrent foot ulceration can promote the reappearance of bone infection. Adequate prevention is mandatory.
The appropriate management of DFO is closely based on both the severity of infection and patient’s characteristics. Surgical and conservative approach shows advantages in some conditions and disadvantages in other. Several factors can influence the outcome. Among the advantages of surgical therapy there is the complete removal of the infected bone and the reduced duration of antibiotic therapy. On the other side an aggressive approach can lead to an extended tissue loss and it should be done only in patients with an adequate blood perfusion.
Further, the surgical treatment can impair the foot balance. In fact, a partial amputation (such as removal of a ray or a metatarsal head), mainly if associated to a pre-existing peripheral neuropathy, can increase biomechanical impairments of the foot and promote re-ulceration or new ulcerations in different areas.
Armstrong et al[58] have shown that forefoot amputation (toes or rays) reduces the joint mobility and increases the plantar pressures, 10-fold higher than that found in patients without forefoot amputation. Furthermore, increased peak pressure and limited joint mobility are significantly related high risk of re-amputation.
Molines-Barroso et al[59] analyzed the risk factors of re-ulceration in 119 diabetic patients who underwent resection of the metatarsal heads due to osteomyelitis. The rate of re-ulceration was higher in case of 1st and 3rd metatarsal head resection (69% and 52% respectively), followed by the resection of 2nd, 4th and 5th metatarsal head (44%, 25% and 19% respectively). The removal of more than one metatarsal heads was associated with a risk of re-ulceration approximately of 50%. The risk of ulceration transfer was significantly higher in case of 1st metatarsal head resection (P = 0.004)[59]. The main advantages of the medical treatment is to avoid the surgical treatment preserving the foot architecture and biomechanics.
The IDSA guidelines define the four clinical patterns where antibiotic therapy without surgery should be considered: (1) high risk of foot function loss in case of radical resection of infected bone; (2) severe deficiency in foot perfusion without chance of revascularization; (3) infection confined to the forefoot with only a minimal loss of soft tissue; and (4) excessive surgical risk according to patients general conditions. Furthermore, antibiotic therapy should be the first choice in case of small ulcers of the forefoot without bone exposure.
The main disadvantages of medical therapy may be the increased risk of infection recurrence, the long duration that can predispose to side effects and promote antibiotic resistance. According to IWGDF guidance, surgical bone resection is recommended in cases of bone exposure, progressive bone destruction and spreading of infection along the soft tissues[22].
| 1. | Prompers L, Huijberts M, Apelqvist J, Jude E, Piaggesi A, Bakker K, Edmonds M, Holstein P, Jirkovska A, Mauricio D. High prevalence of ischaemia, infection and serious comorbidity in patients with diabetic foot disease in Europe. Baseline results from the Eurodiale study. Diabetologia. 2007;50:18-25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 601] [Cited by in RCA: 658] [Article Influence: 34.6] [Reference Citation Analysis (0)] |
| 2. | Reiber GE, Pecoraro RE, Koepsell TD. Risk factors for amputation in patients with diabetes mellitus. A case-control study. Ann Intern Med. 1992;117:97-105. [PubMed] |
| 3. | Boulton AJ, Vileikyte L, Ragnarson-Tennvall G, Apelqvist J. The global burden of diabetic foot disease. Lancet. 2005;366:1719-1724. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1532] [Cited by in RCA: 1595] [Article Influence: 76.0] [Reference Citation Analysis (0)] |
| 4. | Lavery LA, Ashry HR, van Houtum W, Pugh JA, Harkless LB, Basu S. Variation in the incidence and proportion of diabetes-related amputations in minorities. Diabetes Care. 1996;19:48-52. [PubMed] |
| 5. | Nicolau DP, Stein GE. Therapeutic options for diabetic foot infections: a review with an emphasis on tissue penetration characteristics. J Am Podiatr Med Assoc. 2010;100:52-63. [PubMed] |
| 6. | Eady EA, Cove JH. Staphylococcal resistance revisited: community-acquired methicillin resistant Staphylococcus aureus--an emerging problem for the management of skin and soft tissue infections. Curr Opin Infect Dis. 2003;16:103-124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 7. | Nelson SB. Management of diabetic foot infections in an era of increasing microbial resistance. Curr Infect Dis Rep. 2009;11:375-382. [PubMed] |
| 8. | Eleftheriadou I, Tentolouris N, Argiana V, Jude E, Boulton AJ. Methicillin-resistant Staphylococcus aureus in diabetic foot infections. Drugs. 2010;70:1785-1797. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 99] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 9. | Lipsky BA, Berendt AR, Deery HG, Embil JM, Joseph WS, Karchmer AW, LeFrock JL, Lew DP, Mader JT, Norden C. Diagnosis and treatment of diabetic foot infections. Plast Reconstr Surg. 2006;117:212S-238S. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 154] [Cited by in RCA: 174] [Article Influence: 8.7] [Reference Citation Analysis (1)] |
| 10. | Lipsky BA, Berendt AR, Embil J, De Lalla F. Diagnosing and treating diabetic foot infections. Diabetes Metab Res Rev. 2004;20 Suppl 1:S56-S64. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 65] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 11. | M Embil JM. The management of diabetic foot osteomyelitis. The Diabetic Foot. 2000;3:76-84. |
| 12. | Armstrong DG, Lipsky BA. Advances in the treatment of diabetic foot infections. Diabetes Technol Ther. 2004;6:167-177. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 52] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 13. | Hill SL, Holtzman GI, Buse R. The effects of peripheral vascular disease with osteomyelitis in the diabetic foot. Am J Surg. 1999;177:282-286. [PubMed] |
| 14. | Eneroth M, Larsson J, Apelqvist J. Deep foot infections in patients with diabetes and foot ulcer: an entity with different characteristics, treatments, and prognosis. J Diabetes Complications. 1999;13:254-263. [PubMed] |
| 15. | Mutluoglu M, Sivrioglu AK, Eroglu M, Uzun G, Turhan V, Ay H, Lipsky BA. The implications of the presence of osteomyelitis on outcomes of infected diabetic foot wounds. Scand J Infect Dis. 2013;45:497-503. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 95] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 16. | Aragón-Sánchez FJ, Cabrera-Galván JJ, Quintana-Marrero Y, Hernández-Herrero MJ, Lázaro-Martínez JL, García-Morales E, Beneit-Montesinos JV, Armstrong DG. Outcomes of surgical treatment of diabetic foot osteomyelitis: a series of 185 patients with histopathological confirmation of bone involvement. Diabetologia. 2008;51:1962-1970. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 151] [Cited by in RCA: 162] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 17. | Aragón-Sánchez J, Lázaro-Martínez JL, Hernández-Herrero C, Campillo-Vilorio N, Quintana-Marrero Y, García-Morales E, Hernández-Herrero MJ. Does osteomyelitis in the feet of patients with diabetes really recur after surgical treatment? Natural history of a surgical series. Diabet Med. 2012;29:813-818. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 78] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 18. | Faglia E, Clerici G, Caminiti M, Curci V, Somalvico F. Influence of osteomyelitis location in the foot of diabetic patients with transtibial amputation. Foot Ankle Int. 2013;34:222-227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 54] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 19. | Bonham P. A critical review of the literature: part I: diagnosing osteomyelitis in patients with diabetes and foot ulcers. J Wound Ostomy Continence Nurs. 2001;28:73-88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (1)] |
| 20. | Bonham P. A critical review of the literature: part II: antibiotic treatment of osteomyelitis in patients with diabetes and foot ulcers. J Wound Ostomy Continence Nurs. 2001;28:141-149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 21. | Lipsky BA, Berendt AR, Cornia PB, Pile JC, Peters EJ, Armstrong DG, Deery HG, Embil JM, Joseph WS, Karchmer AW. 2012 Infectious Diseases Society of America clinical practice guideline for the diagnosis and treatment of diabetic foot infections. Clin Infect Dis. 2012;54:e132-e173. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1015] [Cited by in RCA: 1206] [Article Influence: 86.1] [Reference Citation Analysis (0)] |
| 22. | Lipsky BA, Aragón-Sánchez J, Diggle M, Embil J, Kono S, Lavery L, Senneville É, Urbančič-Rovan V, Van Asten S, Peters EJ. IWGDF guidance on the diagnosis and management of foot infections in persons with diabetes. Diabetes Metab Res Rev. 2016;32 Suppl 1:45-74. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 338] [Cited by in RCA: 363] [Article Influence: 36.3] [Reference Citation Analysis (0)] |
| 23. | Lipsky BA. Osteomyelitis of the foot in diabetic patients. Clin Infect Dis. 1997;25:1318-1326. [PubMed] |
| 24. | Grayson ML, Gibbons GW, Balogh K, Levin E, Karchmer AW. Probing to bone in infected pedal ulcers. A clinical sign of underlying osteomyelitis in diabetic patients. JAMA. 1995;273:721-723. [PubMed] |
| 25. | Lavery LA, Armstrong DG, Peters EJ, Lipsky BA. Probe-to-bone test for diagnosing diabetic foot osteomyelitis: reliable or relic? Diabetes Care. 2007;30:270-274. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 180] [Cited by in RCA: 152] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 26. | Morales Lozano R, González Fernández ML, Martinez Hernández D, Beneit Montesinos JV, Guisado Jiménez S, Gonzalez Jurado MA. Validating the probe-to-bone test and other tests for diagnosing chronic osteomyelitis in the diabetic foot. Diabetes Care. 2010;33:2140-2145. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 71] [Cited by in RCA: 66] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 27. | Aragón-Sánchez J, Lipsky BA, Lázaro-Martínez JL. Diagnosing diabetic foot osteomyelitis: is the combination of probe-to-bone test and plain radiography sufficient for high-risk inpatients? Diabet Med. 2011;28:191-194. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 130] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 28. | Álvaro-Afonso FJ, Lázaro-Martínez JL, Aragón-Sánchez J, García-Morales E, García-Álvarez Y, Molines-Barroso RJ. Inter-observer reproducibility of diagnosis of diabetic foot osteomyelitis based on a combination of probe-to-bone test and simple radiography. Diabetes Res Clin Pract. 2014;105:e3-e5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 33] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 29. | Fleischer AE, Didyk AA, Woods JB, Burns SE, Wrobel JS, Armstrong DG. Combined clinical and laboratory testing improves diagnostic accuracy for osteomyelitis in the diabetic foot. J Foot Ankle Surg. 2009;48:39-46. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 68] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 30. | Michail M, Jude E, Liaskos C, Karamagiolis S, Makrilakis K, Dimitroulis D, Michail O, Tentolouris N. The performance of serum inflammatory markers for the diagnosis and follow-up of patients with osteomyelitis. Int J Low Extrem Wounds. 2013;12:94-99. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 100] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 31. | Game FL. Osteomyelitis in the diabetic foot: diagnosis and management. Med Clin North Am. 2013;97:947-956. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 38] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 32. | Hartemann-Heurtier A, Senneville E. Diabetic foot osteomyelitis. Diabetes Metab. 2008;34:87-95. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 90] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 33. | Berendt AR, Peters EJ, Bakker K, Embil JM, Eneroth M, Hinchliffe RJ, Jeffcoate WJ, Lipsky BA, Senneville E, Teh J. Diabetic foot osteomyelitis: a progress report on diagnosis and a systematic review of treatment. Diabetes Metab Res Rev. 2008;24 Suppl 1:S145-S161. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 225] [Cited by in RCA: 215] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 34. | Sella EJ, Grosser DM. Imaging modalities of the diabetic foot. Clin Podiatr Med Surg. 2003;20:729-740. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 32] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 35. | Capriotti G, Chianelli M, Signore A. Nuclear medicine imaging of diabetic foot infection: results of meta-analysis. Nucl Med Commun. 2006;27:757-764. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 48] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 36. | Newman LG, Waller J, Palestro CJ, Hermann G, Klein MJ, Schwartz M, Harrington E, Harrington M, Roman SH, Stagnaro-Green A. Leukocyte scanning with 111In is superior to magnetic resonance imaging in diagnosis of clinically unsuspected osteomyelitis in diabetic foot ulcers. Diabetes Care. 1992;15:1527-1530. [PubMed] |
| 37. | Przybylski MM, Holloway S, Vyce SD, Obando A. Diagnosing osteomyelitis in the diabetic foot: a pilot study to examine the sensitivity and specificity of Tc(99m) white blood cell-labelled single photon emission computed tomography/computed tomography. Int Wound J. 2016;13:382-389. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 38. | Filippi L, Uccioli L, Giurato L, Schillaci O. Diabetic foot infection: usefulness of SPECT/CT for 99mTc-HMPAO-labeled leukocyte imaging. J Nucl Med. 2009;50:1042-1046. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 57] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 39. | Lazaga F, Van Asten SA, Nichols A, Bhavan K, La Fontaine J, Oz OK, Lavery LA. Hybrid imaging with 99mTc-WBC SPECT/CT to monitor the effect of therapy in diabetic foot osteomyelitis. Int Wound J. 2016;13:1158-1160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 30] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 40. | Keidar Z, Militianu D, Melamed E, Bar-Shalom R, Israel O. The diabetic foot: initial experience with 18F-FDG PET/CT. J Nucl Med. 2005;46:444-449. [PubMed] |
| 41. | Palestro CJ. 18F-FDG and diabetic foot infections: the verdict is. J Nucl Med. 2011;52:1009-1011. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 17] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 42. | Nawaz A, Torigian DA, Siegelman ES, Basu S, Chryssikos T, Alavi A. Diagnostic performance of FDG-PET, MRI, and plain film radiography (PFR) for the diagnosis of osteomyelitis in the diabetic foot. Mol Imaging Biol. 2010;12:335-342. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 106] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 43. | Levine SE, Neagle CE, Esterhai JL, Wright DG, Dalinka MK. Magnetic resonance imaging for the diagnosis of osteomyelitis in the diabetic patient with a foot ulcer. Foot Ankle Int. 1994;15:151-156. [PubMed] |
| 44. | Dinh MT, Abad CL, Safdar N. Diagnostic accuracy of the physical examination and imaging tests for osteomyelitis underlying diabetic foot ulcers: meta-analysis. Clin Infect Dis. 2008;47:519-527. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 171] [Cited by in RCA: 183] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 45. | Masala S, Fiori R, Marinetti A, Uccioli L, Giurato L, Simonetti G. Imaging the ankle and foot and using magnetic resonance imaging. Int J Low Extrem Wounds. 2003;2:217-232. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 46. | Giurato L, Uccioli L. The diabetic foot: Charcot joint and osteomyelitis. Nucl Med Commun. 2006;27:745-749. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 19] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 47. | Elamurugan TP, Jagdish S, Kate V, Chandra Parija S. Role of bone biopsy specimen culture in the management of diabetic foot osteomyelitis. Int J Surg. 2011;9:214-216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 59] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 48. | Malone M, Bowling FL, Gannass A, Jude EB, Boulton AJ. Deep wound cultures correlate well with bone biopsy culture in diabetic foot osteomyelitis. Diabetes Metab Res Rev. 2013;29:546-550. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 22] [Article Influence: 1.7] [Reference Citation Analysis (1)] |
| 49. | Tan JS, Friedman NM, Hazelton-Miller C, Flanagan JP, File TM. Can aggressive treatment of diabetic foot infections reduce the need for above-ankle amputation? Clin Infect Dis. 1996;23:286-291. [PubMed] |
| 50. | Ha Van G, Siney H, Danan JP, Sachon C, Grimaldi A. Treatment of osteomyelitis in the diabetic foot. Contribution of conservative surgery. Diabetes Care. 1996;19:1257-1260. [PubMed] |
| 51. | Pittet D, Wyssa B, Herter-Clavel C, Kursteiner K, Vaucher J, Lew PD. Outcome of diabetic foot infections treated conservatively: a retrospective cohort study with long-term follow-up. Arch Intern Med. 1999;159:851-856. [PubMed] |
| 52. | Game FL, Jeffcoate WJ. Primarily non-surgical management of osteomyelitis of the foot in diabetes. Diabetologia. 2008;51:962-967. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 102] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 53. | Senneville E, Lombart A, Beltrand E, Valette M, Legout L, Cazaubiel M, Yazdanpanah Y, Fontaine P. Outcome of diabetic foot osteomyelitis treated nonsurgically: a retrospective cohort study. Diabetes Care. 2008;31:637-642. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 177] [Cited by in RCA: 173] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 54. | Acharya S, Soliman M, Egun A, Rajbhandari SM. Conservative management of diabetic foot osteomyelitis. Diabetes Res Clin Pract. 2013;101:e18-e20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 59] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 55. | Lázaro-Martínez JL, Aragón-Sánchez J, García-Morales E. Antibiotics versus conservative surgery for treating diabetic foot osteomyelitis: a randomized comparative trial. Diabetes Care. 2014;37:789-795. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 164] [Cited by in RCA: 166] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 56. | Tone A, Nguyen S, Devemy F, Topolinski H, Valette M, Cazaubiel M, Fayard A, Beltrand É, Lemaire C, Senneville É. Six-week versus twelve-week antibiotic therapy for nonsurgically treated diabetic foot osteomyelitis: a multicenter open-label controlled randomized study. Diabetes Care 2015; 38: 302-307. Diabetes Care. 2015;38:735. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (1)] |
| 57. | Kowalski TJ, Matsuda M, Sorenson MD, Gundrum JD, Agger WA. The effect of residual osteomyelitis at the resection margin in patients with surgically treated diabetic foot infection. J Foot Ankle Surg. 2011;50:171-175. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 75] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 58. | Armstrong DG, Lavery LA. Plantar pressures are higher in diabetic patients following partial foot amputation. Ostomy Wound Manage. 1998;44:30-2, 34, 36 passim. [PubMed] |
| 59. | Molines-Barroso RJ, Lázaro-Martínez JL, Aragón-Sánchez J, García-Morales E, Beneit-Montesinos JV, Álvaro-Afonso FJ. Analysis of transfer lesions in patients who underwent surgery for diabetic foot ulcers located on the plantar aspect of the metatarsal heads. Diabet Med. 2013;30:973-976. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 63] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Manuscript source: Invited manuscript
Specialty type: Endocrinology and metabolism
Country of origin: Italy
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Guerado E, Lowery NJ, Qi L, Puri K S- Editor: Ji FF L- Editor: A E- Editor: Wu HL