Published online Feb 10, 2016. doi: 10.4239/wjd.v7.i3.34
Peer-review started: August 3, 2015
First decision: October 13, 2015
Revised: December 14, 2015
Accepted: December 29, 2015
Article in press: January 4, 2016
Published online: February 10, 2016
Processing time: 178 Days and 17.9 Hours
On a worldwide scale, the total number of migrants exceeds 200 million and is not expected to reduce, fuelled by the economic crisis, terrorism and wars, generating increasing clinical and administrative problems to National Health Systems. Chronic non-communicable diseases (NCD), and specifically diabetes, are on the front-line, due to the high number of cases at risk, duration and cost of diseases, and availability of effective measures of prevention and treatment. We reviewed the documents of International Agencies on migration and performed a PubMed search of existing literature, focusing on the differences in the prevalence of diabetes between migrants and native people, the prevalence of NCD in migrants vs rates in the countries of origin, diabetes convergence, risk of diabetes progression and standard of care in migrants. Even in universalistic healthcare systems, differences in socioeconomic status and barriers generated by the present culture of biomedicine make high-risk ethnic minorities under-treated and not protected against inequalities. Underutilization of drugs and primary care services in specific ethnic groups are far from being money-saving, and might produce higher hospitalization rates due to disease progression and complications. Efforts should be made to favor screening and treatment programs, to adapt education programs to specific cultures, and to develop community partnerships.
Core tip: At global level the phenomenon of migration of people is not expected to slow down in the next years, generating a multitude of clinical problems and economic costs for the National Health System. The increasing burden of chronic diseases, particularly diabetes, in migrant minority populations is today a major public health challenge for several countries, mainly in Europe, fuelled by the economic crisis, inequalities, terrorism and wars. Even in a universalistic healthcare system, differences in socioeconomic status and barriers generated by the present culture of biomedicine might make high-risk ethnic minorities under-treated and not protected against inequalities. Our objective is to pinpoint the problems arising in the prevention and treatment of diabetes on a worldwide scale, aiming to give support to healthcare systems in the provision of effective interventions.
- Citation: Montesi L, Caletti MT, Marchesini G. Diabetes in migrants and ethnic minorities in a changing World. World J Diabetes 2016; 7(3): 34-44
- URL: https://www.wjgnet.com/1948-9358/full/v7/i3/34.htm
- DOI: https://dx.doi.org/10.4239/wjd.v7.i3.34
Migration is an ancient phenomenon, dating back to the time of our African ancestors and occurring on a variety of levels (intercontinental, intra-continental, and interregional)[1].
Several factors contribute to migration. At the beginning of the 19th century, migrants were mostly farmers, farmhands, workmen and refugees but lately, people belonging to the educated and well-off class have started to migrate towards developed countries because of the industrial globalization and the availability of grater opportunities in open-market economies, favored by the Internet revolution[2]. These two sets of factors, “push factors” in native countries (food shortage, wars, civil wars, terrorism) and “pull factors” in host countries (economic booming, job opportunities, well-being) remain the basis of migration.
Massive immigration has generated a series of clinical-administrative problems to National Health Systems throughout the world, and also to universalistic systems. This is mainly the case with the so-called chronic non-communicable diseases (NCD), particularly diabetes, due to the very high number of cases at risk[3], the long duration of treatment, the very high cost of complications[4], as well as the availability of effective preventive and therapeutic measures expected to alleviate the burden of disease[5].
We reviewed the documents of International Agencies on migration and performed a PubMed search of existing literature, using the terms “diabetes” and “migrants”. This manuscript is aimed at pinpointing the problems arising in the worldwide prevention and treatment of diabetes, with specific reference to countries where they have been more extensively investigated, as a support to healthcare systems in the provision of effective interventions.
On a worldwide scale, the total number of economic migrants exceeds 200 million, not considering asylum-seeking refugees. Albeit slowed down in the recent phase of recession, the flow will keep on in Europe and in Asia too, where China will become the main pole of attraction of the migration scenario[2]. Only about 10%-15% of migrants from all over the world are in an irregular situation: most of them have entered in a legal way but remain more long-term than their authorized residence[6].
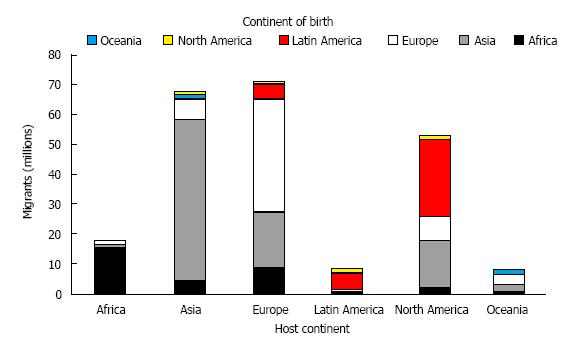
As of January 2014, the number of migrants for economic reasons in the 28 countries of the European Union (EU) totals 19.6 million, representing 3.9% of the population (Figure 1). In absolute terms, the largest numbers are found in Germany (7.0 million persons), the United Kingdom (5.0 million), Italy (4.9 million), Spain (4.7 million) and France (4.2 million), collectively representing 76% of the total. Besides, according to estimates, there is an unknown number of undocumented migrants, accounting for a huge proportion of the population (up to 4%)[7]. The total number is expected to increase dramatically in the near future, due to massive migration of asylum-seekers refugees from conflict areas in Middle East and Northern Africa. A few EU countries are facing for the first time the problem of immigration and multi-ethnic population. Migrants have long been a negligible problem in Italy. In 1991, for the first time the number of migrants exceeded 1% of the total Italian population. Later, the number doubled in ten years to reach 7.5% by the end of 2010[8].
Migration to the United States has also been increasing since 1945 with the current immigrant population estimated at 38.5 million or 12% of the total population[9] (Figure 1). Large waves of immigration occurred over the past 20 years[10]; by 2050, nearly 1 in 5 United States residents is expected to be an immigrant, compared with 1 in 8 in 2005[11].
Since 1945, more than 7 million people have also settled in Australia. The 2011 Census reported that over one in four of Australian 22-million people were born overseas. Most of them were born in New Zealand (16.2%), the United Kingdom (13.6%), India (10.9%), China (10.0%) and South Africa (4.6%) (Figure 1). Pacific Islanders (Samoans and Tongans) represent another large component of immigration[12].
The complexity of migration remains a fundamental problem. Most statistics on migration are based on concepts that are not representative of a good deal of the dynamics of today migration flows. It is nearly impossible to have the exact numbers of short-term movements and status, as well as to assess properly the extent of undocumented migration that exploded around and across the Mediterranean Sea.
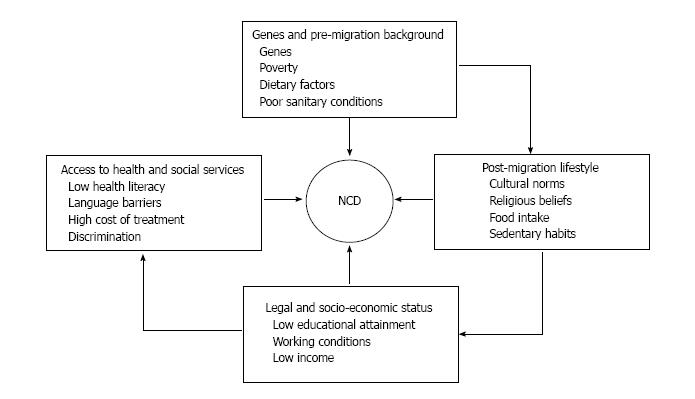
Different data sources may be used to describe the outbreak of NCDs in relation to indicators of migration or ethnicity, as country of birth, self-identified ethnicity, as well as more specific features (language and religious affiliation)[13-15]. The essence of ethnicity implies same origins or social environment, definite culture and customs, and a common language or religious heritage[16,17], but proxy measures are difficult to define. Country of birth is a crude method, which becomes a vague measure as time since migration goes on[15,18]. Nationality or citizenship represent critical indexes as immigrants may have nationality and citizenship of the host country, but yet belong to ethnic groups with different lifestyle habits, religion and culture. Without an overall agreement concerning both the definition of ethnicity and of being a migrant, it is difficult to set the reasons behind the prevalence of NCDs or diabetes. The relation between migration status and disease may be affected by genes, exposure in pre-migration life to poverty, precarious health and sanitary conditions, eating habits, infections, rooted cultural customs retained in adulthood, exposures in post-migration life, as well as quality of health care and access to health services in countries of destination (Figure 2).
Europe: With a few exceptions, prevalence, incidence and mortality rates for diabetes are much higher in migrants than in native people[2,19-22]. In the Netherlands, diabetes is more common (by a factor of 2) among the main groups of immigrants, i.e., those born in Turkey, Morocco, Suriname or the Antilles. Even larger differences are observed in diabetes-related mortality, with rates 3 and 4 times higher among migrant men and women, respectively, compared to the indigenous population. Surinamese migrants have the highest prevalence and mortality rates[23], which are most likely due to the higher incidence, although differences in case-fatality rates may also exist.
In the United Kingdom, the prevalence of diabetes mellitus among migrants of South Asian origin (Afghanistan, Bhutan, Maldives, Nepal and Sri Lanka) is around 20%, i.e., nearly five times higher than the local European population. Furthermore, age at onset of diabetes is 5-10-year earlier and chronic complications are more common amongst migrant populations[24]. In Italy, the prevalence of diabetes in migrants is definitely lower than in the general population, but only 15% of migrants are less than 50, vs 43.1% of the Italian population[25]. When adjusted for age and sex in a case-control study, the overall risk of diabetes in migrants was 1.55 (95%CI: 1.50-1.60)[26]. Notably, the risk varies among ethnic groups; the likelihood of being treated with a glucose-lowering drug is four-fold higher in people from Egypt and the Indian subcontinent, whereas it is halved in migrants from former Eastern socialist countries, in keeping with diabetes prevalence in their countries of origin[13]. Also in African migrants to France diabetes develops earlier compared to those staying in their country of birth[27].
A 20-year longitudinal follow-up of first generation migrants residing in the United Kingdom reports an incidence of type 2 diabetes almost 3 times higher in the Indian Asian population and more than twice in the African Caribbeans, compared with the European controls. Notably, in the female population the increased likelihood of having diabetes was attributed to baseline insulin resistance and abdominal adiposity, not in men[28]. The Healthy Life in an Urban Setting (HELIUS) study, started in 2011, aimed at assessing the factors contributing to the occurrence of diseases, including NCD, cardiovascular diseases and mental disorders, in association with ethnic differences, in a cohort of about 60000 Amsterdam residents representative of 5 migrant groups as well as native residents[29]. Patients with diabetes coming from Asia, Middle East and Sub-Saharan Africa if compared to Western populations are at particularly higher risk of microvascular complications, i.e., diabetic retinopathy, nephropathy and peripheral neuropathy[30]. It is also the case in ethnic minorities of the same regions settled in Western countries; e.g., in the United Kingdom minority ethnic communities with type 2 diabetes, compared to white Europeans, are more likely to develop ocular complications, including sight-threatening retinopathy and maculopathy[31].
In seven European countries diabetes mortality of 30 migrant groups was much higher than in native residents (almost 90% higher for the male population and 120% higher for the female population)[32]. An English follow-up study reported higher diabetes mortality rates in patients from South Asia compared to European patients, particularly among the young population[33]. Similar observations have been made amongst Asian Indian migrants[34].
These differences might be ascribed to a genetic background. Nevertheless, the few studies considering socio-economic factors and quality of diabetes care show a reduction of the role of ethnic differences in complication rates. Therefore, complications among ethnic minority groups with diabetes might also be driven by failure to achieve treatment goals and/or lower screening rates and preventive measures[31].
United States: In 9 regions of birth, covering a hundred countries, representing 16 million United States immigrants, overweight/obesity and diabetes prevalence were regularly estimated and compared from 1997 to 2005. Most of migrants were born in Mexico (48%), followed in order of decreasing number by migrants from all Asian regions (almost 20%), Europe, South America, Africa, the Middle East, and Russia. Among United States immigrants, a substantial heterogeneity is noted, by region of birth, in the prevalence of both diabetes and overweight, with diabetes rates stretching from 3.1% in Europe to 10.0% in the Indian subcontinent[35]. Migrants from South America, generally considered as Hispanic ethnicity, have lower diabetes and overweight prevalence than migrants from Mexico, Central America, and the Caribbean Islands; i.e., gathering individuals by ethnicity may conceal important differences in the prevalence of the disease.
Blacks (without any distinction for immigrant status) have higher rates of diabetes compared with whites[36]. The difference is likely to stem from the increased insulin resistance of black people at adiposity levels similar to whites[37], particularly in African migrant men, not in women. Black women have twice the obesity prevalence of white women[38], and a prospective incidence study on ethnicity and diabetes in middle-aged adults, African American men and, to a lesser extent, women had a considerably higher incidence of type 2 diabetes compared with white people. The elevated incidence and prevalence of diabetes is thus explained by modifiable risk factors such as adiposity[39].
The three largest Asian-American, native Hawaiian, Pacific Islander subgroups [people of Chinese (3.3 million), South Asian (2.8 million), or Filipino (2.6 million) ancestry] are all at increased risk to develop diabetes[40]. In general, their risk is higher relative to non-Hispanic whites, but lower than that of African Americans and Latinos[41,42]. Although data are limited[43], diabetes prevalence is more than doubled among Pacific Islanders (18.3%) vs white participants (7.3%), and significantly higher than among other Asian subgroups, confirming that continental data must be disaggregated on a national scale[42]. Ethnicity-specific risks of microvascular complications (retinopathy) have also been demonstrated[44].
Australia: For all migrant groups, the odds of type 2 diabetes vs native residents are higher, after adjusting for age and across all socio-economic strata[45]. In the Fremantle Diabetes Study, the prevalence in Asians and the general population was similar, but the Asian patients were younger, less obese and less likely to be hypertensive. Nonetheless, they had a higher prevalence of retinopathy. During an 18-year follow-up, Asian ethnicity was independently protective against cardiovascular death, not all-cause mortality[46]. According to the Melbourne Collaborative Cohort Study[47], the baseline prevalence and the cumulative incidence of type 2 diabetes were more than three-fold higher in migrants born in Greece or Italy than in individuals born in Australia[48]. These findings are consistent with the higher prevalence showed by Australian cross-sectional studies[49,50].
Higher BMI in the migrants was responsible for almost one-half the excess relative risk in incidence, whereas other risk factors for diabetes, including the waist-to-hip ratio, and diet, had little impact on the remaining excess relative risk. However, there is no evidence for a specific genetic susceptibility to diabetes in Italian migrants[51]. Health care is universally available in Australia and generally of good standard. Thus, the risk of excess mortality in migrants because of different chances of access to treatment and standard of care is minimized. The poorer outcome of migrant people with diabetes remains a priority study area, subject to continuous scrutiny[52].
When the prevalence of diabetes in migrants is compared with that in the country of origin, the general characteristics, the prevalence of obesity, as well as the general degree of socioeconomic development, as measured by the gross domestic product[32], should always be considered. The lower the socio-economic status in the country of origin, the higher the risk to become obese. For example, in a study investigating on Ghanaian migrants in the Netherlands, people living in Amsterdam compared to those living in rural Ghana[53], were 10 times more likely to be overweight, and overweight represents a risk factor for the development of diabetes. This explains why among migrants from low-income countries compared to locally born European populations, diabetes mortality rates are more than 200% higher, in comparison to a 100% higher rates for migrants from middle-income countries[32]. In view of these considerations the high diabetes mortality of migrants seems to be associated to the movement from a poverty-ridden rural area, in early life, to an obesogenic urban environment in later life, with a few exceptions.
According to previous researches Asian Indians who moved to the United States have worse metabolic profiles when compared to their counterparts still living in India[54]. Contrary to that, the CARRS and MASALA Studies[55] reported a higher diabetes prevalence in indian people living in India than their homologous who have migrated to the United States, even with Asian Indians living in India having lower BMI and lower waist circumference values than their counterparts who have migrated to the United States. Surprisingly, both the overall and the age specific prevalence of prediabetes resulted lower in Asian Indians living in India than in Asian Indians minorities who moved to the United States; the explication could be linked to a more rapid conversion, through the natural history of the disease, in people living in India. Furthermore, the prevalence of type 2 diabetes in Asian Indians living in the United States was still significantly higher than that of the general United States population[41,55,56], despite the fact that the general United States population has, compared to Asian Indians, an overall higher BMI. Therefore it could be probable that India finds itself in an early stage of the diabetes epidemic; thus most susceptible subjects develop it the earliest[57].
Having regard to the current phase of rapid economic and nutritional changes over the Indian continent[58,59], these aspects could increase the risk in Asian Indians both in India and abroad. It is also likely that Asian Indians who have migrated to the United States have adopted healthier lifestyle habits, both in food choices and physical exercise, reducing their risk of type 2 diabetes occurrence[60], thereby altering the relation existing in this population between migration and NCD risk.
Another way of analyzing the role of country of origin is to compare migrants who come from the same country, now living in different countries. From January 2012, a multicenter cross-sectional study is evaluating differences in lifestyle, epigenetics and biochemistry that increase the risk of type 2 diabetes and obesity among homogenous sub-Saharan African participants (i.e., Ghanaians) aged > 25 years living in rural and urban Ghana, the Netherlands, Germany and the United Kingdom[61].
Genetic factors should anyway be considered to dictate the prevalence of NCD in migrants, as compared to the native populations. Genetic studies have confirmed a role of the ethnic background in the higher prevalence of diabetes in South Asian people[62-64] and in the higher rates of hypertension among West African migrants[65,66], whereas the obesogenic environment of the country of immigration makes the difference between NCD prevalence in migrants vs the corresponding prevalence in the country of origin.
In the long-term, diabetes risk in migrants is expected to converge towards the levels of the locally born populations. This relates to the “healthy migrant” effect, i.e., migration is expected to be a selective process favoring healthy individuals, resulting in low occurrence of diseases among migrants in the first period after their arrival in the host countries[67]. As an example, in 2013, the median age of the national population in the EU-28 was 43 years, while the median age of non-nationals living in the EU was 35 years. This protective effect is also present with other NCDs[46], but as time goes by the relative advantage of migrants over locally born subjects could reduce.
Convergence can be also predicted due to the fact that migrants generally integrate over time into the society, and its customs, of their host country[68]. As migrants adopt the same habits being exposed to the same environmental risk factors as indigenous people, albeit gradually and slowly[69-71], their epidemiological profiles may move ever closer to those of locally born subjects[68]. “Period” studies (comparing different time periods)[70,72,73] and “cohort” studies (comparing cohorts of migrants differing in terms of acculturation)[69] supported the convergence hypothesis: The risk of cancer resulted more similar to that of the indigenous populations among people with a longer period of migration, i.e., among the second generation, and, within the first generation, among people who had migrated during infancy. However, convergence takes a lot of time, more than 20 years in some studies[74].
Another theory explains lower mortality in migrants by “the salmon bias” hypothesis, reflecting the trend of sick migrants returning back to their home country before death; in most settings, this does not fully explain the paradox[67,75,76], and it is possible that inaccurate counting of mortality among migrants minority groups lead to an underestimation bias[77].
Predisposition to develop insulin resistance and truncal obesity, the exposure to a particular intrauterine environment and even the biological imprinting all push in the same direction enhancing the risk of diabetes[78], as well as its progression, in migrant populations, frequently fuelled by differences in standard of care. Many migrants in non-Western countries have risen in conditions of poverty and their bodies have been “programmed” to tackle hunger and starvation. The result is that later in life, when exposed to the obesogenic environment of the country of immigration (high-fat diet and sedentary lifestyle), they are particularly prone to stock energy reserves and thereby gain weight[2,53]. A cross-sectional study in a large cohort of migrants from the Philippines to the city of Rome recorded abdominal obesity in 52.5% and a high prevalence of undiagnosed type 2 diabetes and hypertension[79]. Years of residence in Italy showed a significant direct correlation with the degree of changes in food intake (P = 0.001) and weight gain (P < 0.001), suggesting a direct impact of lifestyle.
Also the so-called social determinants of health may be involved (i.e., low socio-economic status, separation from family, anti-migrant feelings in the host community, traditional beliefs influencing the health-seeking behavior, the lack of legislation to ensure migrants’ access to health and social services, effective policies to protect migrants’ labor rights and welfare). This is mainly the case with insurance-type health care systems, but poor access to health services is also demonstrated in health care systems that are essentially built on a principle of equity and equality. Integration of migrant population into the receiving healthcare system is becoming a key issue in developed countries who receive a large number of migrants each year. Independently of the healthcare system, several reports have shown that migrants are undertreated compared with the native population[80,81]. This is probably related to a lower-than-needed attendance of migrants to primary care or preventive health services, due to personal barriers (job and time constraints) or socio-cultural conditions, not only to specific defects in the healthcare system[82,83]. In native Dutch and in various groups of immigrants aged 55 and older, the use of prescribed drugs was explained by Andersen’s behavioral model[84], based on three individual factors of health care use: (1) need (self-rated chronic conditions); (2) enabling conditions (educational level, standardized household income); and (3) predisposing factors (Dutch language proficiency, modern attitudes on family care, male-female roles, family values, religion)[85]. Differences in the verbal interaction of Dutch GPs with immigrant vs Dutch patients have been demonstrated by video recording: Consultations with immigrant patients were over 2 min shorter, with major differences in verbal interaction and less empathy[82]. In diabetes, language proficiency and modern attitudes on male-female roles have been associated with utilization of diabetes drugs, especially in Turkish[86] and Moroccan elderly patients[85], where inequalities might be amplified by behavioral components (smoking, inactivity, alcohol consumption)[87,88].
Leisure time physical activity is definitely lower in migrants[89-91], but the amount of calories spent at work, because of more common manual labor, might be considerably higher[64]. An Australian study reported a higher relative risk of smoking and alcohol use[92], and lower adherence to recommendation for healthy diet is also frequently described. A systematic review from the United Kingdom, on a migrant South Asian population, reported that all South Asian groups were found to have a more sedentary lifestyle than their European counterparts[93]. However, the high variability and the large proportion of different migrant minorities moving across the world make it difficult to draw any conclusions.
Inequalities in migrant health care are not limited to diabetes groups. In a Swiss cohort of forced, asylum seekers migrants, lower scores for physical examinations and breast and colon cancer screening have been reported, despite universal healthcare coverage[94]. In a Swedish population-based follow-up concerning drugs given to patients after acute myocardial infarction, no major differences were observed in relation to socio-economic status[95]. However, among immigrants from outside the EU countries there was a 20%-30% reduced prescription of drugs recommended by Swedish guidelines (aspirin, beta-blockers, cholesterol-lowering drugs and ACE inhibitors). Also in this case, ethnicity may make the difference; in ethnic German migrants from the former Soviet Union to Germany only minor differences in drug utilization pattern were recorded, compared with native Germans[96]. In this case, however, much similar habits and traditions might help canceling the differences. Far from being money-saving for the Health Systems, underutilization of drugs and primary care services in specific ethnic groups is expected to produce a larger-than-needed use of emergency services and hospitalization rates due to disease progression and complications, which might translate into higher costs[97,98].
Data from the ARNO database: Drug use and the direct costs of drug-treated diabetes among migrants and Italian citizens has been extensively investigated on the basis of 2010 prescriptions in the population-based multiregional ARNO Observatory, a database containing the prescriptions and hospital admissions of a population of about 10 million Italian residents, living in 30 Health districts scattered throughout the country[99]. According to Italian rules, a diagnosis of diabetes grants free access to drugs, diagnostic procedures and hospitalization to persons residents in Italy, independently of their citizenship. All drug prescription data or hospital admission records contain a code including the date and place of birth. For people born outside Italy, the city code is replaced by the country code, thus permitting univocal identification of people born outside Italy.
Based on the above criteria, in the nested ARNO population of over 8 million people first and second-generation migrants were classified according to country of birth and citizenship. All patients who had at least one prescription of anti-diabetic medication, either oral agents or insulin (Anatomical Therapeutic Chemical Classification System, code A10A and A10B, respectively) during 2010 were considered as affected by diabetes. The odds of migrants of being diagnosed with diabetes compared to Italians were tested using a case-control study design, with one migrant matched for major confounders (age, sex and place of residence) to one Italian subject. Finally, migrants with diabetes were individually matched for confounders to Italians with diabetes to compare prescriptions, hospitalization rates, use of services and direct costs for the National Health System.
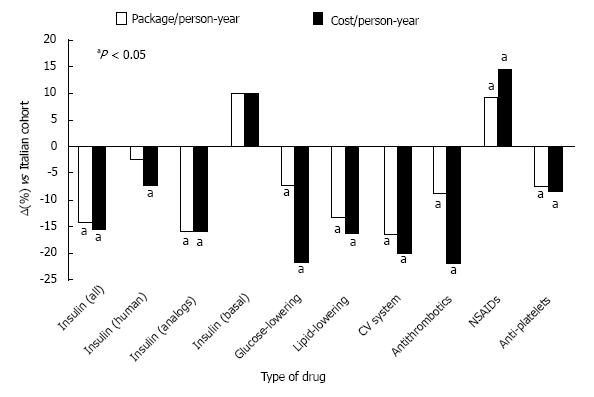
Migrants with diabetes were 15-year younger than native Italians. Both glucose-lowering and non-glucose-lowering drugs were underused in migrants with diabetes, with the notable exception of a few drugs (i.e., non-steroidal anti-inflammatory agents), whose excess use might be related to more intense manual and traumatic work (Figure 3). Migrants had a different pattern of glucose-lowering treatment, with 44% higher prescriptions of oral drugs and 19% lower prescriptions of insulin and a different insulin pattern[26,100]. Also lipid-lowering drugs and antithrombotic drugs were 15%-20% underused in migrants. The total cost was 27% lower in migrants, due to a lower cost of drugs (29%), hospital admission (27%) and health services (22%)[26].
Notably, hospitalization rates due to diabetes per se were 60% more common in migrants vs native Italians of the ARNO observatory[26]. This might represent the consequence of under-treatment, also considering that hospital length-of-stay was longer in migrants. Contrary to that, a report from the London School of Economics found that hospital stay among the immigrant population was significantly shorter in Europe after adjusting for age, case mix and disease severity, suggesting unequal treatment for equal needs[101]. A cross-sectional analysis of health service use among elderly immigrants and native populations of 11 European countries recorded a migrants’ overutilization of hospital stay and consultations in several countries, not in Italy, due to difficulties in the integration of migrants because of very recent immigration and cultural reasons[102]. No data are available on the attendance of migrants to emergency departments not followed by hospital admission, a procedure not traced by the Italian Health System. Emergency services might be overused, fuelled by socioeconomic inequalities[103], to provide immediate care to less complicated conditions.
The growing burden of chronic diseases, specifically diabetes, in migrant and ethnic minorities represents a serious public health challenge for many European countries, also fuelled by the economic crisis, social inequalities, terrorism and wars. Migrant flow is not expected to slow down in the next few years, and it will generate an increasing economic cost for the National Health System. The same is true for United States, where African and Mexican Americans may experience higher rates of diabetes prevalence, which will translate into different and increasing costs.
High-risk migrant minorities may remain undertreated and unprotected also in a universalistic healthcare system[104]. Poorer socioeconomic status and barriers generated by the present culture of biomedicine might make the difference on patients’ side, but inequalities might also stem from physicians’ side, with a different approach by both primary care physicians and specialists[105]. Efforts should be made to favor visits to general practitioners/diabetologists and attendance to screening and treatment programs, to adapt education programs to specific cultures[106], to cope with misbeliefs[107], and to develop community partnerships.
| 1. | United Nations Statistics Division. Recommendations on Statistics of International Migration, Revision 1. Geneva, United Nations. 1998; Available from: http://unstats.un.org/unsd/iiss/Recommendations-on-Statistics-of-International-Migration-Revision-1.ashx. |
| 2. | Misra A, Ganda OP. Migration and its impact on adiposity and type 2 diabetes. Nutrition. 2007;23:696-708. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 173] [Cited by in RCA: 183] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 3. | Hempler NF, Diderichsen F, Larsen FB, Ladelund S, Jørgensen T. Do immigrants from Turkey, Pakistan and Yugoslavia receive adequate medical treatment with beta-blockers and statins after acute myocardial infarction compared with Danish-born residents? A register-based follow-up study. Eur J Clin Pharmacol. 2010;66:735-742. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 32] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 4. | American Diabetes Association. Economic costs of diabetes in the U.S. in 2012. Diabetes Care. 2013;36:1033-1046. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1675] [Cited by in RCA: 1721] [Article Influence: 132.4] [Reference Citation Analysis (0)] |
| 5. | Nicolucci A, Rossi MC, Arcangeli A, Cimino A, de Bigontina G, Fava D, Gentile S, Giorda C, Meloncelli I, Pellegrini F. Four-year impact of a continuous quality improvement effort implemented by a network of diabetes outpatient clinics: the AMD-Annals initiative. Diabet Med. 2010;27:1041-1048. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 52] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 6. | International Organization for Migration. World Migration Report 2010. Geneva, International Organization for Migration. 2010; Available from: http://publications.iom.int/system/files/pdf/wmr_2010_english.pdf. |
| 7. | Karl-Trummer U, Metzler B, Novak-Zezula S; Health Care for Undocumented Migrants in the EU: Concepts and Cases. Brussels, IOM, 2009. 2010; Available from: http://www.migrant-health-europe.org/files/Health Care for Undocumented Migrants_Background Paper(6).pdf. |
| 8. | Karl-Trummer U; Caritas/Migrantes. Dossier Statistico Immigrazione. Rome, IDOS - Centro Studi e Ricerche. 2011; Available from: http://www.dossierimmigrazione.it/docnews/file/pres2011-scheda.pdf. |
| 9. | US Census Bureau. The 2009 American Community Survey. Washington, DC, US Census Bureau. 2010; Available from: https://www.census.gov/newsroom/releases/archives/american_community_survey_acs/cb10-cn78.html. |
| 10. | Kandula NR, Kersey M, Lurie N. Assuring the health of immigrants: what the leading health indicators tell us. Annu Rev Public Health. 2004;25:357-376. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 161] [Cited by in RCA: 159] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 11. | Passel JS, Cohm D. US Population Projections: 2005-2050. Washington, DC: Pew Research Center 2008; Available from: http://www.pewsocialtrends.org/files/2010/10/85.pdf. |
| 12. | Statistics New Zealand and Ministry of Pacific Affairs. Demographics of New Zealand’s Pacific population. Wellington, Statistics New Zealand. Washington, DC: Pew Research Center 2010; Available from: http://www.stats.govt.nz/browse_for_stats/people_and_communities/pacific_peoples/pacific-progress-demography.aspx. |
| 13. | Rafnsson SB, Bhopal RS. Large-scale epidemiological data on cardiovascular diseases and diabetes in migrant and ethnic minority groups in Europe. Eur J Public Health. 2009;19:484-491. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 35] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 14. | Stronks K, Kunst AE. The complex interrelationship between ethnic and socio-economic inequalities in health. J Public Health (Oxf). 2009;31:324-325. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 42] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 15. | Stronks K, Kulu-Glasgow I, Agyemang C. The utility of ‘country of birth’ for the classification of ethnic groups in health research: the Dutch experience. Ethn Health. 2009;14:255-269. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 218] [Cited by in RCA: 256] [Article Influence: 15.1] [Reference Citation Analysis (0)] |
| 16. | Lin SS, Kelsey JL. Use of race and ethnicity in epidemiologic research: concepts, methodological issues, and suggestions for research. Epidemiol Rev. 2000;22:187-202. [PubMed] |
| 17. | Ford ME, Kelly PA. Conceptualizing and categorizing race and ethnicity in health services research. Health Serv Res. 2005;40:1658-1675. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 135] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 18. | Gill PS, Bhopal R, Wild S, Kai J. Limitations and potential of country of birth as proxy for ethnic group. BMJ. 2005;330:196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 14] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 19. | Deboosere P, Gadeyne S. Adult migrant mortality advantage in Belgium: evidence using census and register data. Population. 2005;60:655-698. |
| 20. | Kristensen JK, Bak JF, Wittrup I, Lauritzen T. Diabetes prevalence and quality of diabetes care among Lebanese or Turkish immigrants compared to a native Danish population. Prim Care Diabetes. 2007;1:159-165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 33] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 21. | Ujcic-Voortman JK, Schram MT, Jacobs-van der Bruggen MA, Verhoeff AP, Baan CA. Diabetes prevalence and risk factors among ethnic minorities. Eur J Public Health. 2009;19:511-515. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 108] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 22. | Jenum AK, Diep LM, Holmboe-Ottesen G, Holme IM, Kumar BN, Birkeland KI. Diabetes susceptibility in ethnic minority groups from Turkey, Vietnam, Sri Lanka and Pakistan compared with Norwegians - the association with adiposity is strongest for ethnic minority women. BMC Public Health. 2012;12:150. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 73] [Cited by in RCA: 84] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 23. | Stirbu I, Kunst AE, Bos V, Mackenbach JP. Differences in avoidable mortality between migrants and the native Dutch in The Netherlands. BMC Public Health. 2006;6:78. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 87] [Cited by in RCA: 83] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 24. | Gholap N, Davies M, Patel K, Sattar N, Khunti K. Type 2 diabetes and cardiovascular disease in South Asians. Prim Care Diabetes. 2011;5:45-56. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 143] [Cited by in RCA: 157] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 25. | Available from: https://osservatorioarno.cineca.org/diabete/razionale2011.htm. |
| 26. | Marchesini G, Bernardi D, Miccoli R, Rossi E, Vaccaro O, De Rosa M, Bonora E, Bruno G. Under-treatment of migrants with diabetes in a universalistic health care system: the ARNO Observatory. Nutr Metab Cardiovasc Dis. 2014;24:393-399. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 27] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 27. | Choukem SP, Fabreguettes C, Akwo E, Porcher R, Nguewa JL, Bouche C, Kaze FF, Kengne AP, Vexiau P, Mbanya JC. Influence of migration on characteristics of type 2 diabetes in sub-Saharan Africans. Diabetes Metab. 2014;40:56-60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 20] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 28. | Tillin T, Hughes AD, Godsland IF, Whincup P, Forouhi NG, Welsh P, Sattar N, McKeigue PM, Chaturvedi N. Insulin resistance and truncal obesity as important determinants of the greater incidence of diabetes in Indian Asians and African Caribbeans compared with Europeans: the Southall And Brent REvisited (SABRE) cohort. Diabetes Care. 2013;36:383-393. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 114] [Cited by in RCA: 134] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 29. | Stronks K, Snijder MB, Peters RJ, Prins M, Schene AH, Zwinderman AH. Unravelling the impact of ethnicity on health in Europe: the HELIUS study. BMC Public Health. 2013;13:402. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 164] [Cited by in RCA: 220] [Article Influence: 16.9] [Reference Citation Analysis (0)] |
| 30. | Sivaprasad S, Gupta B, Gulliford MC, Dodhia H, Mohamed M, Nagi D, Evans JR. Ethnic variations in the prevalence of diabetic retinopathy in people with diabetes attending screening in the United Kingdom (DRIVE UK). PLoS One. 2012;7:e32182. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 74] [Cited by in RCA: 103] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 31. | Davis TM, Coleman RL, Holman RR. Ethnicity and long-term vascular outcomes in Type 2 diabetes: a prospective observational study (UKPDS 83). Diabet Med. 2014;31:200-207. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 51] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 32. | Vandenheede H, Deboosere P, Stirbu I, Agyemang CO, Harding S, Juel K, Rafnsson SB, Regidor E, Rey G, Rosato M. Migrant mortality from diabetes mellitus across Europe: the importance of socio-economic change. Eur J Epidemiol. 2012;27:109-117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 58] [Article Influence: 3.9] [Reference Citation Analysis (1)] |
| 33. | Mather HM, Chaturvedi N, Fuller JH. Mortality and morbidity from diabetes in South Asians and Europeans: 11-year follow-up of the Southall Diabetes Survey, London, UK. Diabet Med. 1998;15:53-59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 34. | Zimmet PZ, McCarty DJ, de Courten MP. The global epidemiology of non-insulin-dependent diabetes mellitus and the metabolic syndrome. J Diabetes Complications. 1997;11:60-68. [PubMed] |
| 35. | Oza-Frank R, Narayan KM. Overweight and diabetes prevalence among US immigrants. Am J Public Health. 2010;100:661-668. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 87] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 36. | Department of Health and Human Services, Centers for Disease Control and Prevention. National Diabetes Fact Sheet, 2007. Available from: http://search.cdc.gov/search?query=diabetes fact sheet&utf8=&affiliate=cdc-main. |
| 37. | Okosun IS, Liao Y, Rotimi CN, Prewitt TE, Cooper RS. Abdominal adiposity and clustering of multiple metabolic syndrome in White, Black and Hispanic americans. Ann Epidemiol. 2000;10:263-270. [PubMed] |
| 38. | Flegal KM, Carroll MD, Ogden CL, Johnson CL. Prevalence and trends in obesity among US adults, 1999-2000. JAMA. 2002;288:1723-1727. [PubMed] |
| 39. | Brancati FL, Kao WH, Folsom AR, Watson RL, Szklo M. Incident type 2 diabetes mellitus in African American and white adults: the Atherosclerosis Risk in Communities Study. JAMA. 2000;283:2253-2259. [PubMed] |
| 40. | King GL, McNeely MJ, Thorpe LE, Mau ML, Ko J, Liu LL, Sun A, Hsu WC, Chow EA. Understanding and addressing unique needs of diabetes in Asian Americans, native Hawaiians, and Pacific Islanders. Diabetes Care. 2012;35:1181-1188. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 83] [Cited by in RCA: 105] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 41. | Lee JW, Brancati FL, Yeh HC. Trends in the prevalence of type 2 diabetes in Asians versus whites: results from the United States National Health Interview Survey, 1997-2008. Diabetes Care. 2011;34:353-357. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 206] [Cited by in RCA: 245] [Article Influence: 16.3] [Reference Citation Analysis (1)] |
| 42. | Karter AJ, Schillinger D, Adams AS, Moffet HH, Liu J, Adler NE, Kanaya AM. Elevated rates of diabetes in Pacific Islanders and Asian subgroups: The Diabetes Study of Northern California (DISTANCE). Diabetes Care. 2013;36:574-579. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 171] [Cited by in RCA: 244] [Article Influence: 18.8] [Reference Citation Analysis (0)] |
| 43. | McGarvey ST, Seiden A. Health, well-being, and social context of Samoan migrant populations. NAPA Bulletin. 2010;34:213-228. |
| 44. | Tan ED, Davis WA, Davis TM. Changes in characteristics and management of Asian and Anglo-Celts with type 2 diabetes over a 15-year period in an urban Australian community: The Fremantle Diabetes Study. J Diabetes. 2016;8:139-147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 45. | Abouzeid M, Philpot B, Janus ED, Coates MJ, Dunbar JA. Type 2 diabetes prevalence varies by socio-economic status within and between migrant groups: analysis and implications for Australia. BMC Public Health. 2013;13:252. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 50] [Cited by in RCA: 58] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 46. | Tan ED, Davis WA, Davis TM. Characteristics and prognosis of Asian patients with type 2 diabetes from a multi-racial Australian community: the Fremantle Diabetes Study. Intern Med J. 2013;43:1125-1132. [PubMed] |
| 47. | Hodge AM, Flicker L, O’Dea K, English DR, Giles GG. Diabetes and ageing in the Melbourne Collaborative Cohort Study (MCCS). Diabetes Res Clin Pract. 2013;100:398-403. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 48. | Hodge AM, English DR, O’Dea K, Giles GG. Increased diabetes incidence in Greek and Italian migrants to Australia: how much can be explained by known risk factors? Diabetes Care. 2004;27:2330-2334. [PubMed] |
| 49. | Welborn TA, Knuiman MW, Bartholomew HC, Whittall DE. 1989-90 National Health Survey: prevalence of self-reported diabetes in Australia. Med J Aust. 1995;163:129-132. [PubMed] |
| 50. | McKay R, McCarty CA, Taylor HR. Diabetes in Victoria, Australia: the Visual Impairment Project. Aust N Z J Public Health. 2000;24:565-569. [PubMed] |
| 51. | DECODE Study Group; European Diabetes Epidemiology Group. Age, body mass index and glucose tolerance in 11 European population-based surveys. Diabet Med. 2002;19:558-565. [PubMed] |
| 52. | Anikeeva O, Bi P, Hiller JE, Ryan P, Roder D, Han GS. Trends in migrant mortality rates in Australia 1981-2007: a focus on the National Health Priority Areas other than cancer. Ethn Health. 2015;20:29-48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 17] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 53. | Agyemang C, Owusu-Dabo E, de Jonge A, Martins D, Ogedegbe G, Stronks K. Overweight and obesity among Ghanaian residents in The Netherlands: how do they weigh against their urban and rural counterparts in Ghana? Public Health Nutr. 2009;12:909-916. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 66] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 54. | Bhatnagar D, Anand IS, Durrington PN, Patel DJ, Wander GS, Mackness MI, Creed F, Tomenson B, Chandrashekhar Y, Winterbotham M. Coronary risk factors in people from the Indian subcontinent living in west London and their siblings in India. Lancet. 1995;345:405-409. [PubMed] |
| 55. | Gujral UP, Narayan KM, Pradeepa RG, Deepa M, Ali MK, Anjana RM, Kandula NR, Mohan V, Kanaya AM. Comparing Type 2 Diabetes, Prediabetes, and Their Associated Risk Factors in Asian Indians in India and in the U.S.: The CARRS and MASALA Studies. Diabetes Care. 2015;38:1312-1318. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 49] [Cited by in RCA: 50] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 56. | Kanaya AM, Herrington D, Vittinghoff E, Ewing SK, Liu K, Blaha MJ, Dave SS, Qureshi F, Kandula NR. Understanding the high prevalence of diabetes in U.S. south Asians compared with four racial/ethnic groups: the MASALA and MESA studies. Diabetes Care. 2014;37:1621-1628. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 133] [Cited by in RCA: 201] [Article Influence: 16.8] [Reference Citation Analysis (0)] |
| 57. | Qiao Q, Hu G, Tuomilehto J, Nakagami T, Balkau B, Borch-Johnsen K, Ramachandran A, Mohan V, Iyer SR, Tominaga M. Age- and sex-specific prevalence of diabetes and impaired glucose regulation in 11 Asian cohorts. Diabetes Care. 2003;26:1770-1780. [PubMed] |
| 58. | Griffiths PL, Bentley ME. The nutrition transition is underway in India. J Nutr. 2001;131:2692-2700. [PubMed] |
| 59. | Shetty PS. Nutrition transition in India. Public Health Nutr. 2002;5:175-182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 245] [Cited by in RCA: 223] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 60. | Venkatesh S, Weatherspoon LJ, Kaplowitz SA, Song WO. Acculturation and glycemic control of Asian Indian adults with type 2 diabetes. J Community Health. 2013;38:78-85. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 21] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 61. | Agyemang C, Beune E, Meeks K, Owusu-Dabo E, Agyei-Baffour P, Aikins Ad, Dodoo F, Smeeth L, Addo J, Mockenhaupt FP. Rationale and cross-sectional study design of the Research on Obesity and type 2 Diabetes among African Migrants: the RODAM study. BMJ Open. 2014;4:e004877. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 77] [Cited by in RCA: 96] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 62. | Chowdhury R, Narayan KM, Zabetian A, Raj S, Tabassum R. Genetic studies of type 2 diabetes in South Asians: a systematic overview. Curr Diabetes Rev. 2014;10:258-274. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 15] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 63. | Mahajan A, Go MJ, Zhang W, Below JE, Gaulton KJ, Ferreira T, Horikoshi M, Johnson AD, Ng MC, Prokopenko I. Genome-wide trans-ancestry meta-analysis provides insight into the genetic architecture of type 2 diabetes susceptibility. Nat Genet. 2014;46:234-244. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 899] [Cited by in RCA: 824] [Article Influence: 68.7] [Reference Citation Analysis (0)] |
| 64. | Shah A, Kanaya AM. Diabetes and associated complications in the South Asian population. Curr Cardiol Rep. 2014;16:476. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 105] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 65. | Commodore-Mensah Y, Samuel LJ, Dennison-Himmelfarb CR, Agyemang C. Hypertension and overweight/obesity in Ghanaians and Nigerians living in West Africa and industrialized countries: a systematic review. J Hypertens. 2014;32:464-472. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 56] [Cited by in RCA: 60] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 66. | Rodriguez F, Ferdinand KC. Hypertension in minority populations: new guidelines and emerging concepts. Adv Chronic Kidney Dis. 2015;22:145-153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 28] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 67. | Razum O. Commentary: of salmon and time travellers--musing on the mystery of migrant mortality. Int J Epidemiol. 2006;35:919-921. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 69] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 68. | Bollini P, Siem H. No real progress towards equity: health of migrants and ethnic minorities on the eve of the year 2000. Soc Sci Med. 1995;41:819-828. [PubMed] |
| 69. | Parkin DM, Khlat M. Studies of cancer in migrants: rationale and methodology. Eur J Cancer. 1996;32A:761-771. [PubMed] |
| 70. | Harding S, Rosato M, Teyhan A. Trends in cancer mortality among migrants in England and Wales, 1979-2003. Eur J Cancer. 2009;45:2168-2179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 27] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 71. | Stirbu I, Kunst AE, Vlems FA, Visser O, Bos V, Deville W, Nijhuis HG, Coebergh JW. Cancer mortality rates among first and second generation migrants in the Netherlands: Convergence toward the rates of the native Dutch population. Int J Cancer. 2006;119:2665-2672. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 76] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 72. | Zeeb H, Razum O, Blettner M, Stegmaier C. Transition in cancer patterns among Turks residing in Germany. Eur J Cancer. 2002;38:705-711. [PubMed] |
| 73. | Harding S, Rosato M, Teyhan A. Trends for coronary heart disease and stroke mortality among migrants in England and Wales, 1979-2003: slow declines notable for some groups. Heart. 2008;94:463-470. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 109] [Cited by in RCA: 105] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 74. | Jatrana S, Pasupuleti SS, Richardson K. Nativity, duration of residence and chronic health conditions in Australia: do trends converge towards the native-born population? Soc Sci Med. 2014;119:53-63. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 42] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 75. | Norredam M, Agyemang C, Hoejbjerg Hansen OK, Petersen JH, Byberg S, Krasnik A, Kunst AE. Duration of residence and disease occurrence among refugees and family reunited immigrants: test of the ‘healthy migrant effect’ hypothesis. Trop Med Int Health. 2014;19:958-967. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 95] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 76. | Riosmena F, Wong R, Palloni A. Migration selection, protection, and acculturation in health: a binational perspective on older adults. Demography. 2013;50:1039-1064. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 202] [Cited by in RCA: 175] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 77. | Weitoft GR, Gullberg A, Hjern A, Rosén M. Mortality statistics in immigrant research: method for adjusting underestimation of mortality. Int J Epidemiol. 1999;28:756-763. [PubMed] |
| 78. | Ramachandran A, Ma RC, Snehalatha C. Diabetes in Asia. Lancet. 2010;375:408-418. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 519] [Cited by in RCA: 563] [Article Influence: 35.2] [Reference Citation Analysis (1)] |
| 79. | Gentilucci UV, Picardi A, Manfrini S, Khazrai YM, Fioriti E, Altomare M, Guglielmi C, Di Stasio E, Pozzilli P. Westernization of the Filipino population resident in Rome: obesity, diabetes and hypertension. Diabetes Metab Res Rev. 2008;24:364-370. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 80. | Bhopal R, Hayes L, White M, Unwin N, Harland J, Ayis S, Alberti G. Ethnic and socio-economic inequalities in coronary heart disease, diabetes and risk factors in Europeans and South Asians. J Public Health Med. 2002;24:95-105. [PubMed] |
| 81. | Schouten BC, Meeuwesen L. Cultural differences in medical communication: a review of the literature. Patient Educ Couns. 2006;64:21-34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 386] [Cited by in RCA: 385] [Article Influence: 19.3] [Reference Citation Analysis (0)] |
| 82. | Meeuwesen L, Harmsen JA, Bernsen RM, Bruijnzeels MA. Do Dutch doctors communicate differently with immigrant patients than with Dutch patients? Soc Sci Med. 2006;63:2407-2417. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 71] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 83. | Kressin NR, Wang F, Long J, Bokhour BG, Orner MB, Rothendler J, Clark C, Reddy S, Kozak W, Kroupa LP. Hypertensive patients’ race, health beliefs, process of care, and medication adherence. J Gen Intern Med. 2007;22:768-774. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 78] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 84. | Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. 1995;36:1-10. [PubMed] |
| 85. | Denktaş S, Koopmans G, Birnie E, Foets M, Bonsel G. Underutilization of prescribed drugs use among first generation elderly immigrants in the Netherlands. BMC Health Serv Res. 2010;10:176. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 13] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 86. | Peeters B, Van Tongelen I, Duran Z, Yüksel G, Mehuys E, Willems S, Remon JP, Boussery K. Understanding medication adherence among patients of Turkish descent with type 2 diabetes: a qualitative study. Ethn Health. 2015;20:87-105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 30] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 87. | Mladovsky P, Ingleby D, McKee M, Rechel B. Good practices in migrant health: the European experience. Clin Med (Lond). 2012;12:248-252. [PubMed] |
| 88. | Rechel B, Mladovsky P, Ingleby D, Mackenbach JP, McKee M. Migration and health in an increasingly diverse Europe. Lancet. 2013;381:1235-1245. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 563] [Cited by in RCA: 553] [Article Influence: 42.5] [Reference Citation Analysis (0)] |
| 89. | Fernando E, Razak F, Lear SA, Anand SS. Cardiovascular Disease in South Asian Migrants. Can J Cardiol. 2015;31:1139-1150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 61] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 90. | Dogra S, Meisner BA, Ardern CI. Variation in mode of physical activity by ethnicity and time since immigration: a cross-sectional analysis. Int J Behav Nutr Phys Act. 2010;7:75. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 54] [Cited by in RCA: 62] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 91. | Sorkin DH, Biegler KA, Billimek J. Differences in Self-Reported Physical Activity and Body Mass Index Among Older Hispanic and Non-Hispanic White Men and Women: Findings from the 2009 California Health Interview Survey. J Am Geriatr Soc. 2015;63:2158-2163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 92. | Sarich PE, Ding D, Sitas F, Weber MF. Co-occurrence of chronic disease lifestyle risk factors in middle-aged and older immigrants: A cross-sectional analysis of 264,102 Australians. Prev Med. 2015;81:209-215. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 27] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 93. | Fischbacher CM, Hunt S, Alexander L. How physically active are South Asians in the United Kingdom? A literature review. J Public Health (Oxf). 2004;26:250-258. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 158] [Cited by in RCA: 175] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 94. | Martin Y, Collet TH, Bodenmann P, Blum MR, Zimmerli L, Gaspoz JM, Battegay E, Cornuz J, Rodondi N. The lower quality of preventive care among forced migrants in a country with universal healthcare coverage. Prev Med. 2014;59:19-24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (1)] |
| 95. | Ringbäck Weitoft G, Ericsson O, Löfroth E, Rosén M. Equal access to treatment? Population-based follow-up of drugs dispensed to patients after acute myocardial infarction in Sweden. Eur J Clin Pharmacol. 2008;64:417-424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 29] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 96. | Volodina A, Bertsche T, Kostev K, Winkler V, Haefeli WE, Becher H. Drug utilization patterns and reported health status in ethnic German migrants (Aussiedler) in Germany: a cross-sectional study. BMC Public Health. 2011;11:509. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 97. | Norredam M, Nielsen SS, Krasnik A. Migrants’ utilization of somatic healthcare services in Europe--a systematic review. Eur J Public Health. 2010;20:555-563. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 176] [Cited by in RCA: 204] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 98. | Modesti PA, Bianchi S, Borghi C, Cameli M, Capasso G, Ceriello A, Ciccone MM, Germanò G, Maiello M, Muiesan ML. Cardiovascular health in migrants: current status and issues for prevention. A collaborative multidisciplinary task force report. J Cardiovasc Med (Hagerstown). 2014;15:683-692. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 28] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 99. | Marchesini G, Forlani G, Rossi E, Berti A, De Rosa M. The direct economic cost of pharmacologically-treated diabetes in Italy-2006. The ARNO observatory. Nutr Metab Cardiovasc Dis. 2011;21:339-346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 31] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 100. | Cadario F, Cerutti F, Savastio S, Rabbone I, Tumini S, Bruno G. Increasing burden, younger age at onset and worst metabolic control in migrant than in Italian children with type 1 diabetes: an emerging problem in pediatric clinics. Acta Diabetol. 2014;51:263-267. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 101. | Mladovsky P. Migration and health in the EU, The London School of Economics and Political Science, 2007. Available from: http://ec.europa.eu/employment_social/social_situation/docs/rn_migration_health.pdf. |
| 103. | Imkampe AK, Gulliford MC. Increasing socio-economic inequality in type 2 diabetes prevalence--repeated cross-sectional surveys in England 1994-2006. Eur J Public Health. 2011;21:484-490. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 66] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 104. | Tripp-Reimer T, Choi E, Skemp Kelley L, Enslein JC. Cultural barrier to care: inverting the problem. Diabetes Spectrum. 2001;14:13-22. [DOI] [Full Text] |
| 105. | Giorda CB. The role of the care model in modifying prognosis in diabetes. Nutr Metab Cardiovasc Dis. 2013;23:11-16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 106. | Vlaar EM, van Valkengoed IG, Nierkens V, Nicolaou M, Middelkoop BJ, Stronks K. Feasibility and effectiveness of a targeted diabetes prevention program for 18 to 60-year-old South Asian migrants: design and methods of the DH!AAN study. BMC Public Health. 2012;12:371. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 26] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 107. | Hjelm K, Bard K. Beliefs about health and illness in latin-american migrants with diabetes living in sweden. Open Nurs J. 2013;7:57-65. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 16] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
P- Reviewer: Charoenphandhu N, Guerrero-Romero F S- Editor: Ji FF L- Editor: A E- Editor: Lu YJ