Published online Nov 15, 2025. doi: 10.4239/wjd.v16.i11.113457
Revised: September 16, 2025
Accepted: October 23, 2025
Published online: November 15, 2025
Processing time: 80 Days and 17.7 Hours
Type 2 diabetes mellitus (T2DM) and obesity are growing global pandemics that shares the common characteristic of insulin resistance (IR). IR leads to progressive β-cell failure, worsening T2DM and its cardiovascular complications. Thus, early diagnosis of IR is important to prevent and reverse β-cell dedifferentiation. However, there is a lack of accessible, non-invasive and affordable tools to early diagnose and stratify IR. The gold standard method used in the research setting is the hyperinsulinemic-euglycemic clamp, however it is invasive, laborious, expensive and difficult to apply at a large scale. Hou et al presents a potential novel surrogate biomarker for diagnosing IR in T2DM. Magnetic resonance imaging derived biomarkers can potentially become the accessible and non-invasive alternative to the hyperinsulinemic-euglycemic clamp, enabling the timely diagnosis of IR with potential clinical applications in T2DM treatments and preventative care.
Core Tip: Hou et al presents a potential novel surrogate biomarker for diagnosing insulin resistance (IR) in type 2 diabetes mellitus. Their study demonstrates magnetic resonance imaging-derived multiparametric biomarkers for IR at the L4-L5 paravertebral muscles. If validated, this represents an accessible and non-invasive tool for early diagnosis of IR with potential clinical diagnostic applications.
- Citation: Jiang H, Henley D, Jiang FX. Potentially novel surrogate biomarker for diagnosing insulin resistance in type 2 diabetes. World J Diabetes 2025; 16(11): 113457
- URL: https://www.wjgnet.com/1948-9358/full/v16/i11/113457.htm
- DOI: https://dx.doi.org/10.4239/wjd.v16.i11.113457
We read with interest the recent article “Magnetic resonance imaging derived biomarkers for the diagnosis of type 2 diabetes with insulin resistance: A pilot study” by Hou et al[1] in the World Journal of Diabetes.
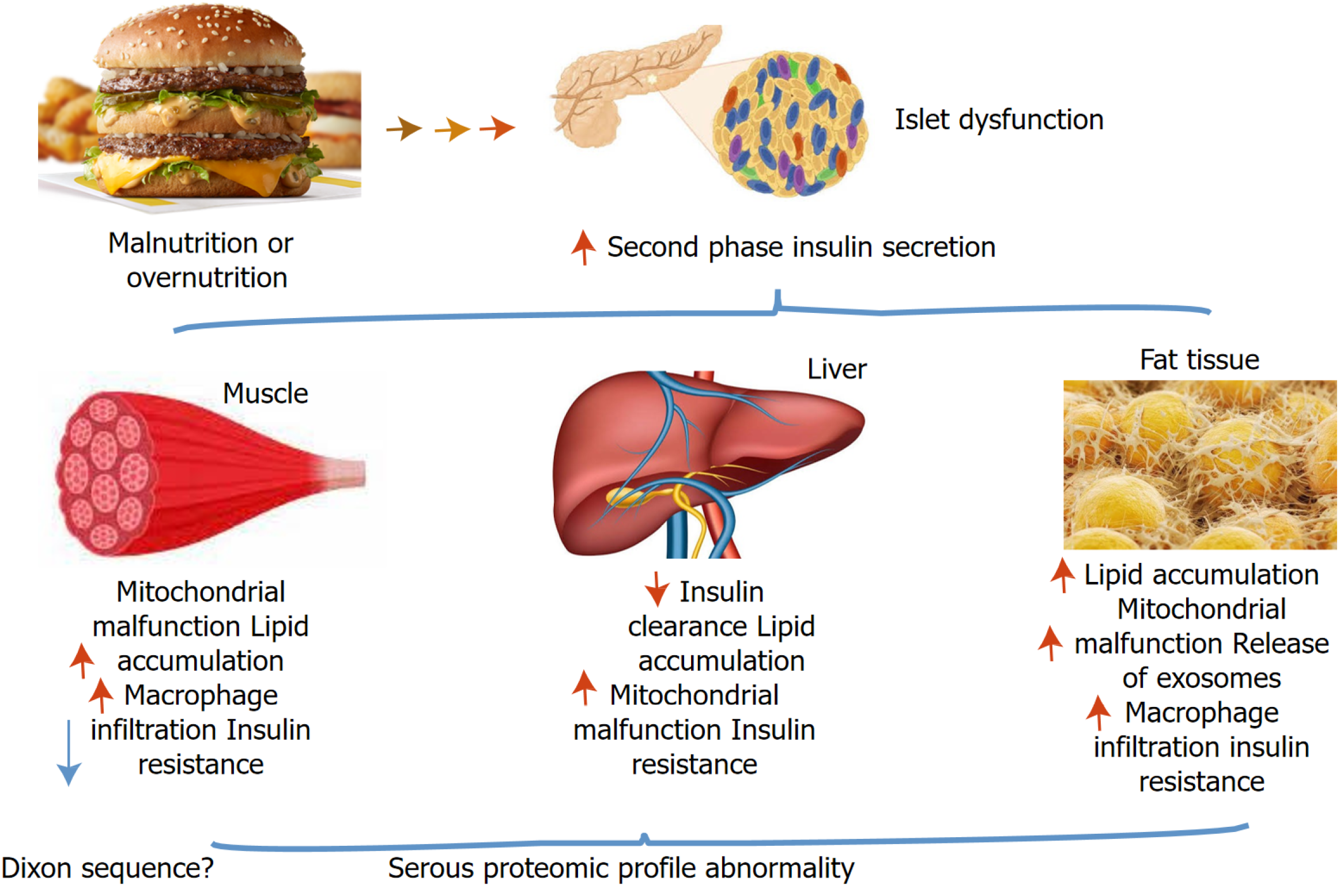
Insulin resistance (IR) is a risk factor for several metabolic diseases including type 2 diabetes mellitus (T2DM) and obesity. The molecular and cellular mechanisms of IR have been thoroughly reviewed recently[2]. Quantitating molecular signalling[3] and phenotypic traits are fundamental to T2DM personalised precision medicine. Non-invasive biomarkers with magnetic resonance imaging (MRI) may help diagnose an IR phenotypic trait in T2DM (T2DM-IR). A pilot study by Hou et al[1] identified a promising non-invasive biomarker. Their study may contribute to the field by improving the diagnosis and stratification of T2DM-IR through MRI of intramyocellular lipid (IMCL) in the erector and psoas muscles (Figure 1), compared to the current invasive gold standard technique.
The current gold standard method for assessing peripheral IR in vivo is the hyperinsulinemic-euglycemic clamp. This method involves co-administration of continuous insulin infusion to increase plasma insulin with an exogenous glucose infusion to maintain constant fasting glucose levels and directly assess whole-body insulin sensitivity through calculation of glucose utilisation in response to hyperinsulinemia. To conduct this laborious and invasive technique requires highly trained staff and is an overall expensive endeavour[4]. Therefore, this method is impractical to apply to large scale research studies. Previously, there were many reports using saliva[5], triglyceride/high-density lipoprotein cholesterol ratio[6] and lipid indices[7] as biochemical markers for diagnosing IR.
Hou et al[1] explores an alternative, non-invasive, less intensive imaging technique focused at the L4-L5 vertebral levels for assessing early-stage IR using multiparametric protocols of quantitative Dixon (Q-Dixon) and diffusion MRI protocols. The Q-Dixon technique assesses ectopic lipid deposition in the paravertebral muscles including the psoas, erector and multifidus; enables fat fraction quantification to measure total fat content, IMCL, extramyocellular lipid and assesses vertebral bone health. T2DM-IR was found to be associated with higher IMCL in the psoas and erector. The most significant biomarkers for T2DM-IR in their study were the IMCL/muscle ratio and total fat content/muscle ratio of the psoas; as well as the IMCL, IMCL/muscle ratio and total fat content of the erector[1].
Although MRI-derived biomarkers are less invasive and more accessible than the hyperinsulinemic-euglycemic clamp, a wide discrepancy of global accessibility to MRI services does exist. There are less infrastructure and dedicated workforce in low and middle-income countries[8], reflecting the cost and accessibility barriers to MRIs themselves. Nevertheless, there has been great advances to MRI technology, hardware and computational technology over the years, along with demand in developing markets generating interest in the development of low-cost, portable and accessible MRI, which may hopefully eventuate in the future[9].
Hou et al[1] was a single-centre, cross-sectional study of 97 participants. Clearly, the study requires further validation with a larger sample size and needs to be reproduced in multiple research centres. The findings of Hou et al[1] presents an interesting development for quantifying IR, which may help to early diagnose and prevent disease advancement with progressive β-cell dedifferentiation and failure, and reduce costly complications of T2DM. With further validation and follow-up multi-centre longitudinal studies, the multiparametric MRI protocol presented by Hou et al[1] could be a potential diagnostic tool with clinical applications for quantitation of IR.
Obesity is associated with not only lipid accumulation in adipose tissue but also in ectopic tissues. Ectopic lipid storage in non-adipose tissues such as the skeletal muscle, liver and heart is associated with IR through lipotoxicity and impairment of insulin signalling[10]. In terms of systemic IR, the skeletal muscle is important as the main site of insulin-dependent glucose disposal. IMCL is a type of ectopic lipid in skeletal muscle found to be a useful predictor of T2DM in this study[1].
If validated, MRI-derived biomarkers may be used not only in research settings as is the case for the hyperinsulinemic-euglycemic clamp but may also have clinical applications. The MRI-derived biomarkers in this study could potentially be used in conjunction with standard serological tests such as fasting/random blood glucose, glycated haemoglobin, C-peptide and lipid profile, to risk-stratify patients with T2DM-IR. Other possible clinical indications may include quantifying IR in obese individuals who are not yet diabetic but at risk of progressing to T2DM, allowing potential early detection of T2DM risk and may help prompt preventative measures in these patients.
With the ever-growing global prevalence of obesity and T2DM, there are likely more individuals with concurrent type 1 diabetes mellitus and IR with a family history of T2DM (“double diabetes”)[11] who require higher doses of insulin. Type 1 diabetes mellitus (T1DM) is traditionally exclusively treated with insulin. For future research, it would be useful to quantify IR in T1DM patients and assess if there is a role for oral antihyperglycemics that enhance insulin sensitivity such as metformin and thiazolidinediones. If found to make a significant reduction in the MRI-derived biomarkers of IR, there may be a role for insulin sensitisers as a valuable adjunct for T1DM treatment, especially in those requiring high insulin doses. Additionally, a study assessing the changes in the multiparametric biomarkers of paravertebral muscle lipid and fat concentration before and after insulin sensitising medications in various other cohorts such as people with pre-diabetes would be interesting to see.
| 1. | Hou BW, Ran Z, Li YT, Zhang J, Chu YQ, Gharaibeh NM, Li XM. Magnetic resonance imaging derived biomarkers for the diagnosis of type 2 diabetes with insulin resistance: A pilot study. World J Diabetes. 2025;16:110183. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 2. | Accili D, Deng Z, Liu Q. Insulin resistance in type 2 diabetes mellitus. Nat Rev Endocrinol. 2025;21:413-426. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 26] [Article Influence: 26.0] [Reference Citation Analysis (0)] |
| 3. | Kjærgaard J, Stocks B, Henderson J, Freemantle JB, Rizo-Roca D, Puglia M, Madrazo Montoya M, Andersson D, Bäckdahl J, Eriksson-Hogling D, Stidsen JV, Wierer M, Rasmussen S, Sakamoto K, Højlund K, Rydén M, Zierath JR, Krook A, Deshmukh AS. Personalized molecular signatures of insulin resistance and type 2 diabetes. Cell. 2025;188:4106-4122.e16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 8] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 4. | Tam CS, Xie W, Johnson WD, Cefalu WT, Redman LM, Ravussin E. Defining insulin resistance from hyperinsulinemic-euglycemic clamps. Diabetes Care. 2012;35:1605-1610. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 156] [Cited by in RCA: 273] [Article Influence: 19.5] [Reference Citation Analysis (0)] |
| 5. | Desai GS, Mathews ST. Saliva as a non-invasive diagnostic tool for inflammation and insulin-resistance. World J Diabetes. 2014;5:730-738. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 100] [Cited by in RCA: 101] [Article Influence: 8.4] [Reference Citation Analysis (2)] |
| 6. | Azarpazhooh MR, Najafi F, Darbandi M, Kiarasi S, Oduyemi T, Spence JD. Triglyceride/High-Density Lipoprotein Cholesterol Ratio: A Clue to Metabolic Syndrome, Insulin Resistance, and Severe Atherosclerosis. Lipids. 2021;56:405-412. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 40] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 7. | Lee J, Kim B, Kim W, Ahn C, Choi HY, Kim JG, Kim J, Shin H, Kang JG, Moon S. Lipid indices as simple and clinically useful surrogate markers for insulin resistance in the U.S. population. Sci Rep. 2021;11:2366. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 84] [Article Influence: 16.8] [Reference Citation Analysis (0)] |
| 8. | Jalloul M, Miranda-Schaeubinger M, Noor AM, Stein JM, Amiruddin R, Derbew HM, Mango VL, Akinola A, Hart K, Weygand J, Pollack E, Mohammed S, Scheel JR, Shell J, Dako F, Mhatre P, Kulinski L, Otero HJ, Mollura DJ. MRI scarcity in low- and middle-income countries. NMR Biomed. 2023;36:e5022. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 43] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 9. | Wald LL, McDaniel PC, Witzel T, Stockmann JP, Cooley CZ. Low-cost and portable MRI. J Magn Reson Imaging. 2020;52:686-696. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 149] [Article Influence: 24.8] [Reference Citation Analysis (0)] |
| 10. | Borén J, Taskinen MR, Olofsson SO, Levin M. Ectopic lipid storage and insulin resistance: a harmful relationship. J Intern Med. 2013;274:25-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 156] [Cited by in RCA: 174] [Article Influence: 13.4] [Reference Citation Analysis (0)] |
| 11. | Cleland SJ, Fisher BM, Colhoun HM, Sattar N, Petrie JR. Insulin resistance in type 1 diabetes: what is 'double diabetes' and what are the risks? Diabetologia. 2013;56:1462-1470. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 142] [Cited by in RCA: 174] [Article Influence: 13.4] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/